Methods for diagnosing stomach pathologies
Statistics say that approximately 95% of the population, to one degree or another, needs regular monitoring by a gastroenterologist. But there is no need to be afraid of this. The current level of diagnosis of stomach diseases in Russia is high. Many clinics have high-tech equipment that allows diagnostics to be carried out with high accuracy, and qualified gastroenterologists who will explain what kind of stomach examination you need and where to start preparing for it.
FGDS (fibroesophagogastroduodenoscopy) is a study for which you need to get a referral for any gastric discomfort. FGDS is the first step in diagnosing stomach or esophageal cancer after belonging to risk groups has been identified. An experienced specialist will not look at the stomach without examining the esophagus. The esophagus looks both during entry and on the “return path”.
Alternative methods for examining the stomach
In addition to FGDS, there are a number of other diagnostic methods that help detect gastric malignancy. Their comparative characteristics are presented in the following table:
| FGDS | Ultrasound | CT | MRI | |
| Description of the procedure | Endoscopic diagnosis with visual examination of the mucosa | Non-invasive technique using ultrasound | X-ray technique with computer processing of the obtained images | Based on the use of magnetic resonance of atomic nuclei |
| Information content for stomach cancer | High (allows you to make a diagnosis and determine the type of cancer) | Low (only large tumors are visualized) | High (detects metastases to lymph nodes and distant organs) | High (detects metastases to lymph nodes and distant organs) |
| Using Contrast | Not required | Not required | Increases the information content of the technique | Increases the information content of the technique |
| Carrying out a biopsy | Held | Not carried out | Not carried out | Not carried out |
| Time spending | 30-40 minutes | 15-20 minutes | 10-15 minutes | 30-50 minutes |
| Side effects | · Traumatization of the gastric mucosa Bleeding Entry of stomach contents into the respiratory tract | None | Frequent use increases the risk of developing tumors. | None |
| Contraindications | · Severe condition of the patient · Blood clotting disorders Acute stage of myocardial infarction or stroke | None | · Pregnancy · Severe obesity | · Presence of metal implants · Severe obesity |
| Price for research in Moscow | 1200-9700 rub. | 700-4800 rub. | 4000-13500 rub. | 7600-21000 rub. |
Early diagnosis in the case of oncology gives a better chance of long-term remission. Want to know if stomach cancer is visible on an ultrasound? Read this article.
Indications
FGDS is prescribed strictly according to indications, even if there are no complaints:
Statistics say that approximately 95% of the population, to one degree or another, requires regular monitoring by a gastroenterologist for
abdominal pain of unknown origin;- discomfort in the esophagus;
- suspicion of swallowed foreign objects (coins, buttons);
- heartburn that occurs over a long period of time;
- unexplained nausea;
- regular vomiting;
- regurgitation after eating;
- difficulty swallowing (dysphagia);
- unexplained weight loss;
- problems with appetite or its complete absence;
- anemia of unknown origin;
- diseases of the liver, gall bladder, pancreas;
- preparation for abdominal and long-term operations;
- hereditary diseases in the family (stomach cancer, ulcers);
- every year during medical examination for patients with chronic gastritis, gastric ulcer of the duodenum;
- control after therapy for gastritis, ulcers and other problems;
- after removal of a stomach polyp every 3 months for a year;
- the need for polypectomy.
Tests for gastritis: blood, acidity, FGDS examination, x-ray and others
Gastritis is an inflammation of the stomach that occurs as a result of poor nutrition, prolonged use of a number of medications, and smoking. The disease can occur in acute or chronic form.
Accompanied by local (heartburn, pain) and general (weakness, fatigue, decreased vitality) symptoms. We will help you find out what tests you need to take for gastritis to successfully diagnose the disease.
Main symptoms
At the initial stage, the inflammatory process occurs without pronounced symptoms. The first signs of the disease include:
- heaviness in the stomach;
- pain;
- nausea;
- sometimes vomiting or diarrhea.
Patients complain of decreased appetite and weight loss. If such symptoms occur, you should immediately consult a doctor who will give you directions for tests. You can contact a therapist or gastroenterologist.
There are a lot of tests to go through: it is necessary to accurately determine the form of gastritis and differentiate it from other diseases.
For example, atrophic gastritis is the most dangerous - it causes cancerous degeneration of the stomach tissue.
However, it is also necessary to distinguish gastritis from other pathologies: infectious diseases, appendicitis. In some cases, myocardial infarction is accompanied by symptoms of gastritis.
What tests are done for gastritis?
To make a diagnosis, examinations and laboratory tests are necessary.
What mandatory laboratory tests are taken:
- general blood analysis;
- blood biochemistry;
- Analysis of urine;
- stool analysis;
- analysis of gastric juice.
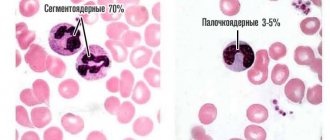
A complete blood count allows you to determine the level of blood components.
Gastritis is characterized by iron deficiency, decreased levels of hemoglobin, red blood cells, and increased erythrocyte sedimentation rate.
In a biochemical blood test for gastritis, a low level of pepsinogens I and II is observed. Autoimmune gastritis is characterized by increased bilirubin, gamma globulin, and low blood protein levels. Pepsinogen level is one of the most important indicators.
- Bacterial gastritis is indicated by its own signs : the presence of antibodies to Helicobacter pylori.
- With pancreatitis, the level of digestive enzymes increases and the level of acid phosphatase increases.
- A urine test can help rule out kidney disease.
FGDS: How to “survive” gastroscopy
There are some medical procedures that people have a subconscious fear of. And gastroscopy of the stomach is one of them.
Doctors in the direction write four letters of the abbreviation - “FGDS”. People say it succinctly and clearly: “Swallow the hose.” And all this is about
the same procedure, which everyone tries to avoid as much as possible.
Until it presses you, and there’s nowhere to go. Swallowing a rubber hose is like eating a pound of raisins. For those who are interested in how this happens, we can explain in detail: “The endoscope begins its journey from the oral cavity, passes through the esophagus, goes down to the stomach and duodenum, and then comes back out.” But it’s scary to even imagine where a hose more than one meter long can be inserted so far.
For those who have not had to endure this procedure, “pray to God that you don’t have to, you are lucky,” say those who have experienced it themselves. Remember how they explained to us: “You can’t eat or drink the day before, so as not to drown the endoscope and the doctor’s hands in the vomit and choke yourself. Please come on an empty stomach!”
Diagnostic features
Fibrogastroduodenoscopy is performed in the endoscopy room on the patient’s “empty” stomach . Most often, local anesthesia is given to the posterior wall of the oropharynx, or a drug is administered for sedation (medicated sleep). FGDS is performed under anesthesia or sedation in a situation where emergency surgery is planned immediately after completion of the procedure.
The probe is inserted through the oral cavity, passes through the esophagus and enters the lumen of the stomach. If an oncological pathology is suspected, the doctor conducts a thorough examination of the mucous membrane. Normally, it should be pink, without defects, signs of inflammation or growth.
How is gastroscopy done?
To avoid complications after the FGDS procedure, it is important not only to prepare for it, but also to follow a diet after its completion. This article will help you cope with the insertion of the probe more easily.
Classification of the disease
Modern recommendations distinguish three types of early gastric cancer, which have different growth patterns:
- Polypous. Upon examination, a small polyp (proliferation of the mucous membrane) is discovered. It is impossible to visually determine its malignancy.
- Superficial cancer. Characterized by differences in the color of the mucous membrane, slight swelling or a reactive inflammatory reaction is possible.
- Ulcerative type. With FGDS, the neoplasm resembles an erosion or ulcer (defect of the mucous membrane). Differential diagnosis with peptic ulcer is necessary.
Visual picture
If the research is carried out at a later stage, then according to Borrman’s classification, 4 options for the visual picture are possible:
- Polypoid neoplasm. The endoscopist sees the growth of the mucous membrane on a wide stalk. Found in a third of cases.
- Polypoid cancer with ulceration. The neoplasm has a trough-shaped shape. From the edge one can see the proliferation of epithelium with erosion or a zone of necrosis, which are located in the center of the tumor. Occurs in approximately 30% of patients.
- Infiltrative-ulcerative variant. The growth of the oncological process occurs mainly in the thickness of the stomach wall. On the surface you can observe an ulcer (sometimes up to 2-3 cm in diameter), a local inflammatory process and swelling without clear boundaries.
- Diffuse-infiltrative. Immediate signs may not be detected during FGDS, since the tumor is almost entirely located in the wall of the stomach. However, the presence of compaction of the mucous membrane, rigidity and unnaturalness of the sweet tooth, and impaired motor skills are noteworthy. Detection rate – 30%. Characterized by early metastasis and poor prognosis.
A separate clinical variant of gastric malignancy is lymphoma . As you know, the stomach wall has a large amount of lymphatic tissue (MALT system).
Reference
Chronic Helicobacter pylori infection plays an important role in the development of the disease, so a rapid test for its presence is almost always positive.
It is necessary to highlight the following characteristics:
- the most common location is the antrum of the stomach;
- the mucous membrane may be little changed, but local redness, surface unevenness and smoothness of folds can be detected;
- proliferation of the mucous membrane;
- swelling without a clear boundary of the stomach wall.
When describing a neoplasm, the endoscopist must determine the nature of tumor growth, the presence of a defect in the mucous membrane, the consistency of the altered tissue, the location and size of the neoplasm.
This article will help you decipher the doctor’s conclusion after FGDS for common pathologies and find out what the protocol normally looks like.
How is a biopsy done?
During FGDS, if areas that resemble a malignant process are detected, a diagnostic biopsy is necessarily performed .
In this case, tissue sampling is done several times. For example, if there is an ulcer, then 3-4 samples are taken from its marginal walls and bottom. During the infiltration process, the deep-seated altered tissues are carefully collected.
After collection, tissue samples are sent for cytological examination, which should determine their type. A biopsy makes it possible to make a final diagnosis of a malignant tumor of the stomach, or to refute it. However, it alone is not enough for a complete diagnosis.
In 85% of cases of gastric cancer, metastases are found in regional lymph nodes or distant organs. Therefore, all kinds of contrast-enhanced imaging methods are used to detect them (CT, MRI, PET).
Forms of oncology
According to WHO recommendations, several histological (by origin and tissue type) forms of gastric cancer can be distinguished :
- papillary adenocarcinoma (from glandular tissue);
- tubular adenocarcinoma (from glandular tissue);
- squamous cell carcinoma (from the epithelium);
- carcinosarcoma (from connective tissue);
- mucinous adenocarcinoma (from glandular tissue, characterized by active mucus production);
- choriocarcinoma (sprouting of embryonic tissue);
- undifferentiated cancer (due to degradation of the tumor cell structure, it is impossible to determine its type);
- poorly differentiated adenocarcinoma.
A common problem in domestic laboratories is the inaccuracy of diagnostics due to the low level of qualifications of personnel (especially in small provincial hospitals) or problems with equipment.
note
Sometimes false positive or false negative results occur. To avoid this, it is advisable to conduct a cytological examination in a specialized oncology clinic.
The results of fibrogastroduodenoscopy are delivered to the patient within a few minutes after completion of the examination. They indicate the nature of the mucous membrane, acidity indicators and detected deviations. The results of the cytological examination are ready in 5-10 days.
Conditions for conducting FGDS
The success of the procedure depends on the qualifications, experience and... hands of the doctor. You need to trust him and do everything they say. For example, hold your breath when necessary. And don't panic! Most often, the procedure does not last long - from two to ten minutes.
Ivan BORISOV is a surgeon at the Medical Center of Yakutsk. According to patient reviews, he is a very friendly and pleasant person. And a professional in his field. And that’s why no one panics at his office and tries to escape under a plausible pretext.
— Ivan Ivanovich, what are people most often afraid of before gastroscopy?
People are afraid not only of the process itself, but rather of possible infection through a common hose with stomach ulcer pathogens, Helicobacter pylori and other dangerous bacteria and viruses. I will dispel these fears: all equipment is after each visitor! – undergoes a full cycle of disinfection and sterilization. High level disinfection kills all germs and bacteria. Only fungal spores do not die.
— For those who are still afraid of “swallowing the hose,” can the procedure be replaced with an ultrasound?
“You see, a video endoscope allows doctors to see a lot on the monitor and evaluate the smallest details of the gastrointestinal tract. The information content of this examination is several times higher than ultrasound. For patients scheduled for a biopsy who have an increased gag reflex, we recommend taking an antiemetic. If desired, the oral cavity can be sprayed with an anesthetic - such manipulations are carried out if the gastroscopy lasts up to one and a half hours. In special cases, general anesthesia is used.
What should be in the document according to the norm?
Often, during an examination, an FGD conclusion is issued that is normal for all parameters. This is especially pleasant after such a procedure is carried out. So, after a lengthy description of all the features, starting from the entrance to the esophagus, with all the sphincters and the condition of the walls, the document contains the conclusion of the FGDS. Ideally, it will be indicated that no pathologically altered phenomena were found or detected in the stomach, as well as in 12 PC (duodenum).
As an introduction, you can give an example of what the FGDS protocol itself looks like, a sample with good indicators:
Esophagus
The entrance to the esophagus is of a normal shape; then it is indicated how many cm are from the incisors. The upper esophageal sphincter is toned. The patency of the esophagus is free, the shape of the lumen, the caliber are normal, the condition of the mucus and walls (in N - elastic, pale pink, smooth, shiny). The shape of the lower esophageal sphincter is normal, the tone is preserved. The distance from the incisors to the dentate line is 35 cm.
Stomach
The distance to the entrance is 36 cm, in the area of the hiatal narrowing. Next, the gaps with narrowings are indicated; normally, there should be a normal caliber. Elasticity of the stomach walls. The color in the area of the lumen, as an option, is straw-colored, as well as the presence of mucus; when performing the procedure on an empty stomach, the amount is small. The mucous membrane may have folds of average height. They can straighten out when air is supplied. The body of this digestive organ is pink in color, with a smooth, shiny, dim vascular pattern. The shape of the antrum is normal. The condition of the walls is characterized by elasticity while maintaining peristalsis. The color of the mucous membrane is normal, without an enhanced vascular pattern. The shape of the pylorus is round, the state is closed.
Duodenum
Normally, during this examination, a 12-pc bulb has a normal lumen shape, with a normal caliber. The condition of the walls is elastic, with preserved peristalsis. It is allowed to fill the lumen with a small amount of bile. The color of the mucosa can be pale pink, the structure is granular, and the vascular pattern is slightly noticeable. Features of the postbulbar sections are ideally not revealed.
This is what the main parameters may look like after an FGD in conclusion. Of course, for various diseases, including gastritis, slightly different parameters will be indicated.
You can study another sample for comparison:
Or another option:
According to the FGDS, the expiration date is given for a decent period so that you can have time to complete all types of services without wasting time. And as long as the cherished conclusion is truly reached, you can continue to be examined for complex treatment or the prescribed operation. And it may be related not only to the gastrointestinal tract, but also to gynecology and other other systems of the body.
Fibrogastroduodenoscopy, or simply FGS, is the “gold” standard in the diagnosis of diseases of the gastrointestinal tract. This technique makes it possible to identify pathological changes in the mucous membrane of the gastrointestinal tract (stomach and duodenum), as well as to conduct additional research methods, such as biopsy. What does FGDS of the stomach show? With the help of this examination, the attending physician has the opportunity to visually examine the inner lining of the organ, examine its suspicious areas, as well as perform a biopsy and a number of simple surgical procedures (polyp resection, stopping bleeding, etc.). Patients are referred for FGDS only if they have signs of a possible stomach disease (pain in the epigastric region, nausea, etc.) and with mandatory adherence to indications and contraindications for the procedure.
A doctor hones his skills in performing FGS on a simulator
Examination of the gastrointestinal tract should be carried out subject to indications and contraindications, and only by a highly qualified specialist.
What does FGDS reveal?
FGDS is a necessary and, in a diagnostic sense, a very valuable procedure. FGDS is a necessary and, in a diagnostic sense, a very valuable procedure. FGDS helps to diagnose (detect):
- stomach and duodenal ulcers;
- stomach cancer;
- stomach polyp;
- varicose veins of the esophagus with cirrhosis of the liver;
- reflux disease;
- esophagitis;
- duodenal stenosis;
- helps evaluate gastric emptying and motility.
FGDS – fibrogastroduodenoscopy
A rather painful procedure, during which a special probe with a video camera is inserted into the patient’s esophagus into the stomach cavity. The doctor sees the image of the mucous membrane of the stomach, esophagus and duodenum on the monitor screen and can objectively determine the presence of inflammatory changes, their nature, and the amount of gastric juice.
During the procedure, the following diagnostic procedures may additionally be performed:
- sampling material for biopsy;
- measuring the pH value of gastric juice;
- taking a sample for bacteriological analysis for the presence of Helicobacter pylori.
Biopsy
A tiny piece of the stomach lining is pinched off with a special instrument to be examined in the laboratory. This will make it possible to judge the presence or absence of oncological changes in tissues, the depth of the process, differentiate the localization of proliferation of cell layers, and preliminarily establish the presence of a bacterial pathogen.
pH-metry
During an internal examination of the stomach, it is possible to check the level of acidity of gastric juice - conduct pH measurements. The results of pH measurements make it possible to differentiate gastritis by the level of hydrochloric acid production and its effect on the nature of the disease: hyperacid or hypoacid gastritis.
Description of the gastroscopy method
Gastroscopy is a method of endoscopic examination of the esophagus, stomach and duodenum. It is used when it is necessary to diagnose a disease, perform a biopsy or surgery to eliminate the pathology. The procedure is carried out if the patient complains of indigestion, frequent heartburn, belching, as well as if there is a suspicion of peptic ulcer, gastritis, or tumor formations. The procedure is carried out using a special device - a gastroscope. It is a long flexible tube, inside of which a fiber-optic system is placed, and at its end is a photo or video camera.
The gastroscope is lowered through the patient's mouth down the esophagus into the stomach, the camera transmits the image to the monitor all this time, and the doctor can monitor the condition of every centimeter of the organs of the digestive system. Gastroscopy is performed by an endoscopist. Order of the Ministry of Health and Social Development of Russia dated June 2, 2010 No. 425-“On approval of the Procedure for providing medical care to the population for gastroenterological diseases” obliges gastroenterological departments or medical organizations that have a gastroenterologist’s office in their structure to be equipped with two gastroscopes with biopsy kits . There are several types of gastroscopy: Traditional endoscopy can be performed with anesthesia, for example, ice caine, or the doctor will ask the patient to take a sedative.
Its advantage is the almost complete absence of side effects after the procedure, but it is extremely difficult for patients to tolerate. Endosonography differs from the previous method in that the ultrasound method is additionally used. This procedure allows you to identify the tumor, determine how deep it has penetrated into the tissue, and choose the right treatment method. Capsule endoscopy is performed using a wireless video camera, shaped and sized like a tablet in a capsule. The patient swallows the capsule, and during its natural movement through the gastrointestinal tract, it records everything that is happening inside the process, and the image is transmitted to a computer monitor in the doctor’s laboratory.
Based on the results of the examined material, the specialist makes a diagnosis. The procedure has many advantages: it is painless, precise, and the capsule is eliminated from the body naturally. But at the same time, during it it is impossible to perform a biopsy or any therapeutic procedure. In addition, capsule endoscopy is expensive: from 50,000 rubles and above. Gastroscopy under anesthesia is performed in cases where any surgical procedure is to be performed: cauterization of erosion, treatment of ulcers, stopping bleeding, etc. In this case, the dosage of the administered drug is calculated strictly individually.
After the procedure, the patient must remain under the close supervision of doctors for several hours. Requires a recovery period. Another type of this procedure under anesthesia is gastroscopy with sedation (during sleep). It eliminates such inconveniences of the traditional method as drooling, gag reflex and others. The patient is immersed in the so-called medicinal sleep exactly for the duration of the procedure. It is widespread in Europe, but not all domestic clinics perform this procedure. After it, you can’t immediately get to work and get behind the wheel.
How often can a gastroscopy procedure be performed?
Gastroscopy is one of the most informative methods for studying the condition of the gastrointestinal tract (its upper section), since this procedure allows you to visually assess the presence of damage to the gastric mucosa, the presence of polyps, erosions, ulcers, bleeding and other pathologies of the walls of the stomach and duodenum.
Many patients are interested in the question of how safe this generally unpleasant procedure is, and how often gastroscopy can be done in the presence of various pathologies of the digestive tract. The frequency of gastroscopy is determined by the attending physician.
However, this study is also prescribed for many other diseases.
For example, cardiovascular: before performing a coronography, an endovascular cardiologist must ensure that there are no gastric erosions or ulcers.
Otherwise, the operation will be postponed, since the patient on the eve of surgery must take strong antithrombotic drugs that thin the blood and promote bleeding.
Indications for gastroscopy
General symptoms such as nausea, diarrhea, vomiting do not always indicate the presence of diseases of the digestive tract, but if the patient complains, he will most likely be prescribed a series of tests that should confirm or refute suspicions of gastritis, duodenitis or other gastric pathologies.
Other indications for prescribing gastroscopy include the following:
- suspicion of the presence of malignant neoplasms in the stomach/esophagus;
- the need for constant monitoring of the condition of the gastric epithelium in the treatment of gastrointestinal diseases;
- symptoms of gastric bleeding;
- if a foreign object enters the stomach;
- if the patient often experiences pain in the epigastric region;
- difficulties experienced by the patient when eating;
- to clarify the diagnosis for a number of diseases not related to gastrointestinal pathologies.
FGDS should be prescribed with caution to children under six years of age, if there is a history of severe mental disorders, if the patient is diagnosed with exacerbation of chronic gastritis or gastric ulcer, or if there is a respiratory tract infection. In any case, the appointment of this procedure can occur repeatedly, and not knowing in what cases and how often gastroscopy of the stomach can be done is very worrying for many patients.
As for contraindications to the appointment of esophagogastroduodenoscopy (the official medical name for gastroscopy), there are few of them:
- some heart diseases;
- narrow compared to the standard entrance to the stomach;
- obesity 2 – 3 degrees;
- hypertension;
- kyphosis/scoliosis;
- a history of stroke/heart attack;
- congenital/acquired blood diseases.
How is gastroscopy performed?
An instrument that allows you to examine the condition of the inner walls of the stomach (and, if necessary, the duodenum) is a type of endoscope. A gastroscope consists of a hollow elastic tube containing a fiber-optic cable with an optical and illuminating device at the end.
Through the mouth and esophagus, the hose is inserted into the stomach cavity for a thorough examination.
Through the cable, the image is transmitted to the eyepiece or monitor screen, and the doctor conducting the study has the opportunity to study the condition of the epithelium in different parts of the stomach by turning and moving the tube in the desired direction.
Is gastroscopy harmful from the point of view of the condition of the esophagus and stomach walls in contact with a solid foreign object? Before the procedure, the gastroscope is thoroughly disinfected, so the likelihood of external infection is extremely low (no more than when eating fruits, bread or vegetables). The possibility of damaging the walls of the esophagus, stomach or duodenum is also close to zero, since the device in its basic form does not have sharp protrusions.
But the procedure itself requires compliance with certain restrictions on the part of the patient. First of all, it should be done on an empty stomach: the presence of food mass makes it very difficult to examine the mucous membrane, so it is very important not to eat 10 - 12 hours before gastroscopy.
Approximately 100–120 minutes before the procedure, you should drink about 200 grams of liquid (weak tea or boiled water), which will clear the stomach walls of food debris and mucus.
It is highly recommended to refrain from smoking the day before, as this provokes the secretion of gastric juice.
Immediately before insertion of the probe, the pharynx and upper part of the esophagus are anesthetized with a spray, and excessive anxiety is relieved with a subcutaneous injection of a mild sedative - the patient’s calm during the manipulation is very important, since fear can lead to involuntary sudden movements, which will make it difficult to examine the walls of the stomach.
Important: the shelf life of gastroscopy before surgery is one month, after which you will have to do a second examination (in a month, significant changes can occur in the stomach cavity, which can affect the result of the operation or be a direct contraindication to its implementation).
The gastroscopy itself is carried out in the following sequence:
- the patient undresses to the waist; if he has glasses or removable dentures that do not adhere well, they must also be removed;
- manipulation is carried out only in a lying position with a straight back, usually on the right side;
- a special mouthpiece is inserted into the mouth, which must be held firmly in order to prevent reflexive clenching of the teeth;
- after instructions to take a few sips and completely relax the larynx, the endoscope is inserted and lowered until it reaches the entrance to the stomach (the most unpleasant moment is the transition from the oral cavity to the esophagus, during which a natural urge to vomit occurs);
- then the doctor begins to turn the gastroscope, which allows you to examine the condition of the gastric cavities from all sides (the viewing angle of the device, as a rule, does not exceed 150 degrees).
Duration of the procedure
When performing a gastroscopy for diagnostic purposes, an experienced doctor only needs 12 to 15 minutes to examine the entire inner surface of the stomach, however, in some cases, a biopsy (taking a sample of epithelial tissue for laboratory testing) or other therapeutic manipulations (for example, administering medications) may be necessary. Such a comprehensive study can last up to 25–40 minutes.
For some time after the manipulation, the patient should be in a supine position; eating during gastroscopy without a biopsy is allowed after 60 minutes.
If the procedure was carried out with a biopsy taken, the first meal of non-hot food is allowed after 180 - 240 minutes.
If the procedure is performed on a child under 6 years of age or a patient with a history of mental disorders, gastroscopy can be performed under general anesthesia.
Decoding the results
The uninitiated will probably not be able to interpret the resulting images, since the resulting picture will more likely resemble some kind of fantastic landscape. But an experienced doctor is able to make an accurate diagnosis, guided by the method of comparison with mucous membranes without pathologies.
It looks like this:
- the color of the mucous membrane ranges from red to pale pink;
- even with an empty stomach, there is always a little mucus on the surface of the walls;
- the front wall looks smooth and shiny, and the back wall is covered with folds.
With gastritis, ulcers, and stomach cancer, deviations from the norm appear that neither x-rays nor ultrasound can detect.
But gastroscopy will definitely reveal them: with gastritis, the disease will be indicated by an increased amount of mucus, swelling and redness of the epithelium, and local minor hemorrhages are possible.
With an ulcer, the surface of the walls is covered with red spots, the edges of which have a whitish coating, indicating the presence of pus. With stomach cancer, the back wall of the stomach becomes smooth, and the color of the mucous membrane changes to light gray.
How often can a gastroscopy be done?
In life, there are often situations when we do not attach importance to certain symptoms that indicate the presence of pathology, and when a diagnosis is made, we begin to intensively look for ways to get rid of it, undergoing consultations and examinations with different specialists.
In the case of gastritis, no doctor will undertake treatment without receiving accurate information about the condition of the mucous membrane. And there are often cases when, after undergoing a gastroscopy, a new specialist may refer the patient for a re-examination to make sure that no significant changes have occurred over time.
Therefore, many patients are interested in how long it will take to repeat gastroscopy.
In principle, in the absence of contraindications, the number of such manipulations is not limited, but in practice they try not to prescribe a test more than once a month - this is the shelf life of the results of the previous study.
In the chronic course of the disease, in order to prevent complications (peptic ulcer, oncology), this study is prescribed 2–3 times a year.
In the process of treating gastritis, if the actual effect of drug therapy does not coincide with the expected one, gastroscopy can be performed more often.
Conclusion
FGDS is a generally safe procedure, although quite unpleasant. Complications are extremely rare: minor damage to the walls of the esophagus/stomach, infection, allergic reaction to medications.
Sometimes after the procedure, painful sensations in the throat occur, which disappear after 2–3 days. How many times gastroscopy can be done over a certain period of time is decided by the attending physician.
If necessary, the procedure is performed with the frequency necessary for successful treatment of the pathology.
Is a biopsy during FGDS painful?
No, the stomach lining does not have pain receptors.
How to prepare for FGDS
The first thing you need to do before gastroscopy is to psychologically tune in to it, realizing that the procedure is necessary. At the first stage, the patient is checked for intolerance to anesthesia or allergies to painkillers. The patient undergoes a general blood test and a biomaterial coagulation test. Patients over 55 years of age undergo an electrocardiogram and, based on its results, a conclusion is made whether the procedure can be performed. On the eve of gastroscopy, if possible, you should stop taking medications. At night, the doctor may allow you to drink a sedative to stop worrying and get enough sleep before the procedure. Gastroscopy is performed on an empty stomach, 10-12 hours before it is necessary to stop eating. Smoking is prohibited 2-3 hours before the test. The patient will be more comfortable if he empties his bladder before the procedure. Before the examination, dentures, jewelry, contact lenses or glasses, if the patient wears them, should be removed. Just in case, you should take paper and wet wipes with you to the hospital. If an additional sheet or towel is needed, the patient will be warned about this in advance.
- The day before - a light dinner.
- No later than 18 hours, before going to bed, tea or water in small quantities is allowed.
- In the morning before the procedure, do not eat, drink, chew gum, or take medications.
- Come strictly on an empty stomach.
- Bring a towel and wet wipes with you.
- People over 40 years old need to bring the result of an ECG, the result of a blood test.
- This procedure is contraindicated for people with diseases of the cardiovascular system.
Preparation for gastroscopy
Gastroscopy should be performed on an empty stomach. The presence of food in the stomach will complicate the examination and will not make it possible to make an accurate diagnosis. Therefore, the last meal should be 8-10 hours before gastroscopy. If gastroscopy is scheduled for the morning, the last meal the night before should not be very heavy and no later than 20.00. In the morning before gastroscopy, you should not eat or drink. If gastroscopy is planned for the second half of the day, then it is also advisable to limit the morning meal to sweet tea.
Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment. Rate how useful the material was 0 Thank you for your rating
Methodology
The procedure is carried out by a doctor after taking written consent from the patient.
The patient's mouth is sprayed with lidocaine solution or a falimint tablet is given under the tongue.
The patient is placed on the couch on his left side so that the left cheek is pressed against the pillow and the arms are folded on the chest or stomach. It is possible to move the left arm across the stomach to the back, and place the right arm on the stomach.
The patient is placed on the couch on his left side so that the left cheek is pressed against the pillow and his arms are folded on his chest or stomach
After preparation, the patient is given a special plastic mouthpiece in his mouth, which he must clamp with his teeth and lips. This is to protect the gastroscope tube from being bitten. The doctor carefully inserts the endoscope into the mouth through the mouthpiece to the root of the tongue, asks the patient to take a deep breath or swallow, after which the fiberscope enters the esophagus.
As the tube passes through the esophagus, the doctor carefully examines its walls. Then it enters the stomach, the walls of which are also carefully examined, and then into the duodenum.
During the fiberscope, the patient should breathe deeply, which will reduce gagging. The patient feels the fiberscope sliding along the walls of the stomach as scraping or itching. The entire procedure lasts from 5 to 30 minutes (depending on the severity of the pathology).
Sometimes it becomes necessary to take a piece of tissue for a biopsy or remove a polyp, which is done during an FGDS (slight pinching). The fiberscope is removed carefully and slowly.
Pathology
When a pathology is detected in the results of gastroscopy
(esophagogastroscopy),
it is usually written what kind of pathology was identified. For example, it may be written that it was revealed:
- ulcerative or duodenal lesions of the stomach;
- signs of inflammatory processes in any of the examined organs or simultaneously in several organs. If it is in the stomach, then it is gastritis; if it is in the esophagus, then it is esophagitis; if inflammation is detected in the small intestine, then it can be either enteritis or duodenitis.
- abnormal (different from normal) openings in a hollow organ. This may be bleeding, swelling, ulceration or perforation;
- varicose veins of the submucosal layer of the organs being examined;
- hiatal hernia is a hernia of the esophageal opening of the diaphragm;
- narrowing (stricture) or pathological expansion (dilatation) of the organs being examined;
- Foreign body in the organs being examined.
The written conclusion issued after the FGD confirms the condition of the digestive organs examined during this procedure. You need to understand that the validity of any analysis may be limited. So don’t delay, and start collecting forms as quickly as possible. It is important to interpret it correctly so as not to be misled about the state of your own health. This can best be done by the treating gastroenterologist in order to take further measures to treat existing pathologies.
Many patients, due to general fear, do not dare to go for a long time for examination. However, you need to understand how informative this FGS procedure is, and that it lets you know everything about the condition of the stomach, esophagus, and also the duodenum, if it needs to be examined.
How is gastroscopy performed under anesthesia?
The procedure is carried out in a specially equipped room and is performed by an endoscopist. The patient is asked to lie on his side, straighten his back, bend his knees. Then the patient clamps his teeth on the mouthpiece, a device through which the endoscope is inserted. The mouthpiece protects the teeth and at the same time protects the endoscope itself; after all, it is an expensive instrument. When inserting the tube inside, you need to make swallowing movements to move it along the esophagus.
When the gastroscope reaches the stomach, the specialist begins to pass air through it to smooth out the folds of the mucous membrane of the internal organs. After this, you can no longer swallow saliva; if it accumulates, the nurse will remove it with a saliva ejector. If surgery or medication is required, it will be very painful for the patient.
In this case, the procedure performed under anesthesia is the best option. When performing gastroscopy under anesthesia, the doctor will not be disturbed by the patient’s reflexes, and he, in turn, will not experience pain. The endoscopist will be able to work calmly while performing therapeutic procedures. The procedure takes 10–20 minutes.
How is gastroscopy performed? Gastroscopy in a dream
Gastroscopy can be performed under local anesthesia, as well as in a state of medicated sleep. Drug-induced sleep should be distinguished from general anesthesia.
If the procedure is performed under local anesthesia, gastroscopy lasts 5-10 minutes. The patient is asked to hold the mouthpiece through which the gastroscope is inserted.
For those who are wary of this procedure, the doctors at Family Doctor recommend using it. This service is provided in a surgical hospital setting. Abroad (in Europe, Israel, the USA, Japan), gastroscopy during medicated sleep is the basic version of the procedure, which is abandoned only if there are contraindications.
To perform gastroscopy in your sleep, it is advisable to approach 30 minutes before the time for which the procedure is scheduled. In this case, you must have a fresh and deciphered electrocardiogram on hand. You will be examined by an anesthesiologist who will determine whether there are any contraindications to the study. To put you to sleep, the drug “Proviv” is used, which is administered under the supervision of an anesthesiologist. When the drug is administered, the patient falls asleep and wakes up almost immediately after the end of the administration. After 15-20 minutes, complete recovery occurs, however, the doctors at “Family Doctor” still recommend staying under the supervision of a doctor for another hour or two, which can be done in our comfortable hospital. It is considered acceptable to drive a car two hours after waking up from sleep, but it is better to drive no earlier than 6 hours later.
During the study, it may be necessary to carry out therapeutic and diagnostic manipulations (biopsy - taking a tissue element for laboratory analysis, removal of polyps, etc.). Similar manipulations are carried out during the study using a gastroscope. The biopsy material is sent to the Family Doctor’s own laboratory, which significantly speeds up the process of obtaining results.
How much does a gastroscopy cost?
The average price of gastroscopy in Moscow starts from 4000–5000 rubles, and the cost of an X-ray examination of the stomach is 3000–4000 rubles. The approximate cost of an ultrasound scan ranges from 2000–3000 rubles. How much a laboratory examination of the stomach costs depends on the set of laboratory tests chosen and methods for studying the biomaterial.
We asked a representative of the INVITRO network of independent laboratories what gastric studies are most in demand today, and how much they cost those suffering from gastroenterological diseases: “Due to the close relationship of the abdominal organs, functional stomach disorders lead to disturbances in the functioning of all gastrointestinal organs - decreased immunity, Metabolism suffers, the absorption of biologically valuable substances in the intestines is impaired, and this entails the development of chronic diseases and a deterioration in the quality of life.
Therefore, a comprehensive examination of the entire gastrointestinal tract is the only method to see in the smallest detail the condition of such an important organ of the digestive system as the stomach. Only based on the results of several studies can various gastroenterological diseases be diagnosed with high reliability. In addition, this allows an individual approach to the choice of treatment for each patient, preventing the development of complications.
Before any hardware examination of the stomach, especially before gastroscopy and biopsy, you can conduct a set of venous blood tests for antibodies to H. pylori, the level of pepsinogen enzymes and gastrin-17, included in the “Gastropanel”, which was developed by the Finnish company BIOHIT.
A comprehensive examination of the entire gastrointestinal tract is the only method to see down to the smallest detail the condition of such an important organ of the digestive system as the stomach
These blood tests make it possible to identify pylori-associated chronic gastritis at an early stage, narrow down the causes of dyspeptic disorders - heartburn, pain, nausea, heaviness and other types of discomfort in the stomach, and assess the risk of developing peptic ulcers and even oncology. "Gastropanel" is indicated for unidentified forms of anemia, if hidden blood loss is suspected. Its cost is 3300 rubles. By the way, the following are usually held together with Gastropanel:
- examination of feces for occult blood using a quantitative immunochemical method (benzidine test) - 340 rubles;
- determination of antibodies to gastric parietal cells, total IgG, IgA, IgM - 1,435 rubles;
- determination of lipase level - 425 rubles;
- determination of Ca 72-4 (carbohydrate antigen 72-4) - 1230 rubles;
- determination of Ca 19-9 (carbohydrate antigen 19-9) - 840 rubles, determination of carcinoembryonic antigen (CAE, Carcinoembryonic antigen, CEA) - 805 rubles, cytological examination of endoscopic material for the presence of Helicobacter pylori - 845 rubles.
Of course, you cannot decide on your own which tests for gastritis should be taken and which should not. This decision is made solely by a gastroenterologist. Only he should interpret the test results. By the way, you can also have a consultation with a gastroenterologist at one of the INVITRO medical offices.
Diagnosis of gastritis
Any diagnosis begins with an examination of the patient by a doctor. Initially, a clinical examination is carried out, during which the doctor determines the condition of the skin and palpates the abdomen in the stomach area: if the patient suffers from gastritis, the pain during palpation worsens.
Clinical examination can only give a guess about stomach disease. To find out the nature and extent of organ damage, instrumental and laboratory diagnostic methods are needed.
Gastroscopy (or fibrogastroduodenoendoscopy, FGDS) is a study of the upper gastrointestinal tract (esophagus, stomach, duodenum) using a gastroscope device - a probe equipped with a camera. The endoscopist sees the condition of the mucous membranes of the organs during the procedure itself, and if necessary, photographs or video recordings of the image from the camera are taken.
FGDS allows for differential diagnosis of gastritis with peptic ulcer disease, as well as determining the localization of gastritis and its type: erosive or non-erosive. Erosive (or corrosive) gastritis is a type of acute gastritis that occurs against the background of exposure to toxic substances (acids, alkalis, alcohol, non-steroidal anti-inflammatory drugs) and is accompanied by deep damage to the gastric mucosa - erosions. Non-erosive gastritis is associated with damage to the upper layer of the gastric mucosa, but over a long period of time it can become chronic or become an ulcer.
A gastroscope makes it possible to carry out not only visual diagnostics of the stomach, but also to take samples of its contents (gastric juice) and tissues, in other words, to conduct pH measurements and biopsies.
A biopsy is the removal of fragments of the gastric mucosa for laboratory testing. This method is very informative for studying diffuse (rather than point) lesions of the mucosa; samples are taken, as a rule, in three different parts of the stomach. The procedure is painless and safe, does not require additional anesthesia, the areas of the mucous membrane taken for analysis are very small and are pinched off only from the surface of the membrane.
The pH-metry method consists of studying the acidity of the stomach, as well as the duodenum and esophagus. The level of acidity of gastric contents allows us to judge the presence of an inflammatory process.
The pH measurement procedure has several methods of implementation. During rapid analysis, a thin pH probe is inserted into the stomach through the mouth, equipped with special electrodes to measure acidity in different parts of the stomach. Daily pH-metry is the study of acidity in the stomach for 24 hours or more. In this case, the probe is inserted into the organ through the nose, and a device for measuring pH is put on the patient’s belt - an acidogastrometer, which records the dynamics of changes in acidity. A technically improved version of daily diagnostics is the ingestion of a mini-capsule, which is attached to the wall of the esophagus and transmits information to the acidogastrometer. After a few days, the capsule detaches from the esophagus on its own and naturally leaves the gastrointestinal tract. Endoscopic pH measurement involves performing the procedure during FGDS; in this case, the pH probe is located inside the gastroscope tube.
Gastric juice is also examined by probing. Samples of gastric contents are taken using special instruments built into the gastroscope. As a rule, before this procedure, the patient is given so-called test breakfasts, which stimulate the production of gastric juice. Analysis of gastric contents makes it possible to determine not only the fact of gastritis, but partly also its nature: with a disease caused by Helicobacter pylori, gastric juice contains a lot of gastrin.
Probing of the stomach is not permitted in all cases (for example, after surgery, with organ stenosis). Then it is possible to measure the acidity level using an acid test: the patient takes special medications that, when interacting with hydrochloric acid in the stomach, form dyes that are detected in the urine.
To diagnose gastritis caused by the bacteria Helicobacter pylori, several types of tests are possible: laboratory analysis of stool or biopath (samples of the gastric mucosa), a blood test for antibodies to this bacterium, and a respiratory test. In the last method of diagnosing gastritis, the patient is given juice to drink in which carbamide (urea) with a labeled carbon atom is dissolved. Helicobacter pylori has the ability to quickly break down urea, increasing the release of carbon dioxide when exhaled. It is the study of the level of CO2 in exhaled air that allows us to conclude that the patient is infected.
The X-ray method is also used in the diagnosis of gastritis, but is in second place in terms of information content after gastroscopy. 12 hours before the study, the patient does not eat, and swallows a contrast agent for radiography. The doctor examines the stomach in several positions of the patient's body. X-ray examination allows you to see the relief of the organ, assess its tone, and identify the presence of gastritis, ulcers, and tumors. A sign of gastritis in many cases are characteristic changes in the relief of the mucous membrane, but often, in order to identify the constancy of these changes, it is necessary to repeat the procedure.
All of these methods are useful for diagnosing chronic gastritis. In the acute form of the disease (at an early stage), examination of the patient and collection of anamnesis are primary. In some cases, FGDS and mucosal biopsy are used to diagnose acute gastritis.
To diagnose gastritis in children, in addition to tests, gastroscopy and ultrasound of the abdominal organs are used. Only in cases of difficulty in making a diagnosis do they resort to taking samples of gastric juice and mucous membranes, pH measurements, and radiography with a contrast agent.
Differential diagnosis of gastritis
Acute gastritis has similar symptoms to a number of other diseases of the abdominal organs (acute forms of cholecystitis and pancreatitis, stomach ulcers, myocardial infarction), infectious diseases accompanied by dyspepsia (typhoid fever, meningitis, scarlet fever).
To differentiate gastritis from other diseases of the abdominal organs, a blood test (general analysis, alpha-amylase test) is indicative. Allows you to distinguish diseases and obtain a more complete anamnesis.
Thus, with acute pancreatitis, patients complain of incessant intense pain in the abdomen, often girdling, and a general serious condition. Acute cholecystitis begins with severe pain, first in the form of contractions, and then turning into constant pain. In this case, the pain is localized in the right hypochondrium and radiates to the right upper part of the body, and a high body temperature is often observed - 38–39 degrees.
Are special conditions needed for FGDS?
Correct FGDS is done in 20 minutes in several stages; chromogastroscopy, biopsy, inversion and examination in a special spectrum (for example NBI) are mandatory. It is necessary to use methylene blue dye to paint the walls. It is with this dye that early forms of the disease can be detected. During each FGDS, a dye must be injected through the instrumental channel of the endoscope (chromogastroscopy). Also, during the procedure, the endoscopist must perform an inversion - turn the endoscope towards the cardia. There are also various options for another spectrum, when mucous membranes and the structure of the vascular pattern are considered.
What does FGDS show for gastritis and how is it carried out - MOSGORMED
Gastroscopy is one of the most objective and informative diagnostic procedures prescribed by a doctor for gastrointestinal diseases. The study helps to assess the condition of the mucosa, make predictions and select the current treatment option.
The peculiarity of the analysis is that a tube with a camera at the end is inserted into the body. Thanks to the equipment, a high-quality image is projected onto the screen, giving the doctor the maximum amount of data about the patient’s condition. Preliminary examination does not always provide information about the characteristics of each specific case. Therefore, the procedure allows us to identify:
- Problems with the mucous membranes of organs;
- The presence of neoplasms and their location;
- Areas affected by the bacterium Helicobacter pylori;
- State of pylorus;
- The presence of erosion of the gastric mucosa.
Timely examination helps begin the necessary treatment.
What does FGD show for gastritis?
Gastroscopy is a variant of the so-called differential diagnosis for gastritis. With its help, the doctor determines the location of the source of the disease, as well as its type. Gastritis can be erosive and non-erosive.
The first option is an acute form of the disease that occurs when exposed to toxins such as alcohol, acid and alkali, and medications. During diagnosis, erosion is detected.
The second option involves the presence of damage to the mucous membrane and often develops into a chronic disease or provokes the appearance of an ulcer.
Gastroscopy gives a visual representation of the condition of the stomach, which allows you to make the most accurate diagnosis. In addition, during the procedure, you can take samples of the stomach contents: juice, tissue. This is how biopsies and pH measurements are performed.
Tips for gastritis
- First of all, diet. At first, while the feeling of heaviness in the stomach is especially painful, refrain from eating altogether. If you feel hungry, eat according to the following requirements.
- Eliminate “rough” foods. Gastritis is an inflammation of the mucous membrane, so there is no need to irritate it mechanically. No crackers, nuts, rough vegetables.
- For gastritis, it is advisable to exclude foods that stimulate the production of gastric juice. These are smoked meats, fried meats, marinades, pickles, strong broths, etc. Since in a number of cases gastritis is caused by increased acidity of gastric juice, eliminate foods containing acid, including cottage cheese and fermented milk products.
- Food that is too hot or too cold is also contraindicated.
- What to eat for gastritis? Oatmeal, buckwheat porridge, boiled lean meat, chicken (but not skin!), boiled fish. You can drink water or weak tea.
- Eat in moderation, often, but little by little. Drink more. By the way, these rules are also good for healthy people - they are the basis of proper nutrition.
- If you have gastritis, alcohol should be completely avoided, and you should also try to quit smoking. If it works out, the disease can serve you well: by giving up a bad habit for a while, you can quit it forever!
How long is the result valid?
The validity period of FGDS results for a doctor is 3 months . However, this term can be shortened. The action depends on the patient’s condition, for example, if signs of gastrointestinal bleeding occur, the study should be carried out as quickly as possible.
Any inflammatory disease first occurs in an acute form. To become chronic, the process requires time and lack of treatment.
Diagnosis of chronic gastritis - inflammation of the gastric mucosa, is based on the receipt and analysis of cumulative data from a conversation with the patient, external examination and internal clinical, instrumental, laboratory, bacteriological and biochemical studies.
Pathology
When a pathology is detected in the results of gastroscopy
(esophagogastroscopy),
it is usually written what kind of pathology was identified. For example, it may be written that it was revealed:
- ulcerative or duodenal lesions of the stomach;
- signs of inflammatory processes in any of the examined organs or simultaneously in several organs. If it is in the stomach, then it is gastritis; if it is in the esophagus, then it is esophagitis; if inflammation is detected in the small intestine, then it can be either enteritis or duodenitis.
- abnormal (different from normal) openings in a hollow organ. This may be bleeding, swelling, ulceration or perforation;
- varicose veins of the submucosal layer of the organs being examined;
- hiatal hernia is a hernia of the esophageal opening of the diaphragm;
- narrowing (stricture) or pathological expansion (dilatation) of the organs being examined;
- Foreign body in the organs being examined.
Indications and contraindications for examination
FGDS of the stomach is performed for those patients who have symptoms of damage to this organ or suspicions of another pathology:
- Pain in the upper abdomen associated with eating or, conversely, occurring during hunger, which is typical for gastritis and peptic ulcers of the stomach and duodenum.
- A feeling of discomfort or burning behind the sternum, which may be a manifestation of cardia insufficiency and gastroesophageal reflux disease.
- Suspicion of the growth of benign or malignant tumors in the wall of the stomach.
- Disorders of motor activity of the esophagus and stomach.
- Frequent attacks of nausea or vomiting.
- Examination of the duodenum is indicated for indirect signs of pancreatitis, most often associated with impaired absorption of fatty foods and pain in the left side of the abdomen.
Thanks to FGDS, the doctor can look at the display screen and see all the changes in the gastric mucosa immediately at the time of the study, which significantly increases the accuracy of diagnosis.
In all these cases, endoscopic examination of the upper digestive tract allows us to see pathological changes in the organs. However, there are a number of contraindications for which FGDS is not done:
- obstructions in the patency of the esophagus due to its stenosis or functional disorders;
- severe somatic diseases affecting the respiratory or cardiovascular system.
If a person has contraindications to endoscopy, then the procedure is not performed, but other examination methods are chosen, for example, ultrasound.