What is leukocytosis in a child and its classification
White blood cells are synthesized by the bone marrow to provide the body's immune response to the penetration of infectious agents. They rush to the site of injury, capture pathogenic microorganisms, destroying their cellular structure, and produce antibodies, which promotes rapid recovery.
The detection of a high number of leukocytes in the blood of a child indicates the development of pathologies characterized by inflammation of various parts of the body, and its fight against infectious agents. It is impossible to make a diagnosis based only on the level of white blood cells, so doctors prescribe additional diagnostic methods.
Doctors classify leukocytosis in the blood of children according to the type of etiological factor:
- physiological. It is caused by the influence of external factors and is not associated with the development of diseases;
- pathological. It is a sign of various diseases. To relieve symptoms, drug therapy is necessary, which is prescribed after confirmation of the preliminary diagnosis.
When taking a general blood test, you must follow certain rules, since neglecting them leads to distorted results. If the doctor identifies such factors during the survey, the study is recommended to be repeated.
Leukocytes in the urine of an infant
A clinical urine test quite informatively illustrates the general condition of the body and the presence of various pathologies. Determining the total number of leukocytes in the urine of an infant greatly facilitates diagnosis and subsequently helps in the treatment of identified diseases.
The normal level of leukocytes in the urine of an infant varies significantly depending on the sex of the child. For girls, a normal indicator is considered to be a leukocyte count of 8-10 cells per field of view, for boys 5-7. The difference is explained by differences in the anatomical structure of the genitourinary system in children of different sexes. In girls, such cells are formed more often as a result of the close proximity of the vagina and the entrance to the urethra, since in this case there is a high probability that the cells will enter the urine along with vaginal discharge, and not from the genitourinary system.
It is important to note that the inflammatory process is directly dependent on how many leukocytes are released during urination. The more of them are released, the more active the inflammation process is.
In addition, the transparency of the urine decreases, it becomes cloudy, and the sediment becomes more pronounced.
Leukocytes in a baby's urine appear as a result of infection entering his body. In this case, the action of protective systems is activated, which, among other things, includes inflammatory cells. Their action is capable of destroying, neutralizing and absorbing pathogenic bacteria, thus eliminating the causative agent of the disease. Thus, it becomes clear that the detection of leukocytes in the urine of an infant may indicate the following diseases:
- process of inflammation of the urinary tract. This could be cystitis or urethritis;
- inflammation of the external genitalia;
- stagnation phenomena caused by abnormalities in the structure of the urinary tract;
- violations of the rules of personal hygiene of the child, they may have forgotten to wash themselves or did it poorly before collecting material for analysis. This also includes the presence of diaper rash.
If an insufficient amount of material is collected for research, errors in the final results of the analysis may occur. A more reliable and accurate way to clarify the diagnosis is the Nechiporenko analysis, which shows the level of leukocytes per milliliter. This particular method can confirm or refute the presence of an infectious agent in the baby’s body. In order to identify it, culture is carried out on a nutrient medium.
Norm
The value of the parameter depends on the age of the child, so a special table is used to interpret the results. In the first days of a baby’s life, the cell level will be at its highest, as the child’s body adapts to new living conditions.
Standard indicators of leukocyte levels in a child’s blood test
| Age | Value, x109/l |
| Newborn | 10-30 |
| 5th day | 9-15 |
| 10-30 days | 8-14 |
| 1-6 months | 6-12,5 |
| 6-12 months | 6-12 |
| 1-2 years | 5,5-11 |
| 2-5 years | 5-11 |
| 5-10 years | 5-10 |
| 10-15 years | 5-10 |
| Over 15 years old | 4-9 |
Attention! An increased level of leukocytes in the blood of a newborn is often associated with a stressful state of the body that occurs during a difficult birth.
These table values are conditional, because different laboratories have their own reference intervals. Therefore, the analysis should be deciphered by a specialist who will take into account the patient’s age and the influence of endogenous and exogenous factors.
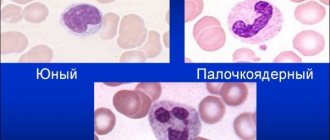
Leukocyte formula
Why can bleeding come from the ear of a child under one year old when cleaning?
The leukocyte formula characterizes the values of all types of leukocytes. In this case, not only their absolute values are determined. It is important what percentage each type occupies in the total volume of blood cells.
Normal values for a child
Normal values for a child depend on his age. So the indicators on the first day of life and a month later are very different.
Normal values of leukocytes in a child under one year old
| Index | Newborn | 1 month | 6 months | 1 year |
| Leukocytes, *〖10〗^9/l | 8,5-24,5 | 6,5-13,5 | 5,5-12,5 | 6,0-12 |
| Band neutrophils, % | 1-17 | 0,5-4 | ||
| Segmented neutrophils, % | 45-80 | 15-45 | ||
| Eosinophils, % | 0,5-6 | 0,5-7 | ||
| Basophils, % | 0-1 | |||
| Lymphocytes, % | 12-36 | 40-76 | 42-74 | 38-72 |
| Monocytes, % | 2-12 | |||
Changing indicators allows you to evaluate the processes occurring in the body and determine the presence of a viral or bacterial infection.
There is such a thing as a shift in the leukocyte formula:
- It shifts to the left if the number of band neutrophils increases. This means that the body is under the influence of infection;
- The formula shifts to the right, respectively, with a decrease in band neutrophils and an increase in segmented neutrophils. This may indicate problems with the kidneys and liver.
In any case, test results alone do not provide a complete picture of the child’s condition. After an examination, in particular, examining the throat, palpating the lymph nodes and talking with the parents, the doctor will prescribe additional tests to make an accurate diagnosis and prescribe treatment.
Usually, the first step is to undergo a general urine test to rule out a urinary tract infection and monitor kidney function.
Doctor visit
Note! Only a specialist who understands what could increase and decrease the main indicators can decipher the test results. He will immediately determine whether we are talking about a dangerous disease or whether there is no need to worry.
Reasons for the increase
White blood cell levels vary throughout the day. Often its increase is observed in the evening due to the influence of various external factors. Therefore, tests are taken in the morning so that the concentration of blood cells normalizes after sleep. Pathological causes of deviation from the norm are considered more dangerous, as the risk of developing serious complications and the need for long-term treatment increases.
An increased level of leukocytes in a child’s blood is considered safe in the following cases:
- excessive physical and emotional stress;
- prolonged exposure to the sun or cold;
- change of climatic zones;
- the presence of a large amount of meat in the diet;
- introduction of complementary foods, transition from breast milk to artificial formula;
- period after vaccination;
- stress;
- poor sleep;
- taking a number of medications;
- premenstrual and postoperative period.
Under the influence of these factors, leukocytes in the blood are slightly increased, their level quickly returns to normal. Physiological leukocytosis does not require therapeutic intervention.
Pathological reasons for the excess of leukocytes in a child’s blood test:
- infections of viral, bacterial and fungal nature;
- acute and chronic course of inflammatory diseases;
- autoimmune pathologies;
- poisoning;
- allergic reactions;
- injuries accompanied by large blood loss;
- malignant tumors;
- kidney diseases provoked by hormonal and antibacterial therapy;
- pathologies of the circulatory system;
- infections accompanied by purulent inflammation;
- extensive burns;
- diseases characterized by increased secretion of leukocytes in the bone marrow;
- rickets;
- parasitic infections.
It is possible to establish an accurate diagnosis and narrow down the number of possible causes of deviation only by considering other parameters of a general blood test. With a simultaneous increase in platelet concentration, the development of a tumor process (erythremia, myeloid leukemia) is assumed. An increase in the level of neutrophils indicates a bacterial infection, lymphocytes - a viral infection, and eosinophils - a parasitic infection. With an increase in monocytes, the presence of disturbances in the functioning of the bone marrow is assumed; basophils - the negative effects of allergens.
Attention! If the etiology of leukocytosis is unclear and there are no symptoms of the disease, it is recommended to exclude all provoking factors and periodically repeat the clinical study.
Reasons for low leukocyte levels
A decrease in the number of white cells in the blood is called leukopenia. This deviation is rare in newborns. A lack of leukocytes indicates that the process of their production by the bone marrow is slowing down. An examination of the child is required to identify the causes of leukopenia.
- HIV infection transmitted from mother to fetus. If during pregnancy a woman took medications to prevent infection of the fetus, the number of leukocytes in an infant may decrease relative to the norm. Infection of the fetus is possible with premature rupture of intrauterine fluid, with a prolonged stage of the disease, with early birth and breastfeeding.
- Toxoplasmosis is a parasitic disease transmitted from animals. Damage to the fetus occurs if the mother has been infected and there are no antibodies to the disease. During pregnancy, all women are required to take a blood test for toxoplasma, and doctors also advise avoiding contact with animals. Signs of the disease may be completely absent in a pregnant woman, but may cause severe visual and auditory disorders and nervous disorders in the child.
- Cytomegaly is a viral infectious disease transmitted from mother to fetus. The mother may not show signs of illness. Often, infection during pregnancy provokes premature birth, miscarriages, fetal death and developmental defects. The severity of complications depends on the stage of pregnancy at which the infection occurred, the timeliness and correctness of therapy.
- Listeriosis is an infectious disease caused by bacteria of the genus Listeria. The bacterium is transmitted to the fetus in utero through the umbilical vein and provokes an inflammation process. In this case, the mother may not know about the infection. The infection process occurs through milk and raw eggs.
In addition to the listed reasons for the decrease in the level of leukocytes, it can also be noted that a pregnant woman takes medications that help reduce white cells and slow down the process of their production. In this case, a deviation from the norm is not a pathology and the leukocyte level will gradually recover.
Leukocytes are important blood cells that perform a protective function in the body of both adults and children. If their level deviates from the norm in infants, a thorough examination is required, which will allow timely treatment to begin and avoid the development of complications. It should be noted that during pregnancy, the mother needs to take responsibility for her health. Following doctors' recommendations will help avoid undesirable consequences for the unborn child.
Symptoms
The clinical picture of the deviation is often accompanied by signs of concomitant pathology. When the level of leukocytes in the blood is higher than normal in children, the following symptoms are noted:
- dizziness;
- headache;
- loss of appetite;
- diarrhea;
- nausea;
- vomit;
- weakness;
- poor sleep;
- sudden changes in weight up or down;
- increased sweating;
- joint and muscle pain;
- decreased vision;
- high body temperature;
- fast fatiguability;
- causeless appearance of bruises, hematomas;
- fainting.
Toddlers usually become whiny and capricious, and older children have a sharp drop in concentration, which causes problems in learning. With minor deviations from the norm, symptoms may be mild and any deterioration in health is attributed to the manifestation of the underlying pathology.
Leukocytes in infant stool
The level of leukocytes in the stool of an infant is one of the main indicators of a coprogram - a general analysis of stool. Research data provides the opportunity to determine the presence of inflammation in the gastrointestinal tract and disruptions in the enzymatic state of digestion.
A single white blood cell count in the stool of an infant is normal. Often their number in the sphere of visibility does not exceed ten. If there is an increased content of white blood cells, this is a signal of a violation of the internal intestinal microflora.
The most common reason for an increase in the level of leukocytes in the stool of an infant is prolonged diarrhea, which causes the loss of a large amount of fluid. The combination of leukocytes and mucus in the stool should cause particular concern.
A sharp increase in the level of leukocytes in the feces of an infant may indicate a number of diseases:
- the onset of follicular rhinitis is characterized by the presence of mucus in the form of lumps in the child’s stool;
- dysbacteriosis is indicated by the presence of cocci, E. coli with a high level of leukocytes in the feces;
- an increased content of eosinophils - leukocytes that destroy foreign proteins, indicates the onset of allergic colitis;
- the appearance of neutrophils - leukocytes that carry the function of protection against various infections, leads to the conclusion about the onset of ulcerative colitis;
- dysentery is characterized by an increased number of neutrophils and general intoxication of the whole body. In this case, urgent measures to correct the situation are necessary, since the trend is extremely dangerous;
- Spastic colitis is indicated by a changing number of leukocytes combined with undigested fiber.
In the case when the baby’s feeding process is not structured correctly, disturbances in the daily diet occur, and the appearance of white blood cells may also occur.
However, it is important to know that quite often there is an increase in the number of leukocytes in the feces even in a completely healthy baby. This suggests that with the disease, deterioration in the general condition of the child, the presence of intestinal colic, loss of body weight and an allergic rash are of greater importance.
When the baby feels well, his appetite is not impaired, he does not feel unwell, he does not have pain in the abdominal area - parents should not be afraid of the greenish tint of the stool.
When your health worsens significantly, you should immediately consult a doctor. You should not self-medicate - in the case of infants this is strictly contraindicated.
Diagnostics
OAC helps to detect elevated leukocytes in a child’s blood. To clarify the cause of the development of leukocytosis, the doctor carries out the following diagnostic measures:
- physical examination of the patient;
- asking parents about the nature and time of onset of symptoms if the baby is not able to describe them himself;
- study of anamnesis;
- clarification of the presence of external provoking factors.
Additional diagnostic methods are:
- general urine analysis;
- blood culture;
- stool microscopy;
- radiography;
- Ultrasound;
- CT;
- MRI.
With the results of the examination, the child is referred for consultation to specialists who, together with the pediatrician, determine the treatment method.
In order for the decoding of the CBC to be reliable, it is recommended to follow the following rules before the study:
- exclude spicy and fatty foods from the menu 2 days before blood sampling;
- with the permission of the doctor, stop taking medications that affect the level of analysis parameters the day before the test;
- eliminate the impact of physical and emotional stress. It is recommended to explain to the child in advance how the procedure will take place so that it does not provoke stress;
- The last meal should be taken 8 hours before blood donation (for infants this time is reduced to 2 hours);
- In the morning you are allowed to drink clean water, which does not affect the results of the study.
Attention! It is advised to arrive at the laboratory early so that the child gets used to the hospital environment and understands the safety of the procedure.
Treatment
When pathological leukocytosis is confirmed, the treatment method is selected taking into account the type of pathology that provoked its development. For children, a conservative treatment method is usually used, which consists of taking medications, following a diet, and using folk remedies.
Taking into account the type of disease, the increased level of leukocytes is normalized with the following drugs:
- antibacterial;
- antimicrobial;
- antifungal;
- NSAIDs;
- antiallergic;
- vitamin and mineral complexes.
In case of poisoning, sorbents are used that relieve intoxication of the body. Treatment of leukemia and malignant tumors involves chemotherapy. In severe cases, leukophoresis is prescribed, during which leukocytes are extracted from the blood using a special apparatus.
The type of drug, its dosage, and duration of use are determined by the doctor. He can make any changes to the treatment regimen only after re-taking the analysis and deciphering the results. You cannot independently draw a conclusion about the need to stop therapy. If the level of leukocytes has decreased, but has not reached normal, and the medication has been stopped, then a relapse is possible.
Folk remedies that are used only with the permission of a doctor help to increase the effectiveness of treatment and speed up recovery. To reduce high levels of leukocytes, it is recommended to drink decoctions of lingonberries, strawberries, propolis, horsetail, birch buds, and linden flowers.
Plant components can provoke allergies in children, so it is advised to give the first portion of the folk remedy in a small amount and monitor the child’s condition. If his health worsens, you should stop taking such medications and consult a doctor. For this reason, traditional therapy is contraindicated for newborns.
How to treat leukocytosis?
Treatment can be prescribed only after the exact cause of this phenomenon has been established, for example, physiological leukocytosis is considered to be the norm. As soon as the causative agent of the infection is detected, the following drugs may be prescribed to the small patient:
- Antiviral agents that effectively fight viruses.
- In severe cases, antibiotics may be prescribed, but they are taken only as prescribed by a doctor.
- Chemotherapy drugs that are aimed at maintaining the immune system.
Sometimes, when leukocytosis is detected in children and the blood has a viscous consistency, leukapheresis is prescribed, during which the blood is purified.
Diet for leukocytosis
If the leukocytes in a child’s blood are elevated, then nutrition is selected taking into account the cause of the symptom. To maintain immunity, it is recommended to make easily digestible foods high in proteins and vitamins the basis of your diet.
The diet requires adherence to the following principles:
- daily fluid intake is 1.5-2 liters;
- meals should be frequent and small;
- preference in the menu is given to plant foods, cereals, legumes, nuts, water soups, stewed vegetables, fruits, low-fat fish and fermented milk products.
Attention! If leukocytes in the blood are high, then sweets, spicy, fried, fatty foods, and foods that can cause allergies are completely excluded from the menu. Meat is allowed in limited quantities.
How can leukocytosis be recognized?
A child may not have any symptoms; sometimes leukocytosis can be detected only through diagnostics, which is why doctors recommend taking a baby’s blood test at least once every six months so that you can respond to such a deviation in the body in a timely manner.
Of course, sometimes you can recognize increased leukocytosis in a child if you pay attention to the following symptoms:
- A small child may get tired quickly, vision deteriorates, dizziness appears, the baby may complain of pain in the legs and sleep often.
- Sometimes low-grade fever occurs.
- The baby sweats a lot, but his body remains cold.
- Weight loss quickly and appetite completely disappears.
- At night the child sleeps restlessly.
You should pay attention to all these signs, as this may primarily indicate an inflammatory process in the child’s body, and this is also how a viral infection can begin. As we can see, if a diagnosis reveals leukocytosis in a child, the causes can be looked for in completely different directions, so a qualified specialist must prescribe treatment.
Complications
An increased number of leukocytes cannot be ignored in the absence of pronounced symptoms of the disease. Inflammation that becomes chronic becomes the cause of dangerous complications.
The long course of such diseases leads to disturbances in the psychoemotional and physiological state of the child, which threaten developmental delays and disability. If diagnosed untimely, leukocytosis provokes the transformation of benign tumors into malignant ones, characterized by a high risk of death.
Any deviations in health, accompanied by changes in the level of blood components, can be life-threatening for the child. It is important to promptly determine the cause of their development and begin treatment.
Prevention and prognosis
Most of the reasons that provoke an increase in white blood cells can be prevented by following the following recommendations:
- undergo medical examinations in a timely manner;
- avoid overheating and hypothermia;
- control the level of physical activity;
- avoid stress and injury;
- balance the diet;
- do not neglect therapeutic courses and medications for chronic pathologies;
- do not refuse vaccination;
- support immunity;
- maintain a daily routine;
- limit contact with sick people;
- do not self-medicate;
- be outdoors regularly.
When leukocytes increase, the prognosis of the health condition depends on the root cause of the symptom, the time of contacting a doctor, and compliance with his recommendations. Serious consequences threaten with the development of dangerous pathologies and refusal of treatment.
A lot of leukocytes in the blood is not always a sign of disease. High levels of white cells are observed in children due to exposure to various physiological factors. This phenomenon passes quickly and does not require medical intervention. If their concentration exceeds the norm due to the development of pathology, then the lack of treatment can lead to dangerous consequences. The right decision in this case would be to follow all medical recommendations.
Diseases in which leukocytes are elevated
If the blood test was done according to the rules, an increase in leukocytes will indicate a pathological process in the child’s body. An indicator above the norm is typical for the following pathologies:
- Purulent infections, for example, meningitis, otitis, appendicitis, pyelonephritis, cholecystitis, pneumonia and others. With abscesses or sepsis, the level of leukocytes increases several times.
- Inflammatory diseases, such as chronic inflammatory bowel disease or arthritis.
- Poisoning from spoiled food, heavy metals, drugs and other poisons.
- Viral infections, for example, bronchitis, ARVI, rubella, hepatitis.
- Allergic diseases.
- Infection with fungi and protozoa.
- Rheumatism.
- Autoimmune diseases.
- Burns.
- Injuries.
- Blood loss, as well as blood transfusion.
- Oncological diseases.
- Bone marrow lesions.
- Splenectomy.
Also, an increased level of leukocytes is detected in children who have undergone surgery. While the child is recovering, the leukocytes in his blood will be elevated.