Hypersegmentation of neutrophil nuclei - what is it?
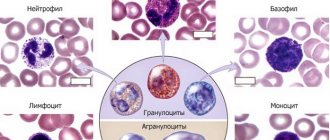
In blood granulocytes during severe infections, the following types of changes in leukocyte morphology have serious prognostic significance: toxogenic granularity of neutrophils, vacuolization of the cytoplasm, Knyazkov-Dele bodies. The presence of at least one of the listed changes indicates the development of bacteremia and generalization of the infectious process. Changes are quantified using the degeneration index
, which reflects the percentage of neutrophils that have toxogenic granularity. If this index exceeds 50%, this indicates a high severity of infection and a serious prognosis. It has been reliably established that the presence of vacuoles in the cytoplasm of neutrophils correlates well with impaired granulocyte function and the presence of bacteremia.
Toxogenic granularity of neutrophils
- coarse granularity of a dark red color, which is detected as a result of physicochemical transformations of the cytoplasm under the influence of an infectious agent, which reflects a violation of the processes of neutrophil maturation, or is the result of the absorption of toxins. The causes of toxogenic granularity of neutrophils are purulent-septic diseases, lobar pneumonia, scarlet fever, and disintegration of tumor tissues after radiation therapy.
Vacuolization of the cytoplasm
- detected in sepsis, abscesses, acute liver dystrophy.
Taurus Knyazkova-Dele
- are large white-blue areas of cytoplasm of various shapes that do not contain specific granules. Knyazkov-Dele bodies are detected in inflammatory diseases, infections, sepsis, and burns.
Hypersegmentation of neutrophil nuclei
- 5 or more segments in the nuclei of neutrophils. Causes: folate deficiency and B12 deficiency anemia, hereditary constitutional feature.
Pelger anomaly
- a dominantly inherited disorder of granulocyte maturation, which is characterized by a decrease in the segmentation of neutrophil nuclei.
Pseudo-Pelger anomaly
- decreased segmentation of granulocyte nuclei. The abnormality of nuclear maturation is based on a violation of nucleic acid metabolism. Causes: myeloproliferative diseases, agranulocytosis, multiple myeloma, tuberculosis. Pseudo-Pelger anomaly is transient, and after the end of the disease, pseudo-Pelger leukocytes disappear.
Leukolysis cells (Botkin-Gumprecht shadows)
- dilapidated nuclei of lymphocytes with remnants of nucleoli, found in chronic lymphocytic leukemia.
ATTENTION! The information provided on this site is for reference only. Only a specialist doctor in a specific field can make a diagnosis and prescribe treatment.
Degenerative changes in neutrophils occur under various pathological conditions (infections, exposure to chemicals, diseases of the hematopoietic apparatus, exposure to penetrating radiation, ingestion of radioactive substances, etc.) and can affect both the nucleus and the cytoplasm. These include:
Symptoms and consequences
If the normal levels of toxic granularity are exceeded, the human body begins to respond to disease processes with certain complex reactions.
Most often, pronounced toxic granularity of neutrophils is a symptom of the development of a pathology in which there is an increase in the number of granulocytes in the blood. This may also indicate a shift in the leukocyte formula to the left.
With the growth of degrading neutrophils, the patient begins to develop bacteremia and generalization of the infectious process occurs. If the number of neutrophils with pathological changes exceeds 50% in septic or purulent diseases, or this indicator increases, then the prognosis becomes unfavorable.
The patient exhibits symptoms of the disease that caused the disorder - lobar pneumonia, radiation poisoning, etc. Chills and toxic granularity of neutrophils often accompany each other.
The doctor must take into account the dynamics of changes in the patient’s blood parameters, adjust treatment if necessary, and prescribe certain medications. A rapid increase in neutrophil concentration is not a good sign.
Therapy for toxic granulation directly depends on the success of treatment of the underlying pathology that provoked changes in blood cells, since toxigenic changes are nothing more than its consequences. In this case, the doctor can only monitor the leukocyte formula.
Toxic (toxogenic) granularity of neutrophils
Toxic (toxogenic) granularity of neutrophils is a coarse granularity, similar to azurophilic granules. Its formation occurs inside the cell as a result of physicochemical changes in the protein structure of the cytoplasm under the influence of intoxication products. Observed during infectious or inflammatory processes. May be accompanied by the presence of cytoplasmic vacuoles and Dele bodies.
Toxic granularity of neutrophils often appears before nuclear shift. Its increase in purulent-septic diseases, lobar pneumonia and a number of inflammatory diseases indicates the progression of the pathological process and the possibility of an unfavorable outcome. Toxic granularity of neutrophils appears in large quantities during the disintegration of tumor tissue under the influence of radiation therapy. Toxic granularity is most pronounced in lobar pneumonia during the period of resorption of the inflammatory infiltrate, in scarlet fever, septicopyemia, peritonitis, phlegmon and other purulent processes. It is especially important in the diagnosis of an acute abdomen (for example, gangrenous appendicitis, which occurs with a slightly elevated body temperature and, often, in the absence of leukocytosis).
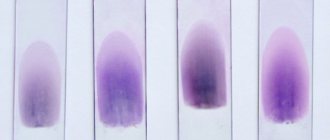
Toxic granularity of neutrophils can be detected by staining smears in the usual way. However, even with high-quality staining, dusty toxogenic granularity may not be visible, and if the smear is repainted (even slightly), the specific granularity of neutrophilic granulocytes can be mistaken for toxogenic. Therefore, to identify toxic granularity of neutrophils, special staining methods have been proposed, of which the most common and accessible is the Freifeld method
Freifeld method
The following dyes are used to color the smear:
- 1 g of basic fuchsin is dissolved with low heating in 15 g of ethyl alcohol (96), cooled and 100 ml of a 5% carbolic acid solution is added.
- 1% aqueous solution of methylene blue.
The working mixture is prepared immediately before painting, as it is unsuitable for storage. Add 7 drops of the first paint to 20 ml of tap water, mix, add 5 drops of the second paint and mix again.
Blood smears, fixed for 3 minutes with methyl alcohol, are stained for 1 hour with the prepared working dye mixture, and then washed off with water and dried. A preparation already stained according to Romanovsky can be stained using this method without prior bleaching.
As a result of this staining, bluish granules of various sizes are revealed in the cytoplasm of neutrophils (from dust-like to flocculent) depending on the severity of the pathological process. The number of cells with toxic granules is calculated as a percentage (per 100 neutrophil granulocytes). The analysis also indicates the grain size (pulverized, fine, medium, coarse, flake).
Toxic granularity of neutrophils (photos)
What affects the quality of the analysis?
In order to obtain a reliable analysis result, it is necessary to prepare for it; laboratory doctors must strictly follow the methodology. The quality of analyzes is influenced by the following factors:
- compliance with the rules of preparation for analysis;
- taking blood for testing only in the morning on an empty stomach;
- the use of anticoagulants, which will prevent blood clotting; without it, a repeat sample will be necessary;
- timely execution of analysis;
- using the correct technique prescribed by the doctor;
- compliance with sterility rules and the use of high-quality reagents.
Preparing for a blood test for neutrophils
To obtain reliable results, the doctor must warn the patient to follow the rules before the study:
- applying a diet 3 days before the study, which excludes fatty, fried, spicy, salty foods;
- lack of physical activity 1 day before testing;
- Alcohol consumption is prohibited 1 day before the test, smoking is not allowed on the day of the test;
- the analysis is carried out before prescribing therapy;
- 5 days before the study, all medications that will not change the patient’s condition are discontinued;
- The test is taken only in the morning on an empty stomach, immediately after waking up.
Neutrophil norms in women, men and children
The number of neutrophils depends on the age of the person. The table shows normal values.
| Age | The norm of neutrophils, % of total immune cells |
| From birth to 1 year | 10-55 |
| From 1 year to 7 years | 20-60 |
| From 8 to 14 years | 30-70 |
| From 15 to 18 years old | 45-70 |
| Adult men and women | 47-75 |
What do low numbers mean?
A low number indicates cell death during the body’s defense. This is a sign of disease progression.
After complete recovery, the number of neutrophil granulocytes should return to normal. If this does not happen, the reasons may be the following processes:
- immunodeficiency state;
- a long-term illness that reduces the activity of the immune system;
- severe infections such as tuberculosis, brucellosis, when the body’s defense system is not able to cope with the infection on its own;
- a malignant neoplasm of the red bone marrow, which reduces the production of formed elements.
Find out why neutrophils are low during pregnancy.
What do high scores mean?
Neutrophilia is a condition of the immune system in which an increased number of neutrophil granulocytes is formed. The reasons for this are the following conditions:
- penetration of a viral, infectious, parasitic agent into the body;
- formation of a malignant neoplasm;
- chronic diseases;
- tissue damage (fractures, cuts, dislocations);
- poisoning with chemicals, poison, expired products, alcohol;
- insect bites, snake bites.
Learn more about why neutrophils are elevated during pregnancy.
Hyposegmentation of the nucleus (pelgeroid, pseudo-pelger anomaly)
Hyposegmentation of the nucleus (Pelgeroid, pseudo-Pelger anomaly) - an increase in the number of bisegmented neutrophils, as well as band neutrophils and neutrophils with a round nucleus. In this case, chromatin has a dense structure. Occurs in leukemia, myeloproliferative diseases, MDS, agranulocytosis, multiple myeloma, myxedema, malaria, infectious diseases, and when taking certain medications. Their formation is associated with the blockade of enzymes responsible for nuclear segmentation. It should be distinguished from the Pelger anomaly (with pelgeroid, changes in neutrophils are inconsistent, unlike the Pelger anomaly).
Pelgeroid, pseudo-Pelger anomaly (photos)
general information
To a lesser extent, this type of leukocyte takes part in the “antiviral program”. Their counting is part of a clinical blood test. The leukocyte formula contains the percentage of neutrophils.
Experts divide this type of leukocyte into segmented and band. In the first case, we are talking about mature cells with a segmented nucleus. In the blood of a person who does not suffer from any pathologies, segmented neutrophils are contained in larger quantities.
In the second case, we are talking about cells that have not yet matured. Their core is shaped like a stick. They do not have a segmented core. Also, band neutrophils have some immaturity of basic functions.
Other degenerative changes of neutrophils
Ring-shaped kernels - the kernels are shaped like a ring. Observed in severe alcoholism.
Chromatinolysis - during decay, chromatin loses its normal structure - dissolves. The nucleus is painted in a light color, its contours are preserved.
Karyolysis is the dissolution of only part of the nucleus while maintaining its normal structure. In places of dissolution, the core loses the ability to be painted with basic colors, its contours are fuzzy and blurred.
Fragmentosis is a process in which individual fragments (particles) are separated from the nucleus. They can be connected to the nucleus by thin filaments of basichromatin.
Pyknosis is a compaction of the basicchromatin of the nucleus. The core becomes dark and structureless. Cell size decreases. The process of pyknotization extends either to the entire nucleus or to its individual sections or segments.
Karyorrhexis is the disintegration of the nucleus into separate parts, unconnected, round in shape and sharply pyknotic, dark, structureless formations.
Karyorrhexis (micrographs)
Cytolysis is the breakdown of a cell. Cytoplasm is often absent. The core loses its usual structure, its contours are blurred. In severe cases, only remnants of the kernel and granularity can be detected.
Microscopic features
When toxic granularity appears, the appearance of neutrophils changes, which is clearly visible in an electron microscope.
Morphological signs of neutrophils in TND:
- 2-3 times more than a mature red blood cell
- Low nucleus to cytoplasm ratio (more cytoplasm than nucleus)
- The nucleus is mature and divided into 3-5 lobes connected by thin threads of chromatin
- Nucleols are absent
- Darker (red/purple) granules are easily visible (similar to primary granules noted in promyelocytes)
The appearance of coarse granularity in the cytoplasm
If you compare a toxically altered cell with a normal one, one significant difference will emerge - next to the usual granules of neutrophils, toxic granularity appears, which looks like larger rounded formations of dark red and purple color. The appearance of additional granules in neutrophils is due to coagulation (gluing) of cytoplasmic protein, which under a microscope looks like the appearance of additional granularity against the background of existing granules.
Literature:
- L. V. Kozlovskaya, A. Yu. Nikolaev. A textbook on clinical laboratory research methods. Moscow, Medicine, 1985
- Fred J. Shiffman. "Blood Pathophysiology". Per. from English - M. - St. Petersburg: "BINOM Publishing House" - "Nevsky Dialect", 2000.
- Guide to practical exercises in clinical laboratory diagnostics. Ed. prof. M. A. Bazarnova, prof. V. T. Morozova. Kyiv, “Vishcha school”, 1988
- Manual of clinical laboratory diagnostics. (Parts 1 - 2) Ed. prof. M. A. Bazarnova, Academician of the USSR Academy of Medical Sciences A. I. Vorobyov. Kyiv, “Vishcha school”, 1991
- Handbook of Clinical Laboratory Methods. Ed. E. A. Kost. Moscow “Medicine” 1975
Increased neutrophil levels
Only a good doctor can answer the question of how to increase neutrophils in the blood. A special diet plays a fundamental role. Without this, it is impossible to increase the level of these leukocytes even while taking medications prescribed by a doctor.
The diet is based on reducing carbohydrate intake. Instead, the human body should receive abundant amounts of proteins and vitamins.
Particular attention should be paid to products containing folic and ascorbic acid. You should also include foods containing the amino acids lysine and choline in your diet.
A person is advised to limit the consumption of meat products. This is especially true for pork and beef. Also, you should not focus on eating animal liver.
It is recommended to replace meat with seafood and chicken eggs. Also, a person is shown high-quality red caviar. You are allowed to treat yourself to a glass of good dry red wine. But if you are allergic, it is better to avoid alcohol.
Rate this article:
(votes: 1 , average: 5.00 out of 5)
Loading...
Related posts:
- What do low neutrophils indicate and how can you help the patient?
- Elevated neutrophils: what is the cause of this condition and how can it be eliminated?
Leukocytosis and neutrophilia
In most cases, the concepts of leukocytosis and neutrophilia are synonymous. They are characteristic of the inflammatory process. The duration and severity of the inflammatory process, as well as the response of the bone marrow to infection will determine the degree of neutrophilia and the possibility of immature forms (band neutrophils, metamyelocytes and myelocytes) appearing in the blood - a shift to the left. A shift to the left is indicated when the number of band neutrophils exceeds more than 1.0x10⁹/ l, which is typical for acute inflammatory processes. A less pronounced shift to the left (0.3–1.0x10⁹/l) is characteristic of chronic and granulomatous processes. There are regenerative and degenerative shifts of the nucleus to the left. With a regenerative shift, mature neutrophils predominate in the blood; it is assessed as an adequate response of the bone marrow to a damaging effect. With a degenerative shift of the nucleus to the left, the number of immature neutrophils is greater than mature ones, and the total number of leukocytes is within normal limits or reduced. A degenerative shift indicates an acute inflammatory process that exceeds the ability of the bone marrow to supply the need for mature neutrophils. At the beginning of the inflammatory process, neutrophilic leukocytosis and a pronounced nuclear shift to the left occur. As the segmented neutrophils that existed in the bone marrow maturation and storage depot are depleted, band neutrophils and metamyelocytes are released. Over time, myeloid hyperplasia in the bone marrow will increase the production of neutrophils. The release of mature cells into the blood will increase and the severity of the left shift will decrease. Once tissue inflammation has stabilized at a sustained low level, the bone marrow should achieve a sufficient rate of neutrophil production so that most of them can mature before being released into the circulation. Thus, during a chronic inflammatory process, leukocytosis is not observed, and a shift to the left is insignificant or absent. Chronic inflammation is difficult to detect with a general blood test. If the need for neutrophils is very strong, hyperplasia of the granulocytic lineage may be observed in the bone marrow, without being reflected in the form of neutrophilia in the peripheral blood. For example, with pyometra in dogs, there may be a normal or slightly elevated white blood cell count and a moderate (to strong) shift in the white blood cell count to the left. After surgery, such animals may experience rebound neutrophilia, reflecting the degree of neutrophilia of the granulocytic lineage. It typically takes about a week for these dogs' blood profiles to return to normal. Persistent neutrophilia should be investigated for the presence of a focus of chronic inflammation, abscess, necrosis, and tumor. In such cases, it is recommended to carefully examine the joints (polyarthritis), the central nervous system (meningitis), the cardiovascular system (endocarditis) and the gastrointestinal tract (ulcerative lesions).
Differential diagnosis of neutrophilic leukocytosis includes:
- Inflammation; – Exposure to corticosteroids (stress, glucocorticoid therapy, Cushing’s syndrome); – Impact of adrenaline (excitement, fear, physical activity); – Leukemia.
Types of neutrophil granulocytes and their ratio
During its development, the neutrophil undergoes certain changes. First, a nucleus is formed inside the cells, resembling a rod in outline; such blood cells are called band neutrophils. As the nucleus grows, it is divided by cords into several segments (up to 5 separate chambers are formed); such cells are called segmented neutrophils.
For the diagnosis of diseases, not only the total number of neutrophil leukocytes is important, but also the ratio of their mature and immature forms. Normally, band neutrophils make up the vast majority of all leukocytes - more than 70%, and segmented neutrophils in a blood test do not exceed 5% of the total number of leukocytes.
Cytological examination in gynecology
Cytological analysis in gynecology refers to microscopic examination of samples taken from the vagina and cervical canal to determine the typical cellular composition.
This diagnosis allows doctors to draw conclusions about the presence of inflammatory processes, precancerous diseases or cancer in the patient’s reproductive organs.
Unlike histological examination, the cytological method is non-invasive. That is, when taking biological material there is no need to perform a biopsy or puncture, and the integrity of the tissue is not compromised at all.
Samples taken using a fingerprint or swab are analyzed. To obtain accurate results, you must carefully follow the rules for preparing for the examination.
Cytological analysis usually takes no more than a day to complete. If a precancerous condition or an oncological process is discovered, invasive diagnostic techniques are used to clarify the diagnosis - biopsy.
Cytology is especially important when biopsy is contraindicated and when examining a large number of patients (when it is necessary to identify women at risk for developing malignant pathology).
Cytology smears are not taken during menstruation. If you need to evaluate the presence of atypical cells, you should not conduct the analysis during inflammation of the vagina and cervix.
- Do not douche.
— Do not use topical medications (suppositories, ointments, etc.).
- Wait until your period ends.
- Do not urinate three hours before taking a smear.
— Abstain from sexual intercourse for two days before the study.
If there is an inflammatory process in which a lot of secretion is released, the disease must be treated and a control smear done to confirm recovery. And only after this does it make sense to perform a cytological analysis.
An oncological smear is taken by a gynecologist when examining a patient. First, using mirrors, the doctor examines the condition of the vagina, examines the entrance to the cervical canal and the mucous membrane of the cervix.
Then, material is taken for analysis from three areas (vagina, cervical canal, cervical inlet) using a special brush. The procedure takes very little time and does not cause patients any pain.
The collected material is placed on a glass slide, evenly distributed and, after drying, transferred to a medical laboratory. There, the smear is stained with special substances and examined under a microscope.
— Cell sizes and their structure.
— Number of cells (per certain unit of area).
- Mutual arrangement.
- Shape of the epithelium.
— The presence of pathological changes in cells.
Structures of stratified squamous epithelium of the cervix
Structures of multilayered squamous epithelium of the vaginal mucosa
A - basal layer (a - basal cells, b - parabasal cells) B - intermediate layer, C - superficial layer; on the right are individual cells of the corresponding layers of the vaginal epithelium.
After the material collection procedure, the patient can immediately return to her normal activities. Normally there should not be any discomfort, since the brush cannot injure the tissue.
True, there is a possibility that a small blood vessel will be affected. Then, within 1-2 days after the analysis, slight bleeding (streaks) will be observed. This phenomenon should not cause concern to a woman.
The cervix of a healthy woman is covered with columnar epithelium, and the vagina is flat. As for the vaginal microflora, it is not cocci, but rods.
Some indicators depend on the phase of the cycle - karyo-pyknotic and acidophilic indices, basal and parabasal cells, the number of leukocytes. They provide information about the functioning of the ovaries.
Class 1. Absence of pathological changes in the examined material. The cells are of normal size and shape and are correctly located.
Class 2. The morphological norm of some cellular elements is reduced, which is a sign of inflammation or infection. This result may be a sign of vaginosis.
Class 3. The material contains single cells with disturbances in the structure of the nucleus and cytoplasm (dysplasia or hyperplasia). The number of such pathological cells is small. The patient is sent for repeat cytology.
Class 4. The examined smear reveals cells with malignant changes in the nucleus, chromatin and cytoplasm. These pathological changes indicate that the patient has a precancerous condition.
Class 5. The presence of a large number of atypical cells in the smear (they are much more than normal). In this case, the initial stage of cancer is diagnosed.
- Normal. The absence of pathology does not have any special designation.
— Vaginosis, koilocytosis – HPV.
- Cervical dysplasia depending on the degree - CIN I, CIN II or CIN III.
— Cervical cancer — Carcinoma (pax).
— CBO. Normal indicators, no pathological changes.
- Cytogram of inflammation. Indicators indicating the development of the inflammatory process (cervicitis).
— Leukocyte infiltration – increased number of leukocytes. This is a sign of vaginosis, exocervitis or endocervitis.
READ MORE: Acetowhite epithelium cytology is normal
— Koilocytes – the presence of cells indicating HPV.
— Proliferation – acceleration of cell division. This condition is typical for the inflammatory process in the uterus. With strong proliferation, advanced inflammation occurs.
— Leukoplakia – the smear contains pathologically altered (but not cancerous) cells.
- Metaplasia - one type of cell is replaced by another. It is considered normal for patients who were treated for non-cancer pathologies of the uterus during menopause.
— Dysplasia is a precancerous pathology.
— ASC-US – the presence of altered squamous epithelial cells of unknown etiology. It most often occurs in patients over 45, when estrogen production decreases.
- AGC - changes in cylindrical cells, which may indicate vaginosis or some other diseases. This result requires additional clarifying diagnostics.
— L-SIL – the presence of a small number of atypical non-cancerous cells. In this case, the patient is referred for further examination (biopsy and colposcopy).
— ASC-H – pathological changes in cells that indicate a precancerous pathology or an incipient oncological process.
- HSIL is oncocytological (modified squamous cells present). Such patients are given immediate treatment to prevent degeneration into a malignant tumor.
- AIS - This abbreviation indicates that cylindrical malignant cells have been identified. With such results, urgent treatment is necessary.
If pathologically changed cells are detected in a smear, the laboratory assistant will definitely indicate this in a written report specifying the type of changes. If there are no special designations in the analysis transcript, then, in all likelihood, the smear corresponds to the norm.
An accurate diagnosis cannot be made based on this test alone. To determine the nature of the pathology, the gynecologist needs to compare the results of different examinations.