Thyroglobulin - what is it?
It is a protein that is a precursor to thyroid hormones in the human body.
The synthesis of thyroid hormones T3 and T4 in the human body does not occur immediately, but through the formation of thyroglobulin. This complex protein consists of amino acid residues tyrosine and iodine. In fact, thyroglobulin is a chain of almost ready-made molecules of the hormone thyroxine (T4), which only needs to be “cut” before the hormone is released into the blood. The protein is stored in the lumen of the thyroid follicles as a kind of “reserve”. The cells of the gland form single-layer spherical clusters, the internal lumen of which is filled with a viscous transparent gel - a colloid containing a large amount of thyroglobulin. It is stored in the lumen of the follicle until it is required by the body - then its molecule is captured by thyrocytes (thyroid cells) and passed through them, cutting into residues of two tyrosine molecules and four iodine atoms in each residue. Such “chopped” thyroglobulin is nothing more than a ready-made molecule of the main thyroid hormone, thyroxine, which is released into the blood.
When is organ removal necessary?
Removal of the thyroid gland may be a necessary step if a tumor is detected or the goiter is significantly enlarged. The causes of thyroid diseases can be:
- Genetic predisposition;
- Low assessment of the environmental situation;
- Untreated infectious diseases;
- Taking certain medications over a long period of time.
- With thyroid disease, a person experiences a number of symptoms:
- Increased fatigue;
- Sleep disturbance;
- Weight gain for no apparent reason;
- Men experience baldness;
- Increased sweating;
- High blood pressure and cholesterol levels in the blood;
- Hoarse voice;
- Performance decreases.
Often patients themselves discover a slight swelling in the neck area, and only then consult a doctor. To make a reliable diagnosis, the endocrinologist refers the patient to the following studies:
- Blood test for thyroid hormone levels;
- Ultrasound examination of the thyroid gland and lymph nodes;
- Computed tomography of the upper chest and neck;
- Biopsy of the thyroid gland and lymph nodes.
If, according to the examination, the disease requires surgical intervention, the patient is given a date for surgery. Currently, surgery can be performed in the following ways:
- Removal of the tumor while preserving the main part of the gland;
- Removal of one of the lobes of the thyroid gland, leaving the isthmus;
- Complete removal of the endocrine organ and adjacent lymph nodes.
The type of surgical intervention largely depends on the type of disease. To completely remove the thyroid gland, the following indications must be met:
- Malignant tumor;
- Enlarged diffuse goiter;
- Adenoma;
- Neoplasms of a benign nature.
The operation itself to remove the thyroid gland is routine and is not particularly complicated. Disability is not assigned in the absence of complications; the patient is discharged on the 7th day. After the operation, patients must take the hormonal drug Thyroxine for the rest of their lives. The drug can replace hormones produced by the thyroid organ. An endocrinologist helps you choose the required dosage depending on the individual structure of the body.
Thyroglobulin is elevated - why? What is the normal thyroglobulin level?
Thyroglobulin is normally located in the lumen of the follicles and enters the blood only in minimal quantities. Its increased “leakage” into the blood is observed when thyroid tissue is destroyed due to various influences:
- autoimmune inflammation in Hashimoto's thyroiditis, diffuse toxic goiter, subacute thyroiditis;
- purulent inflammation with purulent thyroiditis;
- destruction of thyroid tissue in the patient’s body after radioactive iodine therapy;
- destruction of thyroid nodule tissue after ethanol sclerotherapy, radiofrequency ablation, laser destruction, or even after fine-needle biopsy of the nodule;
- destruction of gland tissue after diagnostic scintigraphy of the gland using iodine-131, which, in addition to diagnostic gamma radiation, also has beta radiation that destroys thyroid tissue;
- death of residual thyroid cells after thyroidectomy or partial resection of gland tissue (after any surgery on the gland).
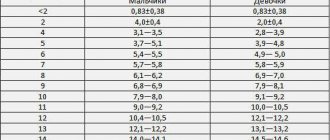
«Thyroglobulin normal
“,” “
increased thyroglobulin
,” “
what to do; increased thyroglobulin
” - these queries are regularly found in search engines such as Yandex or Google. The wording of the search query itself already indicates that most patients do not understand what thyroglobulin is and in what cases its level can be used in diagnosis.
It is important to understand that in patients with a preserved thyroid gland, the level of thyroglobulin should not be determined at all. An analysis for thyroglobulin in the presence of a thyroid gland will only show how large the gland is, how well or poorly it works, and whether there is an inflammatory process in the tissue or not. Indeed, the level of thyroglobulin in the blood depends only on:
- the volume of the thyroid gland and the size of the nodes present in it;
- activity of hormone production;
- the presence or absence of inflammatory processes in the gland tissue.
The larger the volume of the thyroid gland, the more it produces thyroglobulin - this is logical. The more active the thyroid gland is, the more hormones it releases into the blood, the more thyroglobulin is required - this is also logical. The more active the process of inflammation occurs in the gland tissue, the more actively the cells themselves and the follicles formed by the cells are destroyed, and the more actively thyroglobulin leaks into the blood - and this is also quite logical.
At the same time, if a non-specialist turns to Internet materials, the first thing he will glean from them is information that thyroglobulin is a tumor marker, that its level indicates the risk of thyroid cancer. As a result, many patients experience stress, which is usually not based on anything, and which does nothing but cause unnecessary harm.
It is important to understand one feature: yes, this is a tumor marker, yes, its level increases in patients with recurrent papillary or follicular thyroid cancer, but this dependence “increased thyroglobulin = relapse of thyroid cancer” occurs only in those patients WHO HAVE PREVIOUSLY REMOVED THE THYROID GLAND .
Think about it, this is also quite logical - if we know that thyroglobulin in the human body is produced only by the cells of the thyroid gland, as well as by the cells of two malignant tumors of the thyroid gland (papillary and follicular cancer), then we must understand that after complete removal of the gland and complete After removing the tumor, there should be no places left where thyroglobulin can be produced, and therefore its level should become very low, close to zero.
However, this relationship is only valid if the thyroid gland and tumor are first removed. If the patient’s thyroid gland is in its usual place, if no operations have been performed, then the blood test for thyroglobulin itself loses all meaning. Even if you and I see that thyroglobulin is elevated, what will we do? What medical recommendations can an endocrinologist give to a patient in this case? Absolutely none. The level of thyroglobulin in the blood, whether it is elevated or not, with a preserved thyroid gland is not the basis for determining treatment tactics, therefore this test should not be taken - this would be a pure waste of the patient’s funds.
Currently, specialists at the North-Western Endocrinology Center very often have to meet with patients from various regions of Russia who come to us for expert consultation with one question: “What to do - increased thyroglobulin?” It is very sad to see how people come from distant cities - Krasnodar, Murmansk, Magadan, only to find out that their analysis does not indicate any diseases, and that they are generally completely healthy. Of course, it happens that our endocrinologists identify various diseases of the thyroid gland in patients who come to us, it even happens that we perform some kind of surgery on the thyroid gland, but blood thyroglobulin is never an indication for treatment or a diagnostic criterion in such cases. .
Why do doctors prescribe thyroglobulin testing to patients across the country? Don’t endocrinologists themselves understand that this indicator is diagnostically unreliable? There are only two possible explanations for the fact that this analysis is widely used: either the doctor himself does not really understand the meaning of this indicator, or he understands this meaning (or rather, understands that there is no special meaning), but prescribes it simply to increase the patient’s expenses.
What can affect the results of the analysis?
Most often, false results are detected in the presence of antibodies to thyroglobulin. Therefore, their presence also needs to be detected. The results may be affected by taking hormonal medications, iodine preparations, the presence of chronic infectious diseases or hereditary predisposition. In addition, the analysis may be unreliable due to radiation exposure or the presence of toxins in the blood. Even severe stress can affect the level of thyroglobulin and antibodies to it. It has been established that the concentration of this protein increases during pregnancy, as well as in older women. And taking oral contraceptives leads to an increase in antibodies to thyroglobulin. This may also affect the analysis results.
Thyroglobulin as a tumor marker
At the Northwestern Endocrinology Center, a blood test for thyroglobulin is not prescribed during the initial examination. We are well versed in thyroid diseases and we care about our reputation, so we try to save our patients money and not waste it.
At the same time, if you look at the number of thyroglobulin tests that the Northwestern Endocrinology Center performs annually, we are now among the Russian leaders in the number of such tests. The thing is that our center is the Russian leader in the treatment of differentiated thyroid cancer - papillary and follicular. Every year, the center performs about 700-800 operations for thyroid cancer, and several tens of thousands of patients who have been treated previously are under observation. And for all these people, thyroglobulin is the main indicator. All these patients donate blood for analysis annually or even somewhat more often, and each time for them it is stress, it is an expectation - is thyroglobulin elevated or not? And in this group of patients, thyroglobulin is really a tumor marker, since the thyroid gland and tumor had already been removed earlier, then many patients were treated with radioactive iodine to destroy even the smallest remnants of the gland and tumor tissue.
After successful treatment of differentiated thyroid cancer, the blood thyroglobulin level should not exceed 2 ng/ml
(against the background of a three-week withdrawal from thyroxine), if radioiodine therapy was previously carried out, and
5 ng/ml
if radioiodine therapy was not carried out. Of course, the lower the thyroglobulin, the better, but the level, even after successful treatment of the tumor, is rarely completely zero. The sensitive 3rd generation analyzers that we use even the smallest amounts of thyroglobulin in the blood, so its level in the blood is almost always just above zero.
What is dangerous about changes in thyroglobulin levels?
An increase in thyroglobulin is a pathological condition that occurs when the endocrine system malfunctions. If the test results exceed the reference values, this often indicates malignant processes in the thyroid gland:
- Papillary cancer is a common form of adenocarcinoma, which is detected in 85% of cases of all gland tumors. In 30% of patients, regional lymph nodes are involved in the malignant process. With late diagnosis and treatment, metastases are detected in the lungs and bone tissue.
- Follicular cancer is an aggressive, low-quality thyroid tumor that is prone to metastasis to internal organs. More often diagnosed in women and children, they are characterized by the growth of cancerous tissue into the blood vessels in the neck area.
Elevated thyroglobulin values indicate structural changes in the thyroid gland. Because of this, the protein enters the blood undigested. It is recognized by the immune system as an antigen, so antibodies are synthesized against TG. This causes autoimmune inflammation of the gland - Hashimoto's thyroiditis.
Most patients with benign tumors in the thyroid gland exhibit increased concentrations of thyroglobulin. Such results are obtained in acute iodine deficiency, which is dangerous due to thyroid pathology. It manifests itself with the following symptoms:
- memory impairment;
- difficulty swallowing;
- fast fatiguability;
- hair fragility, etc.
Changes in TG levels are fraught with nodular goiter. A decrease in thyroglobulin during pregnancy is dangerous for the thyroid gland of the mother and fetus. Endocrine pathologies in the early stages often lead to spontaneous abortion and hypothyroidism in newborns.
A decrease in TG due to iodine deficiency during pregnancy leads to a severe complication in the child - neurological cretinism.
Rules for donating blood for thyroglobulin
When donating blood after treatment for cancer testing, it is important to know a few rules:
- a blood test for thyroglobulin becomes reliable 3 months after surgical treatment and 6 months after radioactive iodine therapy
; If you take the test early, you may see a false increase in the indicator and think that your cancer is developing a recurrence; - always, together with thyroglobulin, a test for antibodies to thyroglobulin is taken
; an increase in antibodies in the patient’s blood completely eliminates the diagnostic value of the thyroglobulin test - with high antibodies, it will always be at low values, since antibody molecules will bind protein molecules and “mask” them from the analyzer; - a blood test for thyroglobulin, taken while taking thyroxine and against the background of a low level of the hormone TSH in the blood, has diagnostic value
and can detect a relapse of thyroid cancer, but in 20-25% of cases, relapses of thyroid cancer will not lead to an increase in thyroglobulin if the TSH level low - in such cases, only the abolition of thyroxine for 3 weeks followed by an increase in the TSH level will be able to identify existing tumor metastases based on the fact that thyroglobulin will become high; and still, the so-called unstimulated thyroglobulin (i.e., a blood test for thyroglobulin taken while taking thyroxine) has diagnostic value and should be used in clinical practice - a blood test for thyroglobulin, taken after stopping thyroxine for 3 weeks, is the most accurate indicator of tumor relapse
(a prerequisite for using this test in practice is the absence of elevated antibodies to thyroglobulin in the blood); - in many cases, what is more important is not the level of thyroglobulin in the blood, but the dynamics of its change
(i.e. if it is moderately elevated, but falls over time, this is much better than if it was lower at the beginning, but then began to increase).
Indications for analysis
Sometimes it happens that doctors unreasonably prescribe a blood test for thyroglobulin. Not all patients know what it is, and this analysis frightens many. But it is not always done when a cancerous tumor is suspected. Only in those patients who have had their thyroid gland removed, such a study is indicated regularly to prevent relapses. In addition, a thyroglobulin test is also performed for those undergoing radioactive iodine treatment in order to monitor the effectiveness of therapy.
It is also prescribed in some other cases:
— to study the development of congenital hyperthyroidism in children;
- to monitor the development of thyroiditis;
— in a comprehensive study of iodine deficiency;
— to calculate the effectiveness of hyperthyroidism therapy.
And the most important…
At the end of this short article, I would like to say that thyroglobulin is a highly specialized laboratory indicator that is used only in some selected situations. It should be used only for its intended purpose and not used where you can do without it. Elevated thyroglobulin
Blood tests aimlessly scare thousands of people every year, but for thousands of people every year,
the thyroglobulin level
gives hope for a normal life - it’s all just a matter of who prescribes the test, in what situations and how the results are then interpreted. The 3rd generation immunochemiluminescent laboratory of the Northwestern Endocrinology Center determines thyroglobulin with extreme accuracy, and the center’s specialists know very, very much about it, so if you suddenly have any questions or misunderstanding of your tests or your doctor’s tactics, come to us to the center for a consultation or re-analysis in order to remove all questions and understand how and where to move on.
Thyroglobulin after removal of the thyroid gland
- 3 minutes to read
Thyroglobulin is a protein produced exclusively by the thyroid gland. The generally accepted norm for people with a healthy thyroid gland is 20 ng/ml. But in the presence of certain factors (viral diseases, stress, biopsy, diabetes, pregnancy, oral contraceptives, etc.), values from 1.5 to 50 ng/ml can also be considered within normal limits.
Content
When the thyroid gland secretes excess amounts of protein, the immune system begins to produce antibodies. This indicator is also recorded and in the conclusion you can see two points TG (thyroglobulin level) and AT (the number of antibodies).
Detection of more than 50 ng/mg over a long period indicates dangerous pathological changes in the organ (cancer, autoimmune diseases), giving reason to consult an oncologist and further removal of the organ.