Confirming the diagnosis in the presence of signs of pathology of the digestive tract is the main task of the specialist. For this purpose, various diagnostic methods are used. Invasive research is the main direction in patient examination. FEGDS is considered the gold standard for diseases of the esophagus, stomach and duodenum.
With its help, you can see changes in the mucous membrane and take material for analysis. Intravital sampling of tissue sections followed by histological examination is called a biopsy.
Table of contents
- Indications for prescribing a gastric biopsy
- Contraindications to endoscopic manipulation of the stomach
- How to prepare for a biopsy
- How to do a gastric biopsy Chromogastroskopiya
- Biopsy technique
- How is a biopsy specimen examined?
- Long-term complications after biopsy
- Nutrition after gastric biopsy
Following actions
If the results of a gastric biopsy contain terms such as “atypical cells”, “cribrous structures”, “signet ring cells”, “carcinoma”, “cancer” and others, then you should not panic. To clarify the diagnosis, it is recommended to do a repeat gastroscopy with a biopsy (preferably in another clinic and with another doctor) and if oncological pathology is detected again, then only in this case should you contact an oncologist.
In the most modern Israeli clinic Top Ichilov , thanks to the use of the latest techniques and drugs, more than 90% of the clinic’s patients suffering from stomach cancer recover completely or achieve significant improvement and long-term remission.
Treatment of stomach cancer in Israel is carried out by world-class specialists who practice the latest methods of fighting cancer: chemotherapy, immunotherapy and biotherapy using the latest drugs that are selected individually for each patient in accordance with the results of advanced molecular genetic tests, a unique HIPEC chemotherapy technique that allows achieve better results and avoid side effects, the Da Vinci robotic surgical unit, with the help of which microsurgical operations of increased complexity are performed, and many others. You can find out more about treatment in Israel by filling out a request in the form below.
If a study was carried out on H. pylori and a biopsy confirmed the presence of these bacteria, complex eradication therapy using 3-4 drugs is prescribed. After 10-14 days, FGS must be repeated to evaluate the effectiveness of treatment.
Indications for prescribing a gastric biopsy
If a patient experiences symptoms that indicate a malfunction of the digestive system, the doctor recommends undergoing a thorough examination. In most cases, adults require extended gastroscopy. The procedure is prescribed by a gastroenterologist for the purpose of differential diagnosis of the condition or to monitor the quality of therapy.
Why is a gastric biopsy taken?
- to identify tumors of the upper digestive tract;
- clarification of the location, size, nature of the modified tissue;
- confirming the stage of cancer;
- to determine the ulcerative process of the stomach, duodenum;
- for the purpose of visualizing changes in the mucosa during chronic gastritis;
- if polyps or developmental abnormalities are suspected;
- for testing for Helicobacter pylori infection (presence of Hp);
- after surgical treatment to monitor the condition of the organ.
In emergency cases, fibrogastroscopy is performed to stop bleeding. If there is a possibility of developing an oncological process, the intervention is supplemented with a biopsy.
Interpretation of biopsy results
The conclusion usually provides a description of the histological picture (cellular and tissue structure of the biopsy) and the pathomorphological diagnosis. Despite the existence of a clear method for deciphering the results of a gastric biopsy, many doctors give an insufficiently complete description. The table presents the main terms that can be found in the results and their characteristics:
| Term | Description |
| Helicobacter pylori (Helicobacter pylori, HP ) | Bacteria, the leading cause of chronic gastritis, peptic ulcers and stomach cancer. In many laboratories, it is assessed using a system of crosses: 0 – no CP, from 1 to 3 crosses – the presence of bacteria in one quantity or another. |
| Adenocarcinoma | Name of stomach cancer. |
| Adenoma | Benign neoplasm of epithelial cells of the mucous membrane. In structure it can be tubular (in the form of tubes), papillary (in the form of finger-like processes) and mixed. Adenocarcinoma often develops against the background of adenoma. |
| Activity | A conditional indicator reflecting the degree of inflammation of the mucous membrane. Assessed by the number of neutrophils, leukocytes, degree of metaplasia and atrophy. Divided into 4 degrees: 0 – no inflammatory activity, 3 – severe gastritis. |
| Antrum | Section of the stomach, represented by convoluted, closely located glands. |
| Atrophy | Thinning of the mucous membrane, disappearance of folding. It is graded using a cross system from 0 (no atrophy) to +++ (complete atrophy). |
| Goblet cells | Cells that produce mucus. Normally they are not present in the stomach. A common component of intestinal metaplasia. |
| Hyperplasiogenic polyp | Benign growth of the mucous membrane due to pronounced regeneration (recovery) against the background of inflammation. |
| Hyperplastic polyp | In general, an analogue of a hyperplasiogenic polyp. |
| Purulent-necrotic masses | Accumulations of neutrophils and dead cells. Often found at the bottom of an acute ulcer. |
| Cardiac department | A section of the organ that is similar in structure to the antrum, but the glands are more loosely located. |
| Cribrotic structures | Sign of cancer: glands with common walls (normally, each gland has its own walls). |
| Lymphoid infiltration | The presence of lymphocytes, plasma cells and macrophages in the biopsy specimen. A sign of a chronic inflammatory process (gastritis). Evaluated according to the cross system. |
| Lymphoplasmacytic infiltration | The same. |
| Malingization | Malignancy. This means that in some part of a benign tumor there is a cluster of cancer cells. |
| Metaplasia | Replacement of normal gastric epithelium with intestinal epithelium. There are small intestinal and colonic metaplasia, and the latter poses a great danger in terms of cancer development. |
| Mononuclear cell infiltration | The same as lymphoid. |
| Neutrophil infiltration | Accumulation of segmented neutrophils. A sign of acute gastritis and stomach ulcers. Evaluated using a cross system from 0 to +++. |
| Paneth cells | Cells characteristic of the mucous membrane of the small intestine. Occurs with metaplasia of the small intestinal type. |
| Signet ring cells | Cells with a visible “void” in the center, which is why they look like rings under a microscope. Sign of stomach cancer. |
| Pyloric glands | Glands that are located in the final sections of the stomach. |
| Skirr | Cancer with severe fibrosis (overgrowth of connective tissue). |
| Stroma | The connective tissue base in which the glands are located. |
| Body of stomach | Middle section with straight glands and clearly visible parietal cells (which produce hydrochloric acid). |
| Fibrous tissue | Dense connective tissue. Develops against the background of chronic inflammation, occurs in the bottom and walls of ulcers, as well as in cancer. |
| Fibroplastic reaction | Overgrowth of connective tissue. Often found in descriptions of cancer. |
| Foveal hyperplasia | An increase in the number of normal cells located in the mucosal pits. |
Contraindications to endoscopic manipulation of the stomach
A biopsy of the gastric mucosa is a minimally invasive procedure. The risk of complications is very low. However, in some situations, the study is contraindicated. Limitations for taking biomaterial are reflected in Table 1.
Table 1. Contraindications for gastric biopsy
| Absolute contraindications | Relative contraindications |
| Stroke | Increased body temperature |
| Myocardial infarction | Rhinorrhea, swelling of the nasal mucosa |
| Scar changes in the esophagus in the form of stenosis | Epilepsy; mental illness |
| Attack period of bronchial asthma | Severe pathology of the cardiovascular system, hypertensive crisis; |
| Aortic aneurysm | Blood pathology – hemorrhagic diathesis |
Attention! Refusal to undergo a gastric biopsy is a relative contraindication that must be recorded in writing in the patient's outpatient record.
What is gastric endoscopy
Is preparation necessary?
As with any instrumental examination, a biopsy must be prepared in a certain way. What does this preparation include?
- The stomach must be empty - the patient is prescribed fasting for twelve hours before the procedure.
- Two to three hours before the procedure, a sedative and antispasmodic are prescribed.
- Immediately before inserting the endoscope, the pharynx and root of the tongue are treated with an anesthetic - usually a lidocaine spray.
After a gastric biopsy, the patient is prescribed hemostatic agents to prevent possible bleeding.
How to prepare for a biopsy
The preparatory stage is an important factor in obtaining a high-quality research result. When planning an examination, the gastroenterologist familiarizes the person with the procedure, finds out the medical history in order to exclude contraindications, determines the type of anesthesia, and gives nutritional recommendations. There are several general areas of work with a patient:
- Psychological attitude towards an effective result - includes an explanation of the need for this type of diagnosis for a speedy recovery, behavior correction in adults, identifying hidden fear, assistance in relaxation and calm. For emotional lability, sedatives are prescribed several days before the biopsy.
- Stabilization of the patient’s condition in the presence of concomitant pathology is the inclusion of medications that prevent the development of complications during gastroscopy. This is especially true for diseases of the respiratory and cardiovascular systems.
- Careful collection of anamnestic data regarding hypersensitivity to drugs that can be used during gastric biopsy - anesthetics, atropine, magnesium sulfate.
Specific recommendations include the following:
- Elimination of inflammatory processes in the mucous membrane of the oropharynx - local treatment of cracks and aphthae, which are located along the endoscopic tube.
- Preparing hollow organs for examination - adhere to the correct diet 2-3 days before the biopsy. Avoid foods that irritate the stomach and cause increased gas formation in the intestines. The last meal is no later than 19 pm if the procedure is carried out in the first half of the day. Drinking regime is stopped 2 hours before gastroscopy.
- Prescription of medications that eliminate flatulence (drugs based on simethicone, sorbents).
Preparation for gastroscopy of the stomach: rules for the procedure
To study the condition of the duodenum, stomach and esophagus, doctors use a gastroscopy procedure. It is carried out using a special flexible tube with a fiber-optic system. How to prepare for gastroscopy of the stomach? The procedure requires special preliminary measures both at home and in medical institutions.
Gastroscopy is only a type of endoscopic examination - a method for studying internal organs. The esophagus, bronchi and lungs, bladder or stomach can be checked, both in adults and in children.
Gastroscopy is used to determine the condition of the latter. This procedure has several synonyms - gastroenteroscopy, esophagogastroduodenoscopy or endoscopy, fibrogastroscopy or FGS, fibrogastroduodenoscopy or FGDS.
All terms have the same meaning, because its components mean:
- “esophago” – esophagus;
- “gastro” – stomach;
- “scopy” – visual inspection;
- “fibro” is a flexible tube, i.e. fiberscope;
- "duodeno" - duodenum.
A similar method is intubation, only it is aimed at collecting gastric contents using a syringe. In addition, the patient must swallow the tube independently. Gastroscopy is performed for therapeutic and diagnostic purposes. Using this procedure, the following activities are carried out:
- foreign bodies are removed from the stomach;
- pieces of tissue are taken for biopsy;
- benign formations are removed;
- medications are administered;
- cauterization of the bleeding vessel is performed;
- the dynamics of disease treatment is monitored.
There is a special room in the clinic for the procedure. In it, the patient needs to lie on the couch, and on his left side. Before the procedure begins, a plastic mouthguard is inserted into the person’s mouth, which protects against possible injury. The subject is offered local anesthesia by injecting a lidocaine solution or administering it intravenously.
After anesthesia, a specialist inserts a gastroscope equipped with a video camera through the mouth or nasal passage, and then the process of examining the digestive tract takes place. The duration of the procedure is 5-15 minutes. Gastroscopy under anesthesia takes a long time, because the person sleeps during it and wakes up much later in a separate room.
The first and main nuance in preparing for gastroscopy is the psychological attitude. Due to the widespread belief about pain and discomfort during the procedure, a person begins to fear it. There will be discomfort, but we are not talking about pain.
Modern equipment provides tolerable sensations during gastroscopy. In some cases, a person may be prescribed sedatives. Preparation for gastroenteroscopy is carried out both at home and during hospital treatment.
In the latter case, it includes the following steps:
- Consultation with a doctor. The specialist clarifies such nuances as the presence of allergies, heart pathologies, pregnancy, past surgical interventions, as well as information about blood clotting.
- Signing of documents. After discussing gastroscopy, the patient must sign a consent to the procedure.
- Direct preparation for FGDS examination. It consists of limiting food and fluid intake 8 hours before the start. What you can and cannot eat is described below.
Preparation for gastroscopy can be done at home if the person is not in hospital. It is divided into 2 stages, the first begins in another 2-3 days and requires:
- limiting spicy and fatty foods, especially if you suspect a stomach ulcer;
- taking anti-inflammatory herbal teas, such as chamomile;
- restriction of active sports;
- monitoring the condition of the stomach and intestines, i.e. for the possible occurrence of acute pain;
- refusal to take non-steroidal anti-inflammatory drugs.
How to prepare for FGDS? The following rules must be followed on the day of the procedure:
- do not smoke 3 hours before the procedure;
- tell your doctor about a possible pregnancy;
- empty your bladder before the test;
- remove jewelry, glasses or contacts, dentures;
- take a personal towel, which will be needed if you drool during the procedure;
- do not try to speak or swallow saliva during diagnosis.
Is it possible to drink before gastroscopy?
You can drink liquid on the day of gastroscopy no later than 2-4 hours before it. Coffee and mineral water without gas are allowed as drinks, and not more than 0.1 liter. Doctors recommend completely abstaining from liquids.
Such preparation for gastroscopy of the stomach in the morning will not cause discomfort, because you will have to not drink for a couple of hours. If a person last consumed liquid before bed (at about 8-10 p.m.), then by morning there will be no more liquid in the stomach. For this reason, restrictions are not required.
If you need to take a medicine that cannot be skipped, use little liquid.
What can you eat before FGS
Some diseases even require you to follow a special diet in preparation for this procedure. Such ailments include impaired excretion of food through the duodenum and stenosis of the esophagus.
On the eve of the examination, i.e. at approximately 6 pm, the patient should avoid overly hot and cold foods. The consistency of the food should be mushy or even liquid.
You can have dinner with easily digestible foods, for example:
- whole milk;
- pureed cottage cheese;
- fresh sour cream;
- low-fat yogurt;
- non-acidic kefir;
- soups with weak fish, meat or vegetable broth;
- low-fat cheese;
- eggs (soft-boiled or in the form of an omelet);
- boiled or fresh vegetables such as potatoes, carrots, beans, beets, cauliflower;
- lean fish, such as hake, pollock, pike perch, perch or pike;
- fruits such as apples, bananas, pears.
What not to eat before gastroscopy of the stomach
Preparation for FGDS of the stomach requires limiting the following foods:
- nuts;
- alcohol;
- chocolate;
- seeds;
- mayonnaise, sauce;
- fast food;
- pasta;
- dough products;
- salt;
- spicy and fatty foods.
It is better to remove prohibited foods a couple of days before gastroscopy. Before the procedure itself, the stomach must be empty, i.e. You can eat your last meal 8 hours before the procedure. This time is strictly defined, because during this time the food will be completely digested and will not interfere with the examination.
In addition, performing the procedure on a full stomach can cause vomit to enter the upper respiratory tract. If gastroscopy is performed under anesthesia, the fasting period is extended to 10-12 hours.
Stomach examinations are often scheduled in the morning, so the patient simply needs to skip breakfast.
How to do a gastric biopsy
Diagnosis is performed on an empty stomach. The endoscopist selects the optimal anesthetic for the person. When preparing to collect material from different parts of the stomach, general anesthesia is used.
This method is more gentle. Follow these rules:
- The subject is placed on his left side, with a towel placed under his head.
- A mouthpiece is inserted into the mouth to avoid damaging the teeth and mucous membrane of the oral cavity.
- The tube is inserted through the mouth and gradually moved towards the stomach. Along the digestive tract, the doctor examines tissue and takes samples from several areas.
Important! The endoscopic system is equipped with various attachments, including a device for gastric biopsy. Through a special hole, the walls of the esophagus, stomach and initial parts of the intestine are inflated with air for better visualization. They also perform chromogastroscopy and conduct a study for Helicobacter pylori.
- A biopsy of the stomach is performed: for this, pieces of the mucous membrane are taken with forceps in the amount of 3-5 samples in several places. The collection of pathological material is carried out at the border of healthy and modified tissues.
How long does it take to perform a gastric biopsy?
The time for performing FGS with histology ranges from 5 to 20 minutes, depending on the complexity of the procedure.
Chromogastroscopy
An additional type of research is the use of special dyes to diagnose certain conditions. The chromogastroscopy method makes it possible to identify morphofunctional changes in the mucous membrane of the stomach and duodenum, which are difficult to determine with standard FGDS. Several combinations of drugs are used for staining:
- 1.5% Lugol's solution and 0.5% aqueous solution of methylene blue;
- 0.3% solution of indigo carmine and 0.5% aqueous solution of methylene blue;
- 1% Congorot solution and 0.3% acidified Congo red solution.
The use of special substances helps solve the following problems:
- clarifies the state of acidity and pH level in the proximal parts of the digestive tract;
- detects areas of metaplasia and aplasia of the mucous membrane;
- shows cancer in its early stages;
- increases the possibility of predicting the course of peptic ulcer disease.
When staining, modified areas, defects and their borders with healthy tissues are better visible. Therefore, gastric biopsy is performed more accurately and efficiently.
The procedure for collecting suspicious areas of tissue is done through a Teflon catheter, which is inserted into the lumen of the probe. Chromogastrography is performed after the main endoscopic examination, because excess dye makes visualization of the mucous membrane difficult. The solution is distributed pointwise in certain areas or everywhere, if it is necessary to clarify the state of acidity in the lumen of hollow organs. A change in color indicates the presence of pathology.
Biopsy technique
The material for research is selected using special forceps, which are located at the end of the fiberscope. The number of biopsy samples is taken at least 3-4 times in one zone. However, for a complete picture of the condition of the mucosa, the analysis is carried out in the pyloric, fundal and antral parts of the stomach in 6-8 places.
Pieces of tissue are removed at the border of healthy and pathologically altered tissues. If infiltrative forms of cancer are suspected, a deeper biopsy is performed. The patient does not feel pain during the procedure, except for discomfort due to the insertion of the device.
How is a biopsy specimen examined?
Mucosal samples obtained from biopsies are placed in a stable solution that preserves the tissue unchanged. The material is delivered to the histology laboratory, where each piece is cut into thin plates. The sections are stained and examined under a high-resolution microscope.
An important test for biopsy of the stomach and duodenum is PCR of a piece of mucous membrane to determine the DNA of the pathogen. This analysis is highly informative compared to other methods.
Biopsy techniques
In most cases, a small sample of the gastric mucosa obtained during gastroscopy is sent for pathohistological examination. Already in the laboratory, histological preparations are made from this fragment with a diameter of 3-5 mm, which are stained using various methods.
The benefits of gastroscopy with gastric biopsy are on the patient's side. This procedure is low-traumatic, minimally invasive and in some cases is not accompanied by any discomfort. However, from the point of view of a pathologist, such small gastric biopsies have a number of disadvantages:
- Often the wrong fragment is sent for examination: during gastroscopy, the stomach continues to contract and the endoscopist needs to try to “catch” the area of the mucous membrane that interests him;
- It is quite difficult to detach a polyp or a section of mucous membrane without damaging the tissue;
- The vast majority of biopsy samples are sent crumpled and even crushed, which increases the risk of diagnostic error;
- Due to the small size of the biomaterial, it is impossible to accurately determine the histological type of the tumor and the extent of its spread if cancer cells are found in the sample.
Stomach cancer
The main indication for histology is suspicion of a tumor process. Most often, organ neoplasms are malignant in nature, prone to rapid metastasis. Therefore, detecting pathology in the early stages is the main task of a specialist. With other types of research, it is difficult to determine the type of cancer.
If a gastric biopsy is performed, interpretation of the results gives maximum accuracy of the type of metaplasia and the degree of tissue differentiation. This allows timely treatment to begin, which leads to good remission and survival rates.
Types of biopsies
Modern surgery has many options for endoscopic biopsies. With fibrogastroduodenoscopy, the specialist has the opportunity to take samples not only from the stomach - the duodenum is additionally examined, which means it is possible to take scrapings of its walls. In some cases, a partial puncture of the pancreas is taken. The study is carried out under mandatory further ultrasound control, since pancreatic tissue is restored slowly and is most susceptible to transformation into oncology.
Biopsy of stomach tissue
Colonoscopy allows you to take additional examination of the mucous layer of the colon and rectum.
An important place is occupied by the timely detection of liver cancer, as the worst complication after hepatitis or cirrhosis.
Complications during gastrobiopsy
Careful preparation of the patient for the examination reduces the risk of complications. Sometimes unexpected situations happen.
Possible complications of gastric biopsy (rare in practice):
- acute bleeding from the sites where material was taken for gastric biopsy;
- perforation of a hollow organ;
- allergic reactions to the administration of anesthetic;
- damage to teeth.
Long-term complications after biopsy
Compliance with the rules for performing a biopsy minimizes the development of long-term complications. Most often, their occurrence is facilitated by concomitant pathology, anatomical and physiological characteristics of organs, and the degree of immune protection.
Adverse consequences include:
- systemic inflammatory response syndrome;
- inflammatory lesions of the proximal parts of the digestive tract, oral cavity;
- aspiration pneumonia;
- bleeding from an injured vessel.
Possible consequences of a biopsy
For several days after gastroscopy with histological examination, the patient may experience discomfort.
Does the stomach suffer when taking material?
Most often, the consequences of a gastric biopsy are heaviness in the abdomen, pain when swallowing and while eating, and the presence of black stool. Over the course of 3 days, moderately expressed unpleasant symptoms are not pathological and go away on their own after a few days. The mucous membranes of the organ are restored quickly due to their high reparative properties.
Carefully! If pain or bleeding worsens, you should consult a doctor immediately.
Is it possible to eat after FGDS?
Nowadays, the question of whether it is possible to eat after FGDS, and what kind of procedure it is, is especially relevant.
Fibrogastroduodenoscopy is, of course, not the most pleasant procedure, but in many cases it is simply necessary. Using fibrogastroduodenoscopy, the doctor examines the esophagus, stomach and duodenum, and takes the necessary tests. This is done for the purpose of conducting an examination and identifying diseases of the gastrointestinal tract. The patient can find out the exact cause of pain, burning, etc. It is recommended to undergo such an examination at least once a year. Before the examination, the patient is usually warned, or he learns on his own, that special preparation will be required. It consists in the fact that you cannot eat or drink in the evening. And on the day of the study, the stomach should be completely empty. But what about after? Nobody talks about this.
Recommended Diet
Already half an hour after fibrogastroduodenoscopy, the patient is allowed to eat and drink.
Someone may not want to eat food after FGDS, because unpleasant sensations may arise in the throat: pain, burning, discomfort. Of course, it is advisable to first have a light snack, for example, oatmeal porridge, fruit or low-fat yogurt, kefir. Since the stomach has not received food for a long time, you should not overload it. It is better to leave smoked meats, sausages, canned food and other similar products for later. You can drink almost any liquid except alcohol.
Some people ignore the rules and start eating immediately after the test, without subsequently experiencing any negative consequences. It's all about the individual structural features of each person's body. You can consult with the doctor who performed the fibrogastroduodenoscopy on what to eat and what not. He will tell you how to do the right thing, when to have your first snack, and what it should consist of. In most cases, those who are concerned about their health do just that. This allows you to avoid various negative consequences and feel calm.
After the study has been completed, you cannot remain completely hungry. The stomach may begin to get used to doing without food, and this is very bad. It’s not worth worrying and waiting for the moment when you can definitely eat, and constantly delaying this moment. It is better, as already noted, to consult a doctor with a question that is causing concern and get an answer.
Even if the doctor forbids you to eat for the first few hours after the test, he will also tell you that you need to do it in the evening. But in this case there is no need to starve. Among the patients there are those who go hungry and then go back to the clinic for treatment.
Conclusion
So, you can eat after FGDS, but each person has his own rules that relate to the duration of the period of time and the choice of products. To determine them for yourself, you need to consult a gastroenterologist. According to generally accepted rules, the first meal is after 30 minutes, and it should be light so as not to overload the stomach. You can drink it right away.
A person who has never encountered this procedure, of course, asks many questions. But to answer at least 1 of them, it is enough to follow all the above recommendations. If you do this once, in the future there will be no doubt as to whether you can eat after the examination. Perhaps someone who has done this will even be able to advise someone else who needs this information to do the same.
What are the recommendations after endoscopy with biopsy?
In most cases, patients tolerate the procedure well. Therefore, a gentle regime after the examination must be observed for 24 hours. After the biopsy, experts give the following recommendations:
- it is advisable to remain in a lying position for a while;
- do not eat for 2 hours;
- after a restrictive pause in nutrition, fresh warm dishes of a soft structure are allowed to reduce the irritating effect on the gastric mucosa;
- for 12 hours after anesthesia and sedatives, do not perform activities related to concentration - driving a car;
- You can drink boiled water in small sips.
Nutrition after gastric biopsy
People often ask when can they eat their usual food? A diet after a gastric biopsy is prescribed for 3 days, given the traumatic nature of the procedure. Avoid spicy, salty, sour foods that stimulate the production of hydrochloric acid. You can eat neutral-tasting foods. It is better to steam or boil. Dishes should not be hot or too cold. You should not drink alcohol or other irritating drinks after a gastric biopsy.
Nutritional Features
After the procedure, an unpleasant sensation occurs in the throat. A burning sensation and discomfort may also appear. Therefore, you should not immediately eat hard foods. It is best to eat something soft after gastroscopy (mashed potatoes, jelly, soup, fermented milk products). The first meal should be no earlier than four hours after the procedure with a biopsy, without it - no earlier than an hour. You should also not drink after FGDS. This is due to the fact that in order to reduce gag and cough reflexes, the patient’s throat is treated with lidocaine spray before the procedure. This local anesthetic blocks important reflexes, and if you do not wait time, you may end up choking on liquid food.
After FGDS of the stomach, it is recommended to eat only light, soft foods. It could be:
You can drink any liquids except those containing alcohol.
It is strictly forbidden to eat or drink immediately after the FGDS procedure. After the procedure, it should be about an hour before the patient drinks any liquid or eats a snack.
After the procedure, the doctor determines the period during which it is necessary to follow a diet.
What does a pathologist look for when examining a biopsy specimen?
The resulting biopsy sections are carefully examined by a histologist or pathologist.
What does a gastric biopsy show?
The study allows us to answer many questions and draw conclusions in several directions. The specialist first makes a macroscopic description of the drug. First of all, the presence of a pathogenic pathogen is clarified by a direct method and with the help of additional diagnostics. Deciphering a gastric biopsy includes in-depth tissue analysis, which helps determine:
- cellular composition;
- degree of cell differentiation;
- pathological proliferative process or atrophy;
- inflammatory elements;
- villus height and crypt depth;
- presence of Helicobacter pylori.
Possible complications
A correctly performed biopsy, taking into account all indications and contraindications, does not cause complications. However, the patient may have latent conditions that give undesirable consequences during the procedure:
- Bleeding from a destroyed vessel or due to incoagulability of blood.
- Perforation of the stomach wall at the site of the ulcer.
- Collapse.
- Pain after removing the endoscope.
- Anaphylactic shock due to allergy to lidocaine.
Despite its apparent complexity, gastric biopsy is a fairly safe research technique. If there is doubt about the diagnosis, a biopsy is of great help to the specialist and helps prevent serious illnesses.
The main signs of malignant cell atypia
Any tumor is distinguished by autonomous growth, polymorphism and cell atypia. The latter option is characterized by changes in the structural elements of the epithelium with impaired differentiation.
The degree of pathological cell proliferation determines the type of malignancy and treatment tactics. Tumors with high differentiation are considered the most favorable option for prognosis. Medium and low degrees of differentiation indicate the aggressive nature of the cancer. The description includes all parameters and characteristics of pathological changes.
How is it carried out?
Typically, the study is performed after pre-treating the oropharynx with an anesthetic. If the patient does not want to experience rather unpleasant sensations, the examination can be performed under general anesthesia, without hospitalization. The duration of such medicinal sleep is strictly controlled; it lasts for the duration of the study, for which a few minutes are enough.
The awakening process is not accompanied by any unpleasant sensations at all. The patient clamps the mouthpiece in the mouth between the teeth, and the endoscope itself is subsequently inserted through it. The subject will be asked to relax the throat muscles and then perform a swallowing movement. It is at this point that the specialist will insert a probe into the esophagus. Then, a little air is pumped into the esophagus through the device, allowing the internal cavity of the gastrointestinal tract to straighten.
Additional modern research
It is difficult to replace a gastric biopsy with other studies. However, if there are contraindications for invasive diagnostics, other diagnostic measures are resorted to (Table 2).
Table 2. Methods for examining the stomach
| Types of stomach examination | The essence of the methods |
| Capsule endoscopy | Obtaining video and photographic images of the digestive tract as the capsule moves through the gastrointestinal tract |
| Performing sections of organs in various planes using x-ray irradiation. Determine the presence of a tumor and distant metastases | |
| MRI | Layer-by-layer examination of the stomach and intestines using nuclear magnetic resonance to verify the degree of the malignant process and confirm the presence of metastatic foci |
| Ultrasound | Identification of additional formations and defects, carrying out functional tests |
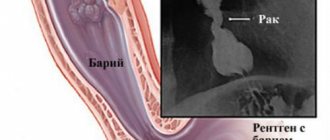
| Barium X-ray | Obtaining images of the contrasted stomach and intestines, where indirect signs of pathology can be observed |
Before and after biopsy
A biopsy is not a pleasant procedure, but its information content is significantly superior to non-invasive examination methods. The procedure for preparing for research is no less important.
- A week before the examination, it is necessary to stop consuming alcohol and foods containing hot seasonings and spices, as they, by slightly burning the mucous membrane, can distort the true picture of its health.
- During a pancreatic biopsy, it is recommended to reduce or avoid the consumption of various sugars, since the delicate tissue of the gland becomes fragile when loaded with glucose and is susceptible to injury.
- If we are talking about taking material from the intestinal walls, you will need to think through the diet so that 4-5 days before the study there is as little gas formation as possible.
- Immediately before the procedure, a cleansing enema is performed so that excess feces do not interfere with the examination and do not serve as an additional source of infection.
- Stop eating completely 14 hours before the test.
- In the morning before the puncture, you should not drink (including water), brush your teeth or use chewing gum.
Behavior after the study:
- Upon completion of the procedure, it is recommended to stay in the hospital for at least 4 hours under the supervision of a doctor.
- It is not recommended to eat food for at least 3-4 hours.
- Any sudden pain, dizziness or nausea should be reported to your doctor immediately.
- It is advisable to return home accompanied by an adult.
Treatment of the disease depending on the results of the examination
The conclusion obtained from a histological examination of gastric biopsy material allows us to prescribe primary therapy, as well as evaluate the result of treatment. If Helicobacter pylori infection is detected in a stomach ulcer, esophagitis or chronic gastritis, an eradication treatment regimen is prescribed.
Detecting a tumor of the stomach or other parts of the digestive tract requires a complex approach that includes surgery, radiation therapy and chemotherapy. The choice of method of care for malignant neoplasms is determined by the type of oncological pathology, the degree of cell differentiation, the condition and age of the patient.
Contraindications
Contraindications to the procedure relate largely not to the biopsy itself, but to the method of access to the stomach cavity - gastroscopy.
Endoscopic examination is not performed in the following situations:
- Stenosis of the esophageal lumen - adhesions or scars.
- Spasm of the cardiac part of the stomach.
- Acute processes – cardiovascular and pulmonary pathology.
- Blood clotting disorder.
- General inflammatory processes with a rise in body temperature.
- Impaired mental state of the patient.
Why is a biopsy performed?
The study of mucous tissue is required when other instrumental or laboratory studies do not provide the necessary data. When performing gastroscopy or radiography, it is impossible to obtain a comprehensive picture of the disease and establish the type of tumor.
In case of a peptic ulcer, the patient is always recommended to undergo a gastric biopsy, since an ulcer can cause mutations in cells and provoke a tumor. If a stomach ulcer develops for a long enough time, then its clinical picture is similar to the manifestations characteristic of a malignant tumor, and the procedure helps the doctor find out how much the disease has progressed and whether it has transformed into cancer.