Preparing for conception is a very important period in the life of a woman and a man. A long time (preferably 3-12 months) before the planned conception, they should take care of their health, start eating right, engage in moderate physical activity, give up bad habits, visit the right doctors and pass all the tests.
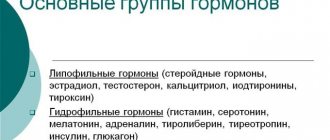
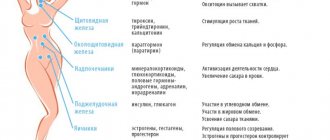
Blood test for sex hormones (female only)
This analysis is required if a woman has problems conceiving (assessing the quality of ovulation), there was an early termination of pregnancy, or an irregular menstrual cycle. The analysis is taken strictly on certain days of the menstrual cycle: on days 2-3 of the cycle
:
- follicle-stimulating hormone (FSH);
- luteinizing hormone (LH) (the peak of the hormone in the middle of the cycle indicates the onset of ovulation);
- estradiol;
- prolactin (increased hormone causes ovulation disorders);
- testosterone (increased hormone causes anovulatory cycles);
- DHEA.
On days 20-22 of the cycle :
progesterone (a decrease in the hormone warns of the threat of miscarriage or a change in the condition of the placenta)
If necessary:
cortisol and thyroid hormones (deficiency leads to anovulation and early miscarriage. Excess leads to developmental abnormalities and premature birth).
Features of the blood type and Rh factor of spouses when planning
It is also necessary to find out the blood type and Rh factor of both the woman and her husband . A positive Rh factor in a wife and a negative Rh factor in a husband does not cause cause for concern. But if, according to the results of blood tests, the expectant mother is found to be Rh negative, and the man is positive, then when pregnancy occurs, a Rh conflict is possible.
This is especially true for women who have ever undergone a blood transfusion, pregnancy, abortion or other surgical operation, because the likelihood of specific antibodies forming in their blood increases.
An Rh conflict may occur between an Rh-positive child and an Rh-negative mother, leading to immune complications, such as hemolytic disease of the newborn.
If a woman is Rh negative, a man is Rh positive, and if there is no Rh antibody titer, Rh immunization is performed before pregnancy. Blood type conflicts are less common, but doctors should take this fact into account.
Ultrasound monitoring (folliculometry)
This study makes it possible to determine how the dominant follicle develops, how tall the endometrium is, and to determine at what time ovulation occurs. For ovulation to occur, the dominant follicle must reach 20 - 22 mm, and the thickness of the endometrium must be 10 - 12 mm. Ultrasound monitoring is carried out several times per cycle, the timing depends on the duration of the menstrual cycle. If a woman’s cycle lasts 28 days, then the first study should be carried out on days 6–8 of the cycle.
Other measures
The expectant mother needs to visit several doctors:
- dentist (at the preparation stage it is advised to treat the teeth, otherwise a lack of calcium during gestation will accelerate their destruction);
- ENT doctor (if chronic diseases of the ears, throat, and nose are discovered during pregnancy, then the weakened body will receive a couple of inflammatory processes that are dangerous to the fetus. After all, even ARVI can cause a delay in the development of the baby’s nervous system);
- a therapist (he will make a conclusion based on blood and urine tests, give general recommendations, and may prescribe additional diagnostics from a geneticist or endocrinologist, if necessary).
Spermogram
Statistics show that 50% of cases of infertility are caused by male problems.
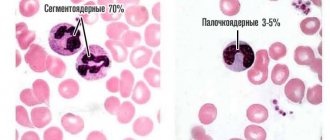
When planning parenthood, you should definitely visit an andrologist or urologist. Determining the qualitative and quantitative characteristics of sperm helps to identify a problem that interferes with normal pregnancy planning. Normal spermogram indicators:
- sperm concentration – the number of sperm in 1 ml should exceed 20 million;
- sperm motility. Category A – sperm with fast motility and category B – sperm with slow motility – there should be at least 25% of each type. Normally, category A+B sperm make up more than 50% of the total. Category C – sperm with non-progressive movements – there is practically no motility. Category D – immotile sperm. The number of sperm of category C+D should not exceed 50%;
- sperm morphology. Normally, more than 30% should have a normal structure;
- the ejaculate volume must be 2 ml or more;
- degree of sperm aggregation and aglutination. Sperm agglutination is the gluing of sperm together, which prevents their forward movement. It shouldn't be normal.
- presence of leukocytes and erythrocytes. There are always 3 - 4 leukocytes in the field of view. There should be no red blood cells.
After testing, one of the following diagnoses is possible:
- normozoospermia – parameters within normal limits;
- oligozoospermia – decreased sperm count;
- asthenozoospermia – decreased sperm motility;
- teratozoospermia – an increase in altered sperm;
- azospermia – absence of sperm in the ejaculate;
- aspermia – absence of ejaculate;
- necrozoospermia – the presence of dead sperm.
Infections, infections - how to protect yourself and your child
The most dangerous thing during pregnancy is internal infections and inflammation. The most important thing is to eliminate them before conception.
Therefore, when studying the body of the expectant mother, special attention is paid to an in-depth study of organs .
The danger of most infections manifests itself during the initial infection, so the test results make it clear which diseases the body has already suffered and which it has not.
The less the body has suffered, the less trained the immune system , the more careful you need to be after conception.
Most infections are dangerous upon initial infection. The most dangerous diseases for the fetus:
- toxoplasma infection (when a parasite lives in your body that is dangerous for the baby; infection usually occurs through poorly cooked meat);
- rubella;
- cytomegalovirus (a little-studied disease, it has a very detrimental effect on the health of the newborn, and therefore it is necessary to undergo tests, which we will talk about later);
- herpes.
Toxoplasma infection
Toxoplasma - test for antibodies of toxoplasma infection. You can get infected from pets, especially cats. 15% of women of reproductive age have already suffered from the disease, 75% of pregnant women will be at risk .
If the test does not detect IgG and IgM antibodies , there is a risk of infection. They give recommendations to refrain from contact with animals, to eat only very well-fried and cooked meat, to thoroughly process vegetables and fruits, and to wash your hands frequently.
Rubella
If a woman does not know whether she has had rubella, she will need to be tested for IgG and IgM antibodies. possible results:
- IgG (their detection means that the body has already suffered the disease and has immunity);
- IgM (this means that you have been infected with the virus for the first time. You cannot plan to conceive within the next 3 months)
- absence of IgM, IgG (it is necessary to get vaccinated to prevent infection after conception. 3 months after the rubella vaccination, you can plan to conceive).
Cytomegalovirus
Infection with cytomegalovirus during pregnancy is dangerous due to developmental pathologies and infection of the fetus in the womb .
Cytomegalovirus is an infection presumably transmitted by airborne droplets, although it has not yet been established exactly how it is contracted.
During preparation for pregnancy, a high level of its development may be detected. With this result, the woman will be required to undergo a course of antiviral therapy . Only after it has passed is it possible to plan conception.
But even a negative result for cytomegalovirus does not mean that the body is not in danger.
It is necessary to take precautions: maintain hygiene, be careful with small children (there is a high probability of infection in preschool institutions).
Herpes
The herpes virus remains in the human body throughout life. The essence of treatment is to reduce its activity. Therefore, since it is impossible to completely get rid of the virus, analysis is needed to assess the risk of primary infection during pregnancy.
STD
What other tests should a woman undergo? A separate study is carried out for sexually transmitted infections.
But usually it is necessary only for those patients who are worried about something (heavy discharge from the genitals, burning) or if they have already had miscarriages, also in preparation for IVF.
Your partner also needs to undergo these tests.
Immune compatibility test
Immune conflict is detected at the level of the cervix. The mucus that is in the cervical canal can delay the progress of sperm and pregnancy may not occur. Normally, this is due to changes in the characteristics of mucus at different periods of the menstrual cycle, and in pathology – with the production of antisperm antibodies (antibodies against sperm that reduce their motility). In order to identify an immunological conflict, the following list of tests is carried out.
Postcoital test
– determination of the number and mobility of sperm in the mucus some time after sexual intercourse. In case of a negative result, it is recommended to repeat the analysis in the next cycle, as well as perform the Kurzrock-Miller test.
Kurzrock-Miller test
– determination of the reaction of the husband’s and donor’s sperm in mucus.
Determination of antisperm antibodies in cervical mucus.
Antibodies inhibit the movement of sperm through the cervical canal, preventing them from attaching and penetrating the egg, so pregnancy does not occur.
What is needed for planning
A visit to the gynecologist is where you need to start. After a gynecological examination and interview, the doctor will determine the scope of diagnostic measures for the couple. In Moscow, you can consult a gynecologist, undergo an examination, get a referral and take the necessary tests at a reproductive medical center. It has its own laboratory and diagnostic equipment, so the results will be ready in just 1-3 days.
When collecting anamnesis, the doctor will be interested in:
- Genetic diseases that may have run in the family.
- Has the woman had viral hepatitis?
- Does the couple have sexually transmitted diseases, tuberculosis, or other dangerous infections?
- Are there any people in your family with endocrine pathologies?
- Duration of the menstrual cycle.
- Has the woman given birth before, have there been miscarriages or abortions?
- What diseases were suffered by future parents in childhood?
- What chronic pathologies are there, do the expectant mother and/or father constantly take medications.
Detailed answers will help you get an idea of the pathologies that can interfere with conception and normal pregnancy. And also prescribe mandatory tests and additional studies.
Karyotyping (genetic analysis, according to indications)
Is the couple at risk for genetic diseases? The answer to this question is provided by karyotyping, a cytogenetic method for studying the blood of both parents. The analysis allows you to identify deviations in the structure and number of chromosomes and determine the degree of risk of unwanted pathology. A genetic risk of up to 5% is considered low. A risk from 6 to 20% is medium, more than 20% is high. If the genetic risk is high, this does not mean that the child will be born with a pathology. It’s just that in this case, prenatal diagnosis is required during pregnancy:
- at a period of 8-11 weeks, a chorion biopsy is used - the cells of the future placenta. Using the analysis, the vast majority of disorders can be identified: Down syndrome, cystic fibrosis, phenylketonuria, hemophilia, etc.;
- starting from the 16th week of pregnancy - amniocentesis (analysis of amniotic fluid);
- after the 17th week, cordocentesis can be performed - fetal blood sampling from the umbilical cord vessels. This analysis allows you to diagnose hereditary immunodeficiency conditions, blood diseases, metabolic disorders, as well as intrauterine infection of the fetus.
Risk group:
- mother's age is over 35 years, father's age is over 40 years;
- consanguineous marriage;
- one of the parents has a hereditary disease or developmental defect;
- the presence of hereditary diseases in relatives of future parents;
- spontaneous miscarriages in previous pregnancies, threatened miscarriage in the early stages, stillbirth;
- exposure to adverse factors in early pregnancy.
You can find out which tests you need to take specifically from your doctor. Having information about what kind of analysis is needed, it is better not to delay diagnosis. Timely testing will allow you to identify an unwanted problem, competently approach pregnancy planning and successfully give birth to a healthy child.
Which doctors should you see before pregnancy?
The main medical specialist that a woman planning a pregnancy should visit is an obstetrician-gynecologist. If necessary, he prescribes consultations with other doctors. When planning to conceive, you should see the following doctors:
- Gynecologist. He will take a vaginal swab, which will help identify the infection. Also, if necessary, this specialist will perform colposcopy - a specialized study aimed at diagnosing cervical cancer.
- Therapist. This medical expert prescribes a range of studies and tests to determine the presence or absence of chronic pathologies.
- Endocrinologist. The specialist will assess the condition of the thyroid gland, the concentration of hormones and will help to promptly determine the increased level of glucose in the blood.
- Dentist. This doctor will perform a thorough examination of the lining of your mouth and teeth. If necessary, it will eliminate damage, relieve inflammation and prevent infection.
- Mammologist. This physician helps determine whether the mammary glands are ready for lactation (breastfeeding).
- Geneticist. Couples who have hereditary diseases in their family should definitely contact this doctor. Based on blood serum tests and oral interviews, the doctor can make an accurate forecast of the possibility of conceiving a healthy baby.
In the presence of chronic pathologies, it is advisable to supplement this list with a visit to a gastroenterologist, cardiologist, ENT doctor, urologist and ophthalmologist.
If you are overweight, you should additionally talk to a nutritionist.