General blood tests
10/25/201801/25/2019 Chernenko A. L. 1183 Views general tests, platelets
The level of platelets in the blood is assessed by performing a CBC (general blood tests). In order to determine the platelet level, venous blood is used (to obtain the most accurate results). However, taking blood from a finger is also allowed.
The level of platelets in the blood makes it possible to assess the state of the hemostatic system, determine the risk of bleeding or thrombosis, assess the effectiveness of anticoagulant treatment, etc.
An increased level of platelets can be observed against the background of temporary functional thrombocytosis, anemia of various origins, oncological pathologies, acute blood loss, erythremia, etc.
- 1 What do platelets show in a blood test?
- 2 Platelets - the norm for women by age and a table of their permissible concentrations
- 3 Normal platelets in men - table of values by age
- 4 When is a platelet level test prescribed?
- 5 How is a blood test for platelets and coagulation performed?
- 6 When can platelet levels in the blood increase?
- 7 When can a decrease in the number of platelets in the blood occur?
- 8 Treatment if low or high platelet levels are detected
Low levels of platelet cells may indicate that the patient has congenital thrombocytopenia, paroxysmal nocturnal hemoglobinuria, autoimmune pathologies, congestive heart failure, renal vein thrombosis, thrombocytopenia associated with infectious diseases, thrombocytopenic purpura, etc.
Normally, the platelet count in the blood may change slightly during the day. Also, in women, the normal platelet count may vary depending on the phase of the menstrual cycle and trimester of pregnancy.
What are they and their importance in the body?
Platelets are small (up to 4 μm), anucleate, round, colorless blood cells. They are 3 times smaller than red blood cells and are formed mainly in the red bone marrow from megakaryocytes. Instead of a nucleus, they have up to 200 granules of various structures.
Upon contact with a surface other than the endothelium, platelets develop about 10 processes that are several times their size.
These branches are important for stopping bleeding. The lifespan of platelets is about 4-7 days. Their destruction occurs mainly in the spleen and partially in the liver. The normal number of platelets is 180-320 thousand in 1 μl. When their number increases, thrombocytosis occurs, and when their number decreases, thrombocytopenia occurs.
The platelet count may fluctuate. Their number increases during intense physical activity, during stress, and during pain. Thrombocytopenia is a sign of some pathology. The main purpose of platelets is to participate in the process of hemostasis.
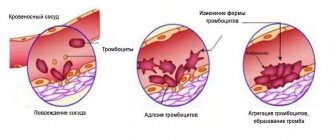
If the integrity of the vessel wall is violated, in order to stop bleeding, it is necessary to form a kind of “plug” that covers this damage. The main blood components involved in this process are platelets and fibrinogen.
When they interact, a platelet “plug” is formed, and the bleeding stops. Damage also causes vasospasm, which leads to a decrease in blood flow. Platelets first adhere to the subendothelium at the site of injury, and then their aggregation occurs.
The formation of a fibrin network, which stabilizes the “plug” and stops bleeding, occurs during the blood clotting reaction. It involves various plasma components, including platelets. The resulting clot dissolves at the last stage of hemostasis, when final healing of the wound occurs.
Platelets also protect the body from foreign agents. They have phagocytic properties and are capable of destroying the membranes of various bacteria. Peptide elements contained in platelets are released into the blood during injury and protect the body from microbes.
General information
Platelets are non-nuclear components of blood that have an oval shape. The approximate size of platelets is 0.002 to 0.006 mm. The unique structure of platelets allows them to change shape. In a passive state, they have a disc-shaped shape, but when activated, they become rounded, and growths form on their surface.
The average lifespan of platelets is about 10 days. This is a fairly short period of time, which is why active formation of platelets constantly occurs to replace used ones. Platelet destruction occurs in liver cells or kidneys, which are a kind of filter for human blood.
With age, platelets are formed more and more slowly, which is associated with the gradual depletion of the body and a number of other factors. The bone marrow is the site of platelet production. The formation process takes place in hollow bones, for example, in the vertebrae, pelvic bone, and ribs.
The bone marrow produces stem cells, which initially do not perform any functions and are not divided into types. Subsequently, under the influence of certain organic substances, plaques are produced from each stem cell. They move freely through the bloodstream and, if there is no need for active functioning, are stored in the spleen.
If any pathological process occurs in the human body, under the influence of adrenaline, blood cells leave the spleen and move to the site of the lesion.
In general, platelets are the most numerous components of the blood and play a vital role in the body. To determine what platelets are needed for, it is necessary to become familiar with their functions in detail.
Normal platelet count in women - table
The normal platelet count (PLT) is 180-320 thousand in 1 μl. Depending on the age and characteristics of the woman’s body, this level may vary. In newborns, the figure is 100-420 thousand in 1 μl. In children over one year old - from 180 to 320 thousand in 1 μl. The largest number of platelets is in adolescence; in girls aged 15 there are up to 340/350 thousand per 1 micron.
Platelets are the norm in women by age (table):
Table of normal platelet counts in women by age.
During menstruation, the figure can drop to 150 thousand per 1 μl. During this period, blood clotting is reduced to ensure complete rejection of the endometrium in the uterus. In pregnant women, the platelet count drops to 150 thousand in 1 μl.
During this period, there is an increased blood flow to the fetus, and the woman’s body does not have time to produce new cells in sufficient quantities. After childbirth, platelet levels recover on their own. If the platelet level is less than 140 thousand per 1 μl, then pregnant women may experience bleeding during childbirth.
Table of average platelet values in women in the normal range, determined by age:
The platelet count may change throughout the day. At night the figure is slightly lower than during the day. The level also varies depending on the time of year. The fewest platelets are in the spring.
Causes and types of thrombocytopenia
A deficiency of the smallest blood cells always means an increased risk of bleeding for the patient. The condition indicates an imbalance in the formation and destruction of cells. There are congenital conditions accompanied by insufficient platelet synthesis. If they are produced in small quantities, they speak of true thrombocytopenia. When the deficiency is temporary, caused by disturbances in the functioning of internal organs, the condition is called secondary. If the deficiency is temporary and can resolve itself (for example, heparin-induced thrombocytopenia, or caused by a lack of vitamins in the body), it is called transient. Based on the level of cells in the blood, the degrees of their deficiency are distinguished:
- light;
- average;
- heavy.
Depending on the pathogenesis, there are several types of thrombocytopenia.
Hereditary
These include thrombocytopenia caused by gene mutations and disorders of their structure. These are rare diseases and syndromes acquired from close relatives:
- Mey-Hegglin is a hereditary pathology in which the process of platelet separation is disrupted (they are formed in smaller numbers, but are larger in size), and in parallel the production of leukocytes is disrupted;
- Wiskott-Aldrich is a hereditary disease of boys, which produces platelets that are too small, which are soon destroyed in the spleen, and is combined with disturbances in the functioning of the immune system;
- Bernard-Soulier - pathology develops only in that case. if both parents are carriers of the defective gene, it produces huge, functionally incompetent platelets;
- TAR - congenital thrombocytopenia is caused by impaired development of megakaryocytes under the influence of a mutated gene, combined with the absence of radial bones.
Amegakaryocyte thrombocytopenia is also isolated. This condition is accompanied by a genetically determined lack of sensitivity of bone marrow cells to thrombopoietin. They do not respond to the hormone and therefore do not produce blood platelets.
Thrombocytopenia destruction
This is the name for conditions in which blood cells are broken down or utilized faster than they are released from the bone marrow. Thrombus-forming elements can be damaged in the spleen, and in much smaller quantities in the liver and lymph nodes. Injuries also lead to active destruction, then the formed elements are damaged directly in the vascular bed. A sharp decrease in platelet levels is observed with:
- thrombocytopenic purpura (autoimmune thrombocytopenia) - the causes of the disease are unknown, during it antibodies are produced to blood cells, due to which formed elements are intensively captured and destroyed in the spleen, liver, lymph nodes, the compensatory capabilities of the bone marrow are gradually depleted;
- Evans-Fisher syndrome - specific antigens appear on platelets and red blood cells, by which the recycling organs recognize them as foreign and destroy them; the causes of the syndrome have not been fully elucidated;
- thrombocytopenia of newborns - the condition begins to develop at the 20th week of pregnancy, if the mother’s immune system “wary” perceives the child’s genetic material, the cells destroy immunoglobulins that enter the fetus’s body through the blood-brain barrier.
Destructive thrombocytopenias include those deficiencies of blood platelets that have developed due to the use of medications. Medicinal substances are able to come into contact with blood cell antigens, they form complexes that the immune system perceives as foreign material and produces antibodies. As a result, platelets labeled with the complexes live for several hours and are quickly destroyed in the spleen. After stopping the medications, the balance of the corpuscles should be restored. Drugs that lower platelet levels in the blood include:
- antiarrhythmic (Quinidine);
- antihistamines (ranitidine, cimetidine);
- anticoagulants (Heparin);
- antibiotics (Rifampicin, Cephalexin, Gentamicin);
- antidepressants.
Antibodies can form against blood cells that have come into contact with viral particles. Thrombocytopenia destruction can be provoked by rubella, chickenpox, influenza, measles.
Productive thrombocytopenia
This is the name for conditions in which the deficiency of corpuscles is caused by their reduced production in the red bone marrow. Disturbances can be caused by pathologies of the hematopoietic system, a lack of regulators of body synthesis, and abnormalities in the structure of producing cells.
Table - Causes of productive thrombocytopenia
| State | The essence |
| Alcoholism | Ethanol has toxic properties and inhibits the functioning of most organs and systems, including hematopoietic ones. Thrombocytopenia develops against the background of prolonged and active consumption of alcohol, in “binge drinkers” |
| Irradiation | Ionizing radiation can be the result of medical treatment or living in unfavorable conditions, it causes cell mutations or directly inhibits the formation of blood cells |
| Medicines | Some drugs reduce the activity of hematopoietic function. These include diuretics, antipsychotics, anticonvulsants, antithyroid drugs, NSAIDs and cytostatics. The latter inhibit platelet formation by inhibiting cell division throughout the body |
| Hypersensitivity | Increased sensitivity to pharmacologically active substances is not included in the list of side effects, but is an individual reaction of the body to certain compounds. It can manifest as inhibition of hematopoiesis and platelet formation |
| Metastases | At the terminal stages of a tumor disease, metastases almost always appear - the tumor grows into healthy tissues and provokes their replacement with atypical ones. Often metastases form in the bone marrow, which is accompanied by a comprehensive inhibition of hematopoietic function |
| Myelofibrosis | Fibrous degeneration of bone marrow stem cells occurs, which gradually displace functional cells |
| Leukemia | Malignant damage to the hematopoietic system is accompanied by degeneration and activation of the division of atypical stem cells, with the gradual displacement of healthy bone marrow tissue. Manifested by a decrease in the level of all blood cells |
| Megaloblastic anemia | It develops against a background of folic acid and cyanocobalamin deficiency and is accompanied by impaired cell division due to the inability to recreate DNA. Primarily affects those systems whose stability depends on the activity of cell division (mucous membranes, blood composition) |
| Myelodysplastic syndrome | Blood cells are produced, but do not fully mature, therefore they cannot perform functions and quickly undergo apoptosis (destruction). The condition is accompanied by thrombocyto-, leuko- and erythropenia |
| Aplastic anemia | This is the inhibition of all hematopoietic functions of the red bone marrow, accompanied by a deficiency of all types of blood cells. The causes of development may be chemotherapy, radiation exposure, poisoning, HIV |
Thrombocytopenia consumption
Such a deficiency of blood elements is observed when the compensatory capacity of the bone marrow is depleted against the background of active consumption of platelets over a long period. Before the level of cells in the blood decreases, there is a significant increase in them. Similar conditions are observed against the background:
- Thrombocytopenic thrombotic purpura. Cells on the inner surface of blood vessels produce a special substance - prostacyclin. It regulates platelet activity and prevents their adhesion and aggregation (sticking together). The lack of this factor provokes the formation of microthrombi, vascular damage, and hemolytic processes (with the destruction of red blood cells directly in the bloodstream).
- Hemolytic-uremic syndrome. When it occurs, toxins appear in the blood (infectious or due to taking medications), which damage the vascular walls. A large number of platelets are activated to correct these defects. As a result, blood clots form and microcirculation is disrupted. The syndrome is more often observed in children against the background of intestinal infections.
- DIC syndrome (intravascular coagulation). It develops with massive damage to tissues or internal organs (burns, transfusion of incompatible blood, necrosis, tumors, chemotherapy), shock conditions, and serious infectious lesions of the body. The release of mediators causes platelets to coagulate, forming a large number of blood clots and causing serious circulatory problems. Subsequently, the supply of cells is depleted, and against the background of activation of the anticoagulant system, multiple and massive bleeding develops, which can lead to the death of the patient.
Platelet redistribution
The spleen acts not only as a recycling organ, but also as a depositing organ for blood cells. As a rule, it stores a third of all platelets in the body. If it increases in size, almost all thrombotic bodies (up to 90%) can be retained in the tissues. Because they cannot be destroyed, the bone marrow does not activate megakaryocytes to compensate for the deficiency. As a result, the level of corpuscles in the total blood volume drops sharply. Changes in the size and function of the spleen occur when:
- autopathologies (systemic lupus, rheumatic diseases - rheumatoid arthritis, rheumatism of the joints);
- oncological diseases (leukemia, lymphoma);
- liver cirrhosis;
- alcoholism;
- infectious diseases.
Redistribution of platelets can also be caused by the growth of hemangioma, a benign tumor consisting of vascular epithelium. In its tissues, bodies can also accumulate and then be destroyed. After the tumor is eliminated, the situation returns to normal.
Thrombocytopenia dilution
It is observed in hospital patients who, due to their serious condition, are given a large number of blood substitutes (for bleeding, severe infections). Even activation of the depot and proper operation of compensatory mechanisms cannot correct the situation and optimize the state of the coagulation system. For platelet production to recover, it will take time and comprehensive treatment aimed at restoring all internal organs.
Useful information: Nitrites in urine - causes, treatment. What to do with nitrituria and is the condition dangerous?
In children
Newborns and children up to six months are characterized by wider limits of platelet norms than adults. This is due to the development of the work of all internal organs. All of the above diseases can provoke a lack of corpuscles in a child.
Doctors note that the condition is common among premature babies, as well as those infants who had to undergo intensive care shortly after birth. If thrombocytopenia is not associated with pathologies of the blood, bone marrow and hereditary gene mutations, it goes away within a few months. In order to detect dangerous diseases in time, the blood picture must be regularly monitored.
In pregnant women
A decrease in platelet levels in an expectant mother is considered a natural process (up to 140*10⁹ units/l). This is the result of a restructuring of the body under the influence of hormones, increased load on internal organs, increased blood volume, and increased consumption of vitamins and minerals. If a woman does not have immune disorders, allergies, signs of intoxication or warning symptoms, no specific treatment is required. The doctor recommends that mom eat right, get plenty of rest, and avoid taking medications. After childbirth, the condition returns to normal.
In case of a sharp and significant decrease in platelet levels, inpatient monitoring is required. This may be a sign of serious illness, intrauterine fetal death. To accurately determine the cause, a comprehensive examination is carried out. If the level of cells drops to critical, the woman is treated in a hospital until the blood picture is completely normalized.
Interestingly, thrombocytopenia below 140*10⁹ units/l can only occur during pregnancy and disappear after childbirth. This is due to the peculiarities of the immune system during pregnancy.
Identification of idiopathic thrombocytopenia in a woman or a decrease in blood platelets of an autoimmune nature is an indication for delivery by cesarean section. Natural childbirth in this case sharply increases the risk of intracranial hemorrhages in the fetus of varying severity. To prevent this and preserve the child’s health, the operation is performed even if the obstetric situation is otherwise favorable.
The risk of intracerebral hemorrhage in the fetus is due to the fact that often a decrease in platelet levels in the mother is accompanied by a similar change in the level of platelets in the child. And this is a risk factor for bleeding. It is impossible to determine platelet values in utero in a child without umbilical cord puncture, and this procedure in itself is dangerous and is performed only in a few maternity hospitals.
Indications for testing
Platelets (the norm for women by age - the table is attached) are detected using an analysis - this is a standard procedure that is prescribed to all patients. As a result of the study, deviations from acceptable values can be detected and pathology can be identified.
A general or biochemical blood test is prescribed. Based on the data obtained, it is possible to understand how the body functions and what disorders exist. A general blood test measures hemoglobin, leukocytes, red blood cells, and ESR. The platelet level is also assessed.
A general platelet test is prescribed:
- to identify inflammatory processes in the body;
- for blood diseases;
- for allergies;
- in case of a failure in the immune system;
- during pregnancy;
- with varicose veins;
- for problems with blood clotting.
Platelet counts should be checked in the following cases:
- functional liver disorders;
- suffered a heart attack or stroke;
- before treatment with anticoagulants;
- during menopause.
The study is carried out to identify violations in the work of:
- of cardio-vascular system;
- Gastrointestinal tract;
- respiratory organs;
- urinary system.
A blood test for platelets is carried out if there is a suspicion of a malignant tumor, disruption of the endocrine system, or immunological disorders. The analysis can also be done for prevention in order to detect pathological processes in the body.
How to prepare for donating blood for platelet determination
A blood test for platelet levels is taken in the morning on an empty stomach. During the day before the test, you must stop eating fatty and fried foods, alcoholic beverages, and smoking. Sweets, taking certain medications (aspirin), carbonated water, coffee or tea with sugar can change the platelet value.
Before the study, you should avoid excessive physical and emotional stress. In emergency cases, blood sampling is carried out 1-2 hours after eating.
The result of the analysis may be influenced by factors such as:
- the patient’s condition (physical fatigue, alcohol intoxication, severe stress);
- quality of reagents;
- menstruation, pregnancy, lactation.
Blood is usually collected from a finger. Some laboratories take material for examination from a vein. A better analysis is obtained from venous biomaterial.
Preparing for analysis
The reason for obtaining a distorted result may be failure to comply with the established requirements for preparation for the study. The list of preparatory measures is compiled by the doctor who issued the referral to the laboratory.
In general, this includes the following measures:
- Stop the use of certain types of physical procedures and medications for the duration of the examination, in particular drugs with a blood-thinning effect (at least 24 hours).
- Doctor's warning about pregnancy, menstruation, lactation.
- Following a special diet - avoiding fatty foods, starchy foods, fried foods, soda, alcoholic beverages, sweet tea, coffee (for 3 days). For the last meal before donating blood, it is advisable to limit yourself to lean porridge.
- Moderate fluid intake the day before blood donation.
- Normalization of the emotional background, sleep patterns, elimination of stress, physical strain, sunbathing (2-3 days).
- Submitting biomaterial strictly on an empty stomach (do not eat for at least 8 hours), it is permissible to drink 1 glass of clean water. Do not smoke (at least 30 minutes).
What tests are taken to determine platelets?
To determine the platelet count, a general study is prescribed. Blood is taken from a finger. If deviations from the norm are detected, the woman must undergo an additional study - a coagulogram analysis. In this case, blood is taken from a vein. The minimum required volume of biomaterial is 1 ml.
Coagulogram analysis is carried out:
- before surgery;
- during pregnancy (if there is a risk of premature placental abruption);
- with a tendency to form blood clots;
- to control the level of blood clotting during treatment with anticoagulants;
- in case of liver dysfunction, vascular problems, after a stroke or heart attack;
- with long-term use of hormonal medications and contraceptives;
- if extensive bleeding begins.
The main indicator of a coagulogram is the coagulation period, that is, the period of time during which a dense clot is formed that stops bleeding. For material from capillaries, this value should be from 30 seconds to 3 minutes, and for venous material – up to 10 minutes.
During the study, the prothrombin index is determined. This is a deviation in the patient's blood clotting time from the normal value. Normally the error is about 7%. Too high a reading indicates liver disease. During pregnancy, it rises for physiological reasons, which is in no way connected with any disorder.
Consequences of thrombocytopenia
Small deviations from the norm are not dangerous to human health. With timely diagnosis and treatment, patients can avoid the development of pathological consequences. However, if thrombocytopenia is ignored and there is no comprehensive treatment, sick people risk encountering the following pathologies:
- development of subcutaneous bruises with minor injuries;
- internal bleeding that poses a threat to human life;
- hemorrhage in the retina of the eye, which can result in blindness for a person;
- hemorrhagic stroke.
The patient may also experience bleeding in the brain. This is a rare, but quite dangerous phenomenon. It develops most often with serious head injuries, but can also occur spontaneously, without any bruises. Bleeding in the brain also occurs against the background of frequent nosebleeds. The prognosis in this case is unfavorable - a quarter of such cases end in the death of the sick person. The prognosis for recovery with a low platelet level depends on the characteristics of the patient’s body, his age, the duration of the disease, and the presence of auxiliary pathologies in the body.
Methods for determining platelets in blood
Platelets (the norm for women by age - table above) are determined based on a blood test. A general analysis is carried out, its result is compared with the norm, thus obtaining the desired indicator. The Fonio method is used as a basis.
Blood is taken from a finger, mixed with a reagent and examined under a microscope. The study can be carried out over the next 2 hours, but the patient usually receives the result the next day.
The Fonio analysis table includes the following values:
- PLT – quantitative composition of platelets in the body (depending on gender and age);
- MPV —mean blood cell volume;
- PDW —distribution area;
- PCT is the percentage of blood cells relative to the total blood volume.
The rate of platelets per 1 thousand red blood cells is calculated. This ratio reduces the risk of detecting pseudothrombocytosis. First, the total number of red blood cells in the smear is calculated, then the indicator is multiplied by μl of blood. The obtained value is compared with the quantitative composition of platelets.
To carry out analysis using the Fonio method, you need a 14% solution of magnesium sulfate and a 2.6% solution of sodium ethylenediaminetetraacetate. Reagents are taken using a Panchenkov capillary. A blood test performed using this method has a high level of accuracy.
Advantages of the Fonio study:
- the analysis can be performed at any time after blood collection;
- the laboratory technician sees the cells in the smear;
- simple calculation formula.
To study platelets, venous blood is taken in Goryaev’s counting chamber. Isotonic sodium chloride solution is used as reagents. A drop of blood is placed on the ground glass of the chamber. The platelet count is counted under a microscope using a phase contrast device.
What processes do platelets perform in the body?
Originating primarily in the bone marrow, these blood platelets have a circular or oval shape, and never contain a nucleus. The diameter of platelets reaches from 2 to 4 microns.
Glycoprotein complexes are located directly on the membrane , as receptors, and assist platelets in activating, establishing a spherical shape and forming pseudopodia (outgrowths of unicellular organisms used by cells for movement).
The gluing of platelets and their attachment to damaged areas of blood vessels are all the tasks of such complexes. They are attached to fibrin, after which they release thrombostenin (an enzyme), resulting in tissue compaction.
The main function of platelets is blood clotting.
Stimulating these blood cells directly also produces benefits. Components involved in blood clotting, while at the same time other useful and active substances are released.
Platelets are distributed throughout all vessels and participate in the following actions:
- Formation of blood clots, the initial thrombus that will stop the bleeding by closing the damaged area,
- Nourishes blood vessels and also narrows them if necessary,
- Processes related to the immune system,
- They also take part in the dissolution of a blood clot, this process is called fibrinolysis,
The lifespan of platelets is from 8 to 10 days; towards the end of their existence, they decrease in size and lose their shape slightly.
Note! More than 75% of bloody discharge from the nose, prolonged menstruation, subcutaneous hemorrhages and gum blood flow are attributed to pathologies of the platelet formation system.
Studies of platelet characteristics using a hematology analyzer
Laboratory studies of platelets are carried out not only using the old methods (staining and counting their number on glass), but also using a hematology analyzer. Thanks to this modern device, quantitative and qualitative blood analysis is carried out.
Using a hematology analyzer, the mean platelet volume (MPV) is determined. The equipment can show the result in the form of a histogram, where old and new cells are displayed.
The increase in MPV occurs:
- with anemia after bleeding;
- thrombocytopenic purpura;
- macrocytic thrombodystrophy.
A decrease in MPV is observed:
- with inflammation;
- pregnancy;
- iron deficiency anemia;
- tumors;
- for blood clotting disorders;
- liver and kidney pathologies;
- heart attack;
- hypercholesterolemia.
Using the analyzer, an indicator of cell heterogeneity is calculated - the degree of change in platelet size (PDW). Its deviations from the norm indicate the development of an inflammatory process, helminthic infestation, anemia, and cancer.
Decoding the results
Platelets - the norm for women by age (the table contains minimum and maximum values) - should be in the range of 180-320 × 109 units. There is no separate blood test for platelets. Its indicator is assessed when taking biomaterial for general analysis.
In addition to platelet level (PLT), thrombocrit (PCT) is measured. It shows the proportion of whole blood volume occupied by platelets. The normal thrombocrit is measured as a percentage. The acceptable rate is 0.1-0.4%.
What do the analysis values indicate:
A blood platelet test is a diagnostic test. Its goal is to identify pathology. If the platelet count is higher or lower than normal, some disease develops in the body.
If there is an imbalance between the formation of new platelets and the disposal of old ones, then the woman develops pathologies that manifest themselves in increased bleeding or, conversely, in a tendency to form blood clots. A decrease in the number of blood platelets is observed with thrombocytopenia. An increase in the number of platelets occurs with thrombocytosis.
Both of these phenomena indicate disturbances in the body and are a reason to consult a doctor.
Features of low platelets during pregnancy
During pregnancy, expectant mothers, especially after the 6th month of pregnancy, experience low platelet counts.
Factors influencing their decrease in the blood may be the following:
- Insufficient intake of vitamin B12,
- Lack of folic acid,
- Infections,
- If the hormonal balance has changed, this can lead to a decrease in the life of the plates,
- The concentration of formed elements in the blood decreases due to an increase in the amount of blood circulation,
- Autoimmune diseases.
During pregnancy, the drop in blood clotting is insignificant and within normal limits. But if you notice symptoms of a more severe fall, you should immediately consult a doctor. Also, a strong fall is fraught with large loss of blood during childbirth, which can be fatal for the mother.
Reasons for increased indicators
There are factors that influence changes in normal platelet levels. With elevated levels, the patient develops thrombocytosis. This condition increases the risk of blood clots and blood vessel blockages. This condition can lead to a heart attack or stroke.
Causes of increased platelets:
- splenectomy;
- development of the inflammatory process;
- different types of anemia;
- postoperative period;
- malignant tumor;
- erythremia;
- exercise stress.
Concept of platelets
The plates are oval or round in shape. When they reach surfaces on which there is no epithelial layer, the formation of special processes is activated. These branches are intended to stop emerging bleeding and close wounds; their length is 5-9 times greater than the size of a platelet.
The granules of the plates contain platelet enzymes that destroy bacterial membranes and protect the body from harmful microorganisms. The processes serve to accelerate movement in the bloodstream by adhering to foreign bodies; the threads capture elements and digest them. A protective barrier is created by gluing with other platelets, that is, blood clotting occurs.
An important function of platelets is to supply micronutrients to the endothelial layer. Their lifespan ranges from 7 to 12 days, then destruction occurs in the liver, lungs and spleen.
Forms of platelets in the blood:
- degenerative varieties - contained in amounts up to 0.2%;
- stereotypes of irritation - range from 0.8 to 2.3%;
- young cells - from 0 to 0.8%;
- mature forms - from 90.2 to 95%;
- old records - from 2.3 to 5.7%.
Inactivated elements are flattened spherical shapes, in which the semi-axes are located one to the other in a ratio of 2:8. This feature is used in the case of recognizing the optical characteristics of platelets and when regenerating parameters using flow cytometry.
Cell structure
Microscopic studies show that the change in cell shape upon activation is associated with transformation of the tubule ring. This phenomenon is caused by the conversion of the amount of calcium ions.
The structure of platelets is heterogeneous, there is heterogeneity, and the structure contains several layers:
- the outer surface is represented by a three-layer membrane, the thickness of which contains phospholipase A, receptors for adhesion to other elements and tissues;
- the lipid layer is a collection of glycoproteins and helps the plates stay glued together for a long time;
- microtubules in the form of a cellular framework help the structure contract to release the contents of the platelet beyond its boundaries;
- The area of organelles is represented in the structure by various components and factors that promote wound healing.
In the early periods of research, there was no photographic technique and there was no unambiguous terminology, so the time of initial observations of platelets is not precisely established. There is information that the first study was conducted by the inventor of the microscope, the Dutchman van Leeuwenhoek. In England, the cells are now called platelets, a term coined by Bizzocero in 181. He is also credited with the discovery of the relationship of elements with homeostasis and thrombocytosis. In Russian, flat blood cells are called platelets, sometimes the name Bozzocero's plaque is used.
Formation and life cycle
Their formation and maturation begins in the body of the red marrow in the area of the pelvic bones and vertebrae. The spongy substance reproduces stem cells that are incapable of the process of differentiation and are not divided into specific types.
Platelets go through several stages during formation:
- stem cells turn into elements of the megakaryocyte series;
- the formation of a megakaryoblast begins - a large formation of a mesh structure without granules, with 2-3 round nuclei;
- the resulting proplatelet turns into a promegakaryocyte and platelet formation occurs.
Transformations occur as a result of the influence of genetic factors. The lack of cells leads to an increase in the duration of bleeding; the increased volume of elements causes the formation of clots and blockage of blood vessels. As a result of blocked channels, a heart attack, stroke, pulmonary embolism, or vascular plug in other organs of the human body can occur.
Inferiority of platelets or their deficiency is called thrombocytopathy. A low overall indicator of the number of plates in the analysis causes a consequence in the form of thrombotic purpura, in which ischemia of various organs or hemolytic anemia develops, and the number of blockages in the vessels after bleeding increases.
Functions of elements
Platelets form the primary plug to tighten the wound of a damaged vessel and accelerate the plasma coagulation reaction. The peculiarity of the plates is that they play a significant role in the healing and restoration of tissues, while releasing polypeptide molecules for cell growth and division. Platelets are quickly activated when needed and enter a new, irreversible state.
The plates are transformed under the influence of pathogens:
- the main protein of connective tissue - collagen;
- the main protein of the coagulation system - thrombin;
- adenosine monophosphate produced by damaged cells - ADP;
- a second-line activator synthesized by platelets to establish vasoconstriction - thromboxane A2.
The modified flat cells attach to the damaged surface and form a plug as a result of adhesion to the walls and each other. As a result, the shape of the plates is updated, and phosphatidylserine and P-selectin are expressed.
In its normal state, the platelet membrane does not support the blood clotting procedure, while phospholipids are located on its inner layer. Activation of flat elements causes excitation of scramblase protein molecules, which transfer phospholipids to the outer shell. As a result, the concentration of phosphatidylserine in both layers is equalized. In the process, transmembrane proteins of the exogenous layer change, which accelerate coagulation through the characteristic coupling of factors.
Reasons for low performance
Platelets - the norm in women varies by age (the table will tell you) - can decrease, deviating from normal values. This condition is called thrombocytopenia. In patients, blood clotting is impaired. Any wound can lead to prolonged bleeding that is difficult to stop.
Reasons for low platelet levels:
- autoimmune pathologies of the blood system;
- hemophilia;
- acute liver damage;
- thyroid diseases;
- bone marrow diseases;
- drug-induced thrombocytopenia;
- infectious diseases;
- aplastic anemia;
- DIC syndrome;
- thrombosis.
Patients with thromocytopenia have long and heavy periods, bruises and bruises appear on the body for no reason. Wounds and cuts take too long to heal. Gums and nasal passages often bleed. Platelets may be low in premature babies.
Bone marrow diseases
Almost all bone marrow pathologies are accompanied by a decrease in platelets in the blood and impaired production of formed elements. The development of bone marrow diseases is influenced by pathogenic external factors. For example, frequent radiation, use of narcotic drugs, long-term therapy with drugs with aggressive composition. Most often, bone marrow diseases develop with long-term use of antibiotics, antidepressants, and antiulcer drugs. Additional reasons include:
- Anemia. The pathology develops against the background of a deficiency of folic acid and cyanocobalamin in a woman’s body. These elements take part in the process of cell reproduction and maturation. If they are deficient, the patient's blood clotting is impaired, which leads to the formation of thrombocytopenia. Also, with low platelets, the likelihood of leukopenia is not uncommon.
- Oncological diseases that affect the bone marrow (leukemia).
- Infectious diseases that affect the hematopoietic organs. For example, HIV, viral hepatitis, mononucleosis.
Hereditary bone marrow pathologies can also lead to thrombocytopenia. For example, the May-Hegglin anomaly. This disease is accompanied by a genetic mutation, which results in a deficiency of megakaryocytes and a decrease in the concentration of platelets in the blood.
Medications
There are many medications that help regulate the level of platelets in the blood. If an increase or decrease in the indicator is caused by some pathology, then it is necessary first of all to treat the disease due to which it deviated from the norm.
Medicines to raise platelet levels:
- hormonal agents – Prednisolone, Dexamethasone;
- to stop bleeding - Dicynon;
- natural preparation – Sodecor;
- for internal hemorrhages - Vikasol;
- for a rapid increase in platelets - Thrombopoietin;
- vitamin C.
Medicines to lower platelet levels:
- Aspirin;
- Thromboass;
- Livarudin;
- Argatoban;
- Aspecard;
- Bivalirudin.
Treatment of pathology
The fight against a problem begins with finding out the root causes that led to its occurrence. For this purpose, additional diagnostic studies are carried out. Then adequate therapy is prescribed. It includes the use of medications that can normalize the level of platelets in the blood. Typically, a person is prescribed antiplatelet drugs or anticoagulants.
Minor increases in platelet levels can be reduced with diet. Doctors recommend:
- Consume foods that irritate the blood. This is olive oil, onion, lemon, fish oil and more.
- Drink at least 2 liters of clean water per day. Green tea, vegetables, natural juice and fruits also have benefits.
- Eat garlic daily. It is capable of dissolving even already formed blood clots.
There are also products that can increase blood viscosity. The list includes:
- chokeberry;
- pomegranate;
- protein and fatty foods;
- bananas;
- baking
Smoking and alcohol, as well as some medications, have a similar effect. Thus, diuretics and contraceptives can increase blood viscosity. For any deviations in platelet levels from normal, it is recommended to minimize physical and emotional stress.
Platelet count is reduced
A decrease in platelet count causes thrombocytopenia. This causes blood clotting disorders. Bleeding is quite difficult to stop. Even small wounds take a long time to bleed. There is a violation of the elasticity of the walls of blood vessels. Their fragility increases. All this can cause internal bleeding.
A decrease in platelet levels can be suspected if a woman experiences frequent nosebleeds and bruises easily appear on her body. Menstruation lasts for quite a long time. At the same time, the discharge is abundant. Bleeding gums occur. Small cell rashes may be present on the body. Cuts and wounds bleed for a long time and do not heal.
There are many reasons that can lead to a decrease in platelet levels. The condition can be provoked by:
- allergies to medications;
- deficiency anemia caused by a lack of folic acid or a lack of vitamin B12;
- entry of antiplatelet bodies into the fetus through the placenta of a sick mother;
- thyroid diseases;
- infectious diseases;
- intoxication of the body;
- production of antiplatelet bodies by the body.
Low platelet levels may be a consequence of chemotherapy or uncontrolled use of strong antibiotics and antiplatelet agents. A number of diseases can also provoke a decrease in the indicator, the list of which includes:
- measles;
- leukemia or other cancers of the bone marrow;
- cirrhosis of the liver;
- rubella;
- hepatitis.
How to increase platelet levels in the blood?
If the number of platelets in a woman’s blood is low after 50 years, the first step will be to look for the root cause of the problem. Then therapy will be prescribed aimed at treating the pathology. Additionally, medications can be used to maintain the platelet count at the proper level. In severe situations, glucocorticosteroid hormones, platelet transfusions, immunoglobulin injections, or anti-Rhesus serum are prescribed.
Additionally, you must follow a diet. The list of foods that have a positive effect on platelet levels in the blood includes:
- mushrooms;
- buckwheat porridge;
- pumpkin seeds;
- rabbit meat;
- peaches;
- apples;
- carrot;
- bananas;
- calf liver;
- egg yolks;
- raspberries;
- beet;
- potato.
Diet
You can increase or decrease your platelet levels with diet. To do this, you need to eat healthy foods and avoid harmful ones. Medical nutrition can only be used as an auxiliary therapy. The main treatment should be medication.
Diet to increase platelet levels:
- red meat;
- buckwheat;
- river/sea fish;
- eggs;
- cheese;
- beef liver;
- meat broths;
- pates;
- salads from cabbage, beets, carrots, bell peppers, nettles with sesame oil;
- bananas;
- parsley dill;
- rowan berries;
- green varieties of apples.
If thrombocytopenia occurs, you should avoid olive oil, raspberries, and ginger. These products thin the blood. It is not recommended to drink wine and other alcoholic beverages. You should reduce your coffee consumption.
Diet to lower platelet levels:
- seafood;
- consumption of large quantities of water;
- green tea;
- olive and linseed oil;
- grapes, citrus fruits, blueberries, cherries, cranberries, lingonberries;
- cocoa;
- ginger;
- celery;
- onion;
- garlic.
If platelet counts are elevated, you need to eat more fresh fruits and vegetables. You should avoid fatty and fried foods. It is advisable to eat less protein foods.
How to normalize platelet levels
A deviation from the norm is a consequence of a woman’s disease. You should fight not with the number of blood platelets, but with the cause of changes in their content in the blood. Therefore, the primary task of the doctor is to establish what was the impetus for the shift in this indicator. The possibility of influence of physiological factors and environmental parameters should be considered.
An accurate diagnosis is made based on all available information taken together; the results of a single blood test are not enough. The following are taken into account: anamnesis, features of the clinical picture, data obtained during the use of laboratory and instrumental diagnostic methods. The optimal treatment regimen is developed after the final diagnosis has been established.
Drug therapy
Medicines for the treatment of the primary disease, correction of platelet levels and symptomatic therapy are prescribed by a hematologist, therapist, or general practitioner. The painful symptoms accompanying low concentrations are usually eliminated with the help of:
- glucocorticoid drugs - Prednisolone, Medopred, Dexamethasone;
- hemostatic agents - Dicynon, Etamzilat, Tranexam;
- coagulants, drugs that enhance blood clotting - Vikasol;
- polypeptide hormone that stimulates platelet production - Thrombopoietin;
- general strengthening agents – elixir or tincture Sodecor, vitamin C tablets.
If you have an excess platelet count, take:
- non-steroidal anti-inflammatory drug with antiplatelet effect - Thrombo ACC, Aspirin, Aspecard;
- thrombin inhibitor – Argatroban, Bivalirudin J;
- anticoagulants – Ticlopidine, Livarudin.
During treatment, systematic monitoring of platelet levels is required. It is also recommended to review the list of regularly taken medications that can affect the content of blood platelets.
Diet
Diet is the most important condition for successful treatment. This should include a nutritious, balanced, varied diet and adequate water intake. With an increased content of non-nuclear blood elements, a woman will benefit from:
- calcium-enriched foods - dairy products, almonds, parsley, lettuce, oranges;
- red meat;
- eggs;
- olive, linseed oils;
- iodine-rich foods - seaweed, fish, cod liver, seafood, fish oil;
- garlic, onion, ginger;
- pomegranates, lemons, grapes, apple cider vinegar;
- berries – blueberries, cranberries, sea buckthorn.
The following are prohibited:
- carbohydrate foods;
- soda;
- smoked meats;
- bananas;
- fried food.
The lack of platelets can be compensated by including in the diet:
- products containing large quantities of vitamins A, C - carrots, red peppers, liver, tomatoes, legumes, fruits;
- buckwheat;
- sources of vitamin K - leafy vegetables, green tea, all types of cabbage, cereals, pumpkin, kiwi and bananas;
- dairy products, meat, eggs;
- products of plant origin containing flavonoids - rose hips, citrus fruits, black currants and rowan berries, grapes, raspberries, green vegetables.
You should avoid dishes with vinegar, marinades, preserves and spicy foods.
Treatment with folk remedies
Self-medication is prohibited. Traditional recipes can only serve as adjuncts to the main therapy. In order not to harm the body, it is recommended to consult with your doctor regarding the use of prescriptions.
Most often they resort to tinctures of medicinal herbs and plants if:
- increased level - wormwood, arnica, mulberry, garlic, cinquefoil. Also take a mixture of ginger and honey diluted in water;
- lower level – nettle juice with milk, chokeberry berries.
Healthy lifestyle
This is a whole range of measures aimed at preventing and promoting women’s health. Includes:
- quitting smoking and drinking alcohol;
- playing sports;
- adequate physical activity;
- walks in the open air;
- healthy sleep;
- positive emotional background, peace of mind;
- regular medical examination;
- timely treatment.
Folk remedies
You can also adjust your platelet levels at home. Treatment with folk remedies should be under the supervision of the attending physician. Tinctures and decoctions are an addition to the main treatment; they cannot replace drug therapy.
Recipe for increasing platelets from nettle:
- nettle juice – 50 ml;
- milk – 50 ml.
Squeeze the juice from fresh nettles and add milk to it. The composition is taken 3 times a day before meals. Duration of admission – 14 days. The mixture is prepared before use; the medicine cannot be prepared for future use, it quickly loses its properties.
Chokeberry improves blood viscosity well. It is recommended to consume 50 berries every day for 3 weeks. The course of treatment cannot be extended.
Recipe for lowering platelet count with garlic:
- garlic – 1 head;
- vodka – 200 ml.
Garlic is poured with vodka and left in a dark place for a month. After a while, grind it through a sieve. Take half a teaspoon 2 times a day.
Recipe for reducing platelets with ginger:
- ginger – 30 g;
- honey – 30 g.
Ginger is crushed. Mix with honey. One spoon of the mixture is diluted in a glass of water and taken 2 times a day. If a blood test shows a deviation from the table norm in the number of platelets - an increased or decreased level - you should undergo a course of treatment. People with thrombocytopenia, regardless of age, should avoid traumatic sports.
You should also avoid alcoholic beverages, vinegar, and certain medications (Aspirin, Analgin). If your platelet count is elevated, you should follow a blood thinning diet and drink as much water as possible. It is especially important to monitor platelet levels in women during pregnancy.