Size of the uterus during menopause: changes, ultrasound norms and pathological conditions
The onset of hormonal changes in the female body leads to a number of anatomical and physiological changes in many systems and organs. To a greater extent, women's reproductive organs, namely the ovaries and uterus, undergo changes during menopause. Let's take a closer look at what changes the female uterine organ undergoes with the onset of menopause.
Uterus during menopause
The main phases of menopause are premenopause and menopause, after going through which a woman begins a long period of postmenopause, which accompanies her throughout her entire subsequent life.
The premenopausal period is quite long: from 3 to 10 years. This period is characterized by changes in almost all organs and systems in the female body. They can appear in a more vivid form or, with timely treatment, in a smoothed form:
- psychological disorders;
- changes in thermoregulatory processes in the body;
- hormonal imbalance, accompanied by a deficient level of production of sex hormones;
- disturbances in the menstrual cycle, until its completion.
The menopausal period begins immediately after the last menstrual period and continues throughout the next year. It is believed that the end of menopause occurs after 12 months of absence of menstruation. During this period, involutional changes in the genital organs occur in the female body. Almost all reproductive organs begin to decrease in size, and even the uterus decreases in size during menopause. Not only the size of the genital organs decreases, but also the amount of cervical mucus, which subsequently has an important impact on the state of the microflora.
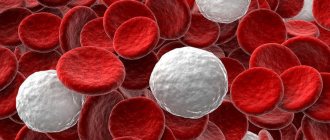
Moreover, during menopause, the overall level of resistance of the body to the effects of pathogenic factors decreases. Some organ systems begin to function less well, which leads to a decrease in the body's immune defense system.
Therefore, many women who have entered the threshold of menopausal changes are faced with various diseases, especially those related to the reproductive system.
Thus, in most cases, the occurrence of tumor-like processes in the area of the mammary glands and uterus is noted during menopause. Therefore, with the onset of menopause, it is necessary to regularly visit a gynecologist and undergo an annual examination. The main most dangerous pathological changes include:
- Inflammation of the uterus.
- Development of benign neoplasms in the uterine cavity.
- Development of a tumor-like neoplasm of oncological nature of the uterine organ.
- Breast cancer.
- Salpingitis or inflammation of the fallopian tubes.
- Endometritis.
- Vaginitis.
- Carcinoma.
- Fibroma, etc.
All these pathological changes in the reproductive system of a woman during menopause are very dangerous, and in the absence of timely treatment, many of them pose a serious threat to a woman’s life.
To prevent the development of serious pathologies, regular examinations in the gynecological office and timely ultrasound are necessary.
Ultrasonography
Ultrasound of the uterus during menopause is prescribed as a standard examination of the pelvic organs and diagnosis of pathologies with symptoms similar to menopausal syndrome.
The ultrasound research method provides a fairly high level of information content, is safe and does not cause hostility.
Despite the fact that menopause is a natural process, for most representatives of the fair half of humanity it can cause a number of unpleasant symptoms and discomfort, expressed as follows:
- disruption of the regularity of the menstrual cycle, up to its cessation;
- occurrence of dizziness and headaches;
- sleep disturbances with the development of insomnia;
- hot flashes;
- dryness in the vaginal area;
- frequent urge to urinate;
- pain during sexual intercourse.
Sometimes women cope with these manifestations on their own, but most often the help of hormone replacement therapy is needed. To assess the condition of the woman's reproductive system, an ultrasound examination is performed using a transvaginal sensor.
During menopause, the norm of changes in the uterus, revealed by ultrasound, is as follows:
- Increased echogenicity (or density) of the uterus.
- Its anteroposterior size decreases.
- Severe atrophy of the endometrial layer.
- Formation of adhesions and synechiae.
During the menopausal period, ultrasound examination may also reveal the presence of fluid in the uterine cavity. This is sometimes perceived by specialists as the development of a polyp or hyperplasia of the endometrial layer, although in fact this is not the case.
The formation of this fluid may normally be a consequence of the process of overgrowth of the cervical canal associated with the aging of the female body. But this condition requires a mandatory additional research method by hysteroscopy, which will help to more accurately assess the benign quality of the processes occurring.
A diagnostic examination using ultrasound examination of the pelvic organs is of great importance for a woman’s life, as it helps to identify serious pathologies in the initial stages of development.
Especially considering the fact that mature women are more susceptible to pathological changes in the uterus, such as its enlargement during the development of oncology during menopause. The process of enlargement of an oncological tumor is sluggish and does not cause specific symptoms. And the appearance of uterine bleeding and pain in the lower abdomen are observed in later stages of the disease.
Therefore, it is so important not to ignore timely ultrasound, which will help identify and promptly begin appropriate treatment.
What do calcifications indicate?
Among other things, sometimes during ultrasound examination, experts note the presence of calcifications in the uterine cavity. And, therefore, all representatives of the fair half of humanity are interested in questions about what it is, what happens to the uterus when they are in it?
Almost all gynecological specialists do not classify the presence of calcifications in the uterine cavity as a separate disease, but consider it a consequence of the chronic course of an inflammatory process, such as salpingitis.
What do calcifications in the ovaries mean on ultrasound?
Sonography has become widespread in medicine due to a number of advantages over other types of examination of internal organs. Ultrasound examination of the ovary is a diagnostic measure aimed at identifying various diseases, inflammatory processes, neoplasms and other pathologies.
Ultrasound of the ovaries
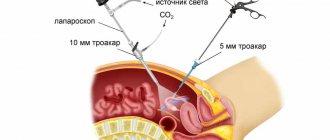
As a rule, an ultrasound of the ovaries is carried out in conjunction with a study of the condition of the entire reproductive system of a woman, but it can also be an independent procedure. This manipulation is indispensable for patients who are undergoing treatment or require laparoscopy (surgery).
During the examination, the structure, size, position, structure and functional state of the organs are studied, on the basis of which the specialist makes a conclusion about the woman’s health.
Medical indications for ultrasound of the ovaries
For preventive purposes, every healthy woman should undergo an ultrasound procedure twice a year. This is necessary to monitor the condition of the patient’s reproductive system, identify possible pathologies and timely take adequate measures.
Ultrasound of the uterus and ovaries is recommended in the following cases:
- various menstrual irregularities or absence of menstruation;
- starting to take hormonal contraception or inserting an intrauterine device;
- pregnancy planning;
- infertility;
- suspicion of gynecological diseases;
- vaginal discharge containing blood in the middle of the cycle;
- before and after the “lapara”;
- evaluation of treatment results;
- pulling, cutting pain in the lower abdomen, in the right or left side.
What pathologies can ultrasound of the ovaries detect?
The ovary is a paired organ responsible for maintaining hormonal levels in a woman’s body, in which an active egg can be formed. The functioning of the ovary affects well-being and general condition, and is also decisive for the menstrual cycle. Any failure or dysfunction of the ovaries entails problems with the reproductive system and health in general.
Polycystic ovary syndrome
Ultrasound of the ovaries can accurately identify some of the most common diseases.
Ovarian cysts are physiological and pathological. Physiological ovarian cysts are not a pathology; they arise as a result of the functioning of the organ and disappear without intervention. Dermoid, endometrioid cyst is a low-quality formation and requires treatment.
An ovarian cyst on ultrasound looks like a ball filled with fluid, having different sizes, structure and degree of staining.
Types of pathological cysts
- A dermoid cyst is formed as a result of impaired tissue differentiation and is considered by doctors as a benign tumor.
- An endometrioid cyst is formed from the tissues of the mucous membranes of the uterus and causes its enlargement.
- Polycystic.
In polycystic (multifollicular) ovaries, many cysts are detected, which is why the organ itself increases significantly in volume. - Ovarian cancer is a dangerous pathology that occurs more often in women during menopause, less often in young girls, sometimes even in little girls.
Diagnosing cancer during an ovarian ultrasound procedure is quite difficult, since it is difficult to distinguish from cystadenoma.If, upon examination, a specialist finds a cyst that has a multi-chamber structure with undetectable filling, which tends to spread to neighboring organs, it is worth conducting additional tests, including a biopsy, and also ordering a repeat study.
The video of the next procedure will clearly show which process is developing, oncological or physiological.
- Apoplexy is rarely diagnosed on ovarian ultrasound, since ultrasound waves are not sensitive enough to detect organ rupture. A sign of ovarian apoplexy may be the presence of a large amount of blood in the abdominal cavity.
- Ovarian calcifications are not a pathology and do not pose a health hazard. Defined as compactions due to the deposition of calcium salts in the organ.
- Editorial board of Oncology.ru
- October 16, 2020
Reasons for education
Calcium is a conductor of nerve impulses, and therefore plays an important role in the body. In tissues, salts are deposited where cell death occurs as a result of inflammatory processes.
Can an ovarian cyst resolve on its own?
Calcifications in the ovaries are detected as a result of past pathologies:
- adnexitis;
- difficult labor with compression of the ovaries;
- polycystic disease;
- follicular cysts.
Sometimes they occur when the venous outflow from the pelvic organs is disrupted, which occurs during prolonged sitting. Without oxygen, cells begin to die. The influence of hormonal changes on the deposition of calcium salts has been proven.
Source: https://xn—-7sbbabkwnixgwr4a5a.xn--p1ai/uzi/yaichnik-s-kalcinatami.html
Pathological changes in the uterine organ
During hormonal changes in the body, especially in premenopause, exacerbation of existing chronic gynecological pathologies may occur, as well as the formation of new ailments that can cause painful symptoms and uterine hemorrhages.
Let's consider the most dangerous pathological changes in the uterus during menopause.
Development of fibroids
This neoplasm itself has a benign course. Typically, fibroids appear during the fertile period, and with the onset of menopause it becomes more acute and begins to increase in size.
Fibroids can form in the form of one or several nodes localized in any part of the uterine cavity. Growing fibroids increase the standard size of the uterus several times, which leads to compression of nearby organs and the appearance of pain symptoms. Enormous growth of this neoplasm can lead to an enlarged abdomen. Moreover, fibroids also cause the following symptoms:
- Uterine bleeding.
- Pain in the lower abdomen.
- Frequent urge to urinate.
- If fibroids grow towards the rectum, stool disturbances and constipation are observed.
Painful sensations may appear during intimacy with a partner.
Treatment for this pathology is prescribed after a full examination, taking into account the individual characteristics of each woman.
Endometriosis
This pathological change in the uterus during the menopausal period is characterized by the growth of the endometrial layer with pathological penetration into the muscular layers of the uterus. Most often it occurs in premenopause, when the menstrual cycle has not yet completely subsided.
Causes symptoms such as:
- painful sensations in the lower abdomen of an aching nature, as well as pain during sexual intercourse;
- prolonged menstruation, when the uterus does not contract for 10-14 days, which is the reason for diagnostic curettage;
- against the background of prolonged menstruation, a disturbance in the psycho-emotional state occurs;
- Infertility may develop.
If one of the presented symptoms appears, you must immediately contact a medical specialist to prevent complications and the development of a more serious pathology.
Chronic form of salpingitis
Salpingitis is an inflammatory process in the fallopian tubes and appendages, which can occur long before the onset of menopause, and with the onset of hormonal changes it can become an aggravated form of the disease. Typically, salpingitis causes symptoms such as:
- Sharp pain in the lower abdomen.
- Increased body temperature.
- Formation of purulent discharge.
In the absence of timely treatment, it can become complicated and lead to the development of pathology requiring immediate removal of the uterus.
Development of the adhesive process
Numerous surgical interventions in the structures of the organs of the reproductive system of the body, as well as inflammatory processes together lead to the formation of adhesions or the spread of connective tissue. With the onset of menopause, a woman’s body experiences a decrease in the toning of muscle fibers.
This leads to anatomical displacement of organs in the pelvis, which causes nagging pain from stretching of the adhesions.
Depending on what kind of disorder occurs in the uterus, appropriate treatment is prescribed. In most cases, if the pathology is not associated with an oncological process, hormone replacement therapy is prescribed. But the dosage and course duration should only be determined by a qualified specialist. Self-medication of any pathology during menopause can result in irreversible consequences.
Useful video on this topic:
Calcifications
When deposits of calcium salts form in soft tissues and internal organs, which normally should not be there, this process is called calcification, calcification or calcinosis.
Calcium salts are deposited at the site of destroyed tissues, and therefore appear in areas where there was previously inflammation, in all kinds of diseases, be it an oncological process, tuberculosis or something else, i.e., in fact, calcifications replace dead or irreversibly changed cells. In addition, multiple widespread calcifications can form if calcium metabolism in the body is disrupted.
Calcifications can appear in any organs and tissues, and most often they are a symptom of an underlying disease.
Common symptoms of calcification itself include signs of chronic inflammation (weakness, fever), poor appetite, sleep disorders (insomnia, daytime sleepiness), neurological disorders (dizziness and headaches, irritability). Local signs appear depending on which organs and tissues are affected by calcification.
Calcifications in the lungs
Calcification in the lungs usually appears due to tuberculosis. However, in order to acquire calcifications in the lungs, it is not necessary to directly suffer from tuberculosis. They can also occur after contact with Koch's bacillus in childhood.
Calcifications are formed as follows: if a person has a strong immune system, the tuberculous nodule is separated from healthy tissue, and the place where it is located becomes calcified.
In more rare cases, accumulations of calcium salts occur after pneumonia, lung abscesses, and cancer.
Symptoms of pulmonary calcification include rapid shallow breathing (tachypnea), shortness of breath, and cyanosis (blue discoloration of the face, hands, and feet). Shortness of breath can develop at a stage when compensatory mechanisms can no longer cope with the load.
The appearance of tachypnea is due to the fact that the body is trying to restore the normal gas composition of the blood, disturbed due to damage to lung tissue.
In addition, with a long course of the disease, “drumsticks” and “watch glasses” are formed: the fingers lengthen, the nails expand.
In most cases, calcifications in the lungs are detected by chance, during a routine examination. As a rule, the calcifications themselves do not need to be treated. But if they are detected in a person, he needs to undergo a full examination so that the doctor can accurately determine the cause of calcification and make sure that the patient does not have active tuberculosis.
Calcifications in the kidneys
The most pronounced clinical picture of calcification is calcification in the kidneys.
The volume of urine decreases sharply (as the filtration function of the kidneys is impaired); Urine toxins accumulate in the blood, causing bad breath (acetone smell) and the skin turns yellow. The face and legs swell.
Renal edema differs from cardiac edema in that it does not have a blue tint and is not cold to the touch. Signs of renal failure also develop (impaired appetite, sleep, weakness, dizziness).
In the kidneys, as with damage to other organs, calcification is the result of inflammation. At the top of the list of causes of calcification of areas in the kidneys, as in the case of the lungs, is tuberculosis. Calcifications may also appear in people who have had pyelonephritis, especially if they have not completed the full course of therapy.
Calcifications in the liver
In some cases, deposits of calcium salts in the liver occur in patients who have had malaria or parasitic diseases (amoebiasis, echinococcosis, etc.). After hepatitis, they appear very rarely, unless a person has been suffering from chronic liver disease for a long time.
With liver calcification, pain occurs in the right hypochondrium, because the Glissonian capsule - a thin fibrous membrane covering the surface of the liver - shrinks or, on the contrary, stretches.
Varicose veins of the anterior abdominal wall (due to the specific appearance that the abdomen takes on, this manifestation is called the “head of a jellyfish”), and the esophagus (this causes bloody vomiting).
Fluid accumulates in the abdominal cavity, i.e., ascites occurs.
Calcifications in the prostate
The cause of the formation of calcifications in the prostate, in addition to the inflammatory process, may be poor circulation. They also often appear in men who have had sexually transmitted infections or who suffer from chronic prostatitis.
Sometimes calcification develops if the patient has impaired venous outflow from the prostate tissue. In this case, some areas of the prostate gland are compressed by swelling, and they are insufficiently supplied with oxygen.
As a result of the action of all of these factors (as well as a number of others), changes appear in the prostate at the cellular level and, as a consequence, areas of calcification.
If calcium salts accumulate in the prostate gland, less sperm is produced and it becomes thicker. Due to the fact that calcifications block the urethra, urination is impaired. In addition, the secretion of the prostate gland stops, and as a result, erectile dysfunction develops.
Calcifications in other organs
Calcifications in the thyroid gland appear most often with diffuse or nodular goiter, as well as after thyroiditis or hypothyroidism.
When it becomes calcified, the amount of thyroid hormones released decreases over time, causing a person to feel weak, drowsy, lethargic (both physical and mental), and constantly cold.
His metabolism is disturbed: a person quickly gets fat, even if he eats very moderately. The thyroid gland itself increases in size and looks like a node with many depressions and tubercles.
Calcification of the myocardium can occur in a person who has suffered a heart attack, myo-, endo- or pericarditis. With myocardial calcification, signs of a severe cardiovascular disorder appear: pain in the heart area, heart rhythm disturbances, lips, ears, fingers, tip of the nose turn blue, swelling appears in the legs (at the same time they also turn blue and become cold to the touch).
Calcifications in the breasts may be a sign of cancer. Therefore, a person who has been diagnosed with them urgently needs to undergo a full examination for cancer pathology. But there is no need to panic ahead of time, calcifications in the breast are a symptom not only of a malignant neoplasm: they can also appear with mastopathy or after mastitis.
Diagnostics
Calcification is revealed by radiography. The consistency of calcifications is similar to bone, so they appear on an x-ray as dense, stone-like structures.
CT or MRI can not only detect calcifications, but also clarify their size and location, and therefore they are used for a detailed examination. Ultrasound is used not so much to diagnose calcification, but to exclude other pathologies.
If calcifications are found in several organs or if there is no obvious cause for calcification, a biochemical blood test for calcium levels is performed: hypercalcemia may be the cause, and the doctor should check whether it is present or not.
When calcification of internal secretion organs (for example, the thyroid or prostate gland), a study of hormone levels is carried out. This is necessary in order to find out whether hormone replacement therapy is needed in this case.
Detailed description of the pathology
Calcification of the right or left ovary is a formation consisting of deposits of calcium salts. To differentiate it, professional diagnostics will be required.
Stones are: medium, large, small, and tend to move (formations are found in the uterus and organs of the genitourinary system).
Doctors do not have a clear opinion about whether stones are dangerous to a woman’s life and health, how they affect the functioning of the organs of the reproductive system, or whether they can cause infertility.
Each case is considered individually, assessing the causes of stones, as well as their impact on a woman’s reproductive ability.
It is believed that difficult pregnancy and childbirth provoke the appearance of formations. But pathology begins to develop not only due to changes in the body associated with bearing a child and childbirth.
The pathological process does not have specific symptoms. For many years, a woman does not suspect that there are calcifications in the paired gonads.
Calcifications in the ovaries: what they are, symptoms, causes, what they mean on ultrasound, treatment, prevention
Calcifications in the ovaries are a common finding during ultrasound diagnostics in women who have no complaints or diseases. Only when cysts and other neoplasms are detected, the deposition of calcium salts is important for further examination and treatment.
What is calcification
Calcifications in the ovaries in themselves are not a pathology. The radiological sign is detected using ultrasound or MRI in completely healthy ovaries. Pathological calcifications are associated with tumor formations: mature teratoma or dermoid cyst, mucinous cystadenoma (a type of ovarian cyst) or serous neoplasia.
Ovarian calcification detected for the first time is not an indication for a biopsy or other intervention. Pathological evaluation is only required if tumors or cysts are present.
Calcifications detected using gynecological ultrasound are of two types:
- psammous - spherical layer-by-layer formations of protein-lipid substances on which calcium salts are deposited;
- non-psammotic - they are integral accumulations that appear during diagnosis as a zone of increased echogenicity.
It is the identification of psammous deposits that indicates the risk of a serous neoplasm and the need for further examination.
Symptoms
Calcifications in the ovaries do not manifest themselves. They are usually discovered incidentally during tests for endometriosis or menstrual irregularities. They do not necessarily affect the function of the reproductive organs.
Treatment
Calcifications are a sign of other pathologies. In normal ovaries they indicate a local metabolic disorder.
In tissues, the pH - acid-base balance - increases, which leads to the accumulation of calcium salts inside the cells. This pathology does not require drug or surgical intervention.
If calcifications are associated with ovarian cysts, then most often they indicate a certain type of formation. Serous and mucinous cystodenomas are subject to surgical removal.
If a malignant process is suspected, a more detailed diagnosis is carried out to identify the stage of the tumor and the presence of metastases.
Calcium salts in the ovaries without concomitant pathologies cannot be treated. There is an opinion that it is necessary to create a calcium deficiency in the body in order to resolve deposits. But this approach may increase the risk of osteoporosis.
Complications
Malignant tumors cannot be called a complication of pathology; rather, the deposition of calcium salts is a sign of a past or existing pathological process. They do not affect ovulation, ovarian function or the possibility of conception.
The study showed that calcifications up to 5 mm are normal. Scientists observed women with calcium salts in their ovaries for 30 months.
None of them developed malignant tumors. Histological examination (biopsy) confirmed that calcium appeared as a result of degeneration of the white corpus luteum.
Prevention
Since inflammatory processes lead to the deposition of calcium salts, women are advised to take preventive measures against chronic infections. In addition to observing the rules of personal hygiene, try to avoid hypothermia, decreased immunity, and the development of dysbacteriosis.
Pelvic congestion develops due to a sedentary lifestyle. Prevention is regular walking and visiting fitness centers. A routine examination by a gynecologist will help you not to miss more serious pathologies.
Source: https://onkologia.ru/dobrokachestvennyie-opuholi/zhenskaya-reproduktivnaya-sistema/kaltsinaty-v-yaichnikah/
Causes of problems
Calcifications are formed for several reasons, which are influenced by various factors. We are talking about gynecological diseases and metabolic disorders. Additional factors leading to the appearance of stones:
- Past diseases of infectious, inflammatory origin.
- Increased consumption of macroelements, calcium.
- Metabolic disorders.
- Difficult childbirth, pregnancy, unsuccessful gynecological manipulations.
Doctors often cannot determine why the stones appeared. The pathological process is associated with poor nutrition, abortion, and medication.
When an ovarian cyst is combined with calcifications, this indicates the presence of inflammatory processes. Differentiated diagnostics will help confirm or refute such information.
Complications
Malignant tumors cannot be called a complication of pathology; rather, the deposition of calcium salts is a sign of a past or existing pathological process. They do not affect ovulation, ovarian function or the possibility of conception.
The study showed that calcifications up to 5 mm are normal. Scientists observed women with calcium salts in their ovaries for 30 months.
None of them developed malignant tumors. Histological examination (biopsy) confirmed that calcium appeared as a result of degeneration of the white corpus luteum.
Diagnosis of the disease
This is done in stages and involves hardware research. Doctors advise being examined by several doctors to identify the cause of the problems:
- detect calcifications in the ovaries using ultrasound. Ultrasound examination is done in 3 ways, transvaginal is considered the most informative; inserting a sensor into the vagina helps to obtain information about the health of the genital organs;
- It is recommended to do Doppler sonography, it is necessary to determine the size of the stones and their locations;
- x-ray of internal organs. The examination is rarely carried out due to toxicity;
- You will have to take blood tests to check for inflammatory and infectious processes.
To determine the concentration of a macroelement, a biochemical blood test is required.
A mandatory consultation with a urologist or nephrologist is necessary; an ultrasound examination of the kidneys and bladder will be required.
Therapy and its techniques
There are several methods for treating the disease. It all depends on the condition of the woman’s body. If the patient plans to become a mother in a year, it is better to remove the formations. Existing removal methods:
- If a corpus luteum with calcifications is found in the ovary, it is removed surgically or laparoscopically. When doctors believe that formations interfere with pregnancy or bearing a healthy fetus, they recommend surgery.
- Pregnancy is not planned: you can get by with drug therapy, which involves taking courses of drugs.
- It is advised to follow a diet, limit the amount of calcium consumed, and stop taking medications containing macronutrients.
If, based on the results of the analysis, it is possible to detect an inflammatory process, anti-inflammatory drugs, antibacterial agents, and antiseptic solutions are prescribed.
The treatment is carried out by a doctor, who selects medications individually. The most effective is complex therapy, including medications that help remove calcium deposits and diuretics.
If you follow a diet and avoid foods rich in macronutrients, the body will begin to compensate for the deficiency from its own reserves.
Stones form slowly, calcium ions accumulate over years. It is difficult, almost impossible, to suspect the presence of such violations. Therefore, do not forget about prevention, regularly visit a gynecologist, undergo an ultrasound of the uterus and ovaries, this will help to avoid unpleasant surprises.
Calcifications in the uterus during menopause
Reading time: min.
Calcified uterine fibroids, what is it? This is a benign neoplasm, which originates from the smooth muscle cells of the middle layer of the uterus, like a regular fibroid, with only one caveat: these tumor cells begin to actively accumulate calcium, a hard capsule is formed, inside which this element also accumulates, thus calcification of uterine fibroids. This neoplasm is a calcified formation - essentially a “stone” located in the thickness of the myometrium. The sizes of such fibroids can vary. It is considered a mistake that tumors with accumulated calcium do not grow. Of course, calcium itself cannot multiply, however, myocytes can further form on top of this formation and increase the size of the main tumor with their divisions.
However, there are significant differences in the severity of symptoms of fibroids and calcified fibroids, provided they are large in size.
The calcified formation is dense and will put more pressure on the organs, which will be accompanied by an increase in the manifestations of such a diagnosis.
Diagnosis of such neoplasms does not differ from the standards of examination for ordinary fibroids: bimanual examination and ultrasound diagnostics will allow us to accurately speak about the nature of the neoplasm, that is, its calcification; such fibroids can be visible even on an x-ray. Magnetic resonance and computed tomography are no exception.
Calcifications are discovered accidentally during an ultrasound examination. Women are rightly concerned with questions: what kind of condition is this, what causes it, how dangerous it is to health and how dangerous it is for pregnancy and the successful birth of a child.
The structure of the uterus and calcifications
The diagnosis “Uterine calcifications” does not exist in the International Classification of Diseases, 10th revision. In other words, calcifications are not a disease, but a condition when deposits of calcium salts are found in any of the sections, layers of the uterus or fibromatous node.
There are three layers of the uterus:
- internal - endometrium;
- middle - muscular;
- serous covering membrane.
Calcifications are accumulations of calcium salts. Their deposition is the result of previous inflammation. In areas of tissue that have been exposed to an infectious process, calcification occurs as a result of the pathological process. Sometimes calcifications are also found in tumor structures, since a number of metabolic reactions in the affected tissues proceed pathologically.
Calcifications are not accompanied by a clinical picture. The condition is asymptomatic and does not cause concern to the woman. Calcifications are usually located in the muscle layer of the uterus. They can be found in any part of the uterus, the anterior and posterior walls. Placental calcifications, which form prematurely, can complicate the course of pregnancy. Typically, the accumulation of calcium in the form of lesions in the placenta is considered normal at the end of gestation, which means a full-term pregnancy.
Calcifications in the ovaries: signs and causes of formation, treatment methods
When the corresponding formations are found during an ultrasound, women, for obvious reasons, become very interested: calcifications in the uterus, what it is, whether it is a diagnosis, how dangerous it is.
In most cases, the gynecologist will say that this condition in itself is not a disease. This is a consequence of the disease, chronic inflammatory processes. Calcifications often form at the site of injury, for example, after complications arising from a difficult birth.
Sometimes they are confused with polyps, so a correct diagnosis is fundamentally important here.
Calcifications are deposits of calcium salts localized in a specific part of the uterus. It may appear at the site of formation of fibromatous nodes; more specific information can be obtained after hysteroscopy. During an ultrasound examination, it is only permissible to assert with some degree of probability that in this case we are talking about calcification.
What kind of phenomenon?
This is not a disease, it is a consequence of a pathological process in the main reproductive organ of the uterus. This phenomenon itself represents the localization of calcium salts in a certain uterine area.
Note that calcifications can occur not only in this organ, but also in other organs, for example, in the liver.
Thus, calcification is not only a gynecological disease, it is a pathological process that occurs due to disruption of the normal functioning of a specific organ.
Such formations are clearly visible during ultrasound and MRI. But during an ultrasound, the tissues that make up the formation are not visible, so the presence of calcification can only be assumed. This situation requires additional examination of the woman in order to exclude diseases much more serious than the presence of calcium salt deposits.
Calcification on ultrasound
What will a thyroid ultrasound tell you?
Okay, that was a lyrical digression. Let's talk about the thyroid ultrasound procedure itself. I will tell you what the norm and pathology look like in ultrasound reports.
Normal and pathological ultrasound of the thyroid gland
First, I’ll explain what an ultrasound procedure can tell you and your doctor. Ultrasound as a method can only show the structure of the thyroid gland, i.e. the structure and anatomy of the organ.
This method does not provide information about the function of the thyroid gland, i.e. how it works.
To find out, you need to take hormone tests, which you can read about in the article “Blood test for thyroid hormones: what you need to take.”
I think that there is no need to talk about the design and operating principle of the ultrasound machine, since this will not provide knowledge about your condition. Therefore, let's skip this point of my story.
Normal ultrasound of the thyroid gland
An ultrasound evaluates not only the internal structure of the organ, but also the size of the thyroid gland. According to the rules, three measurements of the gland are taken: length, width and thickness. But it happens that there are protocols with only two sizes - this is a serious mistake, and you will understand why, but a little later.
First, one lobe is measured, then the second and the isthmus. In fact, the size of the isthmus has no clinical value, so it can be ignored.
Next, the doctor must calculate the volume of each lobe and the total volume of the entire gland. This point is very often omitted and not done.
But this is fundamentally important, because the size of the thyroid gland is estimated precisely by its total volume.
If you have not done this, then you can calculate the volume manually using the formula below:
V thyroid gland = V right lobe + V left lobe
V of one share = length*width*height*0.479
where 0.479 is the ellipsoidal coefficient. As a result, we get the volume of one lobe of the thyroid gland, which is measured in cubic centimeters or milliliters.
Normally, in adult women, the volume of the thyroid gland does not exceed 18 cubic centimeters, and in adult men - no more than 25 cubic centimeters. For children, this formula is not used; the calculation is carried out in other ways, which are unknown to me, as an adult endocrinologist.
But now you don’t need to calculate your volume manually, because there are calculation calculators that will do it automatically faster and more accurately.
So, we figured out the sizes. But that’s not all, because the normal size of the thyroid gland does not always indicate the absence of pathology. The structure of the gland tissue can tell us a lot. Normally, the thyroid tissue is homogeneous, isoechoic, without focal formations, and the blood flow is moderate.
Thus, if you have normal thyroid size and normal structure, this means that the likelihood of pathology is low, but it is not completely excluded. To fully verify the normal functioning of the gland, you need a TSH test (which I talked about earlier).
Source: https://gidroz.ru/zabolevaniya/kalcinaty-miometriya.html
Reasons for formation
Calcinosis is a consequence of various diseases or disorders. There are dystrophic, metastatic and metabolic causes of tissue calcification.
The pathogenesis of the process of calcification deposition is due to:
- disruption of the endocrine system,
- changes in the acid composition of the blood,
- decreased production of chondroitin sulfate,
- hypervitaminosis D.
Calcifications are deposited in tissues that have undergone pathological changes or degeneration after necrotic lesions, in places where scar tissue has accumulated. They are found at the site of postoperative scars, inflammatory processes, fibromatous nodes.
Possible danger
Statistics show that calcinosis is more common in women than in men. Calcium metabolism disorders indicate serious pathological processes in the body. In women of reproductive age, calcifications can complicate the course of pregnancy due to disruption of the process of natural stretching of this organ; in a pregnant woman, they lead to disruptions in the supply of oxygen and nutrients to the fetus.
Reasons for education
Calcium is a conductor of nerve impulses, and therefore plays an important role in the body. In tissues, salts are deposited where cell death occurs as a result of inflammatory processes.
On this topic
Differences between cytology and colposcopy
- Natalya Gennadievna Butsyk
- December 6, 2020
Calcifications in the ovaries are detected as a result of past pathologies:
- adnexitis;
- difficult labor with compression of the ovaries;
- polycystic disease;
- follicular cysts.
Sometimes they occur when the venous outflow from the pelvic organs is disrupted, which occurs during prolonged sitting. Without oxygen, cells begin to die. The influence of hormonal changes on the deposition of calcium salts has been proven.
Every month, a woman’s ovaries produce a corpus luteum, a source of sex hormone production after ovulation. It consists of luteal cells interspersed with fat and reaches up to 1.5 cm in diameter.
7-8 days after ovulation, the corpus luteum involutes, loses the amount of fat in the membrane, and its body becomes white. It is at this moment that, using ultrasound, you can see a focus of connective tissue with calcifications - the result of natural cell death. The corpus luteum is completely reabsorbed within a few months.
On this topic
Echosigns of adenomyosis
- Olga Vladimirovna Khazova
- December 4, 2020
Calcifications can be signs of pathology, but their detection does not indicate ovarian cancer. Salt deposition occurs in only 8% of tumors, predominantly serous cancer. The formations have the shape of concentric circles.
Calcifications detected against the background of malignant tumors are divided into two types:
- metastatic, which are associated with hypercalcemia;
- dystrophic - formed against the background of destruction of epithelial cells and the formation of areas of necrosis.
This process is called ectopic calcification - outside the bone tissue. The deposit is caused by a disturbance in the metabolism of calcium and phosphorus.
Ovarian cancer cells produce specific substances that lead to destruction and changes in surrounding tissue. Calcification is also one of the criteria for tumor destruction during ultrasound examination.
Diagnostics
Ultrasound examination allows one to accidentally detect formations and suggest the presence of calcifications. Differential diagnosis is carried out with uterine polyps.
With calcinosis, a woman is usually worried about the symptoms of the underlying disease. Some patients complain of periodic nagging pain in the lower abdomen.
A gynecologist can clarify the hereditary history - ask whether the mother, grandmother, sister had a similar condition. Conduct a gynecological examination.
For a final diagnosis, the following studies may be needed:
- determination of the level of ionized calcium in the blood;
- transvaginal or three-dimensional ultrasound examination;
- X-ray examination of the pelvic organs;
It may be necessary to conduct hysterosalpingography - an X-ray or ultrasound examination with the introduction of a contrast agent or saline solution into the uterine cavity. Such a study will allow us to determine the location and size of deposits.
If a specialist suspects the presence of calcifications against the background of an inflammatory process - endometritis, the woman will most likely be recommended to do a general blood test and a blood test to determine the source of inflammation using a polymerase chain reaction or enzyme-linked immunosorbent assay.
A bacteriological examination of a vaginal smear - culture for pathological microflora and sensitivity to antibiotics will help determine the choice of antibacterial drug.
Sometimes a computed tomography or magnetic resonance imaging scan of the pelvic organs may be necessary.
Treatment
Only after diagnosing the root cause of calcification, a specialist will prescribe treatment. It is not necessary to surgically remove deposits of calcium salts from the reproductive organ. Surgery always poses a certain risk, and with calcification, the postoperative scar, on the contrary, can provoke the deposition of calcium salts.
Some Internet sites recommend curettage as a method of removing calcifications. The procedure is effective for endometrial hyperplasia, but it is impossible to “scrape out” areas of calcium salts from the muscular layer of the uterus.
Prevention
Since inflammatory processes lead to the deposition of calcium salts, women are advised to take preventive measures against chronic infections. In addition to observing the rules of personal hygiene, try to avoid hypothermia, decreased immunity, and the development of dysbacteriosis.
Pelvic congestion develops due to a sedentary lifestyle. Prevention is regular walking and visiting fitness centers. A routine examination by a gynecologist will help you not to miss more serious pathologies.
Physiological norm
Calcium salts are found in the body in dissolved form. This is completely normal, since this micromineral is directly involved in many reactions; it is necessary for the normal metabolic process inside. Scientists even suggest that people used to consume this substance three times more. A sufficient amount of calcium allows you not to suffer from brittle bones, ensures healthy teeth, and has a positive effect on blood composition and general well-being.
However, an excess of calcium salts leads to a disease such as calcinosis.
We are talking about calcification that occurs in the soft tissues of the body. The appearance of corresponding deposits inside the uterus is a particular manifestation of this process. Also, an excess of the substance under discussion can result in problems with joints, the formation of kidney stones, and bladder stones. With calcification, the kidneys are most often affected. Therefore, detection of deposits in the uterus should be the reason for a visit to a nephrologist to check the condition of the genitourinary system.
Conflicting opinions
It should be noted that most scientists cannot develop a common point of view on calcifications in the uterus. Some are convinced that this symptom is quite alarming and can indicate a serious hidden pathology inside the body. Others believe that the danger of such deposits is greatly exaggerated; as confirmation of their opinion, they cite statistics indicating numerous cases of successful births with this deviation.
Therefore, you should not be surprised when faced with completely opposite opinions. One gynecologist may advise doing nothing, while another may recommend medications that will stabilize the amount of calcium in the blood. A separate group of scientists suggests that when calcifications are detected in the soft tissues of the body, a special shortage of the corresponding salts should be achieved. After this, the body can “reach out” for replenishment, due to which the tumors will be reabsorbed independently without additional effort.
However, another group of doctors does not agree with this practice. They indicate poor process control. It is difficult to say whether such a reaction will be caused or in what specific time frame. The lack of one of the most important components of the normal metabolic process can seriously affect overall well-being. As you might guess, this is far from improving. If other health problems are added to the calcifications in the uterus, for example, a decreased immune status, inflammatory processes, then such experiments can only lead to a general deterioration. Therefore they are undesirable.
Calcifications in the ovaries: signs and causes of formation, methods of treatment - Women's Question
Calcifications in the ovaries do not threaten the health and life of the patient. They are compactions that form as a result of the deposition of calcium salts in the ovary.
Such manifestations are typical for women who have had inflammatory processes in the ovaries. Very often, deposits form at the site of injury, for example, after a difficult birth.
Calcifications can be confused with polyps, so their presence must be diagnosed by an experienced doctor.
The deposits are localized in the uterus. They can form on fibromatous nodes. You can find out the exact location of calcifications during hysteroscopy. This diagnostic method is more accurate than ultrasound examination.
Let's figure out what calcifications in the ovary are. Formations exist in dissolved form. This happens because calcifications are involved in many reactions of the body and help normalize the metabolic process.
A sufficient amount of calcium in the body has a positive effect on the condition of nails, teeth and bones. Calcium has a positive effect on the patient’s blood and general well-being.
But excess calcium provokes the occurrence of calcification in soft tissues.
Important! When the formations spread throughout the uterus, women develop kidney and bladder stones. Moreover, the kidneys suffer to a greater extent. Therefore, a woman needs to visit a gynecologist who will check the genitourinary system and prescribe treatment for the presence of calcifications.
If we talk about the seriousness of the disease, the opinions of doctors are divided. Some gynecologists argue that these formations indicate the presence of a serious pathology inside the body. Others consider this statement to be exaggerated, since many patients successfully carried a child and gave birth in the presence of calcifications.
Therefore, women should not be alarmed by the different opinions of gynecologists. Treatment is prescribed on an individual basis, since each woman’s body is unique. In some cases, doctors will prescribe medications that can regulate calcium levels in the blood.
Some doctors believe that in women with deposits it is necessary to create a calcium deficiency using special medications. This will give the body an incentive to make up for the lack of calcium, which it will draw from the formations.
Thus, the body starts the process of destruction of calcifications.
Other gynecologists fundamentally disagree with this statement. They believe that this process is difficult to control, therefore it is impossible to predict when the body will begin to make up for the deficiency from its own resources.
If the body does not have enough calcium, a woman’s metabolic process is disrupted, which affects her overall well-being.
We recommend you learn: About involutive changes in the ovaries and What are multifollicular ovaries
Diagnostics
In order to determine the presence of calcium deposits in the ovaries, doctors suggest that patients undergo an ultrasound examination. The choice of ultrasound technique depends on the degree and manifestation of the formation.
Most often, gynecologists recommend a transabdominal ultrasound to the patient. The ovaries are studied using ultrasound detectors. The patient's abdomen is lubricated with a gel, which reduces the slipping of the device. The examination does not cause the woman any discomfort.
Transvaginal examination is a more accurate method, as it makes it possible to examine the organ up close. A special sensor is inserted into the woman's vagina, which displays an image of the ovaries on a computer screen.
During the examination, the doctor moves the device, changing its angle. In this way, he manages to get a clear idea of the structure and size of the formation on the ovaries.
If an organ needs to be studied in more detail, doctors perform hysterography and Dopplerography.
Hysterography allows the doctor to examine the pelvic organs. The doctor can see the deposits using a contrast agent that is injected into the woman's vagina. Dopplerography is a method through which the doctor determines the intensity and direction of blood flow in the organs of the genitourinary system.
The most popular method recently is three-dimensional ultrasound. It differs from standard diagnostic methods. This procedure allows the doctor to examine in detail the structure of the organ and its defects in three dimensions.
Although the cost of this procedure is higher than the price of a standard ultrasound examination, 3D ultrasound is more reliable. The data obtained during the study is compared with standards and recorded in the medical history.
Based on the examination results, the doctor determines the presence of abnormalities and also determines the treatment method. We recommend you find out:
Is it possible to heat the ovaries during inflammation and what is an anechoic formation in the ovary?
Source: https://iemc.ru/patologii-yaichnikov/kaltsinaty-v-yaichnikah-priznaki-i-prichiny-obrazovaniya-metody-terapii.html
Solution
A solution to the problem seems quite reasonable, in which the woman is asked to undergo a comprehensive examination. If there is some kind of hidden pathology, a chronic gynecological disease that decides to make itself felt in this way, it needs to be identified and worked with the root cause. In any case, the general normalization will definitely not make things worse.
A blood test is also taken to examine the total amount of calcium. The diet is often adjusted to increase sodium (especially if there is a lack of sodium) and reduce the amount of foods containing the first micromineral. By achieving this balance, the appearance of further tumors can be prevented.
Treatment may vary depending on the woman's age, her general condition, and whether she plans to have a child in the future.
The uterus of a pregnant woman undergoes certain transformations. It should stretch due to natural flexibility. However, calcifications deprive soft tissues of such an opportunity; any change in size occurs in a traumatic way, causes severe pain, and sometimes bleeding can occur. For this reason, it is advisable for a woman to first remove calcifications before a planned pregnancy.
Surgical intervention is rarely allowed; if the problem is mild, it can be removed by curettage (cleaning). However, it is worth keeping in mind that the last named procedure can also provoke the further appearance of calcifications. Therefore, you should be careful here.