Diagnostic results
Osteochondrosis of the cervical spine
Having received the results of the study, the doctor carefully examines what the x-ray of the cervical spine showed. Based on the results of the images, you can see deviations or features in this department:
- consequences of traumatic injury to the spinal column in the neck area. These may be dislocations, bruises, displacements, cracks;
- transformation of the spine in the neck area;
- growths that form around the vertebral artery in the area of the first cervical vertebra are Kimmerle's anomaly. This pathology is congenital, so it can be diagnosed even in young children. When the vertebral artery is compressed, the blood supply is disrupted;
- degenerative-dystrophic changes, for example, cervical osteochondrosis;
- inflammatory pathologies that provoke irritation of the intervertebral nerve. This condition provokes cervical radiculitis;
- the presence of an abnormal bone formation, for example, a sphenoid vertebra;
- curvature of the vertebrae due to the proliferation of bone tissue. Such pathologies include spondylosis;
- osteoporosis in the cervical spine;
- metabolic disorders;
- kyphosis in the cervicothoracic segment;
- tumors localized in the cervical region;
- disc hernias and protrusions.
Is it possible to see osteochondrosis on an x-ray?
A common cause of pain in the spine is degenerative diseases, which include osteochondrosis. The pathology is characterized by changes in the intervertebral discs, which lose their elasticity, become deformed and become thinner. This leads to a narrowing of the intervertebral space and compression of the nerve bundles. The initial diagnosis for clinical manifestations is radiography. What will an x-ray show for osteochondrosis, and at what stage of development of the pathology can changes be visualized?
Types of X-ray examinations for osteochondrosis
There are several types of diagnostics that complement each other and determine what the exact picture of osteochondrosis looks like. A common method is x-ray diagnostics of the spinal column. With its help, gross structural disorders or changes in the thickness of the intervertebral discs are determined. Osteophytes and deformities of individual vertebrae are also detected. The results are visible on the picture or monitor screen.
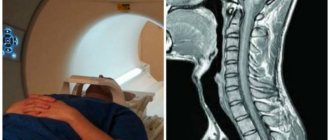
Myelography is used to determine the condition of the spinal canal. To do this, a contrast agent is injected into the spinal cord, and after its distribution, an image is taken. This allows us to identify the presence of intervertebral hernias or the presence of displacements of the internal cavity. Magnetic resonance imaging is a very accurate diagnostic method and makes it possible to detect osteochondrosis at the initial stage of development, even with a mild course.
Diagnostics will determine the extent of bone tissue damage.
Why do specialists write out a referral specifically for an x-ray if there is a suspicion of osteochondrosis?
When it comes to diagnosing osteochondrosis (regardless of the stages of its development), many doctors recommend the X-ray method. The essence of this method is to x-ray the body using ionizing radiation, which allows you to take a kind of “photo” of the human skeleton. X-ray diagnostics is actively used in various fields of medicine, for example, in traumatology, as well as in dentistry and surgery.
The main advantages of why fluoroscopy and radiography are so often used are that such diagnostics are cheap and quite informative. Of course, with the help of an X-ray it will not be possible to qualitatively visualize soft tissues (for this, magnetic resonance or computed tomography with a contrast agent is used), but the image in question shows enough to identify osteochondrosis.
It is worth noting that signs of osteochondrosis can be seen on x-rays only from the second stage of development of the disease (the only exception is the lumbar region). The fact is that lesions of the intervertebral discs at the first stage are extremely small. In fact, at the first stage, a picture is almost never taken, because the disease is not accompanied by severe pain and other symptoms, and the patient most often simply does not even know about it.
X-rays also help determine the presence of other diseases caused by osteochondrosis, such as scoliosis.
What the doctor won't see in the picture
X-ray images obtained during the examination of the spine clearly show the development of osteochondrosis.
Osteocondritis of the spine
In the picture this process is shown as follows:
- decreased height of intervertebral discs,
- deformation of each vertebra,
- indirect symptoms of hernia development,
- dystrophic changes in the structure of the spinal column.
With the development of this disease, the patient experiences severe pain in the back area. Often, osteochondrosis affects the cervical, thoracic and lumbar regions. In these cases, there is a curvature of the spine, which changes posture.
Disorders in the spine
X-ray examination, although informative, does not give a complete picture of the presence of pathologies in the cervical area. The technique has been used for a long time and in attempts to modernize X-rays, new types of diagnostics have appeared, however, some pathologies are still unattainable for X-rays today.
Even with a clear image, a doctor may not identify the following pathologies:
- small hematomas;
- minor cracks or fractures;
- small neoplasms.
In this case, computed tomography can better diagnose such small, difficult-to-visualize abnormalities, and if you need to obtain information about the condition of soft tissues, then magnetic resonance imaging is the right choice.
Despite these features, radiography is widely used as a diagnostic measure, as it provides valuable information about the condition of the musculoskeletal system.
Radiography will be a valuable test for diagnosing osteochondrosis of the cervical spine, which is difficult to visualize without special techniques. This pathology is quite common because it is associated with sedentary work and physical inactivity. Using radiography of the spine, pathology can be diagnosed in a timely manner and treatment can begin.
What you need to know about osteochondrosis?
First, you should consider what this disease actually is, because most people’s knowledge ends with the fact that spinal osteochondrosis is a serious problem that must be dealt with from the very beginning, otherwise you will face chronic ailments, as well as pain and others dire consequences. In fact, this disease should be understood as degenerative and dystrophic lesions associated with intervertebral discs, and they also extend to the tissues of the vertebrae themselves.
If serious negative dynamics are observed, then experts note that a simple intervertebral problem has serious consequences, for example, atrophy occurs that spreads to muscle tissue, sensitivity is impaired, and problems associated with the functions of internal organs appear. Let us immediately mention that the incurable condition of osteochondrosis of the cervical spine or in any other part of the spine does occur, but only in situations where a person tries to ignore the symptoms and does not begin treatment at all.
If osteochondrosis is suspected, an x-ray of the desired part of the spine is prescribed in direct and lateral projections.
The main reason for the development of the disease in question is considered to be constant, and most importantly, uneven load. For example, a person may get used to carrying a bag on one shoulder, and this is typical even for people whose profession requires them to carry objects whose weight exceeds 15-20 kg. Also, nowadays, people often sit incorrectly, choose mattresses that are unsuitable for sleeping (the surface should not be too soft), and wear “wrong” shoes (we are talking about shoes whose soles are anatomically incorrect). Here are the main predisposing factors to the development of osteochondrosis:
- physical inactivity;
- constant exhaustion of a nervous national character;
- sedentary lifestyle;
- genetic predisposition to this disease;
- any disorders associated with the musculoskeletal system;
- overweight or even obesity;
- constantly wearing uncomfortable shoes;
- injuries related to the spine;
- flat feet;
- various age-related degenerative processes associated with impaired blood supply to the spine;
- physical stress;
- disorders associated with the body's metabolic processes;
- smoking;
- poor posture, which is especially dangerous in childhood, when a person is just growing;
- problems of a professional nature, that is, risk factors associated with a person’s profession;
- problems associated with disturbances in the absorption of nutrients;
- dehydration;
- poor diet, lack of essential vitamins;
- pregnancy, and especially if it has multiple births.
An image of the spine is one of the informative diagnostics of various abnormalities and ailments.
Here is a list of the main clinical manifestations of the disease (symptoms can vary greatly depending on the type of disease):
- severe pain, manifested in various parts of the body (for example, osteochondrosis of the cervical spine is always accompanied by pain that affects the cervical spine, and if we are talking about thoracic osteochondrosis, then pain will be observed in the thoracic region);
- the appearance of discomfort in these areas, as well as some stiffness of movement (it is worth mentioning that such symptoms always develop gradually);
- numbness of the limbs, and this never depends on the location of the problem (the case may concern the lumbar region, the thoracic region, or any other part of the spine);
- heartache;
- muscle hypotension;
- disorders associated with sensitivity of the limbs;
- constant dizziness or even headaches;
- excessive fatigue.
Note! You can talk endlessly about this disease, but it is important to understand that it is very dangerous, so you need to act as quickly as possible. If you notice some of the previously listed symptoms or any other disorders, then contacting a specialist should be prompt. And if there are risk factors, it is important to eliminate them if possible, for example, diversify your diet, refuse dangerous work, quit smoking or stop carrying a bag on one shoulder.
Carrying out the procedure
The study is carried out after examining the patient and collecting a medical history, which are the main methods for identifying osteochondrosis. X-rays of the lumbar spine, like others, are taken in several projections, which allows you to see signs of osteochondrosis. When examining the lower back, the patient is asked to arch his back as much as possible.
If radiography of the cervical or thoracic spine is performed, then such manipulation is not required. However, examination of the neck requires photographs in frontal, posterior and lateral projections. In order for the diagnosis to be reliable and osteochondrosis to be visible on x-rays, 3 days before the procedure, the patient is advised to follow a diet with limited dairy products, vegetables and carbonated drinks, as they provoke fermentation in the intestines, and this impairs visualization.
Indications and contraindications for radiographs
Indications for conducting a study to identify osteochondrosis on x-ray are:
- pain in the lumbar region, back, cervical spine;
- limitation of mobility in various parts of the spinal column;
- poor posture: scoliosis, kyphosis, pathological lordosis;
- manifestations of radiculopathy (damage to the lumbosacral region), intercostal neuralgia (damage to the thoracic segment), plexopathy (damage to the cervical region);
- with cervical osteochondrosis, severe headaches, dizziness, darkening of the eyes, tinnitus;
- trophic disorders due to atrophy of the nerve roots (impaired skin sensitivity, the formation of muscle atrophies, the formation of skin ulcers).
Manifestations of osteochondrosis can already appear in adolescence. The peak incidence occurs in females aged 35-40, when degenerative changes are provoked by hormonal changes. With age, the development of pathology becomes more frequent due to a smaller supply of nutrients and calcium leaching. Regenerative mechanisms are depleted, disc destruction occurs faster.
Contraindications to radiography are common to all types of examination. The examination is strictly prohibited for pregnant women; research in children and lactating women is limited. This is due to the ionizing effect of X-rays.
Carrying out radiography
X-ray (x-ray) is the study of human body organs using x-rays.
In this case, the image of the object under study is projected onto sensitive film or photographic paper.
The doctor receives a projection image of the organ by passing X-ray rays through it.
What is X-ray
Obtaining an image on a special sensitive film is based on the fact that X-ray radiation is attenuated when passing through certain tissues.
As a result, the film produces an image with varying degrees of intensity. The X-ray film produces a so-called averaged image. This suggests that in order to obtain the desired image, heterogeneous organs are examined.
It is necessary that the photographs are taken in at least two projections. This is due to the fact that a three-dimensional object is being examined, and an x-ray is a flat, two-dimensional image.
The location of the pathological area can be seen in just two projections.
The power of X-ray radiation depends on the organ being examined and the size of the patient. The recording of images in the Russian Federation is carried out, as a rule, on sensitive film.
Today, this type of diagnosis remains one of the most popular. This is due to its simplicity, low cost and high information content.
Compared to magnetic resonance imaging and computed tomography, spinal radiography is more accessible.
So, what does an x-ray of the spine show:
- curvature of the spine (lordosis, kyphosis, scoliosis, etc.);
- osteochondrosis;
- changes in intervertebral joints;
- spinal subluxations;
- compression injuries;
- spinal tumors;
- infectious lesions of the organ (for example, as a result of tuberculosis).
However, radiography does not allow one to see the pathology of the intervertebral discs.
Comparison with other diagnostic methods
X-ray of the spine is the most commonly used diagnostic method for osteochondrosis. But the information content of this method in relation to soft tissues is low. For uncomplicated forms of the disease, x-rays are sufficient. If clinical manifestations do not fully correlate with radiographic findings, extensive evaluation using other modalities may be required.
MRI and CT are most often additionally used. Computed tomography, like x-rays, is based on the use of x-rays, but thanks to special shooting conditions and computer processing of the results, the picture is more informative. CT scan clearly visualizes the intervertebral discs and surrounding soft tissues. MRI has no less diagnostic value. This is also a high resolution method.
But MRI and CT are less accessible than x-rays, and therefore are not routine tests. It is advisable to start the examination with an x-ray, and if the clinical picture matches the x-ray, and there is a positive response to treatment, then this can be limited. If some other processes are suspected, as well as complications of osteochondrosis, CT and MRI may be used for a more accurate diagnosis.
Signs of osteochondrosis and stages
Displacement of the spinal discs occurs as a result of the destruction of cartilage tissue.
There are several typical radiological symptoms of the disease, depending on which the severity of structural changes in the spine is determined:
- Damage to nearby vertebrae.
- Change in the height of the intervertebral gap.
- Insertion of the disc into the spinal body.
- Destruction of the endplates.
- Determination of foci of ossification in atypical places or osteophytes.
- Impaired bone density with diagnosis of degenerative processes.
- Fusion of adjacent vertebrae, which is typical for a severe stage of the disease.
The degree of severity of degenerative-dystrophic processes in the spinal column according to X-ray diagnostic data is determined in 3 stages of the development of osteochondrosis:
- First. It is characterized by a decrease in the thickness of the cartilaginous plate by one third of normal.
- Second. Causes cartilage to thin by half.
- Third. Looks like complete erasure of cartilage tissue.
3 criteria are used:
- Instability when, during flexion-extension, an adynamic position of the motor structure of the column is observed due to its destruction.
- Hypermobility, defined as severe displacement of a vertebra in the affected area with a decrease in the intervertebral space and destruction of adjacent structures and the posterior parts of the spinal canal. The condition is assessed at maximum flexion-extension of the spinal axis during a functional test.
- Hypomobility, characterized by fusion of adjacent structures with minimal motor activity during flexion-extension. The height of the discs between the vertebrae changes greatly.
What does diagnostics reveal?
Most clearly, x-rays reveal changes in the bone structures of the spinal column - the vertebral bodies and their processes. Cartilaginous formations and intervertebral discs are less clearly visualized. Therefore, radiography is a standard test for diagnosing osteochondrosis.
X-ray of the spine allows you to confirm the diagnosis, determine the stage of the disease and differentiate it from other possible pathologies. Similar complaints manifest themselves as pathological (compression) fractures of the spine, spondyloarthrosis, spondylolisthesis and some other diseases.
Since osteochondrosis begins with changes in the vertebral discs, and they are softer in structure than bones, their image in the pictures is not always contrasting. Therefore, the initial stages of the disease are often not determined or are indicated only by indirect signs.
In addition, the main complications of osteochondrosis - pain, pinched nerve root, compression of a vessel or disc herniation - affect the surrounding soft tissue. Such complications are also difficult to assess using x-rays. Therefore, what osteochondrosis looks like during fluoroscopy does not always correlate with the brightness of the clinical picture. Doctors divide the signs of osteochondrosis on an x-ray into groups depending on the stage of the disease.
Description of the image: what osteochondrosis looks like on an x-ray
Osteochondrosis on x-ray has several manifestations. The stage of the disease is determined by the degree of their severity. All criteria by which osteochondrosis can be diagnosed are divided into 2 main groups:
- Criteria indicating a decrease in the shock-absorbing properties of the discs (decrease in their height, the presence of bone growths, skewness of the vertebral bodies, compaction of the endplate, the appearance of signs of arthrosis and other radiological symptoms).
- Signs of impaired motor function (smoothness of physiological curves, spinal deformity such as hyperlordosis or scoliosis, pathological mobility of the vertebrae revealed during functional tests, segment blocking and several other manifestations).
All criteria are assessed together. If one of the manifestations is weakly expressed and the other is strongly expressed, then the overall severity of the disease is usually determined in accordance with the most pronounced symptom.
How to determine the degree from an image
To unify the assessment of the severity of pathology, several classifications of osteochondrosis are used based on the nature of changes on X-ray photographs. One of them is the Zecker classification:
- The first stage is unexpressed changes in the physiological curve (for example, smoothing of the cervical lordosis).
- The second stage is more pronounced changes. These include: straightening lordosis, changing the width of the intervertebral space, the appearance of exostoses on the posterior or anterior surfaces of the vertebrae, deformation of the uncinate processes.
- Severe osteochondrosis (third stage). All changes are preserved, and a pronounced narrowing of the intervertebral foramina is added to them.
- The most pronounced osteochondrosis. Signs of narrowing of the spinal canal appear (due to massive exostoses directed posteriorly).
In the third stage of osteochondrosis, persistent pain and sensory disturbances associated with compression of the nerve root often develop. Pain appears earlier, but in the early stages it is often caused by a reflex muscle spasm. At the fourth stage, symptoms associated with compression of the spinal cord may appear.
How does the image affect treatment?
Topical diagnosis of changes in the spine and assessment of their severity is important for developing patient management tactics. Pronounced changes, accompanied by compression of the root or narrowing of blood vessels, may serve as a basis for surgery. Surgery is also necessary if the functions of the spinal cord are impaired.
Conservative therapy also requires radiological monitoring. In the treatment of lumbar osteochondrosis, massage and exercise therapy are often prescribed. Before starting the course, it is important to first assess whether there are any contraindications to these procedures. If physical procedures are used, then the area of the back on which the therapeutic effect is applied is accurately determined from the images.
An X-ray of the spine is also necessary to assess the effectiveness of therapy. Dystrophic processes in bones and intervertebral discs are irreversible. therefore, regression of these changes cannot be expected on x-ray.
Most complications of osteochondrosis (pain, root pinching, muscle spasms) affect soft tissues. The positive dynamics on their part during the treatment process can be assessed using X-rays by indirect signs. For example, when a muscle spasm is eliminated, the width of the intervertebral gaps can be leveled, asymmetry can go away, and the physiological curvature of the spine can be restored.
Diagnostics with functional tests
During an X-ray examination with functional tests, doctors have a unique opportunity to study the most mobile parts of the cervical vertebrae. It is carried out with the aim of diagnosing pathological mobility between the vertebrae or, conversely, blocking of the vertebrae.
When performing a functional test, doctors receive the following results:
- see the displacement of the vertebrae relative to each other;
- can establish the degree of changes in the wall of the spinal canal in front and determine the nature of these deviations.
For example, a study is informative if a patient has osteochondrosis at an early stage. Once the disease is diagnosed, it is already possible to take measures to stop the pathological process and treat the consequences of destructive changes.
Photo with functional tests
Symptoms on X-ray
In the later stages, a regular photograph reveals the following symptoms and signs:
- narrowing of the gap between the vertebrae;
- Pommer's nodes - multiple notches with a wavy, clear border, indicating prolapse of the disc into the vertebral body;
- marginal growths at the corners of the vertebral bodies (osteophytes) in the affected area - the addition of spondylosis due to friction between the vertebrae, deprived of the disc layer;
- vertebral displacement or listhesis;
- ischemic changes (thinning) of soft tissues;
- instability of the spinal column.
Pommer's knots
X-ray of the neck in children
X-rays of the cervical spine are performed not only in adult patients, but also in children. Children are susceptible to injuries in the neck area, and will also be necessary if the doctor suspects the presence of congenital pathologies.
There is no need to worry that x-rays may cause discomfort or side effects - children tolerate the examination well, especially x-rays in two or three projections. X-rays through the oral cavity are more difficult - this type of examination is recommended only for young patients over four years of age.
The following pathologies are most often diagnosed in children:
- subluxation;
- orthopedic deviations;
- muscle hypertonicity;
- abnormal mobility of the vertebrae in the cervical area;
- birth injuries.
With correct and timely diagnosis, doctors prescribe treatment for patients, and in most children, defects in the cervical vertebral area are removable.
Is it useful to have an MRI?
We have already mentioned magnetic resonance imaging earlier, but in case of osteochondrosis, whether it is better to choose MRI or X-ray may be a question. In fact, magnetic resonance imaging can also be useful, because such a safe examination of internal organs can complement the picture built up after radiography with information about the condition of muscles and soft tissues. In the process associated with the destruction of intervertebral discs, serious inflammation begins in almost all surrounding tissues, and MRI is excellent for identifying such manifestations.
Complex treatment of osteochondrosis
Effective treatment of osteochondrosis requires an integrated approach, including:
- Diet therapy. Proper nutrition with adequate water regime slows down degenerative processes. Products containing gelatin are useful for discs: jellied fish, jellied meat, jelly.
- Drug treatment. The main groups of drugs necessary to relieve attacks of radiculoneuropathy against the background of osteochondrosis changes are steroidal and non-steroidal anti-inflammatory drugs. Muscle relaxants are used to reduce muscle spasms. They help reduce inflammation and swelling around the nerve roots and reduce pain. Then a course of restorative treatment is carried out using drugs - chondroprotectors containing hyaluronic acid, chondroitin sulfate and glucosamine. Calcium preparations are used to strengthen bone structures and prevent degeneration of bone structures.
- Therapeutic exercise. It is necessary to normalize motor activity, as well as body weight, since obesity increases the load on the intervertebral discs and accelerates their destruction. Physical education helps normalize blood circulation in the affected area and strengthen the muscle corset.
- Physiotherapeutic treatment. With the help of electrotherapy, ultrasound, magnetic therapy, acupuncture and other methods, it is possible to reduce the doses of medications and administer medications locally.
- Massage. It is carried out during the recovery period to enhance blood circulation and activate regenerative processes.
Osteochondrosis is a common disease that affects the intervertebral discs. The primary diagnosis of pathology is radiography of the area. Unfortunately, the method is not very informative and is capable of visualizing pathology during functional diagnostics only at the second stage. Then clarification is required using modern tomographic studies.
Thoracic osteochondrosis: what is it?
Thoracic osteochondrosis is a disease in which degenerative changes in the spine develop in the thoracic region. The most common type of osteochondrosis is the cervical form; the thoracic form is not so common. However, it is a form quite dangerous to health; against the background of thoracic osteochondrosis, many complications can begin to develop.
The ICD-10 code for osteochondrosis of the thoracic spine is M42; this number includes all types of degenerative diseases of the spinal column.
With the development of osteochondrosis of the thoracic region, symptoms do not appear immediately. The thoracic spine is inactive compared to the cervical or lumbar, so pronounced manifestations of the disease become noticeable only in later stages. In general, the thoracic form is not common, since this part of the spine is the least susceptible to injury and various diseases.
At the same time, the degenerative processes occurring during osteochondrosis are quite extensive. They affect cartilage and connective tissues, muscles, which leads to many complications and other diseases. The chest form of the disease can be extremely dangerous to health without proper timely treatment. In some cases, the chest form is combined with the cervical form; with several forms of osteochondrosis, the disease can be especially severe.
Indications
An X-ray of the thoracic spine is done if the following pathological conditions are suspected:
- spinal injuries;
- scoliosis, kyphosis;
- osteochondrosis;
- infection of the vertebrae;
- congenital developmental pathologies;
- tumors in the chest area;
- intervertebral hernia;
- vertebral displacement.
The indication for X-ray of the thoracic spine is the presence of the following symptoms in the patient:
- chest pain;
- abdominal pain not related to pathologies of the gastrointestinal tract;
- increased pain in the sternum when coughing, taking a deep breath, or sudden movements;
- discomfort, unpleasant sensations in the limbs;
- back stiffness;
- loss of sensitivity, numbness;
- paresthesia of fingers;
- chronic tachycardia of an idiopathic nature;
- difficulty breathing;
- poor posture;
- coughing up blood.
X-ray examination of the thoracic region is also prescribed to identify pathologies of the cardiovascular or bronchopulmonary system, inflammatory processes, and microtraumas.
Symptoms of osteochondrosis
To prevent thoracic osteochondrosis and symptoms, treatment and preventive measures are thought out in advance. Osteochondrosis of the thoracic spine is characterized by bone dystrophy and degeneration. With thoracic osteochondrosis, the composition of the elements of the spine, ligaments, and cartilage changes and is destroyed. The disease causes atherosclerosis, pneumosclerosis, prostate dysfunction and infertility.
- We advise you to read: diagnosis of osteochondrosis.
First, osteochondrosis affects the bones, then the cartilage and muscles. In young people with osteochondrosis of the thoracic region, the musculoskeletal system ages without having time to mature and develop.
Known symptoms of osteochondrosis of the thoracic spine, characteristic of various stages of development of the disease:
- Pressure in the back or chest that interferes with breathing;
- Difficulty turning (tilting) the body;
- Periodic sensations of body numbness;
- Reduced temperature of the lower extremities;
- Itching and burning sensation in the extremities (often in the legs);
- Brittle nails;
- Problems with gastrointestinal tract functions;
- Impaired functioning of the genital organs (decreased potency);
- Nausea;
- Heartburn;
- Migraine-like headache;
- Intercostal neuralgia;
- An unpleasant feeling in the anterior part of the peritoneum;
- Pain in the left side of the sternum, reminiscent of heart pain;
- Reflex tension in the back and chest;
- Acute pain at the level of the liver and gall bladder;
- Sometimes shingles.
The main danger in the treatment of osteochondrosis is that its symptoms are often confused with other diseases.
Signs of thoracic osteochondrosis in women are mistaken for migraine. The emerging signs of osteochondrosis of the thoracic spine in men are due to gastric diseases or problems of the genitourinary system. This leads to erroneous diagnosis and incorrect treatment, since the way thoracic osteochondrosis manifests itself is very similar to the symptoms of many other diseases.
To avoid incorrectly prescribed medical recommendations and not to use medications unnecessarily, it is necessary to consult with several specialists and exclude other diseases. Before you begin drug treatment for osteochondrosis, you need to make sure the diagnosis is correct. For osteochondrosis of the thoracic region, the symptoms and treatment must be appropriate.