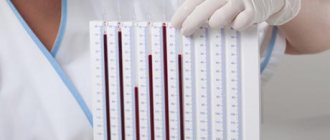
How are platelets counted?
The number of platelets in the blood is determined by laboratory analysis. Doctors consider it one of the most important studies.
What do they mean
Platelets are nuclear-free blood cells. They have a rounded lamellar shape and are responsible for the timely stop of bleeding. The number of platelets in the blood is normalized; an excess or decrease in their content leads to pathological, life-threatening conditions.
Functions of platelets:
- thrombosis of the damaged area to stop bleeding;
- transfer of bioactive compounds, immune complexes and coagulation factors.
While some platelets are being destroyed, others, new ones, are already entering the bloodstream. Blood elements are constantly renewed. However, their concentration remains approximately the same.
On a note! Platelets are formed in the bone marrow. They live in the bloodstream for up to ten days. They are then sent to the spleen, where they are broken down.
Counting options
Clinics use various methods for determining the number of platelets in the blood volume. Each option has its advantages and disadvantages. The platelet count is measured in units per 1 l/ml/µl.
There are two ways to count:
- Manual. A capillary blood smear is examined using a microscope, counting the number of platelets. The result is substituted into a special formula which is used to convert from 1 µl to 1 liter of blood.
- Semi-automatic. Platelets are counted using an analyzer. Any blood, capillary or venous, is suitable. After adding a thinning agent to the blood to prevent clotting, they bring it to the analyzer. The device takes exactly 1 ml for analysis. It determines the platelet count and issues a form with the results.
The manual method allows you to not only count the number of platelets, but also the parameters of blood cells. During the study, their size, shape and pathologies are determined. The disadvantage of the manual method is the risk of errors. You can make mistakes in calculations and make an erroneous diagnosis. Research using an analyzer is more accurate, but the device does not allow determining the parameters and pathologies of cells.
The best option for platelet analysis:
- first examine the blood manually;
- then test the smear on the analyzer.
- compare the results and draw conclusions.
The number of platelets in 1 μl of blood (PLT) is not the only parameter determined during the study. Parameters determined in parallel to PLT calculation:
- Mpv. Characterizes the average volume of blood cells and the degree of their maturity. An increased index indicates the likelihood of anemia, diabetes, cancer, and inflammation. Decreased - about diseases of the kidneys, liver, thyroid gland.
- Pdw is an indicator of cell size heterogeneity. Deviation indicates a risk of anemia, vitamin deficiency, and nervous system problems.
- Pct is the proportion of platelets in the total blood volume. Deviation warns of pathologies.
Where is blood taken from:
- finger;
- vein;
- heel (this option is good for newborns).
Indications for analysis
The platelet count is monitored from birth. The first time blood is taken in the first three days, then - 1-2 times a year.
The study is prescribed:
- According to plan. The absence of specific complaints is not a reason to refuse analysis.
- Unscheduled. Children with increased bleeding are referred for analysis.
Symptoms for which a child is referred for analysis:
- gums bleed;
- the bleeding does not stop for a long time;
- many bruises of unknown nature;
- fast fatiguability;
- pain in the legs and other ailments.
On a note! Platelet monitoring allows us to identify diseases such as leukemia, anemia, spleen pathology and much more.
Preparing for analysis
The analysis may be incorrect, not only due to errors and human factors. The result is influenced by the patient's condition. To get the most correct result, it is necessary to properly prepare the child for blood sampling.
Rules for conducting analyzes:
- To ensure that the resulting figure is objective, the study is carried out no later than 2 hours after blood collection. For children under 7 years of age, the interval between eating and taking the test should be at least 8 hours; for children over 7 years of age – 12 hours.
- The child is not fed before the procedure. Delivery is made in the morning on an empty stomach. When collecting blood from infants, maintain an interval of 2 hours between feeding and blood donation.
- The child should be in a calm state. There should be no increased loads the day before. You can’t be nervous, run, jump, or show emotions violently.
- Hypothermia is not allowed. Your baby should be dressed according to the season.
- If you enter the laboratory from the street, you need to sit in the corridor for 10 minutes.
- If you take any medications during treatment, you must notify your doctor. Taking medications may affect test results.
Factors of influence
Platelet levels change rapidly due to a variety of influences. But there are factors that can cause abnormalities in platelets in the blood of children.
Influencing factors:
- The platelet count in children under one year of age depends on their age. Infants have the most blood cells. Then their number gradually decreases to a certain limit.
- Diseases and medicines. Diseases and acute conditions can significantly affect the result.
- Exercise causes an increase in platelets in a child. This is a common phenomenon and not a pathology.
- Nutrition usually does not affect platelet levels in infants, since it is selected specifically for a small child. But in children 3-10 years old, a significant deviation of platelets in the blood from the norm may be observed when consuming certain foods.
- During the day, the platelet level, both in infants and older children, varies in the range of 9-11%.
Complications
Possible complications include:
- bleeding into the abdominal cavity;
- bleeding in the brain;
- severe blood loss due to minor injury;
- hemorrhage in the eyes, namely in the retina, which leads to loss of vision.
If a child experiences bleeding that cannot be stopped for more than five minutes, or severe pain in the head occurs, bruising appears on the body, stool turns black, or urine turns red, then you should immediately call an ambulance.
Platelet norms
Normal platelet levels in children vary with age. How the number of blood cells changes with age is shown in the table.
Platelet standards:
| Number of years | Minimum PLT, thousand units/µl | Maximum PLT, thousand units/µl |
| up to 1 | 170 | 420 |
| 1-2 | 170 | 390 |
| from 3 | 165 | 360 |
| from 5 | 165 | 375 |
| from 6 | 160 | 380 |
| from 7 | 160 | 375 |
| 10-13 | 165 | 390 |
| 13-15 | 160 | 400 |
PLT in the first year of life:
| Age, months | Minimum PLT, thousand units/µl | Maximum PLT, thousand units/µl |
| up to 1 | 160 | 480 |
| 1-3 | 170 | 450 |
| 3-6 | 180 | 420 |
| 6-12 | 180 | 405 |
The average PLT value is from 180 to 380 units/μl. A discrepancy of 1-2 units is allowed.
Deviation from the norm
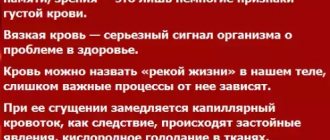
When PLT is within the normal range, the body maintains a balance between platelet production and elimination. If this indicator changes by more than 10% during the day, pathology occurs.
The PLT level depends on:
- accumulation of substances that accelerate platelet formation;
- destruction of harmful organisms;
- counteracting inflammation;
- rate of tissue repair through cellular breakdown.
If there are not enough platelets, the above functions are not performed fully. Cells, unable to withstand increased loads, disintegrate.
When there is an excess of blood cells, the functions, on the contrary, are exceeded beyond measure. As a result, blood flow deteriorates and clots form in the blood.
Thrombocytopenia
When platelets are low, children and adolescents experience thrombocytopenia. Recently, pathology has become often diagnosed in very young children.
With thrombocytopenia, the ability of blood to clot decreases, and the elasticity of blood vessels deteriorates. Pathology usually appears in winter and spring.
Thrombocytopenia may occur due to:
- anemia;
- herpes;
- flu;
- leukemia;
- intoxications;
- tuberculosis;
- infections;
- stress;
- allergies;
- liver diseases;
- hemolysis;
- folic acid deficiency;
- damage to bone marrow cells;
- malaria;
- unfavorable genetics.
Thrombocytopenia is characterized by pronounced symptoms:
- prolonged nosebleeds;
- poor blood clotting;
- formation of hematomas at the slightest touch;
- bleeding gums.
Attention! With thrombocytopenia, eating solid foods can lead to mechanical damage to the mucosa.
Thrombocytosis
Symptoms of thrombocytosis occur primarily with disorders in the bone marrow. Other causes of low platelets are nutritional deficiencies and various diseases.
PLT may be increased due to:
- infectious diseases - influenza, hepatitis, ARVI;
- allergies to medications;
- leukemia;
- iron deficiency;
- spleen diseases;
- primary thrombosis.
At the initial stage of the pathology, no symptoms are observed. Severe symptoms of thrombocytosis appear in later stages.
Symptoms of thrombocytosis:
- enlarged spleen;
- urinary disturbance;
- hematomas;
- bleeding gums;
- insomnia;
- apathy;
- kidney problems;
- redness and itching of the skin;
- dizziness.
How to increase platelets
It happens that a pathological deviation goes away on its own. This can happen due to stress or an allergic reaction. But usually, in order to achieve results, you must first eliminate the cause that caused the decrease in platelet levels.
Raising PLT levels should be under the supervision of a physician. In parallel with drug therapy, traditional methods and diet are used.
Nutrition
It is recommended to adhere to dietary nutrition. The diet must be adjusted by excluding some foods and adding others.
When PLT is reduced, it is recommended to feed children following the following rules:
- do not eat spicy and salty foods, as well as dishes with vinegar;
- increase consumption of apples and citrus fruits;
- eat foods high in folic acid - lentils, legumes, lettuce, spinach, turnips;
- eat more fresh berries;
- eat a lot of fish and liver;
- eat nuts, especially almonds.
If PLT is low, children should not be fed:
- sauerkraut;
- chocolate products;
- salted vegetables;
- sour berries;
- sea cabbage;
- cucumbers and tomatoes;
- watermelons.
Hot spices and ginger should also be excluded from the diet.
Healthy foods:
- buckwheat and oatmeal;
- cabbage;
- corn;
- nuts;
- fish;
- apples;
- liver;
- rose hip;
- greenery.
It is also recommended to take the following medications:
- folic acid;
- corticosteroids;
- immunoglobulins;
- vitamins A, C, B and D.
Doctors also advise:
- protect your child from tobacco smoke if someone smokes in the house;
- do not give useless and harmful food;
- reduce physical activity;
- avoid injury.
In critical cases, surgical intervention is resorted to. The problem can be solved by removing the spleen. A platelet transfusion may also be given.
Traditional methods
You can increase platelets using traditional methods. They are safe and can be used after consultation with a doctor. The main thing is that there is no allergy to any component.
Traditional recipes:
- Nettle drink. Add 1 tsp. nettle juice into milk. Stir and drink once a day. The course is 5-6 weeks. Collect nettles for treatment in May-June. Dry and grind to obtain dry raw material. Subsequently, it can be used throughout the year.
- Verbena infusion. 1 tsp. dry raw materials, pour 250 ml of boiling water. Leave for 3-4 hours. The infusion is drunk throughout the day. Course – 1 month.
- Beet juice. Grate fresh beets on a fine grater. Add 2 tbsp. l. sugar, stir and leave for a day. Strain the juice and drink 1/2 glass before meals.
- Honey-citrus mixture. Grate the lemon and mix with 250 g of honey. Add 2 tbsp. l. sesame Take 2 times a day, 1 tsp. Course – 1 month.
- Sesame oil. It is recommended to consume it 1 tsp. before eating. 3 spoons per day are enough.
Causes of thrombocytopenia
Short-term thrombocytopenia may occur due to:
- monthly bleeding;
- pregnancy;
- vitamin deficiency;
- taking antidepressants, hormones and antibiotics);
- alcohol and chemical poisoning;
- surgical intervention;
- severe injuries;
- abuse of garlic, onions, cherries, lemon and ginger;
- vitamin B12 deficiency.
B12 deficiency
Severe platelet deviation occurs when:
- tuberculosis;
- leukemia;
- hepatitis;
- HIV;
- aplastic anemia;
- liver cirrhosis;
- rheumatoid arthritis;
- herpes;
- heart failure;
- mononucleosis;
- measles;
- allergies;
- ARVI and acute respiratory infections;
- DIC syndrome.
Herpes
How to lower platelets
Before proceeding with platelet correction, it is necessary to assess the degree of discrepancy between the obtained result and the norm. Often the slight difference is due to the individual characteristics of the child’s body.
Diet correction
The most common cause of thrombocytosis is vitamin deficiency due to an unbalanced diet. Proper nutrition helps return platelets to normal.
For elevated PLT it is recommended:
- Consult your doctor about taking products containing acetylsalicylic acid (blood thinner).
- Give your child blueberry fruit drinks and compotes, cranberry and lingonberry drinks.
- Keep iodine under control. Give seafood and sea fish.
- Give cocoa on an empty stomach. Sugar and milk are not added to the drink.
- Flaxseed and olive oil should be included in the diet.
- Maintain drinking regime. The norm is 1 liter of clean water per day.
- Ensure increased consumption of fruits and vegetables.
What is prohibited for thrombocytosis:
- grenades;
- mango;
- rose hip;
- cabbage;
- walnuts;
- bananas.
Beetroot dishes must be included in a child’s diet. It is necessary to give seafood more often - shrimp, mussels, crabs. Beetroot salads with the addition of lemon juice, ginger and garlic are healthy. You need to rely heavily on dairy products. Tomatoes are especially useful among vegetables, and lingonberries and cranberries among berries.
Recommended:
- drink cytostatics - drugs that slow down the rate of formation of blood platelets;
- anticoagulants and antiplatelet agents - thin the blood;
- thrombocytopheresis is a procedure for isolating platelet mass from donor blood.
Attention! If you have digestive problems, adding garlic and ginger root to your food is prohibited.
Traditional treatment
If the increase in PLT is not critical, and the doctor has not prescribed medications, you can use traditional methods. With their help, you can gently lower platelets to normal without side effects.
PLT reduction:
- Grate 100 g of onion and garlic, add 200 g of honey and 50 g of lemon. There is 1 tsp. 3 times a day.
- Brew 1 tbsp. l. hop fruits in 1 glass of boiling water. The decoction is drunk in the morning.
- Grind the ginger and mix 1:1 with cane sugar. 2 tbsp. l. pour boiling water over the mixture. Drink the mixture in small sips before lunch.
- Brew Ginko Biloba leaves. Leave in boiling water for 10 minutes. You need to drink the infusion 2 times a day. The leaves are sold at any pharmacy.
Secondary thrombocytosis
In the case of secondary thrombocytosis, the increase in the number of blood cells is not so pronounced. In rare cases, a value of over a million is recorded in 1 μl, while the function and morphology of platelets are not impaired. Secondary thrombocytosis can have different development mechanisms:
- After removal of the spleen, old blood cells (or obsolete ones) do not have time to be destroyed, and new ones are formed in the same volumes. In addition, the spleen produces antiplatelet antibodies (a humoral factor that is designed to reduce production).
- Thrombocrit increases during the inflammatory process.
- Biologically active substances that have a stimulating effect on the formation of blood platelets increase in malignant tumor diseases.
- An increased platelet count is observed with frequent repeated blood loss.