What is urea
During the digestion of proteins, peptide chains are broken down into amino acids. As a result of their deamination (detachment of the amino group from the amino acid molecule) and further biochemical transformation, ammonia is formed in the body. This is a toxic product of nitrogen metabolism that has a detrimental effect on organs, primarily on the nervous system.
In tissues, ammonia binds with glutamic acid to form glutamine, a harmless transport compound that easily passes through cell membranes. In this form, the nitrogenous compound is delivered to the liver. Here it is neutralized and converted into non-toxic urea.
This process begins in mitochondria and continues in the cytoplasm of liver cells with the participation of a number of enzymes and amino acids. The resulting urea from hepatocytes is transported into the blood and then excreted by the kidneys.
There is always one or another amount of urea in the blood.
Changing its level depends on:
- on the amount of protein consumed in food;
- on the intensity of the breakdown of the body’s own tissue proteins;
- on the functional state of the liver and the capabilities of its enzyme systems;
- on the excretory capacity of the kidneys.
What it is
A certain amount of urea is always present in the body, because protein metabolism in the body occurs continuously. Blood test for urea, what is it? This is a mark showing the state of metabolism of nitrogenous substances in the body. If it is elevated, it means that either the protein is being used irrationally, or the kidneys are not working satisfactorily. Diagnosis of the metabolism of nitrogenous substances will be incomplete without studying the dynamics of creatine, creatinine, ammonia, etc.
An increased level of urea in the blood compared to the physiological norm (physiologica normam) provides grounds for examining the kidneys for possible pathology. It is possible that their unsatisfactory functioning prevents the body from getting rid of excess urea.
Both urea and uric acidum are nitrogen-containing substances. But their origins are different. Urea is a simple substance, formed in the liver during the neutralization of ammonia, which is extremely toxic to the body, and uric acidum is formed during the breakdown of nucleic acids containing a heterocycle.
Determining the urea content in the blood is informative when comparing the actual urea content with the physiologica normam indicators. The concentration of urea in the blood is calculated in millimoles of the substance per liter of blood, varies within significant limits and depends on age. The older the patient, the higher the lower limit of normal. This is understandable; a young body copes better with the utilization of nitrogen metabolism products.
The result of a blood test for urea is greatly influenced by food intake. Therefore, for the determination of urea, .
The most complete information about the process of metabolism of nitrogen-containing substances in the body is provided by analysis of urea and (1-methylglycocyamidine). This substance is synthesized as a result of a chain of biochemical reactions of specific nitrogenous compounds that provide energy to muscle fibers. Creatinine, along with urea, appears to be a waste product of nitrogen metabolism and must be removed from the body. As in the case of urea, the physiologica normam of creatinine has age-related fluctuations.
Indicates renal pathologies. However, in the presence of clinical symptoms of kidney disease, 1-methylglycocyamidine may be normal or lower. Such blood tests are typical for patients with low body weight, amputees and the elderly.
Exceeding the norm of urea in the blood does not in all cases indicate the presence of a disease, and a blood test for urea, the norm does not in all cases indicate the absence of pathology.
Some may occur in people after eating too much protein. Heavy physical labor and overload in athletes also lead to an excess of urea. Most often this phenomenon is observed in men.
It is necessary to distinguish who has elevated urea levels: athletes and people involved in hard work, or alcoholics and heavy smokers. Eating incomplete proteins is accompanied by their low absorption, therefore, there will be an excess of waste turning into ammonia. From constant overload, the liver becomes inflamed, and the kidneys cannot cope with removing waste from protein combustion.
A urea test carried out by a doctor allows one to suspect diseases, the cause or result of which is increased degradation of proteins in the body. These can be chronic diseases: amyloidosis, grosserulonephritis, post-burn complications, malignant tumors, pathologies of the endocrine system.
Deviations from the norm in a downward direction also indicate the presence of pathology. Since the liver is responsible for the synthesis of urea, underproduction of urea indicates the failure of the organ. The cause of this pathology may be cirrhosis (sclerosis) of the liver and hepatitis of various etiologies. If a drop in urea is accompanied by an increase in enzyme activity, indicating an intensification of protein breakdown or synthesis processes, then the suspicion of liver disease receives additional confirmation.
It may also indicate other anomalies: muscle weakness, sudden weight loss, loss of strength, swelling.
The meaning and functions of urea in the body
Urea is a neutral, non-toxic, water-soluble substance, the end product of protein metabolism. It is synthesized as a result of the metabolism of amino acids in order to neutralize ammonia.
Does not perform independent functions in the body. In fact, it is a transport form for waste toxic components that are not needed by the body. Excretion is carried out by the kidneys and urine.
An increase in protein content in food or an increase in the breakdown of tissue's own proteins is accompanied by a change in the rate of urea formation. In this way, nitrogen balance is maintained.
Urea norms
The table showing the norms of urea in the human body is only approximate; the indicators may deviate slightly. In the blood of a healthy person, the urea content in the blood must meet the following standards:
It is important to know that the molar mass of Urea is 60 g/mol. The molar contribution must be taken into account if the urea analysis is calculated in the laboratory in other measurement quantities. This value helps doctors correctly interpret a patient's tests. The level of urea in the blood may vary depending on the presence of pathology and external factors.
Blood urea level
Urea in a biochemical blood test of healthy people varies depending on age and gender.
So, the younger the child, the lower his normal values for this indicator. This is due to increased protein consumption for the needs of a growing body. In newborn days, physiological hyperazotemia may be observed, which is an increase in nitrogenous products in the blood due to increased protein catabolism and insufficient fluid intake.
Women tend to have lower urea levels than men. In pregnant women in later stages, the urea content decreases as a result of activation of protein synthesis to build the tissues of the growing fetus, as well as due to physiological hyperhydration.
With age, the concentration of urea increases due to a decrease in the activity of anabolic processes and the functional ability of the kidneys to excrete.
Urea in a biochemical blood test is measured by the number of millimoles of a substance per liter. 1 mole = 1000 millimoles.
Among women
For women, the norms are:
Urea in biochemical blood test is normal
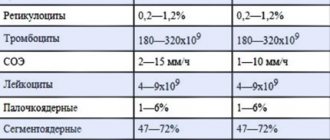
| Age indicator (years) | Urea (mmol/l) |
| 17-21 | 2,8-7,6 |
| 21-51 | 2,5-6,7 |
| Over 51 | 3,6-7,3 |
| During pregnancy up to 19 weeks | 2,9-7,3 |
| During pregnancy at 19-40 weeks | 1,5-4,6 |
In men
The following standard indicators have been established for men:
| Age category (in years) | Indicators (mmol/l) |
| 18-20 | 2,9-7,5 |
| 20-50 | 3,2-7,3 |
| Over 50 | 3,0-9,2 |
In children
Children's indicators differ significantly:
| Age group (years) | Norm (mmol/l) |
| Full-term newborns | 1,4-4,3 |
| Newborns premature | 1,1-8,9 |
| Up to 1 | 1,4-5,4 |
| 1-4 | 1,8-6,0 |
| 4-15 | 2,5-6,7 |
| 15-18 | 2,9-7,5 |
Urea in biochemical blood test: reasons for increase and decrease
Almost every person has had a biochemical blood test at least once in their life. It contains many indicators, each of which is very important. One of these indicators is urea, that is, urea.
What is urea?
Urea is the end product of protein breakdown, which is why it receives so much attention.
And most importantly, it is necessary that the urea level is normal, otherwise this may indicate a malfunction in the body.
Urea is excreted from the body through urine, and the kidneys are responsible for its elimination. If its accumulation occurs, then problems directly with the kidneys are first suspected.
When taking a blood urea test, it should be taken into account that this indicator is very important.
Therefore, it is necessary to take the preparation before it responsibly so that nothing affects the final result.
Normal levels of urea in the blood
Urine normal in blood test
When taking a biochemical blood test for urea content, every person wants everything to be normal.
Experts differentiate test results, since at a certain stage of life they may differ:
- For newborns less than one week old, values from 1.1 to 8.9 mmol per liter of blood are considered normal.
- For children whose age will be from one week to one year, values from 1.4 to 6.8 mmol per liter of blood are considered normal.
- For children whose age will be from one year to eighteen years, indicators from 1.8 to 6.4 mmol per liter of blood are considered normal.
- For people whose age is from eighteen to sixty years, values from 2.1 to 7.1 mmol per liter of blood are considered normal.
- For people over 60 years of age, values from 2.9 to 8.2 mmol per liter of blood are considered normal.
When receiving the test results in hand, the patient can see the above indicators, only formed into a table. But you should not try to decipher them yourself, much less draw conclusions, since, focusing on individual characteristics and existing chronic diseases, the indicators may deviate either upward or downward.
Elevated blood urea levels
Despite the fact that a biochemical blood test can determine the level of urea, this will still not be enough to make a complete diagnosis. Sometimes a person takes a test and does not think that he will have problems with this blood component. But if the urea level is significantly higher than normal, this may indicate a number of diseases.
Kidney problems. Often, the main cause of increased levels of urea in the blood is malfunction of the kidneys, because they are responsible for the excretion of the component from the body. Among the most common diseases are pyelonephritis and kidney tuberculosis.
Heart failure, during which the organs do not receive the required amount of oxygen due to malfunctions of the main muscle.
Often the cause of increased urea levels is direct problems with the urinary system.
That is why it is not excreted as the body requires and is retained in the blood. The main diseases that can provoke urea retention include adenoma, tumors in the bladder, and stones. The main danger awaits those who have stones or a tumor in the bladder. As they increase, the outflow will become even more complicated, thereby urea will reach the most critical levels.
More information about the biochemical blood test can be found in the video.
High levels of urine in the blood can also be affected by:
- Oncological diseases, during which cancer cells affect almost all organs, thereby completely changing the functioning of the body and gradually killing it.
- Severe bleeding, which can occur as a result of surgery, as well as serious injury.
- Intestinal obstruction, during which the body experiences intoxication.
- Burns, both mild and severe.
- Myocardial infarction.
In addition to the fact that an increase in urea levels will be noticeable in a blood test, during a conversation with the patient, you can find out that he was tormented by symptoms such as:
- Rare urination. Moreover, the urine had a very pungent odor, even if a sufficient amount of water had been drunk during the day.
- An increase in blood pressure, which often occurs due to the accumulation of urea in the blood. This is especially common in people who have special urinary catheters.
- Fatigue. Due to the increased content of urea in the blood, a person experiences constant fatigue even though he follows a daily routine, eats right and sleeps more than eight hours a day.
In addition to the fact that urea will be elevated in the biochemical blood test, creatinine will also be high. In any case, even with an increased level of urea in the blood, consultation with a specialist is required; in no case should you make a diagnosis yourself and treat it with folk remedies.
Reduced blood urea levels
Reduced Urea level in blood test
In addition to the fact that an increased level of urea in the blood poses a danger, special attention should be paid to such a phenomenon as its decrease.
A downgrade may occur for the following reasons:
- A person has been poisoned by phosphorus or arsenic.
- A person has symptoms of poor intestinal absorption.
- Hepatitis or cirrhosis of the liver.
- A diet during which the food consumed contains little protein.
- There is excess water in the body, which is manifested by swelling of the limbs.
- Pregnancy. During pregnancy, the female body experiences enormous stress, and often women's arms or legs begin to swell, which indicates excess water in the body, which can lead to a decrease in urea levels in the blood.
Urea in a biochemical blood test is an indicator unknown to many people and frightening. But in most transcripts it is written that urea is nothing more than urea. It’s just easier for doctors to call everything in Latin, for their convenience.
If, after taking a biochemical blood test, a person is found to have an increased or decreased level of urea, he will be recommended to undergo further examination to determine the exact cause of this phenomenon.
diagnosislab.com
Reduced level
Urea may have low values when examined as part of a biochemical blood test. This is due to both physiological factors and diseases.
Reasons for low rates in adults and children:
- Insufficient protein content in food.
- Pregnancy.
- Intensive use of proteins due to rapid growth, increased muscle mass, and the use of anabolic steroids.
- Overdose of drugs that affect the activity of liver enzymes.
- Abuse of diuretics.
- Urea synthesis decreases during acidosis, since part of the ammonia is consumed for neutralization with the formation of ammonium salts.
Possible diseases:
- Diseases of the stomach with impaired secretion of proteolytic enzymes (anacidic gastritis, atrophic gastritis, tumor, peptic ulcer).
- Diseases of the small intestine with impaired resorption (enteritis, duodenitis, tumor, peptic ulcer, celiac disease).
- Liver diseases with a violation of its neutralizing function (hepatitis, cirrhosis, acute liver dystrophy, tumors, hepatic coma).
- poisoning with hepatotoxic poisons (alcohol, organophosphorus substances, arsenic).
- Kidney diseases, accompanied by an increase in protein excretion in the urine and a decrease in its content in the blood (nephrotic syndrome).
- Endocrine diseases (acromegaly, increased production of antidiuretic hormone).
- Congenital enzymopathies.
Clinical manifestations of a decrease in urea concentration, as a rule, depend on the underlying disease. If this is due to a decrease in the intake, digestion or absorption of protein, then signs of protein starvation come to the fore.
Diseases of the stomach and intestines are manifested by a characteristic pain syndrome, dyspepsia. Patients may experience nausea, a feeling of fullness in the stomach, belching, unstable stools, and an aversion to meat foods.
Liver lesions are accompanied by bursting pain in the right hypochondrium, enlarged liver, bitterness in the mouth, vomiting bile, yellowness of the skin and mucous membranes, and unstable stools may be noted.
As a result of a decrease in the neutralizing ability of the liver, the ammonia content in the blood increases. Due to its toxic effect on brain cells, hepatic coma may develop.
With acromegaly, there is a disproportionate increase in some parts of the body: the upper or lower jaw, limbs.
Congenital enzymopathies, almost from the first days of a child’s life, lead to an increase in the blood level of ammonia and intermediate products of nitrogen metabolism - citrulline, argininosuccinate, arginine. They appear in the urine, while the concentration of urea in the urine is reduced.
The severity of hyperammonemia is directly dependent on the decrease in the active activity of enzymes. In severe cases, the outcome can be fatal. In milder cases, due to toxic damage to the brain, the child lags behind in intellectual development, and frequent and prolonged headaches are noted.
Congenital pathology is diagnosed by the presence of ammonia and intermediate products of its metabolism in the blood and urine against the background of a decrease in urea. A decrease in enzyme activity in the liver is also detected.
If low urea is associated with a dietary feature, it is adjusted. If a decrease in urea concentration is a manifestation of the disease, then after a set of laboratory and diagnostic tests, adequate therapy is prescribed.
In case of congenital enzymopathies, protein intake is limited as much as possible. This reduces the amount of damage to brain cells.
Urea (Urea) blood test decoding: norm and deviation
Urea (Urea) is the final product after the breakdown of proteins.
It is excreted from the body through the kidneys, that is, this is the only organ that is responsible for the complete removal of urea from the body. All the rest of its accumulation already indicates the presence of significant problems with the body that need to be treated. Accordingly, for such control in medicine, there is a certain biochemical blood test that shows the final content of urea at a given moment.
This way you can judge the healthy functioning of the kidneys and their basic functions.
Urea is part of the residual nitrogen in the blood. These are special substances that accordingly contain nitrogen, but according to their characteristics do not contain proteins.
In addition to all this, the properties of residual nitrogen include creatine, creatinine, uric acid, ammonia and more.
Most often, an increase in urea indicates the presence of chronic diseases or the occurrence of an inflammatory process in the body.
If there is no normal level of urea in the blood, as shown by biochemical analysis, then it is necessary to immediately check the condition of the kidneys. Perhaps it was their difficult work that caused problems in the results of the study. It is worth noting that urea still differs in its characteristics from uric acid, so you should not confuse these two substances after receiving a biochemical blood test.
A biochemical blood test shows whether urea is normal or not. To carry it out, venous blood is taken, since it is most saturated with all the substances necessary for the study.
In order to get reliable results, it is recommended to take the test in the morning on an empty stomach.
It is at this moment that there are no additional disturbances or irritants in the body and, accordingly, in the blood that act to increase or decrease urea.
The standard of care differs only by age category. For example, in adults the urea rate should be from 2.5 to 6.4 mmol/l. In children under 14 years of age, this rate ranges from 1.8 to 6.4 mmol/l.
For elderly people over 60 years of age, the urea rate should not exceed the limits from 2.9 to 7.5 mmol/l. All subsequent deviations from the norm should not be ignored.
It is better to show the test results to a doctor and consult in order to identify the cause in time.
Taking a biochemical blood test and finding out what urea is is very little to make a correct diagnosis. The fact is that increased urea is not always a sign of disease.
For example, an insignificant increase may occur in people who often consume predominantly protein foods. Also, such results occur in those who actively engage in heavy physical activity.
This happens especially in men.
As for diseases themselves, elevated urea may be a sign of certain diseases. Quite often, the cause of deviations from the norm can be poor-quality nutrition, excessive intake of alcohol and smoking, which has a particularly detrimental effect on the functioning of the liver and kidneys.
Possible diseases
Interpretation of the study results will indicate the presence of kidney disease, which in turn has disturbances in excretory function.
This is chronic and acute glomerulonephritis or renal amyloidosis.
In this case, symptoms such as increased frequency or, conversely, decreased urination, the presence of blood in the urine, increased blood pressure, increased fatigue and weakness are observed.
A biochemical blood test will show a significant increase in creatinine, urea and all other components of residual nitrogen.
There may also be diseases such as heart failure, bleeding or burns that occur as a result of impaired blood access to the kidneys. In this case, the blood is not sufficiently purified by the kidneys and this is what leads to an increase in urea.
Thus, deciphering the results suggests that it is also necessary to pay attention to the functioning of the kidneys.
Doctors' interpretations may indicate diseases that arise as a result of increased protein breakdown. These are long-term chronic diseases, problems of the endocrine system and malignant tumors.
A biochemical blood test can show not only an increase in urea, but also a significant decrease. This may be the result of the presence of certain diseases and disorders of the kidneys.
In this case, the rate will also depend on the reasons for the decline and its results. Thus, the transcript indicates the presence of viral hepatitis, cirrhosis of the liver and tumor, as well as other manifestations.
Since the liver is the main organ for the formation of urea, the level of its content in this organ depends on the work of the excretory organ. Thus, all complications of functioning affect the overall health of the body. A biochemical analysis will immediately show a significant decrease in urea, and a doctor’s interpretation will provide an answer to its causes.
It is worth noting that in this case, biochemical analysis may show an increase in AST and ALT. Diseases of the digestive system can also cause low urea. Not only the decoding may indicate this, but also the presence of possible symptoms. For example, a sharp decrease in body weight, muscle weakness and increased fatigue, severe swelling and others.
If the study shows the presence of some abnormalities and the urea level is absent, then treatment measures must be taken. To do this, you should immediately consult a doctor.
Once the cause of the increase or decrease in indicators is identified, the doctor will prescribe appropriate treatment. In this case, all action will be aimed at “removing” the cause of the increase or decrease in urea, and then at restoring it.
To achieve this, a variety of control methods are used, including taking various medications, droppers, and more.
If we are talking about cancer, then appropriate therapy will be prescribed.
It all depends on what exactly caused the change in the indicator, because everyone can have completely different reasons, in that case, the absence of a serious illness.
Perhaps it’s just poor nutrition or physical overload, which the body cannot cope with in a timely manner. Therefore, no matter what the result of the analysis is, you should not engage in self-diagnosis and self-medication.
Source: https://krasnayakrov.ru/analizy-krovi/mochevina.html
Increased level
Urea in a biochemical blood test may be elevated. A number of factors contribute to this.
Reasons for high rates in adults and children:
- An increase in protein-rich foods in the diet (meat, legumes, protein nutrition for athletes).
- Taking certain medications (antibiotics, sulfa drugs, corticosteroids).
- Heavy physical activity.
Possible diseases:
- Kidney failure.
- Reduced urine flow as a result of obstruction of the urinary tract by a stone or tumor.
- Acute or chronic inflammation of the kidneys (glomerulonephritis, pyelonephritis).
- Cardiovascular pathology, accompanied by impaired blood supply to the kidneys.
- Diseases accompanied by dehydration (infections with uncontrollable vomiting, diarrhea, high fever).
- Diseases accompanied by an increase in the breakdown of tissue proteins:
- hematological (leukemia with high leukocytosis, hemolytic and megaloblastic anemia);
- endocrine (hyperthyroidism, diabetes mellitus with ketoacidosis);
- intestinal diseases with tissue necrosis (peritonitis, thrombosis, obstruction);
- destructive diseases and damage to the skin and soft tissues (extensive phlegmon, gangrene, burns, frostbite, prolonged compression syndrome);
- gastrointestinal bleeding;
- malignant tumors with decay.
An increase in urea concentration (uremia), as a rule, is a manifestation of the above diseases. In practice, most often it is kidney damage. Patients complain of pain in the lumbar region, weakness, dizziness, headache, nausea, vomiting, decreased amount of urine (oliguria) up to its complete absence (anuria).
Polyuria (increased amount of urine produced), frequent and painful urination may occur. Upon examination, swelling of the eyelids and hands, pasty face, and increased blood pressure are detected.
In case of heart failure, shortness of breath, cyanosis and swelling of the legs, heart rhythm disturbances, and pain in the heart area are noted.
An increase in urea content is a sign of diabetic nephropathy. The patient should urgently contact an endocrinologist in order to correct treatment.
If urea increases as a result of errors in the diet, you need to reduce the amount of meat products in the diet, eat more vegetables, fruits, cereals, and juices. Rosehip decoction and fruit teas give good results.
If an increase in urea levels is associated with a disease, treatment is prescribed exclusively by a doctor. Self-medication is unacceptable under any circumstances. Therapy is aimed at curing the underlying disease, restoring kidney function, reducing intoxication and removing nitrogen compounds from the body.
Sorbents (Polysorb, Atoxil, Enterosgel, Silix) are used to bind and remove nitrogenous components. In severe cases, hemodialysis (artificial kidney) is the option of choice. In the absence of qualified treatment, the development of uremic coma and death may occur.
Why is urea called that?
Urea received this name because its discovery is directly related to urine. In 1773, the French chemist Hilaire Marin Ruel isolated it from a liquid human waste product.
However, in 1828, the German chemist and physician Friedrich Wöhler obtained a substance similar to urea by evaporating ammonium cyanate (NH4 CNO) dissolved in water. It is from this event that the history of organic chemistry begins, since for the first time an organic compound was obtained synthetically. It is urea obtained in this way that is used today in a variety of sectors of the economy.
Factors of influence
- When the diet contains a large amount of protein (meat, fish and seafood, milk and dairy products, legumes), the level of urea in the blood increases slightly. When plant foods predominate (vegetables, fruits, grains), it decreases.
- Excessive fluid intake is accompanied by a decrease in the concentration of substances dissolved in the blood, including urea. With a small intake of fluid into the body, some thickening of the blood occurs, and therefore a slight increase in urea.
- Obesity does not affect urea levels. However, it may be a manifestation of metabolic pathology (for example, diabetes mellitus, metabolic syndrome) and be accompanied by impaired protein metabolism and renal function.
Urea/Urea Nitrogen
Urea, BUN (Blood Urea Nitrogen) Test
Urea is formed during the breakdown of proteins in the body. It is produced in the liver through a series of biochemical reactions that break down ammonia. Water-soluble and low-toxic, urea easily passes through cell membranes and is the end product of toxic ammonia.
The conversion of urea from amino acids (ornithine cycle) occurs only in liver cells (hepatocytes) using a significant amount of energy. It consists of sequential deamination and transamination of amino acids, which releases urea molecules.
In addition to arginine, ornithine, glutamine and aspartic acid, more than 20 types of amino acids can take part in the cycle. Their source is tissue proteins of the own muscle tissue, as well as food proteins that come externally with food. Approximately 200-300 g of endogenous proteins are used, 100-120 g of exogenous proteins.
Thus, with normal muscle tissue and sufficient protein intake, there is no disturbance in urea synthesis.
Decipher “General blood test” Decipher “General urine test”
Urea is 90% of all nitrogenous metabolites that the body eliminates. Most of it is excreted by the kidneys using glomerular filtration. But approximately 40-60% is reabsorbed into the systemic circulation and circulates in the blood until the next excretion.
In an adult, an average of about 30 g of urea (from 12 to 36 g) is excreted in urine per day, and the total amount of nitrogen excreted ranges from 10 to 18 g. In this regard, the level of urea in the blood is an indicator of the normal functioning of the hepatobiliary system ( liver, gallbladder and bile ducts), urinary system, as well as protein metabolism.
It is to assess the function of these systems that it is advisable to donate venous blood, including in combination with other indicators of liver and kidney tests.
Blood urea measurement
All over the world, essentially the same method of measuring urea levels in the blood is used, but the result can be expressed in two completely different ways.
In the United States and some other countries, blood urea concentration is expressed as the amount of urea nitrogen. This test is called blood urea nitrogen (BUN), and the unit of measurement is milligrams per deciliter (mg/dL).
In all other parts of the world, urea is expressed as the whole molecule (not just the nitrogen part of the molecule) in the international SI units of millimoles per liter (mmol/L).
Since urea nitrogen only reflects the nitrogen content of urea (molecular weight 28) and the urea measurement reflects the entire molecule (molecular weight 60), then urea is approximately 2 times larger than urea nitrogen (60/28 = 2.14). Thus, 10 mg/dL urea nitrogen is equivalent to 21.4 mg/dL urea.
To convert urea nitrogen (mg/dL) to urea (mmol/l), the urea nitrogen value must be multiplied by 10 to convert deciliters to liters, and divided by 28 to convert milligrams to millimoles, that is, 10/28 = 0.357 . Therefore, the conversion factor is 0.357.
Blood urea nitrogen (BUN) in mg/dL * 0.357 = urea in mmol/L.
Urea (mmol/L) / 0.357 = urea nitrogen (mg/dL).
Blood urea levels
Urea norms range from 2.4-8.3 mmol/l (urea nitrogen norms - 4.8-23.4 mg/dl). There are banal reasons for increasing the level of the indicator - this is the consumption of proteins in large quantities. Conversely, if a person adheres to a low-protein diet, then urea may be reduced. More often observed in vegetarians.
Increased blood urea
An increase in urea in the blood is called hyperazotemia or uremia.
When the glomeruli and tubules of the kidneys, that is, the renal filter, are damaged, the pressure in the renal vessels sharply decreases, the processes of filtration and excretion of metabolic products are disrupted.
This leads to an increase in urea in the blood serum in acute or chronic pyelonephritis, glomerulonephritis, amyloidosis with renal failure of varying severity. Diabetes mellitus often occurs with kidney damage, which leads to impaired excretory function.
The concentration of urea increases with dehydration, congestive heart failure, shock, and bleeding. An increase is also observed with increased protein breakdown during burns and cancer, fevers, and heavy power loads.
Reduced blood urea levels
A decrease in urea levels is associated with liver diseases, when hepatocytes are affected and the energy for the synthesis of nitrogenous metabolites is reduced.
These are, first of all, cirrhosis, hepatitis of various etiologies, occurring with liver failure.
Also, urea may be slightly reduced due to hormonal changes (acromegaly, diabetes insipidus), impaired absorption processes in the intestine, and rare hereditary genetic pathologies (hyperammonemia).
A physiological decrease in urea includes flooding of the body, since the volume of circulating blood increases, and not the concentration of the metabolite itself. Ascorbic acid and anabolic agents can slightly reduce urea.
In children and pregnant women, urea levels may be reduced. Protein is actively synthesized, but is also quickly consumed as a building material during growth.
Source: https://testresult.org/opisaniye-pokazateley/biohimiya-analiz-krovi/bun
Reactions and methods for determining urea
Several methods have been proposed for determining the concentration of urea in biological fluids:
- Gasometric method. As a result of chemical transformations, urea decomposes into several components, one of which is carbon dioxide. Its volume is used to judge the level of urea in the sample.
- Colorimetric method with diacetyl monooxime. In an acidic environment, when urea reagents are added, a colored substance is formed. The intensity of its color corresponds to the urea content. Optical density is measured on a photometer, and the concentration of urea is determined from it.
- Enzymatic (urease) colorimetric end point method. A substance that triggers a reaction is added to the sample. After a strictly defined time, she is stopped. The content of the resulting colored reaction product is used to judge the concentration of urea in the sample. The higher the urea level, the brighter the color. Optical density is measured using a photometer.
- Enzymatic (urease) kinetic method. An enzyme is added to the sample to catalyze the reaction of urea conversion. The rate of NADH oxidation, determined photometrically, is used to judge the urea in the sample.
When performing a CBC, hematological parameters and cellular composition of the blood are determined. Urea is a biochemical parameter. It is not included in the list of general analysis indicators.
What is the function of urea
Urea is a natural, essential moisturizer that is not only suitable for humans, but is also a natural component of the human body. It is able to draw moisture from the deep layers of the skin and move it closer to the upper layer of the epidermis. As a result, the appearance improves.
The high hygroscopicity of this component is capable of binding water molecules to each other, which prevents the evaporation of moisture from the surface of the epidermis. Urea also exfoliates dead skin cells, which promotes skin regeneration and healing.
View on Instagram
How to take the test correctly
In order for the result of “biochemistry” to be informative, certain rules must be followed. Blood for research is donated in the morning on an empty stomach, no earlier than 8 hours after the last meal with normal water intake.
The day before the analysis, avoid alcohol, heavy physical activity, and visiting a sauna or steam room. It is recommended to avoid smoking, physical and emotional stress 2 hours before. Before donating blood, you cannot undergo physiotherapy, massage, x-rays and ultrasound.
Urea in a biochemical blood test is determined in combination with other indicators during a comprehensive examination for diagnostic purposes or during a preventive examination. This is the most common examination method.
It allows you to judge the basic metabolic processes of protein, carbohydrate, lipid, mineral metabolism, as well as assess the functionality of organs.
If deviations of the obtained research results from normal values are detected, it is necessary to find out its cause.
For this purpose, several more biochemical parameters are determined:
- Residual nitrogen is nitrogen contained in protein breakdown products. 50% of them are urea, 25% are individual amino acids, 5% are creatine and creatinine, 4% are uric acid, the rest are ammonia, indican, peptides. Usually either residual nitrogen or urea is determined, since both indicators indicate the same changes.
- Creatine - enters the body as part of meat foods or is formed endogenously in the liver and kidneys. Its function is energetic. By combining with a phosphoric acid residue, it forms creatine phosphate, which is a source of energy for muscle contractions. It is rarely determined in laboratory practice.
- Creatinine is a derivative of creatine. It is completely filtered by the glomerular apparatus of the nephrons and is absolutely not absorbed in the tubules of the kidneys. This makes it convenient for assessing the filtration capacity of the kidneys. Along with urea, it is an indicator of uremia.
- Total protein is the total amount of serum proteins (albumin and globulins). This indicator is used to judge the state of protein metabolism as a whole.
- Bilirubin is a toxic substance formed from hemoglobin. By binding to the plasma protein albumin, it enters the liver. If the level of albumin in the blood is low, the delivery of bilirubin to hepatocytes is impaired, and it accumulates in the blood and tissues. For example, in newborns with hypoalbuminemia, physiological jaundice is observed, which disappears when albumin synthesis is normalized. Liver cells absorb free (indirect) bilirubin from the blood. Here it binds to glucuronic acid, becoming soluble. This is bound (direct) bilirubin. As part of bile, it is excreted into the intestines. Bilirubin, especially its indirect fraction, is used to judge the functional state of the liver.
If deviations in urea from normal values are detected, before starting treatment with folk remedies, you should consult a doctor. Only after a complete examination will he be able to give appropriate recommendations. Folk remedies are not always harmless.
So, in case of kidney failure, diuretic herbs are contraindicated. Self-medication with decoctions and tinctures of medicinal herbs can be useless at best, and harmful to health at worst.
The study of Urea is necessary in the diagnosis of a number of diseases. Therefore, this indicator is mandatory when conducting a biochemical blood test.
Biochemical veterinary blood test, Dnepropetrovsk, Dnepr
Details
Veterinary biochemical blood test (cats, dogs, other animals) (Blood Clinical Biochemistry, blood biochemistry)
Internal organs in the animal's body actively participate in metabolism. As a result, changes in the level of concentration of substances and their ratios occur in the blood and organs of the body.
A biochemical blood test allows us to judge the quality of the functioning of organs such as the liver, kidneys, pancreas, gall bladder, and so on. Some indicators allow us to judge, for example, heart problems or other functional disorders in the body. In most cases, a clinical (general) blood test is also prescribed, which shows the general health of the animal’s body at the time of the examination.
In modern laboratories, biochemical blood tests are carried out mainly using photocolorimetric methods. However, there are many factors that influence the accuracy of the results obtained, including: the quality of the reagents, the influence of temperature conditions, the correctness of the extinction measurements of blank samples, test tubes, the correct constants, taking into account statistical errors, etc., etc.. Any of these parameters may affect the accuracy of the result, so everything in the laboratory must be arranged in such a way as to provide conditions for conducting research with maximum accuracy.
In the laboratory of the Kotofey veterinary clinic, we use a modern spectrophotometric biochemical analyzer with microprocessor control to analyze the biochemistry of animal blood. This machine provides high measurement accuracy and a high degree of automation. The quality control program makes it possible to check the correctness of test results at any time, and maintaining quality control statistics allows the laboratory assistant to verify the reliability of the measurements. A computer running sophisticated software ensures control of the measurement technology, accurately follows the methods and parameters of tests, temperature conditions, time intervals (which is especially important when kinetic methods are used), makes calculations and takes into account a lot of other subtleties. This approach not only makes the laboratory assistant’s work easier, but also increases the efficiency of his work and minimizes the human factor. All this ultimately ensures high productivity, accuracy and reliability of results.
An important advantage of our laboratory equipment is the fact that a minimum amount of blood is sufficient for analysis. This is very important for diagnosing diseases of small animals, kittens, puppies.
How to pass a biochemical blood test (how to donate blood for biochemistry) to a cat, dog, or other animals?
Before donating blood for biochemical parameters, it is necessary that the animal does not take food for at least 7-8 hours. You can drink water. Eating triggers a number of processes in the body that can change the clinical picture, and if you donate blood for biochemistry during this period, the results of the analysis will not be sufficiently informative.
Most often, we perform a comprehensive, standardized blood chemistry profile. Additional tests for each patient are ordered by the veterinarian as needed.
At the time of writing, the following biochemical blood tests are available in our laboratory (the range will expand):
| № | Index | Description |
| 1 | Albumin | Albumen. It is synthesized mainly in the liver, participates in maintaining colloid osmotic pressure, is a quickly realized protein reserve, and performs a transport function for the transfer of fatty acids, pigments (bilirubin), cations, bile acids, vitamins, hormones, organic dyes, and medicinal substances. |
| 2 | Total Protein | Total protein, the total concentration of proteins found in the blood serum. They perform many functions, such as participating in blood clotting, maintaining a constant blood pH, performing a transport function, and taking part in immune reactions. A decrease in total protein is observed in some diseases of the liver and kidneys, accompanied by increased excretion of protein in the urine. Increased in blood diseases and infectious and inflammatory processes. |
| 3 | GLB | Globulins. Concentration of globulins in blood serum. |
| 4 | A/G | The ratio of albumin and globulins. Albumins and globulins are the main types of proteins present in blood serum. A decrease in the ratio of albumin to globulins indicates increased levels of globulins, decreased albumin synthesis, low levels of albumin in the blood (losses in kidney disease). An increase in the ratio of albumin and globulins indicates hypothyroidism, hypogammaglobulinemia, excess glucocorticoids, etc. |
| 5 | ALT | ALAT, ALT, ALAT, alanine aminotransferase. An enzyme used to assess liver function. An increase in ALT levels mainly indicates a disorder in the functioning of the liver. |
| 6 | AST | ASAT, AST, ASAT, aspartate aminotransferase. The AST enzyme is involved in the metabolism of amino acids, which occurs in all metabolically active cells. AST is present in the tissues of the myocardium, liver, skeletal muscles, kidneys, pancreas, brain, and spleen. The most dramatic changes in AST activity are observed with damage to the heart muscle and liver diseases. |
| 7 | De Ritis | De Ritis coefficient. The ratio of the activities of serum enzymes aspartate aminotransferase and alanine aminotransferase. Clinically indicative only when aspartate aminotransferase and/or alanine aminotransferase deviate beyond normal values. An increase in the De Ritis coefficient indicates cardiac damage, and we can talk about myocardial infarction or another process associated with the destruction of cardiomyocytes. A decrease in the de Ritis coefficient indicates liver damage. |
| 8 | A.L.P. | Alkaline phosphatase, alkaline phosphatase. An enzyme that catalyzes the hydrolysis of orthophosphorus monoesters with the elimination of the phosphate group, exhibiting optimal activity in an alkaline environment. An increase in serum alkaline phosphatase activity is associated mainly with bone diseases (reflects the processes of bone tissue remodeling) and liver pathology associated with bile duct obstruction. |
| 9 | GGT | The gamma-glutamyl transferase, γ-glutamyl transferase (GGT, GGTP, GGT) is a membrane enzyme that catalyzes the transfer of glutamyl groups from glutathione to amino acids or peptides. The main function of GGT is participation in the metabolism of amino acids and the metabolism of inflammatory mediators. GGT determined in serum is mainly hepatic. A large amount of GGT is found in the endocrine organs: kidneys, liver, biliary tract, pancreas. Despite the fact that the highest enzyme activity is in the kidneys, increases in serum GGT concentrations are more common Most often it is caused by liver diseases. An increase in enzyme activity is observed both in primary liver tumors and in malignant neoplasms of other localizations with the presence of metastases to the liver. In this case, there is a gradual increase in the indicator. Also, GGT activity can serve as a marker for pancreatic and prostate cancer, as it can indicate relapse and remission of the pathological process. In bone tissue pathology, the level of GGT, in contrast to alkaline phosphatase, remains normal, as well as in conditions associated with bone growth, pregnancy and renal failure. |
| 10 | GGT/ALT | |
| 11 | GGT/AST | |
| 12 | GGT/ALP | |
| 13 | Bilirubin total | Total bilirubin. Yellow blood pigment, which is formed as a result of the breakdown of hemoglobin, myoglobin and cytochromes. The main reasons for the increase in the amount of total bilirubin in the blood: damage to liver cells (hepatitis, cirrhosis), increased breakdown of red blood cells (hemolytic anemia), impaired outflow of bile (for example, cholelithiasis). |
| 14 | Bilirubin direct | Direct bilirubin |
| 15 | Bilirubin indirect | Bilirubin indirect |
| 16 | Cholesteroltotal | Cholesterol is the main blood lipid, a steroid characteristic only of animal organisms. It enters the body with food and is synthesized in many tissues of the body, but the main place of synthesis is the liver. |
| 17 | Glucose | Glucose is a common carbohydrate in the animal body. An increase in blood glucose concentration (hyperglycemia) is observed when:
A decrease in blood glucose concentration (hypoglycemia) occurs when:
|
| 18 | a. Amylase | Amylase is an enzyme secreted mainly by the pancreas and salivary glands. Its level in the blood increases when the pancreas is inflamed/damaged. |
| 19 | Creatin kinase | Creatine kinase (creatine phosphokinase) is an enzyme that catalyzes the high-energy compound creatine phosphate from ATP and creatine, which is consumed by the body during increased physical activity. Contained in the cells of the heart muscle, skeletal muscles, brain, thyroid gland, lungs. An increase in the activity of total creatine kinase is observed when any of the above cells are damaged and is therefore not specific. Most often, a significant increase in the activity of this enzyme is observed in acute myocardial infarction within 2-4 hours after an acute painful attack. |
| 20 | Urea | Urea. It is the end product of ammonia neutralization in the body. Urea is excreted by the kidneys, so determining its concentration in the blood gives an idea of the functional abilities of the kidneys and is most widely used for diagnosing renal pathology. Excess urea indicates insufficient excretory function of the kidneys and impaired filtration. |
| 21 | BUN | Urea nitrogen is a blood test that reflects the state of protein metabolism, one of the indicators of impaired renal function. Blood urea nitrogen is considered to be the nitrogen contained in the end products of protein metabolism, and, in particular, urea. This indicator directly depends on the concentration of urea in the blood. Urea nitrogen is indicative in the following cases:
|
| 22 | Creatinine | Creatinine is one of the metabolites of biochemical reactions of amino acid-protein metabolism in the body. The formation of creatinine is associated with metabolic processes in muscle tissue and occurs continuously. Muscles constitute one of the main volumes of the body; their contraction requires a constant energy substrate; powerful energy carriers must be embedded in their structure. This is necessary in order to meet emergency energy needs. The main supplier of ATP for muscle tissue is creatine phosphate - the phosphorylated non-essential amino acid creatine. After synthesis in the liver, it enters the muscles, where it is dephosphorylated by the enzyme creatine phosphokinase. The result of these processes is the formation of energy and creatinine. ATP is used by muscles to meet energy needs. Creatinine is filtered and excreted from the body by the kidneys and urine. If the concentration of creatinine in the blood increases, this is a sign of kidney dysfunction. |
| 23 | Calcium | Calcium (Ca, Calcium) is the most common inorganic element in the animal body. Calcium is essential in a large number of processes, such as:
|
| 24 | Phosphorus | Phosphorus in blood plasma and bones is found mainly in the form of phosphates. The concentration of inorganic phosphorus in the blood depends on the reabsorption of phosphates in the kidney tubules, the ratio of the processes of synthesis and resorption in the bones (where about 85% of the total amount of phosphorus in the body is located). To a lesser extent, from the release of phosphates from the cells of other tissues and the processes of absorption and excretion in the gastrointestinal tract. The main regulators of the balance of phosphorus in the body are parathyroid hormone, calcitonin and vitamin D. For clinical diagnosis, the ratio of calcium and inorganic phosphorus in the blood and determination of the concentration are important of this element in urine. |
| 25 | Ca/P | Determining the ratio of calcium and phosphorus in the blood of animals is of great clinical importance and makes it possible to diagnose a number of abnormalities in the calcium-phosphorus metabolic processes of the body. |
| 26 | Mg | Magnesium. It is a calcium antagonist. Its deficiency is accompanied by the accumulation of calcium in the blood serum. High concentrations of magnesium in the serum lead to the replacement of calcium with magnesium in the bones, a delay in the conduction of impulses in the conduction system of the heart, blockade of neuromuscular transmission, loss of tactility, sensitivity to pain, and temperature. Low levels of magnesium cause muscle tremors, cramps, and delirium. Magnesium deficiency manifests itself primarily at the cellular level, so magnesium deficiency can also occur with normomagnesemia. A blood test for magnesium allows you to determine the concentration of magnesium in the blood serum, which is used in the diagnosis and treatment of hypomagnesemia (low magnesium concentration) and hypermagnesemia (high magnesium concentration ). The most well-known manifestations of magnesium deficiency are deterioration of neuromuscular function, such as hyperirritability, tetany, convulsions and changes in the electrocardiogram. Hypomagnesemia is observed in diabetes, chronic alcoholism, forced diuresis, hyperthyroidism, hypoparathyroidism, hypocalcemia, malabsorption and acute pancreatitis. Elevated magnesium levels in the magnesium blood test are observed in renal impairment, dehydration, severe diabetic acidosis, and Addison's disease. |
In Europe and America, special profiles of tests for biochemical blood parameters have been developed. This is convenient when a doctor suspects a particular pathology in his patient. In this case, only those studies that are necessary are done. Some clinics and laboratories may have their own characteristics and the list of tests may differ. Approximate common profiles of biochemical studies are displayed in the table.
| № | Profile | Description of tests |
| 1 | General | ALB, ALP, ALT, CREA, GLU, TP, UREA, BUN |
| 2 | General/Geriatric(general/age) | ALB, ALP, ALT, AMYL, Ca2+, CHOL, CREA, GLU, PHOS, TBIL, TP, UREA, BUN |
| 3 | Pre-surgery | ALB, ALP, ALT, CREA, GLU, PHOS, TBIL, TP, UREA, BUN |
| 4 | Gastrointestinal (gastrointestinal) | ALB, CREA, Nh4, TP, UREA, BUN, Na+K+Cl- |
| 5 | Cardiac (cardiological) | ALB, ALT, AST, CHOL, CK, CREA, GLU, LDH, TP, UREA, BUN, Na+K+Cl- |
| 6 | Endocrine (endocrine) | ALP, ALT, AMYL, Ca2+, CHOL, CREA, GLU, LIPA, PHOS, TRIG, UREA, BUN, Na+K+Cl- |
| 7 | Hepatic (liver) | ALB, ALP, ALT, GGT, Nh4, TBIL, TP |
| 8 | Lipid | ALB, CHOL, GLU, TP, TRIG |
| 9 | Pancreatic | ALP, ALT, AMYL, Ca2+, CHOL, GGT, GLU, LIPA, PHOS, TRIG, UREA, BUN |
| 10 | Renal (renal) | ALB, Ca2+, CREA, PHOS, TP, UREA, BUN, Na+K+Cl- |
You can take a biochemical blood test of a cat or dog to a laboratory in the city of Dnepr (Dnepropetrovsk) at the Kotofey veterinary clinic.
kotofey.dp.ua