Ultrasound of the parathyroid glands is a non-invasive diagnostic method that provides general information about the condition of the organ. The parathyroid glands, shaped like four small beans, are located on the posterior surface of the thyroid gland. Using ultrasound, you can visually assess their size, structure and outline. The examination is completely painless and makes it possible to identify the type of pathology and prescribe a suitable treatment regimen. The procedure is prescribed for symptoms indicating a malfunction of the organ.
Anatomy of the parathyroid gland
The parathyroid glands are 4 small compacted tissue formations that are located on the back wall of the thyroid gland. Dimensions: 6 mm long, 4 mm wide and 2 mm thick. The parathyroid gland consists of elongated or oval epithelial bodies that have a smooth surface. In their structure, parathyroid cells are the structural and functional units of the gland. The color of the parathyroid gland is pale, becoming yellowish with age. The dissected organs are transparent in appearance.
Anatomically, there are two pairs of glands: two upper and two lower. The mass of each varies from 0.05 to 0.09 g. The lower pair is larger in size than the upper one, and are located in the lower part of the thyroid gland. The left and right superior glands are located on the upper part of the posterior wall of the thyroid gland, approximately at the level of the lower edge of the cricoid cartilage.
All 4 glands are covered with a capsule of connective tissue. The capsule functions to protect the organ from infections and mechanical damage. Innervated by branches of the vagus nerve. Blood flows through the inferior thyroid artery.
Interpretation of ultrasound for formations
The predominant type of pathological neoplasm is adenoma; cysts and cancer are much less common.
Adenoma
It is the cause of primary hyperparathyroidism in 80-90% of cases. Refers to a benign formation with the following characteristics:
- the structure is moderately heterogeneous;
- there are zones of increased echogenicity (connective tissue fibers), high (calcium deposits), low (cystic cavity in the adenoma);
- tumor shape - drop, wedge, hourglass, oval;
- single or multiple (adenomatosis).
When examining the blood flow, symptoms of a branch or vascular arch are detected, which makes it possible to distinguish a parathyroid adenoma from thyroid diseases.
Cyst
It is a cavity filled with liquid. It has a thin capsule (up to 1 mm), low echogenicity. The size of the cyst can be up to several centimeters in diameter. Secondary cysts are formed due to hemorrhage or destruction of the tumor. Then there may be areas of tissue or calcium salts inside its cavity. Parathyroid cysts are quite rare.
Cancer
The distinctive characteristics of a malignant neoplasm are difficult to detect on ultrasound. To confirm the nature of the tumor, examination of its tissues is necessary. Indirect signs of cancer can be:
- lack of a clear capsule;
- the contour is lumpy;
- lymph nodes are enlarged;
- large sizes.
One of the indirect signs is enlarged lymph nodes
Indications and contraindications for ultrasound of the parathyroid glands
Ultrasound examination is indicated in the following cases:
- prevention and prevention of parathyroid diseases;
- if the patient suffers from recurrent urolithiasis, in which stones form after surgery;
- congenital defects of the skeletal system, acquired bone diseases: osteoporosis, frequent fractures for no reason;
- if the QT interval is shortened in the electrocardiogram, this is a sign of increased calcium in the blood;
- if the patient complains of cramps in the skeletal muscles - a symptom of decreased function of the parathyroid gland;
- increase in size;
- disturbances in blood biochemistry: deviation from the norm in the amount of hormones;
- suspicion of a cyst.
There are no contraindications to ultrasound diagnostics. Ultrasound as a method is safe. During the entire existence of the method, not a single case of side effect has been recorded.
Secondary hypothyroidism: symptoms, diagnosis, treatment
Secondary hypothyroidism is a lack of thyroid hormones when the thyroid gland is completely healthy. Sounds paradoxical? It occurs much less frequently than the primary one, and regularly confuses young doctors.
The thyroid gland is a captive organ. It has two bosses: the pituitary gland and the hypothalamus. The thyroid gland is directly controlled by the pituitary gland, and its activity is controlled by the hypothalamus. Both are controlled by the thyroid gland. The more thyroid hormones in the blood, the more passive the pituitary gland and hypothalamus are. This hierarchy allows the thyroid gland to secrete exactly as many hormones as the body currently needs. Hypothyroidism is classified accordingly:
- Primary – the thyroid gland itself is “to blame” for the disease. Damage to its tissue does not allow the organ to fully cope with its function.
- Secondary - the thyroid gland is absolutely healthy and is quite capable of performing its functions, but does not do this because there is no order from the pituitary gland. Pituitary commands are transmitted through TSH, which stimulates thyroid hormone production. If there is no TSH, then the thyroid gland does not work. There is not enough TSH - it does not work well. Both are hypothyroidism.
- Tertiary – both the thyroid gland and the pituitary gland are in perfect order, but the body does not have enough thyroid hormones. The hypothalamus does not secrete thyroid hormone-releasing hormone for the pituitary gland, and therefore it does not secrete TSH - the thyroid gland is inactive, and the person has tertiary, or hypothalamic hypothyroidism.
Secondary and tertiary hypothyroidism are collectively called “central” because the culprits in these diseases, the pituitary gland and hypothalamus, are located in the brain and are part of the central nervous system.
Causes
If you notice symptoms of hypothyroidism, you should have your thyroid checked.
The etiology of secondary hypothyroidism is essentially a list of diseases of the pituitary gland; it is also called pituitary.
- Pituitary tumors, when hormone-secreting gland tissue is replaced by useless tumor tissue. This disease is the most common of the following, especially microadenomas.
- Impaired blood supply to the pituitary region, aneurysm of the internal carotid artery.
- The pituitary gland is surgically removed or damaged during surgery.
- Abscess, encephalitis and its consequences, histiocytosis and other inflammatory pathologies of the pituitary gland.
- Congenital underdevelopment of the pituitary gland is very, very rare, and is usually detected in childhood.
- Rare mutations when the structure of the pituitary gland receptors for TRH is disrupted.
- Long-term, uncontrolled use of dopamine, glucocorticoids, and some toxins in high doses.
- Sometimes, with long-term and untreated primary or thyroid hypothyroidism, a cyst, hemorrhage or other pathology develops in the pituitary gland. This happens because with a lack of thyroid hormones, the pituitary gland constantly and actively secretes TSH, and there is a long-term overstrain. In this case, hypothyroidism is essentially both primary and secondary at the same time.
Diagnosis, or how to distinguish secondary hypothyroidism from primary
Symptoms of hypothyroidism usually prompt a thyroid test. And when it turns out that it is quite healthy, but for some reason does not work, then central hypothyroidism is suspected. Symptoms of secondary are similar to those of primary. The differences are few and not always found. Weight gain is not necessary; even exhaustion is possible. The swelling is very slight, the skin is thin, pale, wrinkled.
The main thing in diagnosing secondary hypothyroidism is tests. They start by determining the TSH level. If TSH is elevated in primary hyperthyroidism, then in secondary hyperthyroidism it is lower than normal. As for thyroid hormones, they are low in both types of the disease.
The main thing in diagnosis is tests. You should start by determining the TSH level
To be completely sure, a test with thyreoliberin, TRH, is prescribed. This substance is secreted by the hypothalamus to stimulate the pituitary gland to release TSH. If the pituitary gland is healthy and functioning, then TSH increases in response to thyroid hormone-releasing hormone. When this does not happen, the doctor speaks with confidence about secondary hypothyroidism. After this, it is determined which disease led to pituitary hypothyroidism.
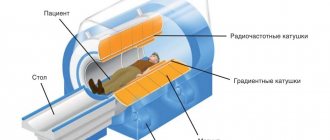
The simplest and cheapest method is an X-ray of the skull from the side, that is, in the lateral projection. You can see the so-called sella turcica, in the niche of which the pituitary gland is located. A common cause of secondary hypothyroidism is pituitary tumors. If the sella turcica is irregularly shaped, partially destroyed, or contains some kind of compaction visible on an x-ray, then it is highly likely to be a tumor. The pituitary gland itself is not visible on a simple x-ray, so this method is quite crude.
CT is much better, but the radiation exposure is much higher. The ideal method is MRI. MRI shows even very small tumors, hemorrhages and much more. Of the minuses: high cost and the inadmissibility of the presence of metal in the body. MRI is a large and strong magnet, so any pacemakers, metal endoprostheses, even metal sutures will simply be torn out of the body.
Treatment
As with any hypothyroidism, it is necessary to prescribe thyroid medications, i.e. thyroid hormones. During primary and secondary treatment, the doses of these hormones are the same. Problems with the pituitary gland rarely lead to hypothyroidism alone. This organ, like the conductor of an invisible orchestra, controls other glands in the same way as the thyroid.
A common companion to hypothyroidism in this case is insufficiency of the hormonal function of the adrenal glands, which are inactive for the same reason as the thyroid gland. Therefore, adrenal hormones are first prescribed, selecting the dose, then, starting with small doses, the thyroid hormone levothyroxine or another thyroid drug is added. Doctors themselves call this treatment replacement therapy. Patients often have to take these hormones for life.
If the cause of secondary hypothyroidism is completely curable, which is not often the case, then the pituitary gland is also treated in parallel with thyroid hormones.
Objectives and advantages of ultrasound diagnostics
Ultrasound diagnostics sets itself the following tasks:
- Pathology research.
- Assessment of disease severity.
- Evaluation of the effectiveness of the therapy.
The benefits of ultrasound include:
- Harmlessness of the procedure: ultrasound radiation is safe for the health of patients.
- Low cost of the study in comparison with computed tomography and magnetic resonance imaging in Moscow.
- Ultrasound can be performed on children and pregnant women.
- Diagnosis does not require surgical intervention and is carried out without damaging the skin.
- The results are interpreted in real time: information about the structure of the gland and its blood supply is immediately displayed on the screen.
- Reliability of the information received and ease of interpretation of the results.
Sensitivity reaches 75%. However, the accuracy of the study depends not so much on the device as on the competence of the diagnostician.
However, ultrasound has disadvantages:
- the clarity of the resulting image is limited;
- photo resolution is inferior to computer and magnetic resonance imaging;
- There may be interference during the study.
Feature of the procedure
According to experts, ultrasound examination of the parathyroid glands is highly effective. This is due to the fact that:
- If the gland is completely healthy, then when checked using ultrasound, it will not be displayed on the screen.
- Analysis of neoplasms, which are carried out using histology, helps to identify hyperplasia.
- The ultrasound machine has high resolution, which is very important when diagnosing PTG.
All the described features should be taken into account by the specialist performing the ultrasound.
If, after numerous studies, there are still doubts about the diagnosis, a fine-needle biopsy of gland cells is performed as an additional procedure.
Share link:
Partner advertising and related articles
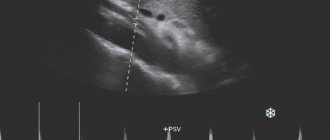
The essence of the parathyroid ultrasound procedure
The essence of the study is the effect of ultrasonic waves directed on tissues, their susceptibility by the organ and reflection. The degree of this reflection depends on the density of the tissue. The information obtained about the structure of the parathyroid gland is sent to the device, where it is processed. As a result, the diagnostician receives a black and white picture of the organ. Dense fabrics have a white tint, loose fabrics have a dark tint.
Ultrasound terminology:
- Echogenicity is the reflection of ultrasonic waves. The denser the fabric, the more it is reflected and vice versa: loose fabric is reflected worse.
- Isoechogenicity – when tissues are reflected evenly.
- Hypoechogenicity is a decrease in tissue density. Synonym: echo-negative area.
- Anechoicity - black areas on the image - tissue density is almost absent. Observed in the presence of fluid (cysts, arteries).
- Hyperechogenicity - increased tissue density. Synonym: echo-positive area. Hyperechogenicity can be observed with excessive accumulation of connective tissue and the deposition of calcifications.
The best motivation for sports for girls and women
- Prevention of cancer development. This fact was proven by American scientists who found that women who play sports and do not drink alcohol or smoke have a 20% reduced risk of cancer. Agree, 20% is quite a large percentage.
- Prevention of obesity, but not with the goal of fitting into your favorite dress for the New Year, but with the goal of preventing more serious diseases from developing, for example, diabetes mellitus or hypertension. Many people do not know that excess weight is not only visually unsightly, but also very dangerous for health, because obesity leads to other more serious problems.
These are my main motivations. And the fact that I won’t fit into a dress or become less attractive to men doesn’t bother me at all, because you can always buy a dress that fits your size, and even better, and real men care about not only beauty, but also intelligence, a sense of humor and kindness. And to those who do not care about these qualities, they can look for their pupae elsewhere. After all, you can’t get your health back...
Ultrasound examination technique
The study uses devices with sensors with frequencies ranging from 5 to 10 MHz. Diagnosis begins with the isthmus and lobules of the thyroid gland, while the image shows round-oval formations with clear edges, the echogenicity of which is slightly higher than that of the thyroid tissue.
Ultrasound of the thyroid and parathyroid glands is recommended to be performed in a lying or reclining position with the head tilted back. This way the neck muscles relax, which is convenient for both the diagnostician and the person being examined. Dental and cosmetology chairs that can be adjusted in height and tilt are most suitable.
The ultrasound technique of the parathyroid glands consists of several successive stages:
- Overview of the parathyroid gland. It is carried out by scanning in the transverse and longitudinal plane. In this case, the doctor examines the localization of the glands and its echogenicity.
- Assessment of gland volume.
- Search for neoplasms in the structure of the organ.
- Assessment of nearby structures: lymph nodes, thyroid gland, cysts.
Anatomical features suggest that all 4 parathyroid glands are sometimes not recorded in one image. It is believed that if they cannot be detected on ultrasound, the structure of the organ tissue is not disturbed.
Due to their small size, the parathyroid glands are always evaluated together with the thyroid gland: the procedure for determining mass, volume and tissue reflection is identical.
Structure of the thyroid gland
The thyroid gland, by its origin, belongs to the intestinal canal. At 3-5 weeks of gestation, a protrusion appears on the anterior wall of the pharynx, between the I and II pairs of gill pouches. The bottom of the resulting bag is directed down the anterior surface of the larynx and trachea. The rudiment of the anterior part of the thyroid gland descends along the ductus thyreoglossus, then the duct is overgrown (the rest of it is for. caecum on the root of the tongue). The lateral parts of the gland are also formed by eversion of the wall of the digestive tube, but below the unpaired bud, in the area of the esophagus.
Click on pictures to enlarge.
The thyroid gland lies in the anterior part of the neck, with its upper edge touching the thyroid cartilage; consists of two lobes of unequal size and an isthmus; sometimes the isthmus is absent.
Sometimes a pyramidal process extends upward from the isthmus; sometimes it reaches the hyoid bone, and to meet it from for. The coecum of the tongue stretches a canal that may be in connection with the accessory lobe of the thyroid gland, which lies above the body of the hyoid bone.
The parenchyma of the gland consists of round, completely closed vesicles - follicles. The wall of the follicle consists of thyrocytes surrounded by a basement membrane.
The basal surface of thyrocytes is closely adjacent to the capillaries, the apical part faces the lumen of the follicle; colloid with thyroglobulin is secreted into the lumen of the follicle, and the hormones thyroxine and triiodothyronine are secreted into the blood.
Each lobe of the thyroid gland is covered in front by the sternohyoid, sternothyroid and superior belly of the omohyoid muscle; from the sides - the sternocleidomastoid muscle; behind is the longus colli muscle.
The thyroid gland is adjacent to the neurovascular bundle of the neck - the common carotid artery, internal jugular vein, vagus nerve; The recurrent laryngeal nerve passes along the posterior surface.
The posterior surface of the thyroid gland wraps around the upper rings of the trachea; the lower sections reach the fifth and sixth rings.
The thyroid gland is covered with two connective tissue capsules. Violation of the integrity of the capsule when the tumor grows beyond the gland indicates the generalization of the malignant process and dictates the need for external beam radiation treatment or iodine therapy.
With connective tissue bundles, the external bursa secures the thyroid gland to neighboring organs - the cricoid cartilage, trachea, sternohyoid and sternothyroid muscles.
Lymphatic drainage from the thyroid gland is directed to the lymph nodes along the neurovascular bundle, along the sternocleidomastoid muscle, supraclavicular and pretracheal lymph nodes.
Parathyroid glands on ultrasound
Healthy parathyroid glands are almost never visualized, even if modern medical technologies with a frequency of 10 MHz are used: under normal conditions, the size of the organs is too small.
In a typical case, on ultrasound examination the parathyroid gland appears as a round and oval-shaped formation, the dimensions of which do not exceed 30 mm in any direction. Their edges are clear and smooth, they are hypoechoic, have a homogeneous tissue composition and are located at the poles of the thyroid gland. Normally, there is no vascularization (changes in blood vessels). With hypertrophy, the organ can acquire internal blood flow.
Nodes
Nodules in the thyroid gland remain the most common diseases of this organ. What does the thyroid gland look like in a person with nodes on it? At the initial stage of nodule formation, they are practically invisible from the outside and do not manifest themselves clinically. Cysts and nodules in this case are usually discovered by chance during a medical examination or medical examination.
When the node reaches a diameter of 5 mm, it is sometimes detected by palpation - if the formation is close to the surface or edge of the organ, it can be palpated. The knot under the skin does not move when pressed and feels different from normal tissue.
As a rule, a patient consults a doctor about a nodular formation only when it becomes noticeable—the neoplasm becomes highly visible from the outside. Usually, the nodule appears externally when its size begins to exceed 3 cm. By this stage, the patient already has a number of specific complaints:
- pain in the neck;
- feeling of a lump or foreign body in the throat – difficulty swallowing progresses;
- the part of the thyroid gland pressed out by the knot can begin to put pressure on the trachea and partially compresses it, which causes breathing problems;
- overgrown tissue puts pressure on the laryngeal nerve, which causes voice changes;
- thickening and tenderness of the cervical lymph nodes.
If the size of the nodes does not exceed 1 cm, the patient is monitored. If there is more formation, puncture is performed to determine the benign quality of the formation. Treatment is carried out according to the results of the study.
For women of any age, it is extremely important to pay attention to your thyroid gland. If anything is suspicious, you need to see a doctor, since any dysfunction of an organ can affect the entire body.
Pathologies that can be detected
Ultrasound of the parathyroid glands can reveal:
- Parathyroid adenoma . In the picture it appears like this: an arcuate blood vessel enters the pole of the gland and feeds the pathological neoplasm. For this study, Doppler is additionally used.
- Increase in size of the gland. Image: linear size exceeds 30mm.
- Tumor-like changes . It is manifested by the presence of a homogeneous mass, which has several echo-negative areas; signal amplification is also observed in this area.
- Multilobular interposition . The parathyroid glands on ultrasound show several homogeneous large neoplasms, which have septa inside them.
- Heterogeneous parathyroid glands . There are several hypoallergenic areas inside the gland.
- Cyst in the gland . The image shows a neoplasm, the wall of which does not exceed 1 mm, and an increase in the signal in this area is noted.
- Diffuse hyperplasia . The parathyroid glands increase in size, their structure is homogeneous and hypoechoic. With nodular hyperplasia, signal conduction deteriorates and the structure is heterogeneous.
Normal organ size
Women have smaller parathyroid glands than men. But for adult patients, uniform standards are established, regardless of gender. Normally, an ultrasound of the parathyroid glands should show the following results:
- length – from 4 to 8 mm;
- width – from 3 to 4 mm;
- thickness – from 1.5 to 3 mm.
The permissible weight of each gland is from 50 to 90 mg, the total tissue mass varies from 200 to 280 mg. If the ultrasound shows minimal deviations, additional examinations are prescribed.
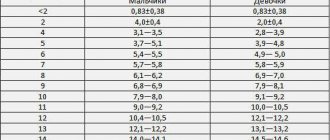
In children, ultrasound of the parathyroid gland is performed in the same way as in adult patients. But in this case, the technique is not so informative, which is due to the small size of the organs. For children, a study of this type is usually prescribed if abnormal sizes of glandular tissue are suspected. In the absence of pathologies in the child, the total mass of the glands should be as follows:
- up to 12 months – 6-9 mg;
- year – 18-36 mg;
- 5 years – 36-70 mg;
- 10 years – 70-100 mg.
Although in childhood ultrasound allows only a partial assessment of the condition of the organ, the technique is performed quite often, since it is completely painless and does not pose a threat to health.
Often, ultrasound shows false results, which is due to the similarity of the structures of the organ with neoplasms on the thyroid gland.