The fallopian tubes are essentially two tubes with a lumen inside, on both sides of the uterus - they function as a connecting duct between the reproductive organ and the ovaries. After the sperm penetrates into the female cell through one of these tubes, it enters the space of the uterus, where the fetus further develops.
If the permeability of the fallopian tubes is impaired, the zygote will not be able to pass into the uterine environment, which is comfortable for development and growth, and after a certain period of time it will die or be implanted outside the uterine space and a pathology will occur, the so-called “ectopic” pregnancy.
The leading causes of this deviation are inflammation and STIs. In addition, impermeability of these canals may occur due to an abortion or after surgery in the abdominal space.
When all the indicators are in order, but it has been impossible to get pregnant for more than six months, experts advise women to test for patency of the uterine tubes.
When is it prescribed?
It is recommended to undergo an ultrasound to determine the patency of the tubes if:
- a woman has been diagnosed with infertility (both primary and secondary);
- the menstrual cycle is irregular;
- inflammation of the uterus is chronic;
- no periods, but pregnancy is excluded;
- the patient has pain in the lower abdomen;
- the woman has been treated for any of the sexually transmitted infections (especially if the treatment was not completed).
Is it worth restoring passability?
Age becomes important in this matter.
If a woman is young and, apart from obstruction in the tubes, she cannot experience any other pathologies that would prevent conception, the patency of the ducts may return and one can try to conceive a child within a year.
When you fail to get pregnant, you should not waste time; you must immediately use the IVF method (in vitro fertilization).
It happens that after the birth of the first child conceived via IVF, conception occurs naturally in the future.
This occurs due to the fact that during the period of bearing a child, the uterus grows in size and spontaneous elimination of adhesions and the appearance of lumen of the fallopian tubes can occur.
Over the age of 35, if you have been infertile for a long time and have blocked fallopian tubes, you should choose IVF. As time passes, the quality characteristics of the eggs become worse and the risk of genetic abnormalities in the child increases.
For this reason, spending time trying to recreate the lumen of the tubes is simply fruitless - time passes, and this fact, unfortunately, is not in the woman’s favor. In addition, it becomes possible to conceive independently, following the appearance of the first one.
It must be borne in mind that after the lumen of the fallopian tubes returns, the risk of pregnancy outside the uterus increases.
Are fallopian tubes visible on ultrasound?
Usually, the tubular organs of the uterus cannot be seen on ultrasound.
However, if liquid has accumulated in them, then the likelihood of seeing them increases.
But neither adhesions nor internal inflammation can be diagnosed.
These phenomena are not determined due to the lack of ultrasound signs and can only be detected using contrast fluid.
Therefore, to study the patency of the tubes, a special procedure is required, which is accompanied by the introduction of fluid into the uterine cavity .
Hydrosonography (Echohysterosalpingography)
This type of examination is similar to the previous one. Some patients are wary of exposure to X-rays and prefer ultrasound examination. The result is visible not in the image, but on the screen of the ultrasound machine, and since there is no radiation, this type of study is applicable to pregnant patients.
On what day of the cycle is the study carried out?
The patency of the fallopian tubes is checked in this case on days 5-10 of the cycle, before ovulation, due to the fact that during this period the cervical canal is sufficiently open and the cervix is still in a relaxed state. Pregnant patients are examined any day.
Preparing for the study
Echohysterosalpingography is a relatively new type of examination, but it does not require complex tests.
You need to provide a standard series of tests:
- Ultrasound of the pelvic organs (3 months);
- flora smear (1 week);
- UAC (2 weeks);
- OAM (2 weeks);
- blood for hepatitis, HIV and syphilis (3 months).
Refrain from any food or liquid for several hours before the procedure, and empty your bladder immediately before the procedure.
How does the procedure work?
The examination takes place on a gynecological chair. The principle of this method differs from the X-ray method in that it is implemented using an ultrasound machine.
- A special disposable catheter is inserted into the cervix.
- A special liquid is gradually passed over it.
- After administering the entire volume of the solution, the doctor uses the monitor of a real-time ultrasound machine to examine the features of the fallopian tubes and uterus.
Decoding the results
EchoHSG is a fairly simple procedure and recovery after it occurs quickly , just like with the X-ray examination method. Unpleasant sensations in the form of nagging pain may appear due to the insertion of the catheter. The peculiarity of this method is that the specialist who performs the ultrasound examination must make the final diagnosis.
There are few such specialists, so echoHSG is not as common as HSG. The information content of this method is somewhat lower than that of X-ray, but due to the lack of radiation exposure, the procedure can be repeated.
Recovery
For a maximum of 3 days, the patient may experience spotting blood clots and pain in the abdominal area, which can be eliminated with the help of any antispasmodic. Postponing pregnancy after echoHSG is not required, since there was no dietary intervention.
Preparation
Before determining how passable the tubes are, the patient will need to prepare for an ultrasound examination. To do this, you need to pass several tests:
- flora smear - taken by a gynecologist during an examination;
- general clinical blood and urine tests;
- PAP test (Papanicolaou smear for oncocytology);
- for infections using PCR (for mycoplasma, ureaplasma and chlamydia)
Preparation for such procedures certainly includes a hygienic part - immediately before visiting the doctor, you need to thoroughly clean your genitals (wash yourself or take a shower).
Reference! If the doctor deems it necessary, then 40 minutes before the GSS, antispasmodics can be prescribed.
You also need to clarify which sensor will be used for the study - if transabdominal, then you will need to fill the bladder.
Hysterosalpingography (HSG)
This method is used more often than others, since the reliability of the result is very high. The examination takes place using fluid entering the uterine cavity, after which it moves through the tubes to the ovaries. Many women note that pregnancy occurs after the procedure.
this is explained by the fact that the contrast, which enters the cavity of the pipes, moving along them, washes them, and the adhesions are removed on their own.
On what day of the cycle is the study carried out?
The patency of the fallopian tubes is checked from the end of menstruation to ovulation. That is, with a cycle of 28 days, the HSG procedure is performed from days 6 to 12 of the cycle. These days, the endometrium is thin and the neck is soft, so the catheter is inserted without effort.
Preparing for the study
The HSG procedure requires special preparation, since it can be called a mini-operation; intervention occurs in internal organs.
Some tests need to be done:
- HOW (valid for 1 month);
- examination for sexually transmitted infections (valid for 3 months);
- urine test (valid for 1 month);
- flora smear (valid for 1 week);
- Ultrasound of the pelvic organs.
In addition to medical tests, you should avoid sexual intercourse from the day of menstruation until the day of the examination.
The day before the procedure, you need to empty your bowels, and on the day of the procedure, do not take heavy food; generally, HSG is prescribed in the morning and is done on an empty stomach. You also need to wash yourself and empty your bladder before the procedure. It is recommended to take a painkiller half an hour before.
How does the procedure work?
The examination is carried out on a transparent glass table designed for x-ray procedures:
- The patient lies on the edge of the table and bends her knees. Above it is an X-ray machine.
- The gynecologist disinfects the external surface of the genital organs with a special antiseptic solution, and the patient may feel a burning sensation.
- Using special medical devices, the cervix is released.
- Using a large syringe from which comes a thin tube, contrast is gradually injected into the uterus . First, the doctor injects no more than 3 ml of liquid and takes the first picture, which will clearly show the uterine cavity.
- After adding a few more ml of contrast, the liquid gradually passes into the fallopian tubes.
If the tubes are at least partially passable, the fluid passes into the abdominal cavity and the doctor takes a 2nd picture.
The duration of the procedure is no more than 40 minutes. As a rule, the examination is painless, but discomfort is inevitable. When inserting gynecological equipment and a contrast agent, most patients feel nagging pain, as at the beginning of menstruation.
Decoding the results
Hysterosalpingography allows you to detect pathology of all female organs. From the resulting X-ray images, the doctor sees the size of the organs, how the pipes are located, whether the contrast moves throughout the pipe or stops. The images can also show inflammation in the uterus, adhesions and fibroids.
When the liquid contrast reaches the end of the fallopian tube, the doctor observes whether it exits into the abdominal cavity.
If patency is difficult, the contrast will be delayed at the adhesion site and the tube will be slightly stretched due to pressure. If the tubes are only partially patent, only a small amount of fluid will leak into the abdominal cavity. The presence of adhesions is noticeable by the lumens in the fallopian tube. After deciphering the results, the images are given to the patient for further examination and observation by a gynecologist.
Recovery
After HSG, the woman needs to be in a horizontal position and at rest for some time. As a rule, the woman is placed in a hospital room for several hours under the supervision of a doctor. For several days after the HSG examination, spotting and bleeding may be observed , this is due to irritation of the mucous membrane; in addition, mild nagging pain is possible that does not require anesthesia.
It is not recommended to take a bath, visit the sauna or use tampons in the first days after the procedure; you should abstain from sexual activity.
How do they do it?
Hysterosalpingoscopy is performed in one of two ways: externally (through the abdominal wall) or transvaginally (by inserting a sensor into the vagina).
Progress of the procedure:
- The back of the gynecological chair is lowered, and the woman takes a lying position on it.
- Then a thorough treatment of the cervix and vagina is performed.
- A disposable small-diameter catheter with a balloon at the end is inserted through the neck, which is necessary for fixation.
- Using an ultrasound, the doctor makes sure that the catheter is positioned correctly (a vaginal sensor is used for the procedure).
- A saline solution or a special gel is injected into a woman’s body, which, as it moves through the fallopian tubes, makes it possible to examine their structure (its amount varies from 20-40 ml to 100-110 ml). The procedure allows not only to determine the presence of adhesions, but also to identify inflammation.
The study is carried out on an outpatient basis, and the patient does not need to stay in the hospital after its completion.
Video 1. Ultrasound of the fallopian tubes.
In terms of time, the GSS takes from 10 minutes to half an hour.
Pertubation
Pertubation is a method of checking the patency of the fallopian tubes, the essence of which is that gas is supplied through the uterine cavity, after which it reaches the fallopian tubes, eliminating adhesions. During the procedure, slight discomfort is felt in the abdominal area.
The examination takes place in a hospital setting.
On what day of the cycle is the study carried out?
Pertubation of the fallopian tubes is done in the 1st phase of the menstrual cycle, after the critical days. Mainly on days 8-20 of the cycle, since during this period the surface of the uterus and tubes is smooth and gas passes through them more easily.
But there are cases when the examination is carried out in the second phase of the cycle, it depends on the estrogen saturation of the individual patient.
Preparing for the study
Pertubation is a method in which it is important to exclude any infectious diseases, so you should undergo a standard series of tests:
- vaginal smear for flora (1 week);
- bimanual examination (examination of the vagina and abdominal walls);
- UAC (2 weeks);
- OAM (2 weeks);
- coagulogram (2 weeks);
- biochemical blood test (2 units);
- blood test to determine blood group and Rh factor;
- blood test for HIV and hepatitis (3 months);
- blood test for syphilis (3 months);
- fluorography (1 year);
- ECG (3 months);
- Ultrasound of the pelvic organs (3 months).
In addition, an important point in preparation is to empty the bowels and bladder immediately before the examination.
How does the procedure work?
The pertubation procedure can be carried out both in a hospital and in an office setting in a antenatal clinic , if the necessary equipment and tools are available.
- The woman sits on a gynecological chair.
- Using mirrors, the doctor frees access to the cervix and disinfects it.
- A cannula is inserted into the uterine cavity, which tightly closes the cervical canal.
- Carbon dioxide is injected into the uterus through the tip at a pressure of no more than 200 mmHg. Art. Gas through the uterine cavity under pressure enters the tubes and passes into the abdominal cavity.
Provided that the pipes are passable, the patient experiences discomfort in the area of the shoulder blades, this is due to the formation of a gas bubble.
Decoding the results
The patient’s sensations during the procedure largely indicate the result of the examination. During the transition of gas into the abdominal space, the doctor may hear a noise through a stethoscope, and the patient may feel pain in the collarbone area.
If a woman feels pain in the lower abdomen, most likely there is a tubal obstruction.
If the maximum gas pressure is 90 mmHg. Art., fallopian tubes are passable. If the pressure does not increase at around 100-140 mm Hg. Art., one can judge about spasm of the fallopian tubes. At a pressure level of 160-180 mm Hg. Art., gas movement is suspended.
When the fallopian tubes are completely blocked, the gas pressure constantly increases and can reach a maximum point of 200 mmHg. Art. At 200 mm Hg. Art. the gas supply stops because there is a risk of pipe rupture.
Recovery
After the examination, the patient is recommended to remain under medical supervision for 2 hours. Complications can only arise if there were infectious diseases of the pelvic organs before the procedure or if the pressure exceeds 200 mm Hg. Art. when gas is supplied.
These consequences are extremely rare and are associated only with medical incompetence and violation of surgical technique.
Norm and decoding
If the woman is healthy and there are no pathologies in the pelvic area, then the injected contrast liquid should completely remain in the recess of the abdominal cavity (more precisely, between the rectum and the uterus). If there is no fluid there, but it is found in the fallopian tubes and the uterus itself, it means that the patency of the tubular organs is seriously impaired.
Increased diameter
One of the possible pathologies detected during ultrasound of the fallopian tubes is their expansion (scientifically called hydrosalpinx).
Important! Often the disease is a consequence of fluid accumulation, the development of inflammation or impaired blood circulation.
What causes the fallopian tubes to become dilated? The reason may be:
- Hydrosalpinx, both simple and follicular. The first leads to an enlargement of the pipe in only one cavity and occurs in a mild form, but is dangerous with a high probability of complications. Therefore, it is so important to identify the disease in time and completely treat it.
- Salpingitis is an inflammation that occurs in the tubular organs of the uterus.
- Enlargement of the isthmus of the tube.
Which method is better?
Tubal patency is checked for all women diagnosed with infertility. For each patient, the treating gynecologist prescribes the examination method that will help and suit her. But, of course, each type of examination has its positive and negative sides.
Surgical methods for treating infertility require the use of anesthesia, this is a significant burden on the body. A woman must undergo a series of mandatory tests that will show whether she is ready for this stress. Therefore, it is preferable to choose hysterosalpingography or hydrosonography, these are non-surgical diagnostic methods.
The advantage of these methods is that immediately after the examination the patient receives the result. The procedure does not require pain relief and does not cause any complications. The disadvantage of HSG is that the body receives radiation exposure, and the liquid contrast that is injected into the uterus contains iodine, which can cause allergies.
The positive side of the procedure is the absence of exposure to x-rays; discomfort is also minimal.
Laparoscopy is used when other methods have been unsuccessful. But this type of examination assumes rapid recovery and ensures that new adhesions may appear after a long time. Hysteroscopy provides a wide view of the pelvic organs, which increases the accuracy of the diagnosis.
At the time of hysteroscopy, the doctor can immediately eliminate the cause of infertility and also perform a biopsy. The absence of scars after this operation is an important advantage. The least reliable is the Perturbation method; this method of examination is used quite rarely these days.
Advantages and disadvantages of UZGSS
Like any diagnostic procedure, examination of the fallopian tubes has positive and negative aspects, related both to the patient’s comfort during the ultrasound and to its information content.
Minuses
The UZGSS procedure has a number of disadvantages:
- due to spasmodic compression of the uterus and tubes or a large volume of injected fluid, the patient may feel discomfort;
- The cause of obstruction of the gel or saline solution can be not only adhesions, but also severe spasms.
pros
This diagnostic study has clear advantages over other methods for determining tubal obstruction:
- When planning a pregnancy, conception is possible in the same cycle, because unlike X-ray examination, GSS does not lead to irradiation of the genital organs. Therefore, the question “which is better - X-ray or ultrasound examination” does not arise here.
- In some cases, the procedure is a stimulus for the onset of gestation , since the contrast liquid leads to the washing away of the derivative that clogs the tubes. It also separates thin adhesions and activates the work of the fimbria, which captures and promotes the egg.
- The patient does not require hospitalization or a long wait for diagnosis.
- The procedure will not take much time .
- At the same time, it allows us to identify pathologies of the uterus.
- It is performed non-invasively, that is, without punctures of the abdominal skin.
- Painlessness allows you not to resort to anesthesia for ultrasound examination.
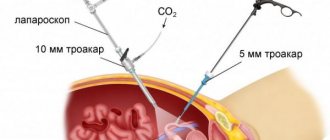
Diagnostic laparoscopy
Laparoscopy is a modern surgical procedure, the essence of which is to study the condition of organs. In this case, large incisions are not made on the abdominal wall. During the examination, the doctor directly sees the patient’s organs and their condition.
During diagnostic laparoscopy, the doctor can refute or confirm the alleged diagnosis, namely patency of the fallopian tubes.
As a rule, diagnostic laparoscopy is performed in a hospital. But the procedure is quite serious in terms of preparation for it, because the patient is under anesthesia during the examination.
On what day of the cycle is the study carried out?
The passage of eggs is most often checked after menstruation. Laparoscopy is prohibited during critical days and 3 days before them. If this examination is carried out to determine the reasons for the lack of conception or to check the fallopian tubes, the ideal period would be 15-25 days of the cycle.
that is, after ovulation, and in some operations laparoscopy is performed immediately after menstruation.
Preparing for the study
Laparoscopy quite effectively eliminates obstruction of the fallopian tubes and, according to statistics, in 90% of cases, thanks to this intervention, the patient manages to become pregnant soon.
Since any type of laparoscopy is an surgical intervention, it requires a complete examination of the patient’s body:
- UAC (2 weeks);
- OAM (2 weeks);
- biochemical blood test to study the level of all indicators (2 weeks);
- flora smear (2 weeks);
- blood coagulogram (2 weeks);
- analysis for sexually transmitted infections (3 months);
- smear for oncocytology (1 year);
- ECG (1 month);
- Ultrasound of the pelvic organs (1 month);
- analysis for blood group and Rh factor;
- fluorography (1 year).
On the eve of the examination, you must refuse food for several hours. In the cycle in which the procedure takes place, protection with oral contraceptives is prohibited.
How does the procedure work?
Diagnostic laparoscopy must be performed in a hospital , since the procedure requires the use of anesthesia.
- Before the operation, the patient is examined by an anesthesiologist and decides what anesthesia to use (as a rule, diagnostic laparoscopy is performed under local anesthesia).
- After administering anesthesia to the patient, a small incision of up to 1 cm is made in the abdominal wall.
- Through this incision, carbon dioxide is introduced into the abdominal cavity to push the walls of the abdominal cavity apart. In this way, the doctor creates space for a better view of the organs.
- In addition to this hole, 2 more punctures are made at the locations of the fallopian tubes, measuring 5-10 mm.
- An optical system (laparoscope) is inserted into the first hole , which is equipped with a backlight, thanks to which the doctor can observe the condition of the organs on the screen.
- Through two other incisions, instruments are inserted, with the help of which surgical manipulations will be carried out.
- To check the patency of the fallopian tubes during diagnostic laparoscopy, the doctor first examines the condition of the uterus and tubes.
- Fluid enters the uterine area.
- After the operation is completed, the punctures are sutured.
The duration of diagnostic laparoscopy depends on the complexity of the case; on average, the examination lasts from 40 minutes. up to 1.5 hours.
Decoding the results
The result of laparoscopic diagnosis is visible to the doctor before the examination is completed. The good condition of the pelvic organs is visible from the smooth abdominal wall covering the internal organs. The correct shape of the uterus and fallopian tubes, their size and anatomical position also indicate the absence of tumors, fibroids and other developmental anomalies. With inflammation, the organs become enlarged and their color changes.
The absence of adhesions can be seen after the fluid from the fallopian tubes exits into the abdominal cavity.
Recovery
Compared to any other operation, the recovery period after diagnostic laparoscopy is very short. The stitches are small, so healing occurs quite quickly. As a rule, after 2 days the patient is discharged.
In the postoperative period, the woman is prescribed antibacterial drugs to avoid suppuration of the sutures. A couple of days after the examination, the patient is allowed physical activity , this will speed up the recovery process.
After any type of laparoscopy, the patient should abstain from sexual activity and physical activity for a month.
Reviews
On the Internet you can find different reviews from patients about this procedure. Most women agree that assessing tubal patency was not painful .
Some say that during the examination they experienced practically nothing.
But there are also patients for whom the procedure left the most unpleasant memories - they were in so much pain that they had to resort to the help of antispasmodics or painkillers.
Such a variety of reviews indicates how individual everything is in the context of this examination, because each woman has a different pain threshold.
Transvaginal hydrolaparoscopy (Fertiloscopy)
Transvaginal hydrolaparoscopy (THL) is a modern method for diagnosing infertility. TGL differs from diagnostic laparoscopy in that once a pathology is detected, it cannot be immediately eliminated.
On what day of the cycle is the study carried out?
The patency of the fallopian tubes is checked immediately after ovulation, that is, on the 15th day of the cycle. This type of examination is not carried out during menstruation and 3 days before it. If a hysteroscopy procedure is planned at the same time, the optimal period for the start of the cycle, namely 7-10 days, immediately after menstruation.
Preparing for the study
Most often, the TGL procedure does not require hospitalization and is well tolerated.
Despite this, before the examination it is necessary to undergo a number of tests:
- UAC (2 weeks);
- OAM (2 weeks);
- biochemical blood test (2 weeks);
- coagulogram (2 weeks);
- blood to establish blood group and Rh factor;
- blood test for HIV and hepatitis (3 months);
- blood test for syphilis (3 months);
- flora smear (2 weeks);
- smear for oncocytology (1 year);
- fluorography (1 year);
- ECG (1 month);
- feces for helminth eggs (1 year).
In addition, on the eve of the examination, you need to cleanse the intestines, and on the day of the procedure, refrain from solid food. In the cycle in which TGL is planned, it is prohibited to take oral contraceptives.
How does the procedure work?
THL examination is carried out under local anesthesia as follows:
- The doctor opens access to the cervix using gynecological speculum.
- A painkiller is injected into the cervix.
- A puncture is made in the back wall of the vagina, into which a probe with a light bulb and a camera is inserted.
- Then saline solution is injected into the abdominal cavity, this greatly facilitates the conditions for examination.
- After examining the condition of the uterus and ovaries, the doctor inserts a camera into the fallopian tubes and assesses their level of patency.
- At the end of the examination, fluid is pumped out of the abdominal cavity and the probe is removed. The vaginal puncture heals after a few days, no suturing is required.
It should be noted that this procedure is impossible if the uterus is bent towards the rectum. The gynecologist sees this anatomical feature during a preliminary examination.
Decoding the results
You do not need to wait long for results after the procedure. The doctor currently sees on the screen the condition of the organs and the patency of the fallopian tubes. After completion of the examination, the result is printed and given to the patient for further observation by a gynecologist.
But even if any pathology is detected, it is impossible to eliminate it immediately; this is an exclusively diagnostic method. As a rule, if tubal obstruction is detected during TGL, the patient is prescribed laparoscopy, during which the adhesions are removed.
Recovery
The examination lasts no more than 40 minutes, immediately after completion the patient returns to her usual rhythm of life. Transvaginal laparoscopy is a painless diagnostic procedure that does not require painkillers.
Contraindications for the study
Ultrasound to check the patency of the fallopian tubes is a fairly simple procedure. It does not involve invasive intervention and does not require complex preparation for implementation. But even such a simple examination has a number of contraindications.
It is strictly forbidden to perform an ultrasound:
- with uterine bleeding;
- gynecological diseases occurring in acute or chronic form;
- violations of the vaginal microflora;
- inflammatory diseases of the pelvic organs;
- pregnancy;
- tumors (benign, malignant) localized in the pelvis;
- infectious pathologies during exacerbation.
Anatomical features of the organ
The uterus is an unpaired hollow muscular organ that is located near the bladder and rectum. The fallopian tubes are hollow, paired organs that are an important part of the female reproductive system. They are located in a horizontal plane and originate from the lateral surfaces of the uterine fundus. Their length is up to 11-13 cm. The tubes are located in the folds of the peritoneum and are narrow cylindrical channels, which are covered from the inside by ciliated epithelium, and from the outside by a connective tissue membrane.
According to static data, the length of the left pipe is slightly less than the right one. The fallopian tubes are such tiny structural elements of a woman's reproductive system that most modern ultrasound machines simply cannot visualize them. These organs are in a constant “floating” state, which also makes it difficult to examine them in detail using ultrasound. In most cases, if the pipes are not visible, this indicates the absence of pathological changes.
Complications and consequences
After an ultrasound or x-ray examination, unpleasant consequences are extremely rare. In rare cases, an allergic reaction may be a possible complication. It should also be taken into account that with several attempts in a row to restore patency by washing or blowing, there is a risk of overstretching of the pipes and inflammation of the appendages.
Many, on the contrary, point to the fact that after MSG or HSG, patency results improve and fertility increases significantly.
Degrees of obstruction
When the lumen closes, partial or complete obstruction may occur. In the first case, the organ narrows in a certain place, resulting in an increased risk of ectopic pregnancy.
Localization of the adhesive process
Adhesions form against the background of inflammatory lesions in the organs of the genitourinary system or intestines.
But also a pathological condition can occur after removal of appendicitis, as a result of any surgical intervention in the peritoneal area. Adhesions can form both inside and outside the fallopian tubes, thereby preventing conception.
Is it possible to evaluate pipes at home?
Passability can only be checked in hospitals that have special equipment. Women may suspect a pathology if they have the following characteristic signs:
- disrupted menstrual cycle;
- pain syndrome in the lower part of the peritoneum;
- a feeling of fullness in the right or left side, at the location of the appendages.
Attention! If alarming symptoms are detected, you need to contact a gynecologist and undergo a comprehensive examination.