The liver is the largest gland. All processes occurring in the organ are provided by enzymes. In the blood, liver enzymes may be higher or lower than normal if the disease develops. Because of this, blood testing for this indicator is an important diagnostic method. The activity of liver enzymes can be used to assess the condition of the entire organism, which is why they are often of great interest to doctors.
Groups of liver enzymes: excretory and endocrine
Enzymes regulate all metabolic processes in the body
In medicine, there are three groups of liver enzymes. The substances of each of them are responsible for a certain amount of functions in the body, which is why the analysis examines the levels of the components of each group.
- Excretory. The main representative of the group is alkaline phosphatase. The enzymes included in the group are present in bile. An assessment of their level is required to determine the quality of the biliary system.
- Incretory. The group includes enzymes AST, ALT, GDH, GGT, LDH. When they deviate from the norm, they indicate pathologies leading to tissue destruction.
- Secretory. The group includes prothrombinase and cholinesterase. Substances take part in blood clotting processes, maintaining them at a normal level.
Based on the results of the study of the material, depending on the degree of disturbance in the blood picture of liver enzymes, an additional examination may be prescribed to clarify the cause of the deviations.
Stool analysis
Stool analysis helps determine abnormalities in the enzymatic function of the stomach, liver, and pancreas.
The color of stool is given by a special pigment – stekrobilin. Change in stool color is one of the main symptoms of disease. When the structural composition of stool changes, the analysis can reveal pus, blood, and even parasites. The detection of a significant amount of protein compounds in a stool analysis means pancreatic dysfunction or stomach problems. Microscopic examination of feces determines the main elements of feces: muscle fibers, plant fiber, neutral fat, fatty acids and their salts, leukocytes, red blood cells, intestinal epithelial cells, malignant tumor cells, as well as mucus, protozoa, helminth eggs.
Causes of elevated liver enzymes
Fatty hepatosis is the cause of elevated liver enzymes
A slight increase in indicators usually occurs due to taking medications that are eliminated from the body with the participation of the liver; as well as from external toxic influences. Typically, these events do not require treatment and are considered normal. In case of significant excess of the norm, pathology occurs. Most often the phenomenon is observed in such cases:
- inflammatory liver diseases of a viral nature;
- fatty liver disease;
- primary cancerous lesions of the liver;
- inflammatory processes in the pancreas;
- myocardial tissue infarction;
- myocarditis of infectious nature;
- heart failure.
Elevated levels of liver enzymes are not the only diagnostic indicator. Additional examination is required for an accurate diagnosis.
Many blood proteins are enzymes
Changes in specific enzymatic processes can be the cause or consequence of various pathological conditions. Most enzymatic processes are localized inside cells, but determining the activity of enzymes in the extracellular environment (serum, plasma, saliva, urine) has diagnostic significance and is called enzyme diagnostics .
To correctly interpret the results, the doctor needs to know the basics of enzyme diagnostics, have information about the tissue localization of the enzyme, its activity in various cell compartments, the effect of medications taken by the patient on the enzyme activity, the stability of the enzyme during storage, the presence of isoenzyme forms, etc.
Reasons for changes in enzyme activity in the blood
The degree of change in the activity of cellular metabolic enzymes in the blood serum depends on the weight of the affected organ, the distribution of enzymes between tissues, and the localization of enzymes in intracellular organelles. During inflammatory processes, cytoplasmic enzymes are the first to leave the cell; as the disease progresses, cell necrosis is observed and organelles are destroyed. Enzymes from mitochondria and lysosomes are found in plasma. For example, alanine aminotransferase (ALT, AlAT) is localized in the cytoplasm, and aspartate aminotransferase (AST, AST) is both in the cytoplasm and in mitochondria, glutamate dehydrogenase is a mitochondrial enzyme.
Increased activity in blood serum may be the result of accelerated processes:
- synthesis – alkaline phosphatase for rickets, hepatitis,
- cell necrosis - AlAT, AST, LDH, CK in myocardial infarction, acid phosphatase in prostate adenoma, lipase, amylase in pancreatitis,
- decreased excretion - alkaline phosphatase in cholelithiasis,
- increasing the permeability of cell membranes - AlAT, AST, LDH in hepatitis.
The decrease in activity is caused by:
- a decrease in the number of cells secreting the enzyme (cholinesterase in liver cirrhosis),
- insufficiency of synthesis,
- increased enzyme excretion,
- inhibition of activity as a result of the action of proteinases.
In some cases, establishing the relationship between changes in the activity of individual enzymes and obtaining unique enzyme spectra of blood has a certain diagnostic value. In this case, it is possible to establish reliable enzymatic symptoms of individual diseases.
For example,
- acute hepatitis is characterized by a sharp increase in the activity of alanine and aspartate aminotransferases and aldolase,
- myocardial infarction is accompanied by an increase in the activity of lactate dehydrogenase, creatine kinase, aspartate aminotransferase,
- with mechanical jaundice, an increase in the content of alkaline phosphatase is characteristic without a large increase in the activity of aminotransferases and aldolase.
Serum enzymes
- Enzymes secreted into the plasma and performing specific functions in it are true plasma enzymes. In plasma their activity is much greater than in organs (ceruloplasmin, pseudocholinesterase , lipoprotein lipase , protein factors of blood coagulation systems , fibrinolysis and kininogenesis , renin ). A decrease in the activity of these enzymes in plasma will indicate a decrease in the synthetic ability of cells or the accumulation of inhibitors in the blood plasma.
- Enzymes that are not typical for plasma are organ-specific. It is the determination of the activity of these enzymes that is most often used to verify the diagnosis and control treatment. There are two groups of organ-specific enzymes:
1. Enzymes of cellular metabolism ( indicator ) - their activity increases sharply in the blood plasma in the event of a violation of the permeability of cell membranes or their alteration:
For example,
- with changes in the heart muscle, there is an increase in the activity of the cardiac isoenzyme creatine (CK-MB), lactate dehydrogenase 1 and 2 (LDH-1 and LDH-2), aspartate aminotransferase ,
- disorders of skeletal muscles - muscle isoenzyme creatine kinase (CK-MM), alcohol dehydrogenase ,
- bone tissue – alkaline phosphatase (ALP), aldolase (ALD),
- prostate gland – acid phosphatase ,
- hepatocytes - alanine aminotransferase , glutamate dehydrogenase , cholinesterase , sorbitol dehydrogenase ,
- biliary tract - alkaline phosphatase , γ-glutamyl transpeptidase (γ-GTP).
2. Enzymes excreted into the excretory ducts of the bile ducts, pancreatic and salivary ducts. Normally, the activity of such enzymes in plasma is much lower than in cells and has a constant value ( α-amylase , pancreatic lipase Studying the activity of these enzymes allows us to judge the functioning of the corresponding organ.
Enzyme Activity Units
Enzyme activity is expressed in katals (1 katal = 1 mol/s), in units of activity (1 E = µmol/min or 1 U, 1 unit - standard international unit of enzyme), in derivatives from other units of measurement (mol/s×l , µmol/s×l, µmol/h×ml, mg/h×ml, in µkat/l).
0
Signs of elevated enzyme levels
Loss of appetite is a warning sign
Increased levels of liver enzymes in the blood rarely go unnoticed. With this phenomenon, the patient in most cases seeks medical help due to the following conditions:
- chronic fatigue;
- pronounced decline in performance;
- pain in the liver area;
- change in appetite;
- itching of the skin of varying intensity;
- yellow eyes and skin;
- frequent nosebleeds;
- the formation of bruises even with minor mechanical impact.
As the condition worsens, weight loss and an increase in the main symptoms are added.
Lipid metabolism indicators
Indications for laboratory testing of lipid metabolism are the diagnosis of the following diseases:
- atherosclerosis and its complications,
- IHD - coronary heart disease,
- myocardial infarction,
- stroke.
Increased concentrations of lipids in the blood significantly increase the risk of developing vascular complications in atherosclerosis. The level of substances largely depends on the quantities in which they are supplied with food. Therefore, to correct lipid status, a low-fat diet is often prescribed.
Analyzes allow you to determine the content of the main lipids - cholesterol and triglycerides. For transport in the blood, they bind to proteins - apoproteins. Such combinations are called lipoproteins. There are several types, differing in the level of triglycerides, cholesterol and apoproteins.
As part of a laboratory study of lipid metabolism, the concentration and ratio of all indicators of lipid status are determined:
- cholesterol,
- triglycerides,
- high and low density lipoproteins,
- apolipoproteins A1 and B.
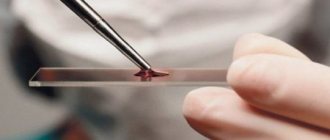
A blood test is performed for diagnosis. Biomaterial is given on an empty stomach in the morning. Before the study, you must refrain from eating for 12 hours. In the morning you can only drink water. The blood collection procedure is painless and takes only a few minutes.
The study is carried out over 3 days. The results are available on our website after filling out a special form. You can also pick up the report in person or use a courier delivery service. The cost of the study is indicated on the website. Collection of biomaterial is paid separately.
Causes of decreased liver enzymes
A decrease in enzymes may occur with liver metastases
A drop in enzyme levels is observed less frequently than an increase. Deviation from the norm to the lower side may indicate the following pathologies:
- cirrhosis;
- metastasis of cancer tumors to the liver;
- stagnation of bile in the ducts.
A non-pathological reason for a decrease in enzyme levels is a woman taking a number of hormonal oral contraceptives for a long time. In this case, only a doctor can decide on the possibility of continuing to take a drug that has affected the functioning of the liver. Usually contraceptives are replaced.
Liver enzyme analysis
The liver is a special organ. It is one of the largest internal organs in humans. The liver has the property of regeneration, it cleanses our body of poisons and helps cope with metabolism. Carrying out a huge amount of work, the liver can become unusable. Therefore, it is very important to monitor the level of concentration of liver enzymes - these are indicators of its functionality.
An enzyme or enzyme is a protein molecule that allows you to increase the rate of chemical reactions occurring in the human body. Scientists who study enzymes are called enzymologists.
Indications and preparation for analysis
When detecting liver pathology, enzyme analysis is mandatory
Indications for donating blood for liver enzyme testing are:
- diagnosis of liver diseases;
- monitoring the condition of the liver during long-term use of a number of medications;
- determining the degree of liver damage in cirrhosis;
- monitoring the effectiveness of treatment in the presence of liver diseases;
- suspicion of liver pathology;
- period of pregnancy planning;
- stage of preparation for any operations.
To obtain accurate data, proper preparation for the analysis is required, which requires the exclusion of fatty, fried foods and alcohol a week before the analysis; informing the doctor about taking any medications; donating blood on an empty stomach. The last meal before the analysis can be no later than 10 hours. Before donating blood, you can only drink clean water.
Result
The norm for biochemical analysis of residual nitrogen is from 14.3 to 28.6 mmol/l.
An increase in residual nitrogen may indicate:
- acute or chronic renal failure;
- renal dysfunction;
- heart failure;
- dehydration;
- obstruction of the urinary tract;
- bleeding from the upper digestive tract;
- severe bacterial infections;
- decreased adrenal function (Addison's disease).
A decrease in residual nitrogen levels may be a symptom of:
- liver failure;
- viral, toxic and autoimmune hepatitis;
- celiac disease.
The importance of the AST indicator
An increase in the plasma concentration of this enzyme can be regarded as a harbinger of:
- Myocardial infarction.
- Hepatitis A.
- Initial stages of angina pectoris.
- Pancreatitis.
- Cancerous pathologies of the liver.
- Rheumatic carditis.
- Excessive power loads.
- Heart failure.
Given the origin of plasma enzymes, AST may increase due to injured muscle tissue, severe heat stroke, or as a side effect after cardiac surgery.
A decreased AST reading may indicate:
- Deficiency of vitamins in the body.
- Complications after severe infectious and viral diseases.
- Liver rupture.
Note! In women, the permissible AST level is up to 32 U/l, in men – up to 43 U/l.
Causes of liver disease
According to the World Health Organization, today more than 2 billion people suffer from various liver diseases - and this is a third of the adult population of the Earth.
Experts attribute the main reasons for the increase in the incidence rate to: poor lifestyle, stress, bad habits (smoking and alcohol), taking a large number of medications at the same time, and sudden weight loss. All these factors contribute to the overload of the organ with cholesterol and fat, resulting in its destruction.
Viral hepatitis also plays a role, and you can become infected in the most unexpected ways. For example, if you ate with dirty hands (hepatitis A) or visited a nail salon or medical facility where they are dishonest about sterilizing instruments (hepatitis B and C). The virus multiplies, adapts, and then causes serious inflammation of the organ tissue.
Effect of prostatic acid phosphatase
The place of origin and localization of CF is considered to be the prostate gland (PG). If the result of a blood test shows the active activity of this enzyme, the patient may be diagnosed with:
- A prostate cancer tumor that has already metastasized.
- Benign prostatic hypertrophy.
- Prostatitis.
- Infarction of the pancreas.
- Complications from prostate treatment.
Many examples have proven that this indicator enzyme does not show much activity in the early stages of any pancreatic diseases. That is why specialists prefer to analyze the functioning of CF after determining the diagnosis. The purpose of this action is to monitor the outcome of therapeutic measures.
Pigment metabolism indicators
A biochemical test for bilirubin allows you to determine the condition of the liver and biliary tract. It is carried out according to the following indications:
- liver diseases,
- cholestasis,
- hemolytic anemia,
- diagnosis of jaundice of various origins.
As part of a biochemical blood test, two indicators are assessed.
- Direct bilirubin is synthesized from free bilirubin due to binding with glucoronic acid. By its concentration one can judge the condition of the biliary tract and liver and identify the causes of jaundice. The enzyme content increases when there is a violation of the outflow of bile, hepatitis and other pathologies. A significant release of bilirubin into the blood causes yellowing of the skin and sclera of the eyes, and darkening of the urine.
- Total bilirubin is a breakdown product of myoglobin, hemoglobin and cytochromes. It is formed in the cells of the liver and spleen and is one of the main components of bile.
There is a normal value for bilirubin content: indirect - up to 17.1 µmol/l, direct - up to 4.3 µmol/l. Exceeding the concentration may indicate the following violations:
- vitamin B12 deficiency,
- liver cancer,
- hepatitis, primary cirrhosis,
- formation of gallstones,
- Gilbert's disease
- poisoning - medicinal, alcoholic or toxic.
To make an accurate diagnosis, additional tests are prescribed.
Before taking a bilirubin test, you should undergo simple preparation. The procedure is carried out strictly on an empty stomach, at least 8 hours must pass after the last meal. The day before, give up alcohol and fatty foods, reduce physical activity and try to avoid stress. Following these recommendations allows you to obtain the most reliable data.
Inorganic substances, macro and microelements
A biochemical blood test for trace elements is a study that allows you to comprehensively assess the condition of the body, the functionality of systems and organs, identify symptoms of diseases or determine which vitamins and minerals a person lacks.
Most often, biochemical tests are taken to determine the content of vital (essential) elements in the blood:
- calcium;
- potassium;
- sodium;
- chlorine;
- magnesium;
- phosphorus;
- copper;
- gland;
- zinc
A blood test for microelements allows you to:
- reflect the functional state of organs and systems;
- identify an active inflammatory process;
- establish the fact of a violation of water-salt metabolism;
- identify rheumatic processes;
- correctly diagnose and prescribe effective treatment that will be effective;
- prevent the development of diseases.
Knowing the microelement profile of the body is important for the correct prescription of vitamin-mineral complexes, since some initially beneficial microelements in high concentrations become hazardous to health. An imbalance of vitamins and minerals can lead to:
- decreased immunity;
- diseases of the skin, hair, nails;
- allergies, bronchial asthma;
- diabetes, obesity;
- hypertension;
- diseases of the cardiovascular system;
- scoliosis, osteoporosis, osteochondrosis;
- blood diseases;
- intestinal dysbiosis, chronic gastritis, colitis;
- infertility, decreased potency in men;
- delayed mental and physical development.
You can take a biochemical blood test for microelements at any of our laboratory offices. The study should be carried out on an empty stomach; it is recommended to stop taking medications 3 days before. You can get additional information by phone.
Importance of aldolase indicator
This compound ensures the correct flow of energy metabolism in the human body. Aldolase is considered a tissue-specific enzyme because it is present in all tissues of our body. Acceptable values for an adult are no more than 3.3 U/1.
If the analysis table shows increased aldolase activity, this can be caused by:
- Heart attack.
- Injured muscle tissue.
- Infectious, viral and mechanical liver diseases.
- Pancreatitis.
- Neoplasm of a malignant nature.
- Inflammation and breakdown of muscle fibers.
- Hemolytic anemia.
- Infectious mononucleosis.
- Advanced stage of pneumonia.
- Schizophrenia.
- Excessive force load.
Preparation
A biochemical blood test requires special preparation.
- You need to take the test strictly on an empty stomach, after 8-12 hours of fasting, you can only drink still water.
- You should not change your diet for 3 days, but try to exclude fatty, spicy and fried foods.
- It is recommended to stop playing sports 3 days before the test.
- You should take a biochemical test in the morning, from 7 to 11 am.
- You should stop taking medications 3 days in advance; if this is not possible, notify your doctor.
- It is advisable to take tests in the same laboratory
Why is SDH important?
Sorbitol dehydrogenases are the indicator enzymes of blood plasma, the main location of which is the liver. If SDH levels are elevated, a specialist can immediately regard this as a clinical symptom of liver pathologies. According to international standards, the biochemistry of blood plasma for SDH enzymes should show an activity of 1-3 U/l.
Increased activity of SDH is influenced by:
- Acute stage of viral hepatitis.
- A sharp exacerbation of chronic hepatitis.
- Hepatic coma.
- Obstructive jaundice.