What is urea and its functions in the body
Urea is a biochemical substance that is formed at the final stage of protein breakdown. The reasons for the increase in its concentration in the blood serum is a decrease in the filtration function of the kidneys. The higher the concentration of residual urea compounds, the more serious the disease of the excretory system.
An excessive level of the product of the final stage of protein breakdown indicates a critical condition of the kidneys and the initial stage of failure in their work. In a person who does not have problems with protein metabolism, urea is removed along with urine, entering the bloodstream in small quantities.
Urea formula
It is necessary to distinguish between urea and the component of urine - uric acid, since the mechanism of their formation is associated with completely different metabolic processes.
Uric acid is synthesized after the breakdown of high-molecular nucleic acid compounds, and the nitrogen-containing substance urea is the result of the entire protein metabolism as a whole. This substance does not provide any benefit to the body and must be eliminated from the blood serum as soon as possible.
Reasons for high and low values
High or low levels of urea are a serious reason to consult a doctor, since a significant increase or decrease in the enzyme is dangerous to health and life. This is a huge burden on the kidneys , which cannot always cope with their function.
The final cause of pathological conditions can only be determined by a doctor, and the only diagnostic sign is a significant increase in urea . The patient most often experiences alarming symptoms in the form of poor health, dehydration, headaches, dizziness, urination problems, pain in the lumbar region, and problems with blood pressure.
Often, examination reveals elevated values of urea, creatinine, and uric acid , which already indicates renal pathology. The urea/creatinine ratio allows you to find out whether the patient has renal failure. High rates are most often found in the following conditions:
- Various kidney diseases (renal failure, pyelonephritis, nephritis), accompanied by a violation of their functions;
- Intestinal obstruction;
- Heavy bleeding;
- Shock conditions;
- Neoplasms of the genitourinary organs;
- Stones in the kidneys, ureters;
- Use of drugs that have a toxic effect on the kidneys;
- Dehydration;
- Heart diseases;
- Taking hormonal drugs.
reasons for increasing/decreasing urea . The goal of medical practice is to ask the patient in detail about the existing symptoms. If renal symptoms , then the main cause of the disease lies in nephrotic diseases. The doctor subsequently prescribes an ultrasound examination, MRI, CT scan of the urinary system, and the patient also needs to undergo a general analysis and urine culture for sensitivity to antibiotics.
All indicators of blood biochemistry, as a rule, are assessed together, since in case of kidney diseases, all enzymes responsible for their work increase significantly or moderately. Low values are considered less life-threatening, but they usually occur with a low-calorie vegetarian diet or the cause is liver pathologies (cirrhosis), which is where urea is formed. With concomitant liver diseases, its synthesis is disrupted .
How and under what conditions is urea produced?
Urea in the blood is increased (the causes of the alarming symptom may be interconnected with a person’s lifestyle) only in cases where there is a daily consumption of food rich in proteins, but at the same time there is a decreased performance of the kidneys.
The process of producing a biochemical compound occurs as follows:
- Food products containing proteins of plant or animal origin enter the digestive tract.
- Under the influence of enzymes and gastric juice, food nutrients are broken down and absorbed.
- In the liver tissue, the stage of protein metabolism is completed, as a result of which nitrogen-containing products are converted into urea.
- The biochemical substance enters the bloodstream and then passes the filtration barrier of the kidneys.
- The organs of the excretory system, which fully perform their functions, remove urea from the body along with urine.
Urea contains at least 46% nitrogen. People who do not consume animal proteins for a long time, or who deliberately limit themselves to eating foods containing large amounts of protein, have low urea levels. Moreover, this result is characteristic of both the composition of blood serum and urine.
Diet
Elevated urea in the blood can be normalized after nutritional correction: animal proteins that promote the active formation of urea are excluded from the diet.
In order to lower the level of urea, a therapeutic diet of table 7 is used, which is gentle on the organs of the excretory system.
The basic principles of a therapeutic diet to reduce urea levels are as follows:
- eat 4-5 times a day in small portions to avoid stress on the liver and kidneys;
- drink plenty of fluids (1.5-2 liters per day);
- completely eliminate protein of animal origin (meat, sausages, by-products and dishes made from them, canned meat and fish, smoked meats, meat and fish broths);
- exclude chocolate and cocoa, strong tea and coffee, baked goods, alcoholic drinks;
- limit the consumption of fermented milk products (low-fat cheese, cottage cheese, sour cream, yogurt) and eggs (up to 2 per week);
- You can consume vegetable oil, butter and biscuits on a limited basis.
The diet should consist of complex carbohydrates, the digestion of which does not release ammonia and does not produce increased urea, namely:
- cereals (buckwheat, oatmeal, rice, wheat, etc.);
- fresh and thermally processed vegetables (carrots, onions, zucchini, cabbage, potatoes);
- fruits and berries, nuts, dried fruits.
Normal blood urea table
In the bloodstream of children, adult men and women of young and mature age, as well as elderly people, a small concentration of breakdown products of nitrogen-containing substances is allowed. The table below shows urea standards that are considered optimal and do not pose a threat to human health and life.
| Age | Normal indicators for men and women (unit of measurement – mmol per 1 liter of blood serum |
| Baby 7 days after birth | From 1.1 to 8.9 |
| Children aged from 7 days to 1 year | From 1.4 to 6.8 |
| Child from 1 year to 18 years | From 1.8 to 6.4 |
| From 18 to 60 years old | From 2.1 to 7.1 |
| From 60 to 90 years | From 2.9 to 8.2 |
| Elderly people over 90 years old | From 3.6 to 11.1 |
Any deviation from the optimal indicators, which are displayed in the table above, indicates a chronic or acute phase of the development of kidney, liver, genitourinary or digestive system disease. Further establishment of the cause of the painful condition requires a comprehensive diagnosis.
Exceeded performance
An increase in urea concentration may have nothing to do with kidney or liver pathologies, or with increased consumption of protein foods. Because there are a number of reasons that do not indicate the presence of the disease. For example, this is stress, intense physical activity, taking medications (steroids, anabolic steroids, androgens, salicylates, etc.). But the key reason for exceeding the indicators is problems with the kidneys, namely, violations of their excretory function:
- glomerulonephritis;
- acute renal failure;
- pyelonephritis;
- insufficient blood supply to the kidneys due to cardiovascular pathologies, dehydration, shock;
- blockage of the urinary ducts (tumors, stones, sand).
An increase in urea concentration is possible due to the presence of serious diseases that increase protein synthesis. These are: hematological diseases, infectious, oncological and intestinal diseases.
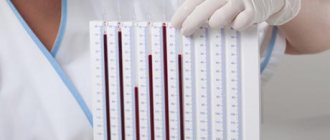
To make a correct diagnosis, the patient submits not only blood for analysis, but also urine, in which the urea content is also determined. To correctly diagnose the disease, indicators such as levels of glucose, lymphocytes and red blood cells are taken into account.
Symptoms of elevated blood urea levels
Urea in the blood is increased (the reasons for its excessive formation may be associated with the development of an acute form of renal failure) in people who have severe diseases of the genitourinary and excretory systems. The first signs of a high concentration of urea are a rapid deterioration in the patient’s general well-being, as well as an increase in the intoxicating effect.
The following symptoms appear:
- sharp jumps in blood pressure towards its increase, although the person has not previously suffered from cardiovascular diseases;
- frequent urge to urinate, but at the same time the release of completely transparent urine without the characteristic shade of wheat straw (after this, the outflow of urine rapidly decreases, and its portions become scarcer each time);
- the appearance of edema, which is localized in the tissues of the lower extremities, around the eyes, fingers and palms of the hands;
- an increase in the level of creatinine in the blood serum (this substance is also the result of complex protein metabolism, so the simultaneous increase in urea levels coincides with an increase in creatinine);
- lack of appetite, aversion to food;
- decreased ability to work, physical weakness, dizziness;
- attacks of severe headache, the appearance of which is associated with severe intoxication of the body;
- excess in the blood serum of other toxic compounds that accumulate together with urea during the breakdown of nitrogen-containing products - ammonia, peptides, microglobulin, cyanate, phenolic substances (are carcinogens), acetone, oxalic acid;
- vomiting;
- stool disorder, which is expressed in the form of liquid diarrhea;
- the development of hyperkalemia, which entails heart rhythm disturbances.
Signs of a critically high level of urea in the blood serum can be detected independently.
For example, in addition to the above symptoms, it is necessary to pay special attention to the surface of the skin. People who have urea in their blood have epithelial tissues covered with nitrogen frost. These are small crystals of mineral salts that were not excreted by the kidneys along with urine.
Symptoms
A high concentration of urea in the blood is most often manifested by symptoms from the excretory system, namely:
- severe pain in the lower back;
- acute pain in the lower abdomen;
- rare or frequent urination;
- blood in the urine and pain when urinating;
- presence of edema;
- increased blood pressure;
- weakness and fatigue.
Causes of increased urea in the blood
Urea in the blood is elevated (the causes of the pathological symptom in 85% of cases are associated with the presence of a current disease) in people who suffer from concomitant diseases of the kidneys or other organs of the excretory system.
Frequent stress is a possible cause of high urea levels in the blood
The following reasons for the increase in urea concentration in the bloodstream are identified:
- a side effect of prolonged use of medications such as Lasix, corticosteroids, cephalosporin antibiotics, Tetracycline, Eutirox, steroid hormones, androgen-based sports nutrition;
- eating large amounts of protein foods of animal or plant origin;
- long-term fasting, when due to a systematic deficiency of proteins, as well as other nutrients, protein metabolism is disrupted and the performance of the heart, kidneys and liver decreases;
- intense physical activity, labor associated with daily movement of heavy objects;
- frequent stress, nervous strain, psycho-emotional breakdowns of various etiologies;
- renal failure, which is in the acute phase of development (at the initial stage of the disease there is a sharp surge in the concentration of urea, and then creatinine, the levels of which reach 10 mmol per 1 liter of serum and blood);
- prostate cancer;
- blockage of the urinary tract of the kidneys by stones or tumors that make the natural outflow of urine impossible;
- inflammatory kidney diseases – glomerulonephritis, as well as pyelonephritis;
- complication of existing heart failure or sudden myocardial infarction;
- pernicious anemia;
- thrombosis of the main vessels feeding the kidney tissue, which ultimately led to disruption of their blood supply;
- prolonged thirst and failure to receive into the body a sufficient volume of fluid necessary for the functioning of the excretory system and the removal of metabolic products along with urine;
- renal failure, which has become chronic;
- hemolytic type jaundice;
- thermal or chemical bodies covering more than 10% of the skin;
- severe infections that affect the gastrointestinal tract - cholera, bacterial dysentery, typhoid fever;
- obstruction of food through the intestines, the appearance of blood clots in the veins of this organ (in this case, the filtration function of the kidneys remains normal, but the accumulation of nitrogen-containing substances in the blood serum is due to a violation of protein metabolism).
Timely detection of the cause that provoked an increase in the level of urea in the bloodstream is considered a prerequisite for successful treatment and restoration of the functionality of the entire body. Without treatment of the underlying disease, it is impossible to achieve stable remission and complete cleansing of blood serum from mineral impurities.
Causes of the disease
Elevated urea in the blood is detected in a wide range of different abnormalities. Their number is so large that sometimes even specialists are not able to determine at first what causes the increase in carbonic acid diamide. Uremia is a consequence of both pathologies that require immediate treatment, and multiple biochemical processes that do not pose any danger to human health.
Diseases
So, the most common pathological causes of increased urea in the blood are as follows:
What is uric acid responsible for in the blood?
- renal failure (chronic and acute);
- thyrotoxicosis (excess of hormone synthesized by the thyroid gland);
- stomach ulcer;
- nephritis (kidney inflammation);
- diabetes;
- thrombosis;
- pneumonia of viral origin;
- BPH;
- intestinal obstruction;
- myocardial infarction;
- typhoid fever;
- rubella;
- nephroblastoma (malignant tumor of the renal parenchyma);
- heart failure;
- peritonitis;
- measles;
- dysentery;
- severe dehydration;
- calculi (stones) in the bladder and kidneys;
- abscess;
- thrush;
- cardiac ischemia;
- glomerulonephritis (inflammation of the kidney glomeruli - glomeruli);
- myositis (damage to muscle fibers);
- polycystic kidney disease;
- meningitis;
- cholera;
- sepsis;
- angina.
Receiving 3-4 degree burns forces the body to intensify the process of protein breakdown, as a result of which the urea indicator increases significantly.
Diseases associated with the hematopoietic and circulatory systems can increase urea levels: pernicious anemia, leukemia, leukemia, etc. In people suffering from cirrhosis, hepatosis (fatty liver), hepatitis or hepatic tuberculosis, it will most likely also appear in the biochemical analysis. high urea content.
Another cause of uremia in some cases is hemorrhagic fever. We are talking about an extremely dangerous anomaly, which is expressed by the manifestation of severe symptoms: chills, increased body temperature, convulsions, heavy bleeding, swelling, paralysis, hardening of muscles.
Patients experience paresthesia (impaired sensitivity of the mucous membrane and skin), dyspepsia (stomach dysfunction), the formation of extensive hematomas and destruction of vascular walls. If this disease is not treated, then all internal organs will soon begin to fail, which will lead to death. If you identify the above symptoms, you should consult a specialist as soon as possible.
Poisoning with toxic substances can provoke an increase in urea: phenol, trichloromethane, arsenic, ethylene glycol, lead and sublimate (mercuric chloride)
And it also increases the level of urea in the blood. Leptospirosis is an infectious disease characterized by the negative impact of pathogenic worm-like bacteria on the cells of the kidneys, liver, skin, blood vessels, stomach, heart, muscles, brain and spinal cord. This disease is accompanied by muscle pain, hyperpigmentation, skin rash, red eyes, sleep disturbance and difficulty breathing. Bleeding occurs (uterine, intestinal, nasal).
Such a deviation must be treated immediately to avoid severe complications or even death (for example, from pulmonary edema). Not so often, high levels of urea are observed in young children due to impaired synthesis of enzymes that are responsible for protein metabolism.
As a rule, such diseases develop as a result of a malfunction in the genetic program of babies at the stage of their formation in the womb. Information on various methods for reducing urea is contained in this article.
Non-pathological causes
Excess urea indicated in the results of biochemical analysis is in many cases explained by dietary habits. The indicator increases with a significant predominance of protein foods in the diet: seafood, fish, fermented milk and dairy products, meat. If the patient ate a large portion of protein-rich food the day before donating blood, the carbamide content will be high, but completely harmless.
To obtain more objective information about the state of your health, it is better to limit the consumption of such products at least a day before diagnosis. Any diet that excludes sodium chloride (table salt) also causes uremia. Regular sports or dancing, as well as prolonged stress, lead to accelerated breakdown of proteins in the body.
Excess urea is observed during the use of such drugs:
- androgens (male sex hormones of steroid origin);
- thyroxine (the main hormone produced by the thyroid gland);
- sulfonamides;
- some aminoglycoside antibiotics;
- aristolochic acid in dietary supplements;
- diuretics (diuretics);
- NSAIDs (non-steroidal drugs that have an anti-inflammatory effect).
If you are using medications that belong to the previously designated groups, you should inform your doctor.
Indications for blood urea testing
Urea in the blood is increased (the reasons for the increase in the concentration of the protein breakdown product are determined by the results of a diagnostic examination of the body) in patients with diseases of the gastrointestinal tract, organs of the excretory system or disorders of protein metabolism.
A study of blood serum for the concentration of urea in it is indicated if the patient has the following complaints:
- frequent urination with discoloration of urine, or cessation of daily diuresis;
- headache, nausea, vomiting;
- arrhythmia, asthma attacks;
- the appearance of salt discharge on the surface of the skin (most often this symptom of high urea levels is localized on the epithelial tissues of the head);
- loss of appetite;
- loose stools without signs of intestinal infection or food poisoning;
- swelling of the legs, soft tissues around the eyes and the entire facial disc as a whole;
- the smell of acetone or urine from the oral cavity (in conditions of a critically high level of urea in the blood, the patient’s skin begins to emit a characteristic odor of ammonia).
The initial appointment and diagnosis of the patient is carried out by a general practitioner, nephrologist, and hematologist. The choice of a specialized specialist depends on the type of disease that caused pathological symptoms and an increase in urea concentration. If the patient has not yet been diagnosed, then first of all it is necessary to seek advice from a general practitioner.
Urea standards
The normal level of urea in the blood of men is in the range of 3.7-8.3 mmol/l. In the female body, the blood contains slightly less carbamide. This is due to less muscle mass and less physical activity. A good indicator is considered to be 2.5-6.7 mmol/l. The levels of urea in the blood of women during pregnancy are even lower due to the acceleration of the processes of protein formation and their elimination.
In children, the level of urea in the blood is normal at 1.9-6.5 mmol/l. For newborns, an increase in this value is considered normal.
With age, the filtration capacity of the kidneys weakens, so a level of 3.2-7.8 mmol/l after sixty years is considered an indicator of a healthy person.
How is urea in the blood determined?
In order to determine the concentration of urea in the blood serum, it is necessary to undergo a preliminary consultation with a general practitioner.
After listening to the patient’s current complaints and determining the symptoms characteristic of high urea levels, the doctor prescribes the following tests and laboratory tests:
- collection of venous blood for biochemical analysis and determination of the concentration of urea, creatinine, residual nitrogen compounds (non-protein), total protein and bilirubin;
- Ultrasound of the kidneys to promptly detect the possible presence of foreign tumors, blockage of ducts and stones that disrupt the stable functioning of the excretory organ;
- submitting urine for biochemical testing for urea and protein levels;
- collection of urine with further analysis using the Nechiporenko method in order to promptly determine the inflammatory process in the tissues of the kidneys and the urinary system as a whole;
- daily diuresis (in this case, urine is collected for 24 hours, and the attending physician analyzes the total volume of urine excreted over a specified period of time);
- Ultrasound of the liver to identify diseases of this organ (cirrhosis, hepatitis, cancer, which affect the breakdown of nitrogen-containing products and the production of urea);
- gastroscopy of the stomach and endoscopic examination of the intestines, if there are concomitant gastrointestinal pathologies that exclude normal digestion and absorption of protein foods.
The main analysis that allows us to establish the real level of urea in the blood serum is a biochemical study of venous blood. Other diagnostic methods are considered auxiliary and are also aimed at identifying the disease that provokes an increase in the concentration of a nitrogenous compound in the blood.
Low urea factors
The level of urea in the body decreases in rare cases as a result of the following reasons:
- Pregnancy (during this period, the level of water in the blood rises, and protein is intensively consumed). In later stages, protein utilization increases;
- Liver dysfunction : viral and bacterial hepatitis, liver cirrhosis, malignant neoplasms, liver failure as a result of poisoning;
- Impaired absorption of protein in the intestine as a result of chronic pancreatitis, helminthic infestations, complications after operations in the intestinal area;
- Vegetarianism, diets;
- Parenteral administration of fluid (bypassing the digestive system) into the body and its excess;
- Hemodialysis (blood purification using a special device without the participation of the kidneys);
If the reason for the decrease in urea levels is diet or vegetarianism, you need to introduce protein into the diet in sufficient quantities.
The level of the indicator in pregnant women normalizes independently after childbirth. In other cases, it is necessary to treat the pathologies that caused its decrease.
Preparing and performing a blood urea test
To obtain the most reliable data on the study of blood serum for urea levels, it is necessary to follow the rules for preparing for the analysis.
The patient is recommended to do the following:
- 3 days before collecting biological material, exclude meat dishes, fried, pickled, smoked, and too fatty foods from the diet;
- 48 hours before the test, do not drink alcohol, do not visit baths and saunas;
- the last meal should take place no later than 8-12 hours before donating venous blood;
- dinner, on the eve of collecting biological material, should be light, consist of cereal porridge, vegetable salad (you cannot overeat);
- if the patient uses tobacco products, the last cigarette should be smoked no later than 1 hour before visiting the laboratory;
- 24 hours before the analysis, you should not engage in sports, expose your body to heavy physical activity, or expose your nervous system to psycho-emotional stress;
- blood from a vein is donated on an empty stomach during the period from 07-00 to 09-00;
- before entering the manipulation room, you need to rest and restore your breathing;
- If you are taking any medications, you should inform your doctor about this, since their active components can affect the breakdown of nitrogen-containing products.
Blood is drawn by a laboratory technician at the site of the analysis. Biological material is taken from the ulnar vein.
For research and obtaining the most accurate results, 2 to 5 ml of blood is enough. In a public hospital, medical services are provided free of charge. In a private clinic, you will have to pay about 850 rubles for a urea test. The average duration of a laboratory test is from 3 to 5 hours.
How is urea concentration tested?
To perform a urea test, blood is taken from a vein. The reliability of the study depends on the correct preparation of the person, which begins 24 hours before the analysis. Biochemical analysis is reliable if you follow these rules:
- blood is taken in the morning on an empty stomach;
- within 12-24 hours before the study, you should not drink or eat sweets;
- Until the analysis is carried out, you are allowed to drink clean water;
- avoid strong physical activity and emotional stress.
Advice! Analysis in children does not require special preparation; blood is taken from the heel or veins of the head.
You can find out the test results within a few hours after sending the blood to the laboratory. After receiving the study data, the doctor evaluates the results, reports deviations, if any, and prescribes additional diagnostic procedures.
There are three options for the analysis conclusion: normal, decreased and increased level. If the indicator is normal, it means that the kidneys are functioning normally and urea is freely excreted from the body. Other indicators require a detailed examination of the kidneys, blood, liver and other systems.
Interpretation of blood urea test results
Interpretation of the results of a biochemical study of blood serum for urea levels is carried out taking into account the indicators that are displayed in the table above. If the concentration of a nitrogen-containing substance deviates from the established norm, one can judge the possible development of the following pathologies.
| Increased performance | Reduced performance |
| Renal failure in acute or chronic form. | Cirrhosis, as well as other liver diseases, leading to total destruction of its tissues and a decrease in synthetic function. |
| Ureteral stricture, prostate enlargement in men, urolithiasis, urinary tract obstruction. | Overhydration, protein malnutrition, or malabsorption |
These diseases, more often than any other disease, cause a sudden increase or decrease in the concentration of a nitrogen-containing substance in the blood. If urea readings deviate from the established norm, immediately upon completion of the laboratory report, it is necessary to undergo an examination for the presence of the above pathologies.
What is urea
In the body of every person, urea is one of the end products of natural protein metabolism. This substance is formed as a result of a very complex cycle of natural processes.
The concentration of urea is directly dependent on the proper functioning of the kidneys and the functioning of the excretory system as a whole.
Proteins, breaking down in the body under the influence of special substances, form ammonia, which is a very toxic substance for the body, causing serious harm. Detoxification of this element occurs in the liver, where, thanks to complex biological and chemical reactions, as a result of the neutralization of ammonia, urea is formed, which does not have toxic properties. The resulting substance is excreted without harm to the body through the kidneys along with urine.
Based on the level of urea, doctors can judge the condition of the patient’s liver and kidneys and how well these organs cope with their function.
At what level of urea in the blood should you consult a doctor?
Any excess of the norm of a nitrogen compound in the blood, or a decrease in its values, should be a motivation to seek advice from a general practitioner or nephrologist.
Specialists of this profile will conduct an initial examination of the patient and will also be able to prescribe a set of tests. Their results will make it possible to establish the true cause of changes in the biochemical composition of the blood and disruption of the process of breakdown of nitrogen-containing products with their further removal outside the body.
Traditional medicine for relief
You can remove urea from the body using traditional medicine recipes. Experts recommend drinking herbal infusions and herbal mixtures from various beneficial plants, including St. John's wort and cornflower flowers, rosehip leaves and black currants, elderberry and juniper. Taking drinks according to the recommendations of traditional medicine should be with the consent of the attending physician and begin with small doses. Based on the medical history, the doctor can select the necessary plants and herbs, check the patient for allergies to the components of herbal preparations, and also recommend the necessary dosage and duration of use.
More on the topic: Reasons for the appearance of uric acid salts in urine
One of the popular recipes is bearberry leaves, two large spoons of which are cooked in a water bath in a glass of water. The mixture is boiled for 15 minutes over low heat, then the sediment is discarded and two large spoons are taken half an hour or an hour before meals.
The effectiveness of licorice root has been proven, which you need two large spoons in dry and crushed form per glass of boiling water. The infusion sits on low heat for 10 minutes at a low boil, sits in a dark place for 8 hours, if brewed in the evening, then until the morning. Recommended dosage is 0.1 liter three times a day.
How to bring the urea level in the blood back to normal
Normalization of the level of this nitrogen-containing substance is carried out through the use of medications, as well as through other methods of artificial blood purification from toxic compounds.
Medications
To reduce the concentration of urea in the blood serum, sorbent drugs are used, which allow the removal of toxins in a short period of time, namely:
- Polysorb is a drug that is taken orally in the form of a suspension of 1 tbsp. l. 3-4 times a day 1 hour before meals, pre-mixed in a glass of still water (course of administration - 10-15 days, and the cost of the medication is 240 rubles);
- Atoxil is a universal remedy for eliminating signs of intoxication and cleansing the body of toxic substances, which is taken 1-2 sachets, pre-dissolved in 200 ml of warm water (therapy is symptomatic as the level of urea increases, the price of the sorbent is 150 rubles per jar) ;
- Enterosgel paste is an absorbent drug that has a jelly-like mass, taken 1 tbsp. l. 3 times a day 1.5-2 hours before meals, or after a similar time, but after a meal (the course of treatment ranges from 7 to 14 days, and the cost of the drug is 230 rubles);
- Silix is a powder for preparing an oral suspension, the daily dosage is 12 g, the sorbent is dissolved in 250 ml of boiled water with a course of therapy of 14 days (the price of the medicine is 190 rubles).
The above drugs are effective in the initial stage of disease of the liver, kidneys or digestive system, which has caused an increase in urea. If the disease has already reached the stage of uremia, or the patient suffers from acute or chronic renal failure, then methods of hardware blood purification in the form of hemodialysis should be used.
Consequences
Lack of drug treatment for elevated urea levels can lead to acute or chronic renal failure. In this case, the urea content can reach 100-200 mmol/liter with a norm of 1.4-8.3 mmol/l.
The development of renal failure leads to an increase in urea and other chemical metabolic products in the blood, since there is no filtration of blood plasma by the kidneys. In this case, associated complications are observed, namely:
- arterial hypertension (persistent increase in blood pressure);
- proteinuria (protein in urine);
- hyperelipidemia (increased levels of lipids in the blood);
- hyperparathyroidism (overactive parathyroid gland);
- problems with blood clotting;
- electrolyte imbalance.
Traditional methods
The increase in the level of nitrogen-containing substances in the blood must be stopped exclusively by medications or other methods of official medicine. Taking decoctions, teas and tinctures prepared on the basis of medicinal herbs will not bring a positive effect, and in some cases may even cause a deterioration in the patient’s well-being.
In addition, the transition of the pathology to the stage of uremia with the further onset of toxic coma cannot be ruled out.
Other methods
A critical increase in the level of urea in the blood serum requires urgent removal of the toxic compound from the body. In this case, sorbent drugs are ineffective, since they are not able to cope with a large volume of nitrogen-containing substances.
Patients with high levels of urea in the blood or signs of uremia are advised to undergo hemodialysis using an artificial kidney machine. The patient is admitted to the inpatient nephrology department or dialysis center. The blood purification procedure is carried out by qualified medical personnel.
The patient is placed in a special chair-couch, and a medical device is connected to his circulatory system, which removes urea and other toxic compounds using a bicarbonate or acetate solution. The hemodialysis procedure itself is performed under completely sterile conditions using disposable consumables.
Patients who have accumulated nitrogen-containing substances due to acute or chronic renal failure are forced to undergo blood dialysis on an ongoing basis from 1 to 3 times a week. In case of temporary dysfunction of the liver and kidneys, which causes an increase in urea concentration, hemodialysis can become a one-time procedure to restore the biochemical composition of the blood.
Factors that caused a change in normal concentration
Why is urea in the blood elevated? Its level depends on 3 factors:
- The amount of amino acids formed after protein metabolism, since ammonia is then produced from them,
- Liver performance (the ornithine cycle is used for urea synthesis),
- Condition of the kidneys (for its excretion).
The causes of increased urea in the blood are conventionally divided into 3 groups:
- Physiological,
- Medicinal,
- Pathological.
Physiological factors include our diet and physical activity. If a person prefers protein foods, and it takes up a large part of his daily menu, then this can cause an excess of urea. The content of this element begins to increase with the consumption of 2.5 grams of protein per 1 kg of weight. Fasting can also cause (NH2)2CO to rise in the blood as large amounts of protein are released from muscle tissue. Physical activity and nervous stress are also factors that lead to the removal of protein from muscles and, as a result, the results of studies on urea will be overestimated.
Deviations in a larger direction can also be caused by medications. The group of medications that give a similar effect include:
- Cephalosporins,
- Anabolics,
- Steroids,
- Corticosteroids,
- Salicylates,
- Androgens,
- tetracycline,
- "Euthirox"
- "Lasix"
- neomycin,
- sulfonamides.
Urea levels may increase when increased protein breakdown and blood changes occur, the reasons for these phenomena are:
- Temperature for 2 weeks,
- Infectious diseases,
- Burns,
- Sepsis,
- Bleeding in the gastrointestinal tract,
- Tumors (leukemia, lymphoma),
- Postoperative period
- Constipation,
- Intoxication with phenol, mercury salts, chloroform,
- Dehydration due to vomiting, diarrhea, or excessive sweating.
But still, the main cause is considered to be kidney dysfunction. Elevated levels of urea in the blood are observed in the following disorders:
- CRF - chronic renal failure. As the urea concentration increases, creatinine also increases. Analyzes show values of more than 10 mmol/l,
- Blockage of the urinary tract by stones or tumors,
- Pyelonephritis,
- Poor blood supply to the kidneys due to heart attack, dehydration, shock.
Possible complications
Excessive concentrations of nitrogen-containing compounds found in the blood must be removed as soon as possible.
The absence of medication or other therapy can lead to the development of the following complications:
- severe form of uremia, which involves the accumulation of urea to critical levels and the onset of coma;
- general intoxication of the body;
- development of heart failure;
- the occurrence of a hypertensive crisis;
- cardiac ischemia;
- hepatitis or cirrhosis of the liver;
- lifelong dependence on an artificial kidney machine with the need to undergo dialysis blood purification at least once a week;
- the onset of death.
The reasons for the increase in urea in the blood serum are established in the first 1-2 days from the moment the patient seeks help from a doctor.
In this case, you can count on emergency measures aimed at reducing the level of nitrogen-containing substances without significantly disrupting metabolic processes in the body. In general, a violation of normal urea levels in the blood serum is a clear symptom of severe diseases of internal organs, or systemic dysfunction of kidney and liver tissues.
What does increased performance mean?
An increased level of urea in the blood is not always an indicator of a pathological condition. This may be the result of increased physical activity, excessive consumption of protein foods, prolonged fasting, lack of water, stress, or taking certain medications (sulfonamides, antibiotics, blood pressure medications, corticosteroids).
A lot of urea in the blood is observed with changes in the glomerular filtration rate caused by inflammation due to bacterial infection (pyelonephritis, glomerulonephritis), replacement of renal connective tissue (nephrosclerosis). Sometimes it indicates the formation of stones or tumors in the urine outflow path.
The reasons for the increase in urea in the blood may lie outside the urinary system:
- diseases of the liver, pancreas, heart;
- hormonal disorders;
- malignant formations of any localization;
- external or internal bleeding.
Treatment methods
Correction methods depend on the specific cause of development. Because there are many factors. It makes no sense to fight the urea level itself, it is useless. You need to influence the source.
If we talk about a number of specific steps towards normalization:
- Liver diseases. Hepatoprotective drugs are used. Like Karsila, Essentiale. In some cases, phytotherapeutic agents are used. Dynamic control is required. Diagnoses of the type of cirrhosis in subcompensation are an indication for transplantation. Dietary adherence is mandatory. Changing your diet is one of the key measures.
- Kidney pathologies. Mainly represented by filtration disorders. In which the amount of urine increases. It is necessary to find out the root cause and eliminate it. If it is central diabetes insipidus, synthetic vasopressin drugs are prescribed. Further depending on the circumstances. Under the supervision of a nephrologist.
- Dehydration. It is necessary to compensate for electrolytic disturbances by drinking enough fluid.
- Postoperative and post-traumatic complications. They go away on their own as soon as the damage is repaired.
- Hormonal imbalance. It is necessary to restore the level of specific substances. When the urea is normal, examine the background and decide on the advisability of further treatment.
- Insufficient protein intake can be corrected by simply changing your diet. The inclusion of animal products. Oils, meat. Eggs.
In any case, a complete cessation of smoking and the preferential exclusion of alcohol from life is necessary.
The issue of treatment is extremely variable. Because there are many reasons for possible deviation.
The level of urea in the blood shows a group of disorders: from the liver, kidneys, etc. You need to understand the etiology and only then act for sure. You won’t be able to do anything on your own without knowing the nature of the phenomenon.
The role of urea in the body
The named compound does not have much independent significance when it comes to the functional activity of the body. But this goes far to show that the substance does not have any capabilities at all.
In fact, there are two main points to talk about:
- Urea has the ability to bind nitrogen compounds. These chemical structures are dangerous and cause oxidation and destruction of body tissues. They act as carcinogens, provoke aging processes and other dangerous aspects.
At high concentrations, such a harmful effect is observed to a particular extent. With a sufficient amount of urea, the body can independently adjust nitrogen levels in the blood and return biochemical processes to normal.
- In addition, the named substance is used by doctors, mainly as a marker of a group of pathological processes. Any deviations carry a lot of information and are quite indicative from a diagnostic point of view.