Indications
A tomography of the lumbosacral region is recommended in the following situations:
- traumatic injuries (fractures, dislocations, traumatic spondylolisthesis);
- degenerative diseases (osteochondrosis, spondyloarthrosis, disc protrusion or herniation, etc.);
- congenital developmental anomalies;
- primary neoplasia, metastases of tumors of other localizations;
- spinal canal stenosis;
- inflammatory diseases;
- hemorrhages in the spinal cord;
- curvature of the spine (scoliosis, kyphosis, kyphoscoliosis);
- osteoporosis.
CT scan of the POP is prescribed for pain of unknown etiology in the back, lower back, and disturbances in sensitivity and movement indicating possible damage to the lumbar spinal column.
The contrast technique is used at the stage of preparation for surgery, as well as to evaluate the effectiveness of treatment after surgery, chemotherapy, and radiation therapy.
Indications for computed tomography (MSCT) of the lumbosacral spine
- Degenerative dystrophic changes in the spine (osteochondrosis, spondylosis)
- Injuries to the spine (compression fractures) or soft tissues
- Secondary destruction of the vertebrae (infectious or metastatic destruction of the vertebrae)
- Hernias, disc protrusions
- Spinal canal stenosis
- Diagnosis of low back pain of unknown origin
- Compression of roots or spinal cord
- Presence of decreased bone density (osteoporosis)
- Developmental anomalies
- Tumors, both benign and malignant
- Planning of surgical treatment and monitoring the results of surgical treatment.
Contraindications
For non-contrast CT of the spine
- Pregnancy regardless of term. An exception is cases when the examination is prescribed for health reasons.
- Childhood. The use of the technique is permitted in children over 14 years of age if other diagnostic procedures are not informative.
- Weight more than 150-200 kg. The impossibility of the study is due to the limited carrying capacity of the tomograph.
- Inappropriate behavior, hyperkinesis. These conditions interfere with maintaining immobility, which reduces the information content of tomography. The procedure can be performed under sedation or general anesthesia.
- The patient's condition is serious, requiring urgent resuscitation measures.
For contrast CT
- Allergy to iodine preparations.
- Insufficiency of renal function (the method is not used due to the slower removal of contrast in this disorder).
During the lactation period, a woman is advised not to breastfeed for two days after a tomography in order to prevent the contrast agent from entering the child’s body.
A contrast study of the lumbar region is prescribed with caution in cases of bronchial asthma, a history of allergic reactions, severe pathologies of the liver and cardiovascular system, severe hyperthyroidism, pheochromocytoma, and sickle cell anemia.
How to prepare for a CT scan
Preparation includes following a diet. To increase the accuracy of the results of a CT scan of the spinal column, the patient is recommended to avoid eating foods that contribute to the formation of gases in the intestines for two days. Sometimes carminatives are prescribed.
Before the tomography, it is advised to abstain from eating for 6 hours. Before the contrast procedure, the creatinine level is preliminarily assessed.
They take with them all medical documentation related to the spinal disease: referral, extract from the medical history, results of ultrasound, radiography and other additional examinations. Immediately before entering the tomograph room, remove metal objects from yourself.
How do they do it?
Here's how the research works:
- you come at the appointed time, take off all metal products and lie down on a mobile couch;
- the radiologist or laboratory assistant helps you take the correct position and goes into the next room, then the machine starts up and the couch moves inside the arch;
- During the examination, you need to lie still and follow the doctor’s audio commands;
- When the CT scan is completed, the couch will return to its original position and you can leave the office.
Non-contrast tomography technique
The patient is placed on the tomograph table in a supine position, sometimes secured with belts, and asked to remain motionless. Then the doctor goes into the next room.
The table begins to move slowly through the tomograph ring. The ring rotates, cameras mounted on it take successive pictures with a distance of 2-5 mm between slices. The equipment makes a low noise. Native CT and SCT of the lumbar region last up to 5 minutes. During the examination, the doctor and the patient communicate via a two-way communication system.
How the research works
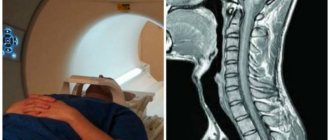
During the scan, the patient is placed in the tomograph tunnel. Before doing this, he needs to remove all metal objects. When the tomograph ring rotates around the extendable table, numerous layer-by-layer images are created. To ensure that the images are not distorted, you must remain still during the procedure. The procedure is absolutely painless and lasts from 5–10 minutes to half an hour (for examination with contrast).
After the scanning is completed, the resulting images are processed on a computer, deciphered by specialists and given to the patient along with a medical report.
Contrast tomography technique
The introduction of contrast increases the information content of the study, especially in cases of tumors and hemorrhages. The duration of contrast CT is 20-30 minutes.
The iodine-containing substance is administered in three ways:
- manually into a vein on the forearm;
- intravenously using a syringe-injector with automatic adjustment of the drug supply (bolus contrast);
- in the lumbar region (myelography).
First, native images are taken. Then contrast is injected, which reaches the spine in 45-60 seconds, and another series of tomograms is made. After the injection, the patient sometimes feels warm, mild nausea or a metallic taste in the mouth; this is normal and does not require interruption of the procedure.
Note! The appearance of shortness of breath, cough, palpitations or severe dizziness may indicate the development of side effects. You should immediately report any symptoms to your doctor.
Research results
After completion of the procedure, the radiologist examines the tomograms and draws up a conclusion, which is given to the patient in writing or on a disk. Preparing results takes up to 1 hour.
The specialist records the changes, but does not make a clinical diagnosis. The final diagnosis is carried out by the attending physician based on complaints, examination data and additional studies.
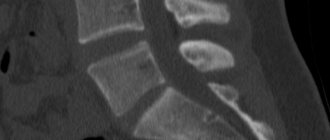
Normally, a CT scan shows no signs of destruction, rarefaction of bone substance, cortical defects, or marginal growths. Physiological lumbar lordosis is revealed, there are no lateral deviations of the spinal axis. The spinal canal is not narrowed, the height of the discs is not reduced, the discs themselves have a uniform structure, their edges do not bulge. Nearby tissues are unchanged.
Violation of one or more of the listed parameters is grounds for contacting a doctor of the appropriate profile.
- If there are signs of a fracture or dislocation, an examination by a traumatologist is required.
- For degenerative changes, narrowing of the spinal canal and other manifestations of neurological diseases, consultation with a neurologist or neurosurgeon is indicated.
- When tumors are detected, an examination by an oncologist is necessary.
- Sometimes a consultation with a rheumatologist is recommended.
Advantages and disadvantages
The advantage is detailed visualization of the solid structures of the spinal column. The technique provides high accuracy in identifying traumatic injuries, degenerative processes, tumors and other pathologies.
The study is non-invasive and painless; it allows you to determine the location, size and configuration of lesions in the lumbar region, make an accurate diagnosis and choose the optimal treatment tactics.
When examining soft tissues and the spinal cord, CT is inferior to MRI (CT shows hard structures better). A significant drawback is the significant dose of X-ray radiation. Taking this into account, the technique is used only when necessary, observing the required time intervals between studies. If this rule is followed, the procedure has a low risk of negative consequences.
What does it show?
- development of degenerative processes;
- foci of inflammation;
- primary and secondary malignant tumors;
- abnormal neoplasms of a benign nature;
- foreign objects;
- compression and trauma-induced fractures, dislocations, ligament ruptures;
- internal bleeding;
- spinal cord compression;
- destruction of the vertebrae due to infections or cancer;
- disturbances in the stability of the structural elements of the musculoskeletal system;
- hernias;
- spondylosis and spondyloarthritis;
- blockage of the spinal canal.
Alternative techniques
Traditional radiography is considered the basic method of examining the lumbar region. Its advantages are accessibility, low cost, disadvantages are insufficient information content when studying bone structures, the impossibility of studying soft tissues and the use of x-rays.
Ultrasound is an inexpensive, safe procedure that can be used without restrictions even when examining children and pregnant women. However, the accuracy of ultrasound diagnostic results is lower than CT.
The best alternative to computer diagnostics is magnetic resonance imaging, which also provides layer-by-layer visualization and the creation of a three-dimensional image. Disadvantages of MRI include high cost and less accuracy in imaging bone and cartilage. The choice between CT and MRI is made depending on the type of pathology.
CT or MRI of the lumbar spine
MSCT is based on the action of x-rays; they are absorbed by body tissues. The intensity of this process depends on the density of the structure of the studied area. Magnetic resonance imaging is carried out based on the operation of the magnetic field, which affects the location of water dipoles in tissues.
With any type of tomography, many layer-by-layer images are obtained in three mutually perpendicular projections. The technique helps to obtain photographs of thin sections of the tissues being studied, which gives an idea of any changes in the shape and structure of the object being studied.
If you need to check the condition of the hard elements of the spinal column, it is more advisable to use a lumbar CT scan. As a result of the study, MSCT will show inflammatory processes, cracks, fractures, displacements, and neoplasms of dense tissue. An MRI will show the condition of the ligaments, muscles and other soft elements of the area being examined.
CT and MRI of the lumbosacral spine, performed with the use of a contrast agent, will help assess the quality of blood supply to tissues in this area, identify the presence of tumors and morphological changes.
Magnetic resonance imaging is safe for the patient. But the prices for MRI are much higher than the cost of computed tomography, so the choice of diagnostic method in each case is individual, depending on the presence of contraindications and indications for the study.