In absolutely healthy people, the number of eosinophils in the blood is usually insignificant. Data from medical practice accumulated over the years show that there are special diseases in which an increase in eosinophils in an adult is possible, both in the peripheral blood and in various other tissues.
The eosinophil was first designated by Wharton Jones in 1846, but it was not until 1879 that it was described as an individual cellular element (EO). Scientist Ehrlich Paul was the first to use the definition of eosin as an acidic dye, named after the ancient Greek goddess Eos (goddess of the morning lightning). Eosin was used in the staining of histological tissues, as well as blood elements.
What are eosinophils?
The large white blood cells are components of the “granular” subtype of leukocytes called eosinophils. The normal level in the blood is considered to be from 4 to 9 thousand leukocytes per cubic millimeter, and eosinophils among them range from 1 to 5 percent. The main function of eosinophils is regulation and protection against infections.
The following tasks facing this subtype of leukocytes can be identified:
- protecting the human body from bacterial and viral infections;
- participation in antiparasitic immunity and allergic reactions;
- regulation of the unchanged state of the body, its internal environment (tolerance).
Eosinophils are classified as non-dividing granulocytes - these are leukocytes that are a continuously formed product of the bone marrow. The formation time of eosinophils is 72-96 hours. These large immune cells are produced by the bone marrow, and then leave it, rushing into the bloodstream, and circulate through the blood for several hours (up to 12 hours).
Such blood cells are called upon to be responsible for fighting foreign protein in people's bodies.
As soon as allergens and parasitic antigens enter the body, they are neutralized by eosinophils. A decrease in white blood cells is a sign of weak immunity and fatigue of internal organs from fighting the disease.
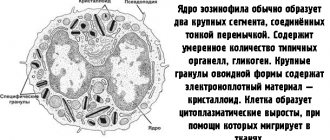
Eosinophil has many receptors:
- to immunoglobulins (IgG, IgE);
- to complement;
- to biologically active substances (histamine).
These large blood cells are capable of chemotaxis and phagocytosis. An eosinophil can act against a mast cell (a type of white blood cell also known as a mast cell or mast cell), reducing the level of histamine it releases.
What to do
Sometimes it is not possible to find out why there is a decrease in eosinophils in the blood. In addition, with a short-term decrease in the level of these bodies, separate therapy is not required.
The goal of treatment is to combat the factor of change in test results:
- When the cause is bacterial infection, the basis of therapy is most often antibacterial drugs. As a supplement, you may be prescribed medications that support the intestinal microflora - probiotics and restrictions on the consumption of fried, fatty, canned and smoked products.
- If a low level of eosinophils is caused by toxic substances, detoxification treatment and symptomatic therapy are prescribed. In case of disruption of the heart and blood vessels, arrhythmia and shock are treated, and tracheal intubation is performed against the background of acute respiratory failure. In case of a critical disorder in the functioning of vital systems, artificial blood circulation or ventilation, hemodialysis can be used.
Important information: The norm of eosinophils in the blood of a child by age (table)
With sustained relief of painful sensations through local action, antispasmodic and analgesic drugs, the level of eosinophilic cells in the blood is normalized.
When the condition stabilizes, remission occurs or the underlying pathology is cured, the indicators in laboratory blood flow tests stabilize. Do not forget that it is strictly forbidden to use medications when there are few eosinophils in the bloodstream, without medical advice.
To prevent the occurrence of conditions that can lead to the eosinophil count being lower than normal, and to strengthen the immunity of the entire body, you need to follow some rules. A person should adhere to a balanced diet, drinking regime, exercise the body moderately, walk outside more often, not get too cold, and be sure to follow a work and rest schedule.
Functions of eosinophils in the body
An increase in eosinophils in an adult is associated with two important tasks of the human body’s immunity:
- Destruction of foreign microparticles, toxic elements, viruses. The main purpose of granular leukocytes is to penetrate focal inflammation, and then initiate cell receptors there that are responsible for activating immunity directed against parasites in the body. Foreign substances are consumed by eosinophils, especially those of a viral nature or helminth infestation. Bacterial particles and various harmful components are “marked” by the immune system as other foreign components for subsequent removal. The cellular composition near the parasites self-destructs, then a membrane capsule is formed. A number of substances called mediators accumulate in eosinophils: phospholipases, endogenous histamine, which are involved in important reactions.
- Regulate the inflammatory process. Under the influence of eosinophil mediators, an inflammatory area appears, designed to isolate and control a foreign microorganism or harmful particle. But it happens that sometimes the source of inflammation grows wider than required, which leads to the formation of damaged tissue and the appearance of painful acute symptoms. Basically, formed elements play a major role in controlling the manifestations of allergies, asthma symptoms, and hay fever. They delay the development of allergic and rheumatic factors and prevent the development of a total disease.
Low eosinophil count
Low eosinophils are also indicators of poor child health. They indicate exhaustion of the body and weakened immunity.
A low eosinophilic index occurs in the following conditions:
- Diseases of the adrenal glands and thyroid gland;
- Acute inflammation;
- Prolonged stress;
- Heavy metal poisoning;
- Severe purulent infection, including blood poisoning;
- Acute pancreatitis;
- Acute appendicitis;
- Long-term use of glucocorticosteroids;
- Leukemia.
Eosinophils are low in children with Down syndrome and premature babies.
If you receive a test result with an eosinophil count of less than 1% or no eosinophils, you should immediately show the child to a pediatrician. It is better to take the test again to rule out a laboratory error. Next, you should look for the cause of this condition.
Normal levels in the blood of an adult
The normal number of cells of the white components of the blood of an adult varies from one to five percent of the total number of leukocytes. An increase in eosinophils in an adult is called eosinophilia. It can be insignificant (up to 10%), moderate (up to 20%), high (over 20%).
In the mature population, a value of 500 eoz/μl is considered normal. in blood. Exceeding the level to 5000 eoz/μl for several months means the development of hypereosinophilic syndrome in the patient.
What values are considered reduced?
Normally, eosinophils in the bloodstream should not exceed 1-5% of the total volume of leukocytes. The level of these bodies can change throughout the day. For example, the eosinophilic index is reduced during the day, and during night rest it increases to its maximum.
According to standards, the number of eosinophils in the blood of an adult and a child over 13 years of age should be 0.5-5%, which in absolute numbers means 0.02-0.03*109/l. While in children this figure is slightly higher - 0.5-7%.
Eosinophils may be absent in adults if eosinopenia has begun to develop, a condition during which the number of cells in the bloodstream decreases.
In the case when the proportion of eosinophils in an adult is 0 in the leukocyte formula, but the level of blood cells themselves remains unchanged, this means that relative eosinopenia is developing.
Important information: What is platelet anisocytosis in a general blood test (result interpretation)
A reduced level of eosinophilic cells in women after fertilization is the norm (sometimes they are completely absent), since leukocytes perceive such an egg as a foreign body and destroy it.
Eosinophils and lymphocytes
Thanks to a general blood test, the presence of the following formed elements can be determined: hemoglobin, red blood cells, reticulocytes, platelets, leukocytes. In addition, there is a division into subtypes of leukocytes with specific functions: basophils, lymphocytes, monocytes, eosinophils.
Leukocytes contain LYMP lymphocytes, which are responsible for the formation of general local immunity, the norm of which ranges from 18 to 40%. With a viral infection, the number of lymphocytes will increase greatly. Due to them, humoral and cellular immunity is created, producing antibodies as a response to pathogens.
When the virus enters the body, the number of lymphocytes immediately increases in the body along with the number of eosinophils. This occurs in people susceptible to chronic allergies, in people with parasitic infestations, allergic dermatosis, and sarcocidosis.
High levels are observed when taking a course of antibiotics or sulfonamides. Such indicators occur in children during scarlet fever, under the influence of the Epstein-Barr virus. Therefore, it is necessary to test the blood for immunoglobulin E, for antibodies to the Epstein-Barr virus and for helminthiasis.
Treatment
If eosinophils in a child or adult deviate from the norm or are completely absent, then you need to address the provoking factor as soon as possible. In this case, treatment can be conservative or surgical, but often takes an integrated approach.
Sometimes, to restore the normal eosinophil count in a blood test, it is enough to:
- stop taking medications or replace them with analogues;
- avoid contact with the allergen;
- to refuse from bad habits.
The following can also be used to normalize eosinophils:
- medications prescribed by a doctor;
- diet therapy;
- traditional medicine.
In any case, treatment will be tailored individually for each person.
Symptoms of elevated eosinophils in the blood of an adult
An increased eosinophil threshold in an adult patient is reflected in the following symptoms of eosinophilia:
- primary - are the main symptoms of severe diseases of the hematopoietic system;
- secondary, or reactive, which arise as a result of diseases not entirely related to blood pathology;
- of unknown origin.
As a rule, an excess of the normal level of eosinophils in the blood is manifested by the following symptoms:
- increased fatigue;
- drowsiness;
- apathy;
- pallor;
- severe headaches.
Symptoms and signs
There are no signs that characterize eosinophilia as such, since it is not an independent disease. Although, under the influence of certain factors, when eosinophils in the blood are reduced, patients complain of similar symptoms.
For pathologies of a parasitic nature:
- lymph nodes, liver and spleen enlarge;
- the development of anemia is noted - especially against the background of damage to the intestinal system, malaria;
- weight loss;
- the temperature always remains within the subfebrile range;
- joint and muscle pain, lethargy, and lack of appetite appear;
- dry paroxysmal cough and skin rashes occur.
Important information: What does it mean that the width of platelet distribution by volume is higher than normal?
The person complains of constant fatigue, loss of body weight and a feeling of hunger even with increased food consumption, dizziness due to anemia, prolonged causeless hyperthermia. Such signs indicate poisoning of the body with waste products of helminths and other harmful microorganisms, an increase in an allergic reaction to them, and disruption of digestive function and metabolism.
If low eosinophils in an adult are accompanied by allergies, the development of skin itching (nettle fever), blisters, swelling in the neck (Quincke's edema), and a characteristic urticarial rash is noted.
Collapse, a sharp decrease in blood pressure, skin peeling and shock are possible.
If low eosinophilic cells have led to damage to the gastrointestinal tract, the patient complains of vomiting, diarrhea, pain and discomfort in the abdomen, blood or pus in the stool due to colitis. In this case, the symptoms are due to the development of the disease in the gastrointestinal tract.
When eosinophils below normal are accompanied by oncology, the occurrence of fever, lethargy, weight loss, joint and muscle pain and aches, an increase in the size of the liver, spleen and lymph nodes, and diseases of an infectious-inflammatory nature are observed.
Non-pathological reasons for the increase
Eosinophils may be elevated in an adult for the following non-pathological reasons:
- blood disease (in particular, sickle cell anemia - the incorrect shape of red blood cells provokes an increase in their sedimentation rate, and will differ significantly from the standard values);
- the presence of a heart attack or stroke (such cases of inflammation when acute-phase proteins are adsorbed into the surface of blood cells and reduce their electrical charge);
- diseases that are associated with impaired metabolism (diabetes, cystic fibrosis, obesity);
- bronchial asthma;
- liver diseases and problems with the biliary tract.
How and under what conditions are they produced?
Eosinophils in a child (the norm depends on age) and an adult are produced in the bone marrow, provided that it functions normally. The maturation process of these cells takes 6 to 8 days. The specific period depends on the individual characteristics of the organism. At the first stage, a universal cell called a precursor is formed in the bone marrow.
It is the initial stage for almost all cells. After this, the precursor becomes a monoblast. This species is more similar in structure to an eosinophil. The next stage of formation is the eosinophilic promyelocyte. Its size is smaller than that of a mature eosinophil.
After this, the promyelocyte turns into a myelocyte, which, in turn, turns into a metamyelocyte. The next form is band eosinophil. These cells are also called immature because they are not able to fully perform their function. After the band eosinophil phase, a full-fledged segmented cell is formed, which can already enter the bloodstream.
Mature eosinophils are present in the blood for no more than 4 days, after which they are distributed throughout the body, concentrating in the tissues. For 10-14 days, the cells remain in organs and tissues, protecting them from foreign microorganisms. After this, the cells die. If necessary, the brain commands the bone marrow to form a new colony of eosinophils.
Degrees of eosinophilia
A general clinical blood test reflects the percentage of blood leukocytes, as well as the quantitative level of eosinophils. Their significant excess in the red fluid of blood vessels is called eosinophilia.
Hematologists believe that eosinophilia comes in three stages:
- light - from 400 to 1500x10^9 per liter, when the peripheral blood contains no more than 15% of white blood cells;
- moderately expressed, moderate - from 1500 to 5000x10^9 per liter, in case of excess from 15 to 20%;
- severe, called major blood eosinophilia - more than 5000x10^9 per liter, when the number exceeds 20%, a condition usually combined with an increase in the total number of leukocytes.
The upper limit of eosinophil content EO makes it possible to assess the level of immunity and more accurately determine the root of the disease. A sharp increase is observed during infection with bacterial infections, during acute purulent inflammation, in the case of an existing allergic reaction, during a parasitic invasion.
In opposite cases, a drop in the leukocyte blood level means the presence of a viral infection in the body. The percentage of different types of leukocytes is reflected in a special leukocyte formula.
Increased level
An increase in the number of eosinophils – eosinophilia. There are several degrees of this pathological process:
- Light – increase in cell level by no more than 10%;
- Moderate – increase in the number of cells by 10 – 15%;
- Pronounced – the cell level increases by more than 15%.
Causes of eosinophilia:
- The physiological reason in women is the 1st half of the menstrual cycle;
- The presence of parasites in the body;
- Allergic reaction of the body to various foreign agents (dust, food, medications, plants, care and hygiene products, and so on);
- Autoimmune diseases (polyarthritis, bronchial asthma, gout and others);
- Pathology of the gastrointestinal tract (gastritis, peptic ulcer of the stomach and intestines);
- Skin diseases (eczema, dermatitis);
- Acute and chronic course of infectious processes (tuberculosis, mononucleosis, sexually transmitted infections);
- Lack of magnesium in the body;
- Rhesus conflict pregnancy;
- Malignant tumors of organs and blood.
To normalize neutrophil levels, it is necessary to identify the cause of eosinophilia. Treatment tactics directly depend on the etiology:
- If allergies are to blame, then first of all it is necessary to identify and eliminate the allergen from the patient’s life. Antihistamines are prescribed to relieve symptoms. If a severe allergic reaction develops (Quincke's edema, anaphylactic shock), then it is necessary to provide the patient with emergency care and hospitalize him;
- In the presence of infection, appropriate treatment is indicated under the supervision of a physician, strengthening the immune system with the help of nutrition, vitamin complexes and herbal remedies (Eleutherococcus, Echinacea);
- If parasites (worms) are detected, antiparasitic drugs are prescribed according to the regimen and an appropriate diet;
- If a specific disease is detected (tuberculosis, cancer, etc.), then special treatment is prescribed.
Features of pulmonary eosinophilia in adults
Pulmonary eosinophilia is also called eosinophilic lung disease. It is described by various conditions that are characterized by opacities in the lungs on an x-ray or computed tomogram. This is associated with eosinophilia of the lung tissues, as well as peripheral blood.
The diagnosis is established by at least one of the following signs:
- infiltrates in the pulmonary tissues, as well as eosinophilia observed in the peripheral blood;
- confirmation by open biopsy or bronchobiopsy of eosinophilia of lung tissue;
- bronchoalveolar lavage fluid contains an increased number of eosinophils.
Many drugs of various categories (leukotriene inhibitors, GCs, type 4 phosphodiesterases, chemokine receptors, cromolyns, cyclosporines, antihistamines, monoclonal antibodies to IL5 (mepolizumab) and IL13 (lebrikizumab), alpha interferon) inhibit the activity of eosinophils or the harmful effects of their products.
Symptoms
There is no specific clinical picture that eosinophils in the blood are low. The nature of the symptoms will depend on what exactly provoked such a violation. In some cases, symptoms may be completely absent for a long time or may occur in a latent form.
In general, the symptom complex may include the following signs:
- general deterioration of health, malaise;
- low-grade body temperature, possibly high;
- disruption of the functioning of the gastrointestinal tract;
- unstable blood pressure;
- loss of appetite;
- weight loss for no apparent reason;
- skin rashes;
- inflammation of the lymph nodes;
- ARVI symptoms – cough, runny nose, sore throat, drowsiness;
- pain in the chest, which can radiate to the back and arms;
- irritability, apathy, sudden mood swings.
If eosinophils are low in a child, the clinical picture may include signs such as:
- moodiness, constant crying;
- the baby sleeps poorly, refuses to eat;
- inactive;
- burps frequently.
The manifestation of at least a few symptoms from the above list may indicate the development of a certain disease, the nature of which can only be determined through diagnostic measures.
Eosinophilia during pregnancy
During pregnancy, allergies can cause eosinophilia.
Patients may exhibit the following symptoms:
- red spots on the skin, hives;
- stuffy nose;
- presence of a slight itching sensation;
- the skin is peeling.
Excessive intake of foreign protein into the blood triggers one of the body’s protective reactions in the form of eosinophilia. With the development of hypoxia, the same condition may develop in the case of a lack of magnesium in pregnant women.
A similar disease is also typical for expectant mothers who have received a dose of radiation, or for those who have various forms of congenital heart disease, or who have recently had scarlet fever. From this, a mixed group is also distinguished, which consists of other various diseases that cause persistent eosinophilia.
Hepatosis of pregnancy, that is, a violation of cellular substances in the liver during pregnancy, can also provoke eosinophilia. A disease that is not cured in a timely manner can even lead to a terrible death for the fetus and the pregnant woman herself. The main goal of treating eosinophilia is to eliminate the causative agent of the disease itself.
A specialized medicinal course is carried out, which includes the following:
- painkillers;
- medications to eliminate edema;
- drugs that eliminate allergic reactions.
The diagram shows the main causes of increased eosinophil levels.
There are special cases when you should avoid prescribing medications altogether during pregnancy.
What to do in case of a “bad” analysis?
The doctor who ordered the study should read the results of the OAC. If a person passes the test on his own, violations should be addressed to a pediatrician (if this is a child) or a therapist. It is important not only to study indicators that are outside the normal range, but also to correlate them with the values of other blood cells.
Eosinophilia and elevated ESR may indicate a disease accompanied by an inflammatory process. High levels of eosinophils and low platelets accompany viral infections and bone marrow pathologies. Diseases of the hematopoietic system are indicated by an increase in the level of eosinophils and a change in hematocrit. Cells can be detected in biopsies and various biological fluids. This helps in identifying the place where toxins enter the body or the location of malignant tumors.
If there is a significant increase in eosinophil levels, you should take the CBC again. This will eliminate errors during the study or disruption of preparation for it. If violations are detected again, an examination should be started. If eosinophils are elevated, you need to take the following tests:
- blood biochemistry;
- general urine examination;
- feces for helminth eggs or blood for worm antigens;
- immunogram;
- liver tests;
- allergy tests;
- antinuclear antibody test;
- rheumatoid factor.
To clarify the analysis information, ultrasound of internal organs, CT or MRI, and fluorography of the lungs are performed. To exclude malignant diseases, tumor markers and a bone marrow or lymph node biopsy are prescribed.
Diagnostics
In practice, to refute or, conversely, to confirm the presence of the disease, sick people need to take a blood test. Only its results will be able to accurately indicate whether the level of eosinophils is elevated. They also indicate the percentage of white cells, and recognize such signs of anemia as a lower number of red blood cells and a sharp decrease in hemoglobin.
At the stage of diagnostic processes, the doctor carefully studies the patient’s complaints and analyzes the history of the course of his illness. A preliminary diagnosis of the disease is established based on the results of blood tests and the results of a general examination. Often some specialized research is required.
The following additional tests are usually required:
- general urinalysis;
- to identify parasites - taking a stool sample;
- checking kidney and liver function;
- upper chest x-ray;
- puncture of the affected joint;
- bronchoscopy.
FAQ
Question: What is eosinophil cationic protein? How and why is it defined?
Answer: A cationic protein is a specific substance that acts as a mediator for eosinophils and is released from their granules when immunoglobulin E comes into contact with allergens. The indicator is measured in blood serum. The value is important for diagnosing most types of allergies (food, contact, bronchial asthma, atopic dermatitis, allergic rhinitis), as well as for monitoring the effectiveness of therapy.
Question: Is it possible to get vaccinated if you have elevated eosinophils?
Answer: The issue of vaccination should be resolved with the pediatrician who is monitoring the baby. It all depends on age, the presence of anxiety symptoms, and individual characteristics. In children under one year of age, the blood picture is unstable. If at this time there are no signs of allergies, viral or parasitic infections, slight deviations in eosinophils are not considered a contraindication. During periods of active sensitivity reactions, accompanied by rashes and general poor health, it is better to refrain from vaccinations.
Question: What does a rhinocytogram result in which eosinophils are highly elevated mean?
Answer: A rhinocytogram is the study of a smear from the nasal mucosa under a microscope. It helps to assess the functioning of local immunity, detect infectious diseases and other causes of inflammation of the membranes. Exceeding the norm of eosinophils always indicates an allergic origin of rhinitis. However, even if the cell level is within normal limits, an allergy cannot be ruled out. The analysis is needed for a comprehensive diagnosis of seasonal allergic reactions; its results are studied together with other information obtained during the examination.
Question: Have you heard that the level of corpuscles is checked in the urine, nose, and sputum? Why do they do this and how do blood cells end up in other fluids?
Answer: Eosinophils are everywhere. These bodies are released into the blood and eventually migrate to peripheral tissues. Large concentrations are concentrated on the mucous membranes. Here the cells are involved in local immunity. The level of eosinophils in a nasal swab, as well as in sputum, is indeed determined. This is necessary for diagnosing allergic diseases. The total number of leukocytes in the urine is counted (without defining groups). Exceeding the norm accompanies inflammatory lesions of the kidneys and urinary tract.
Question: What is better to take if the levels are only slightly elevated - an anthelmintic or an antiallergic?
Answer: Drugs from these groups cannot be taken independently in order to correct the blood picture. You need to focus on the symptoms. If the cause of the deviation is obvious, it is permissible to begin treatment, but you need to understand its nature - determine the type of parasites, detect the allergen and the method of its penetration into the body. One-time use of drugs instead of full-fledged therapy cannot lead to recovery or a decrease in the levels of protective cells in the blood.
Treatment of eosinophilia in adults
In order to determine the disease that provoked eosinophilia, in addition to taking a clinical blood test, patients are also given a biochemistry test. Treatment is usually carried out by a hematologist. Such a disease is not considered an independent disease, but is only a pronounced symptom of another disease; therefore, it is necessary to treat its original cause.
First, you need to determine why the number of white blood cells has increased, and then carry out therapeutic measures, including prescribing medications with physiotherapy. The choice of different treatment methods is carried out based on the actual physical condition of the patient, the nature of his illness, his age, well-being, and other concomitant diseases.
It happens that in order to cure, on the contrary, it is necessary to stop taking medications.
Close attention should be paid to enzymes that are located in the liver. To completely exclude the possibility of helminthic infestation, antiparasitic tests are required. And to confirm a runny nose due to allergies, a nasal swab is taken. The doctor may also prescribe an x-ray examination of a person’s air breathing organs and take a puncture from his diseased joints.
If rheumatoid arthritis is suspected, a bronchoscopy will be necessary. Often, the attending physician prescribes a specialized course of treatment, including: painkillers, medications to reduce swelling, drugs that eliminate a pronounced allergic reaction.
The main direction of healing lies in the elimination of the pathogen itself - the source of the disease. The course may have a different duration, depending on the results it will be regularly adjusted, or even completely changed.
Along with drug therapy, physiotherapy and herbal medicine are often used in treatment. In addition, your doctor may prescribe a specialized diet.
It is necessary to periodically monitor blood tests in the clinic in order to prevent an increase in the level of eosinophils in an adult. Such an increase always means the presence of a serious illness. When there are other additional signs, you should definitely consult a doctor. The process of eosinophilia itself cannot be overcome; only the disease that provoked it can be cured.
If eosinophils are elevated in an adult, what does this mean?
The level of the indicator in the blood is affected by the time of collection of biomaterial. In the evenings and early mornings, the amount of EO increases by 15%, which is a variant of the physiological norm. At night the rate can increase by 15-25%.
The patient receives recommendations for further diagnostics if the EO level is consistently higher or at the upper limit of normal.
An increase in EO levels in a nasal swab or blood test is commonly referred to as eosinophilia. This is a pathological condition that can be caused by a wide range of different diseases.
Read further: All about low eosinophils in the blood in adults and children
Main reasons for increased EO in adults by disease group
Let us consider the reasons for the increase in eosinophils in adult patients by disease group.
Atopic diseases
The first group: atopic diseases, which indicates a person’s genetic predisposition to an allergic reaction. The mechanism of atopic diseases is carried out due to an immediate hypersensitivity reaction. These include:
- allergic rhinitis or “hay fever” is an inflammatory reaction of the nasal mucosa upon contact with allergens. Accompanied by nasal congestion, itching and sneezing. It may occur episodically (less than 4 days a week) or become chronic (more than 4 weeks a year). Eliminating contact with an allergen that irritates the nasal mucosa significantly alleviates the person’s condition;
- bronchial asthma – chronic allergic inflammation of the respiratory system. Accompanied by narrowing of the bronchial lumen and hypersecretion of thick mucus;
- serum disease is a pathological condition that occurs in response to the administration of immune sera. They are based on foreign protein antibodies of animal origin. In this case, the human body may exhibit an allergic reaction to them;
- atopic eczema is a chronic inflammation of the skin. It is characterized by frequent relapses and seasonality: in summer the disease manifests itself much less than in winter;
- Seasonal allergic rhinoconjunctivitis is a particular type of human allergic reaction to pollen.
Parasitic infestations
Increased eosinophils in the blood of an adult are observed during parasitic infections: roundworms, lamblia, opisthorchiasis, toxocara and other types of parasites.
Diseases of the digestive system
Diseases of the gastrointestinal tract are another reason for the increase in the rate. Possible pathologies: peptic ulcer, gastritis, liver cirrhosis or eosinophilic gastroenteritis. If these pathologies are suspected, the patient is advised to consult a gastroenterologist and conduct additional diagnostic methods.
Blood diseases
A separate group of reasons for increased EO are blood diseases:
- Addison-Beermer disease or megablastic anemia, when a person’s normal hematopoietic process is disrupted due to a lack of vitamin B12;
- leukemia resulting from a mutation in a stem cell. As a result, complete differentiation of blood cells is impossible;
- Hodgkin's disease is a malignant pathology, the causes of which have not been established;
- primary polycythemia, leading to an increase in the concentration of red blood cells and leukocytes in the blood.
Others
A deviation in the number of EOs also accompanies oncological pathologies, rheumatic diseases and a state of immunodeficiency, acute infectious diseases (scarlet fever, chickenpox, infectious mononucleosis, tuberculosis), myocardial infarction (an increase in the level of eosinophils is an unfavorable diagnostic criterion), some lung pathologies (pulmonary eosinophilic pneumonia, eosinophilic pleurisy, sarcoidosis, eosinophilic pulmonary infiltrates (Leffler's disease), etc.).
Causes of eosinophilia
Allergies
This is the most common cause of eosinophilia. Any hypersensitivity reactions are accompanied by an increase in the production of eosinophils by the bone marrow. The pathogenesis of eosinophilia in allergies has been well studied. When an allergen enters the body (inhalation, through the skin or mucous membranes), it interacts with IgE on the basophil membrane. This leads to their degranulation of the latter and the release of histamine, leukotrienes and other mediators, as a result of which allergic inflammation develops in the tissues, which causes symptoms of the skin (atopic dermatitis, urticaria), mucous membranes (allergic rhinitis, conjunctivitis), as well as respiratory systems (bronchial asthma).
In parallel with this, basophils secrete the eosinophilic chemotactic factor of anaphylaxis, which stimulates the migration of eosinophils from the peripheral blood to the site of inflammation. Eosinophils, in turn, suppress the production of allergy mediators. During the height of the allergic reaction (exacerbation), the level of eosinophilia is maximum; as symptoms resolve, it gradually decreases and normalizes into remission.
With severe exacerbation, the content of eosinophils, on the contrary, may be reduced (eosinopenia) or even zero (aneosinophilia). This happens when there has been a massive migration of eosinophils to the site of allergic inflammation, and new eosinophils have not yet had time to be synthesized in the bone marrow. Also, if during a relapse of bronchial asthma a secondary bacterial infection (bronchitis) occurs, then eosinophil levels may remain within normal limits.
Mostly with allergies, a mild degree of eosinophilia occurs. Bronchial asthma, especially the atopic and aspirin-induced form, is characterized by moderate eosinophilia. In allergic pathologies, an increased content of eosinophils is observed not only in the blood, but also in other biological fluids (in sputum and bronchoalveolar fluid - with bronchial asthma, in nasal mucus - with rhinitis, in scrapings from the conjunctiva - with conjunctivitis).
Helminthiasis
Another common cause of eosinophilia (especially among children) is infection with helminths. Eosinophilia in this case is caused by two pathogenetic mechanisms. Firstly, eosinophils have antiparasitic activity - they secrete eosinophilic cationic protein and reactive oxygen species, which are harmful to helminths. Secondly, helminth metabolic products can induce hypersensitivity reactions. This is why helminthic infestations are often accompanied by allergic symptoms.
The most common helminthiases associated with high eosinophilia among children are ascariasis and toxocariasis; among adults, hookworm disease and opisthorchiasis. In strongyloidiasis, eosinophilic leukocytosis may be the only manifestation for a long time. Eosinophilia is detected already on days 4-5 of infection. Then it increases very quickly and reaches a maximum at about 30-40 days, and then slowly begins to decrease, but continues to remain at high levels for a long time. The level of eosinophils is very high (can range from 20% to 70-80%). A sharp increase in eosinophilia occurs during the stage of larval migration throughout the body and penetration into tissues.
Lung diseases
There is a group of lung diseases called pulmonary eosinophilia, which combines a high content of eosinophils in the blood, in the bronchoalveolar fluid and the formation of eosinophilic infiltrates in the lung tissue. The exact pathogenesis of peripheral blood eosinophilia and eosinophil infiltration of lung tissue in most of these diseases is unknown. The following pulmonary eosinophilias are distinguished:
- Eosinophilic pneumonia.
These include Loeffler's syndrome (simple pulmonary eosinophilia), acute, chronic eosinophilic pneumonia (AEP, CEP). With Loeffler's syndrome, mild eosinophilia is observed, which resolves quickly and spontaneously. CEP is characterized by constant moderate eosinophilic leukocytosis. With OEP, eosinophilia is observed, sharply increasing to high numbers (up to 25%) and just as rapidly regressing during glucocorticosteroid therapy. - Allergic bronchopulmonary aspergillosis.
Caused by the hypersensitivity of patients to fungi of the genus Aspergillus. The pathogenesis is similar to allergic pathologies (IgE-mediated reaction). Eosinophilia is moderate and occurs only during the acute phase. During the period of remission, the level of eosinophils is within normal values. - Churg-Strauss syndrome.
Eosinophilic granulomatosis with polyangiitis is a severe disease of unknown etiology from a number of systemic vasculitis, affecting several internal organs. Eosinophilic leukocytosis is the highest among all pulmonary eosinophilias; during relapse it can reach up to 50%.
Eosinophilia may occur in lung diseases
Blood diseases
During some malignant hematological diseases, an increased level of eosinophils is observed in the blood with a different pathogenetic mechanism. In myeloproliferative pathologies (acute and chronic eosinophilic leukemia, chronic myeloid leukemia), aggressive systemic mastocytosis, eosinophilia is caused by tumor (clonal) proliferation of the eosinophilic lineage of hematopoiesis.
Eosinophilia increases slowly over several years. With mastocytosis it reaches moderate values, with leukemia – pronounced (up to 60-70%). It decreases very slowly under the influence of chemotherapy. In addition to peripheral blood, eosinophilia is also observed in the myelogram (bone marrow punctate smear). For leukemia, there is a specific laboratory sign - a simultaneous increase in eosinophils and basophils (basophil-eosinophil association).
In lymphogranulomatosis and non-Hodgkin's lymphomas, eosinophilia occurs due to the production of cytokines (including interleukin-5) by lymphatic cells, which stimulate the proliferation of normal eosinophils. Eosinophilic leukocytosis is moderate, slowly increasing.
Gastrointestinal diseases
Eosinophilia accompanies some diseases of the digestive system. These include eosinophilic esophagitis, gastritis and enterocolitis. The morphological substrate is the infiltration of eosinophils into the walls of the esophagus, stomach, and intestines. Pathogenesis is still a matter of debate.
It is assumed that in hereditarily predisposed individuals, exposure to food allergens on the mucous membrane causes activation of antigen-presenting cells (T-lymphocytes), producing interleukins and eotaxin-3. As a result, eosinophils migrate and infiltrate the mucous membrane of the gastrointestinal tract. Eosinophilic leukocytosis is usually mild and is observed only during severe exacerbation of the disease. A high concentration of eosinophils in mucosal biopsies, on the contrary, is a constant occurrence.
Endocrinopathies
Some hormones, such as glucocorticosteroids (hormones of the adrenal cortex), stimulate apoptosis (programmed cell death) of eosinophils. Therefore, diseases accompanied by a decrease in the level of glucocorticosteroids are accompanied by eosinophilia. Such pathologies include primary adrenal insufficiency (Addison's disease), congenital dysfunction of the adrenal cortex, as well as multiple endocrinopathies, such as Schmidt's syndrome, panhypopituitarism. The degree of eosinophilia is mild. The number of eosinophils quickly normalizes after administration of glucocorticoids.
Immunodeficiency conditions
Eosinophilia occurs in so-called primary immunodeficiencies - severe diseases with high mortality caused by a genetic defect in one or more components of the immune system (cellular, humoral reactions, phagocytosis, etc.). Such diseases are Wiskott-Aldrich syndrome and Jobe syndrome (hyper-IgE syndrome). Eosinophilia is probably associated with abnormal hyperproduction of immunoglobulin E. The level of eosinophils in tissues and blood is very high (up to 60%) and cannot be corrected.
Malignant neoplasms
Some tumors, especially adenocarcinomas of the lungs, digestive and genitourinary systems, have the ability to produce eosinophilic chemotactic factor, which stimulates the bone marrow production of eosinophils. In such diseases, eosinophilic leukocytosis increases slowly and reaches high values (up to 20-40%). The concentration of peripheral blood eosinophils returns to normal after long-term chemotherapy or surgical removal of a malignant tumor.
How to get it back to normal
Depending on the disease that caused the decrease or increase in indicators, the specialist prescribes appropriate treatment.
Medications
Scroll:
- Claritin is an antiallergic drug based on loratadine that has a pronounced effect. Used in combination with other agents or as the main treatment. Children under 12 years of age are prescribed syrup; the dosage is determined based on weight. Adult patients can take 1 tablet per day. The duration of the course can be 5-10 days.
- Sumamed is an antibiotic from the macrolide group that has a pronounced anti-inflammatory effect. Used when the number of eosinophils is changed as a result of the inflammatory process in the internal organs. Available in tablet form and also in the form of syrup. The dosage is determined individually, taking into account body weight, if we are talking about a child. Children over 16 years of age and adults can take 2 tablets per day for 3-7 days.
- Vermox is a drug used to combat various types of helminths. It is highly effective and destroys parasites in the intestines. After receiving the results of additional diagnostics, the specialist uses one of the possible schemes. The first is used in case of detection of one type of parasite. In this case, a child or adult takes 1 tablet once. If several types of different helminths are detected, the course lasts 6 days, the patient takes 1 tablet daily.
- Filtrum is an enterosorbent used for intestinal upset, stomach pain and other symptoms of the digestive system. The duration of the course usually does not exceed 3-5 days. During this period, a child 1-2 years old is given 0.5 tablets, from 2 to 7 years old - 1 tablet. Patients over 7 years of age receive 2 tablets, patients over 12 years of age and adults are allowed to take 3 tablets per day.
- Ibuprofen is a non-steroidal anti-inflammatory drug based on the active ingredient of the same name. Usually used in combination with antibiotics, it helps relieve signs of inflammation and reduces body temperature. A child receives from 5 to 15 ml of syrup per day, depending on age. Adults take 2-3 tablets per day. The course lasts no more than 5 days.
- Imudon is an immunostimulating drug that is used for pathologies of the throat and pharynx during exacerbation of colds and viral diseases. The tablets contain dry bacterial cultures. The medicine is intended for resorption. Children from 3 to 14 years old are prescribed 6 tablets per day, adults and children over 14 years old - 8 tablets per day. They must be absorbed regardless of food intake, but the interval between procedures must be at least 2 hours. Duration of treatment: 5-7 days.
- Dexamethasone is a hormonal medication based on betamethasone. Prescribed for serious allergic or inflammatory disorders. The solution is administered intramuscularly, but the dosage is determined individually taking into account the age and weight of the child. The duration of the course is 2-5 days.
- Alphabet is a vitamin complex that is used to strengthen the patient’s immune system. The complex is selected taking into account age, since the line contains vitamins for preschool, school and teenage children. The daily dose is 1 tablet, duration of use is 30 days.
During the treatment period, all means are not used simultaneously; the regimen is drawn up depending on the specific disorder.
Traditional methods
Eosinophils in a child (cell norms are clarified by a specialist) can be produced intensively or slowly, not only as a result of any diseases. Overwork, mental stress and weakened immunity can cause the disorder. That is why indicators should be adjusted using natural remedies.
An infusion based on viburnum berries is a good remedy for maintaining immunity and relieving fatigue. You can prepare it from 1 tbsp. l. berries and 300 ml of boiling water. It is necessary to infuse the product for 20 minutes; it is better to mash the berries before adding boiling water.
Filter the finished infusion, add a little honey to taste. Children from 3 years old can take 50 ml per day, repeat for 2 weeks. A mixture based on honey and dried fruits is considered the best immunostimulating agent.
To prepare you will need:
- 150 g honey.
- 100 g figs.
- 100 g dried apricots.
- 100 g raisins.
- 100 g walnuts.
All dried fruits and nuts must be chopped in a meat grinder; the lemon and peel must also be chopped. Mix the resulting mass and pour in honey. Take the mixture 2 tsp. per day until the composition runs out.
Other methods
Other treatment methods include regular exercise, which helps maintain immunity and stimulate the renewal of all cells in the body. It is better to create a set of exercises together with a specialist who will suggest the most optimal ones and also adjust the program.
In addition, it is useful to visit the pool, which will help not only train muscles, but also strengthen the child. It is enough to visit the pool 2 times a week and spend 30-40 minutes swimming. It is also important to normalize your diet, to include fresh vegetables and fruits, nuts, cereals and other foods that contain the maximum amount of useful components.
General information
Eosinophilia is diagnosed in a patient if a laboratory analysis reveals an absolute or relative increase in the number of eosinophils in the blood.
Eosinophilia is defined if the number of eosinophils in the peripheral blood exceeds 500/μl. This condition is a marker of pathological changes in the body; it is characteristic of a very large number of diseases. Very often, a similar phenomenon is observed with a parasitic infection, as well as with allergic manifestations. Hypereosinophilic syndrome is a condition in which there is eosinophilia in the peripheral blood and there is damage or dysfunction of organ systems. Hypereosinophilic syndrome is characterized by eosinophilia in people without parasitic, allergic manifestations, or other causes of eosinophilia.
This article will discuss why eosinophilia occurs and what to do if such a condition has been diagnosed.
Tests and diagnostics
Since there is a very large list of reasons why a person’s number of eosinophils increases, during the diagnostic process the doctor needs to study the medical history in detail and conduct an examination of the patient. First of all, the doctor conducts a survey and analyzes the likelihood of the most common causes - allergic reactions, neoplastic complications, infectious diseases. The specialist must find out what medications the person took and whether he had systemic symptoms.
A blood test for eosinophils is performed as part of a general blood test. A biochemical blood test is performed to more accurately determine the condition of the body.
If necessary, eosinophilic cationic protein is determined - a non-invasive marker of eosinophilic inflammation in allergic diseases and other conditions. Speaking about what eosinophil cationic protein shows, it should be noted that the ECP content is directly proportional to the number of eosinophils.
Another indicator, eosinophil cationic protein (ECP), allows you to determine the severity of eosinophilic inflammation.
If eosinophilia is confirmed, additional studies are performed:
- A nasal swab for eosinophils (rhinocytogram) is carried out to exclude the allergic nature of the disease. It is advisable to perform a nasal swab if allergic rhinitis is suspected.
- Examination of stool for the presence of worm eggs and parasites. A repeat test may be required, as well as testing for other parasites.
- Other tests - to find out the cause of the condition, they examine the heart, skin, nervous and respiratory systems. A urine test, chest x-ray, liver function tests, etc. may be required.
In children
The norm of eosinophils in children, depending on their age, is 0.07-0.65 x 10^9/ml. If a blood test determines that a child’s eosinophils are elevated, the reasons may be associated with a number of diseases and conditions:
- parasitic infections, helminthiasis;
- autoimmune diseases;
- allergic manifestations;
- asthma;
- granulomatous processes;
- taking medications;
- lymphogranulomatosis , malignant formations (the level of eosinophils is several thousand times higher than normal, a basophilic-eosinophilic association is possible).
However, eosinophilia in children can occur due to a variety of reasons, so when interpreting the tests, it is important to take into account the general health of the child.
In an infant, this condition may be associated with a reaction to medications, the consequences of an intrauterine infection, allergies, or eosinophilic colitis. In infants, this condition can also be a consequence of lactose intolerance.