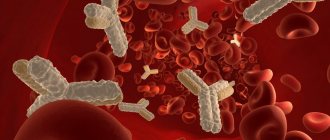
The formed cells that circulate throughout the body are represented by a wide group of structures. The following elements can be roughly distinguished:
- Leukocytes. White bodies. Participate in all immune reactions without exception. They themselves are heterogeneous. They exist to protect the body. This is a kind of defense force.
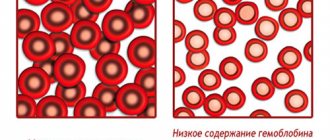
- Red blood cells. Red blood cells. They act as transporters of carbon dioxide and oxygen. Without them, there can be no tissue respiration, and, consequently, life itself as such. Any deviations in the red blood cell count are accompanied by ischemia and disturbances in the functioning of the body.
- Platelets are red blood platelets. They do not have a core, they act as temporary building material. They close the wound surface and do not allow liquid connective tissue to leave the vessels.
PLT in blood testing is the abbreviation for platelets. In the general study (GSC), this is how the number of formed elements is designated.
Deviations clearly speak in favor of bone marrow diseases, inflammatory processes, liver disorders and other conditions.
The role of platelets in the body
If we talk about the functions of these formed cells, they can be represented by the following list:
- Creation of a primary plug that prevents blood from leaving the body. This process takes place in several stages. It all starts with adhesion, that is, attachment to a damaged vessel.
Then aggregation is observed. The clumping of platelets, the creation of the actual plug itself. Fibrinogen takes an active part in the process. A special protein that ensures the connection of platelets.
- Regeneration of damaged tissues. As it turned out recently, the plates are also capable of producing special substances that increase the intensity of cell division in place. Thus, normal tissue restoration is accelerated. This is another powerful feature.
- Nutrition of the vascular wall. A close task. The point is to restore normal blood circulation at the local level. This happens due to the release of special substances.
How to improve your performance
If there is no threat of severe bleeding or intracranial hemorrhage, wait-and-see tactics are more often used in children. With a progressive decrease in PLT, Prednisolone is urgently administered.
In adults, spontaneous recovery is rare. More often, in a hospital setting, the patient is administered Prednisolone, Immunoglobulins and Steroids. If there is no positive dynamics, the spleen is removed.
From helper methods
There is no special diet, but a gentle approach to nutrition is recommended. It involves eliminating fatty, fried and spicy foods and alcohol.
Traditional medicine offers infusions and decoctions of strawberry leaves.
Tables of norms by age
The abbreviation PLT (short for platelets) in a general blood test refers to platelets.
The rate of red plates, regardless of gender, is highest in the first days after birth and steadily decreases with age.
Among women
| Age | Indicator in thousands U/μl |
| Up to 17 | 160-382 |
| 17-25 | 170-380 |
| 26-36 | 175-400 |
| 37-60 | 170-350 |
| 60 years and older | 175-310 |
The PLT norm in women is in the range of 160-400 thousand units/μl of blood and may vary slightly during one age interval, deviating from the presented calculations.
In men
| Age (years) | Norm in thousands of units per µl |
| Up to 17 | 175-380 |
| 17-25 | 175-390 |
| 26-36 | 185-400 |
| 37-60 | 190-395 |
| 60+ | 175-370 |
In children
| Age | PLT level thousand units/µl |
| Newborns | 180-490 |
| First month | 185-400 |
| Up to a year | 180-400 |
| 1-2 years | 155-390 |
| 2-3 years | 160-385 |
| 3-10 years | 160-380 |
During pregnancy
| Trimester | Normal value (thousand units/μl) |
| I | 170-340 |
| II | 155-321 |
| III | 145-310 |
The PLT norm in a blood test is a dynamic level, we are talking about ranges from 145 to 490 thousand units/μl of blood. Natural factors can also affect the results: physical activity, stress, habits. Also past illnesses. This needs to be taken into account.
Low platelet count
The reason for low PLT in the analysis may be:
- decreased production of platelets in the bone marrow due to diseases of the blood, thyroid gland, or liver. Also, a decrease in the indicator may be observed due to the effect on the body of a viral infection or intoxication;
- rapid destruction of platelets, which may be associated with the following diseases/conditions: thrombocytopenic purpura, infectious, autoimmune or oncological diseases, blood transfusion or the use of certain drugs (antihistamines, sulfonamides);
- disturbance of the distribution of blood platelets in malaria, tuberculosis or viral hepatitis.
Liver disease may cause low PLT levels
The following symptoms may indicate that PLT is low:
- severe bleeding that develops after surgical procedures or tooth extraction;
- subcutaneous hemorrhages of various sizes. Initially, they may look like small dots, but later merge into large spots and bruises. They can occur independently or after minor damage to the skin;
- rashes on the skin that have different colors; depending on the time of appearance, they can be brown, blue, red, green or yellow;
- prolonged and very intense bleeding during menstruation;
- nosebleeds that appear spontaneously;
- development of uterine, gastric, hemorrhoidal or pulmonary bleeding;
- enlarged spleen;
- hemorrhages in the retina or brain;
- pain in the joints.
Reasons for the increase
An increase in platelet concentration or PLT is associated with pathologies of the excretory, hematopoietic or digestive systems. Other problems are also possible.
Let's try to summarize the list of pathological processes.
Inflammatory conditions
Multiple in character and properties. We are talking about a variety of disorders. This can include infectious and autoimmune diseases.
Particularly common are:
- Respiratory problems.
- Respiratory system lesions.
- Lupus erythematosus.
- Rheumatoid arthritis.
- Autoimmune disorders of the heart, myocardium.
- Crohn's disease.
And others. There are actually dozens of options. Just look at the ICD classifier to get an idea of the number of possible diseases.
Symptoms depend on the specific pathological process. If we talk about a general clinic, there will always be the following symptoms:
- Uncomfortable sensations.
- Increased body temperature. Systematic or rare. Indicators are also determined by the disease.
- Weakness, nausea, drowsiness.
For the rest, you need to start from a specific diagnosis. Therapists and rheumatologists treat pathological processes.
Correction includes the use of antibiotics, anti-inflammatory drugs, and antiviral agents. If there is an autoimmune process, glucocorticoids cannot be avoided. If they are ineffective, immunosuppressants are prescribed.
The list of medications, as well as treatment regimens, is determined by the doctor. PLT values will return to normal on their own as soon as the underlying disease is treated.
Sepsis
It stands apart from other pathological processes. We are talking about generalized inflammation. All body systems are involved. The disorder is always infectious in nature. It is provoked by a variety of agents.
The condition is accompanied by several typical symptoms.
Among them:
- Pain of unclear localization.
- Serious increase in body temperature.
- Impaired consciousness. If nothing is done, the patient will very quickly go into shock and die.
Sepsis is a deadly disorder. The concentration of platelets in this pathological process increases rapidly. This is due to the body's attempts to compensate for the disorder.
Treatment is carried out strictly in intensive care. Loading doses of antibiotics are prescribed. Hardware methods of blood purification. The goal is to return the patient to an adequate state.
The primary disorder is then treated. The one that provoked the development of generalized inflammation.
Oncological processes
Simply put, cancer. Benign tumors do not cause an increase in PLT concentration. Localization doesn't matter much. However, the process is especially aggressive during the degeneration of bone marrow cells. Which is quite understandable: this is where the formed elements of blood are produced and mature.
For cancer, especially advanced cancer, a typical group of symptoms is:
- Increased body temperature. Up to 37-38 degrees. The condition is stable, because the body is poisoned by the decay products of neoplasia.
- Weakness, drowsiness. Loss of performance.
- Loss of body weight. The person is not getting better. This is due to the increased need of altered tissues for nutrition.
The clinic is also focal. Depends on the type and location of the formation. Its size.
The therapy is carried out by oncologists. The goal is to remove the tumor. It is excised surgically. Chemotherapy and radiation treatment are provided as needed.
An increased concentration of PLT means that the cancer continues to develop. Based on the dynamics of the indicator, it is quite possible to talk about the progress of the process.
Consequences of surgical interventions
This includes almost any surgical treatment that affects the spleen. This organ acts as a kind of storage facility for blood cells.
If damage occurs, platelets (among others) are released into the bloodstream, PLT in the blood is increased steadily, although there is a temporary increase in the indicator.
Then, after a few weeks, everything returns to normal. It is possible that the process of change will end many times faster.
A pathological condition is also observed with injuries to the spleen. For example, its increase and further rupture. Deposited reserves of blood cells circulate throughout the body and are recorded using objective laboratory methods.
There is no need for correction as such. After surgery, you just need to wait. After some time, everything will recover on its own. If we talk about injuries, surgical treatment is necessary. Splenectomy.
Anemia
Most often, this reason for an increase in platelet count is observed in younger patients. From approximately 3 to 12-15 years. Although changes are also possible in adults.
Elevated PLT indicates anemia due to insufficient iron intake or absorption. This is a classic case. Other options are also possible: megaloblastic forms, congenital pathological conditions.
The clinical picture, especially in the early stages, is atypical or completely absent.
Typical symptoms include:
- Weakness, drowsiness.
- Increased sweating.
- Decreased performance.
- Nausea.
- Brittle hair and nails.
- Paleness of the skin.
- Decreased exercise tolerance.
- Perversion of taste preferences.
Bleeding is possible despite a formally high platelet count. They do not perform their function sufficiently, although there are many of them.
Treatment is carried out under the supervision of a hematology specialist. Therapy involves external administration of a deficient substance. Whether it's iron or vitamins.
If the problem is in the absorption of a beneficial compound, the cause must be treated. Gastritis, inflammation of the digestive tract.
Blood levels of PLT will remain high until the anemia resolves. Therapy may take more than one month. As a help, a diet is prescribed. Balanced, fortified diet.
Read more about the causes and treatment methods of iron deficiency anemia (IDA) here.
Colitis
Isolated inflammatory process. We are talking about intestinal damage. Thin or thick, that's a different question. The point is different.
The disease is accompanied by bleeding. Even if not so noticeable at first glance. The body is forced to produce more formed cells to replace those that are eliminated, this leads to an increase in the concentration of PLT. Until the condition is stabilized, the disorder will not stop.
Colitis is accompanied by typical manifestations, so it is difficult not to notice it.
Among the clinical signs of the disorder:
- Stomach ache. Intense, cramping.
- Nausea.
- Vomit.
- Weakness.
- Diarrhea. Including interspersed with mucus, blood, pus.
- Disorders of normal digestion.
- Increased body temperature.
Treatment rests on the shoulders of a gastroenterologist. The goal is to stop the inflammatory process. It almost always has an infectious origin.
Antibiotics and drugs are prescribed to restore microflora and protect it. Therapy requires several weeks.
During this entire time, be sure to adhere to a gentle diet. The diet is developed individually or a standard treatment table is used for patients with colitis.
Blood clotting disorders
The platelet concentration may change if coagulation (blood clotting) occurs directly within the vessel itself. This is the so-called DIC syndrome.
The disease is associated with profound fundamental changes in the body. In this case, a paradoxical situation is observed.
On the one hand, platelets stick together and die, breaking down on their own. On the other hand, the body produces them in inadequately high concentrations, which is why an abnormally high level of PLT is recorded.
The condition does not have any specific symptoms. However, it causes a lot of discomfort to the patient.
Among the clinical manifestations:
- The appearance of hematomas and bruises on the body for no apparent reason.
- Thrombosis. They are more likely to be considered complications. The formation of clots can lead to tissue necrosis. The condition is often urgent and requires hospitalization and intensive treatment.
Therapy is carried out under the supervision of a hematologist. As a rule, this is not a quick matter. Up to several months of close correction is required.
The problem is solved with the help of anticoagulants and antiplatelet agents. The prognosis is mostly favorable.
Genetic abnormalities
In some cases, the reason lies deeper than it seems at first glance. The pathological process may well be congenital.
In this case, the bone marrow works too intensively. Produces many shaped cells. And not necessarily only platelets. Complex disorders also occur.
Diseases are caused by mutations and are established before birth. If nothing is done, life-threatening complications are likely.
There are no symptoms as such. Thrombosis is possible. The abundance of red plates makes the blood thicker, this is a serious risk factor.
Treatment as such makes no sense. At least radical ways. All that remains is symptomatic correction. The problem is that the violation is encoded at a genetic, deep level. There's nothing you can do about it.
As for methods that will alleviate the condition, anticoagulants and antiplatelet agents are prescribed. They help prevent thrombosis and serious complications.
An increase in indicators indicates in favor of diseases.
Etiology
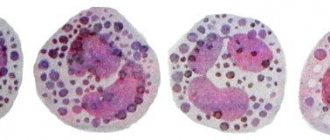
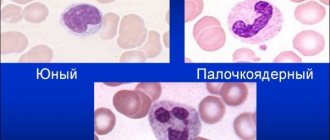
Normally, the size of red blood cells in the blood of a healthy adult can vary from 6.8 to 7.5 microns. In children or adolescents, depending on the age category, the average cell volumes should not exceed the boundaries of 7 to 8.12 micrometers.
Red blood cells that are less than 6 microns in size are called microcytes, and their concentration is more than 25-75% of the total number of red blood cells - microcytosis of varying severity.
This pathological condition can be provoked both by the course of a serious illness and by factors that are not related to the disease.
Main provocateurs:
- microcytic or iron deficiency anemia;
- oxygen starvation of body tissues;
- microspherocytosis - in 75 cases it is of a hereditary nature; those genes that are responsible for the formation of the erythrocyte membrane, which take on a spherical shape, but after passing through the spleen are significantly reduced in size, undergo mutations;
- Thalassemia or Cooley's syndrome is a form of hemoglobinopathy that is inherited, characterized by a decrease in the formation of adult hemoglobin;
- chronic course of an infectious or inflammatory disease - cirrhosis of the liver, hepatitis, peptic ulcer of the duodenum or stomach, kidney pathology;
- the formation of oncological tumors with localization or metastases in the spinal cord, thyroid gland, lungs, prostate or mammary gland;
- congenital blood abnormalities;
- massive blood loss.
The occurrence of microcytosis can be associated with completely harmless conditions:
- pregnancy period - if the number of reduced red blood cells does not exceed 40%, there is no reason for concern for clinicians and the expectant mother;
- breastfeeding the baby;
- poor nutrition - lack of iron-containing foods in the diet;
- intake of insufficient amounts of vitamins and nutrients;
- nervous fatigue;
- hormonal imbalance observed in adolescents during puberty.
Microcytosis in the blood of a child is considered normal, but only before the age of 3 months. This is due to the incompletely formed composition of the biological fluid. By about 6 months from the moment of birth, the blood in children becomes approximately the same as that of an adult. This means that the quantitative and qualitative composition of red blood cells should return to normal.
Reasons for the decline
This condition occurs no less often. Among the development factors.
Hepatitis
Inflammatory liver damage. Accompanied by acute dysfunction of the organ. In the chronic phase it is not so dangerous.
Among the symptoms:
- Pain in the right side of the abdomen.
- Nausea.
- Vomit.
- Change in color of stool.
- Diarrhea, constipation.
- Digestive disorders.
- Bitter taste in the mouth.
- Increased body temperature (not always).
The disease is progressing. Not at the same speed, but steadily. If nothing is done, necrotic changes will begin.
The condition is corrected under the supervision of a hepatologist. When such a narrow specialist is not available, a gastroenterologist is involved. The goal is to slow down, and ideally stop, change altogether. Protective drugs are prescribed.
Be sure to prescribe a gentle diet low in animal fat. If hepatitis is of infectious origin, you cannot do without special antiviral medications.
The prognosis for systematic treatment is positive, PLT concentration will recover quickly.
Cirrhosis of the liver
Necrotic process. Characterized by the death of organ tissue. In the acute phase, days and even hours count. It is necessary to transport the patient to the hospital. Then carry out urgent correction.
The clinical picture corresponds to that of hepatitis, only more severe. Problems begin with the nervous system and hematopoietic structures.
Among the manifestations:
- Pain in the right side.
- Impaired consciousness.
- Nausea.
- Vomit.
- Decline in cognitive level and intellectual abilities.
- Discoloration of stool.
- Diarrhea or constipation.
- Bleeding.
- The formation of spider veins on the body.
Chronic forms allow more time for treatment. Therapy consists of using protectors. We must do everything we can to stop the progression of the disease.
At the initial and middle stages of the pathological process, there is a chance of a liver transplant. The operation can only be successful during these periods.
In the decompensated stage, transplantation will make little sense. Bleeding begins and surgery is no longer possible. The disease is serious and must be dealt with quickly.
PLT decreases because cells die and new ones are not produced in sufficient quantities.
Thyroid disorders
Pathologies in which too much hormones T3 and T4 are synthesized. The lifespan of platelets in this case is significantly reduced. Hematopoiesis slows down. This is the reason for the deficiency of red PLT plates.
Pathology is treated under the supervision of an endocrinologist. The task is not quick, it takes several months. Iodine preparations are prescribed, as well as a diet low in this element.
Radiation sickness
As such, it inhibits the normal functioning of the bone marrow. This just ends with insufficiently rapid platelet maturation.
Attention:
The same is possible with a systematic, but weak influence of radiation. For example, when performing X-rays, CT scans too often.
PLT: what is it?
The number of platelets per unit volume of blood is designated PLT or Platelets, which is translated into Russian as plate. And not without reason, because these shaped elements have the appearance of a flat, rounded plate, devoid of a core, with several outgrowths.
The lifespan of a platelet is 10 days, after which the element is destroyed in the liver and spleen
These cells are synthesized in the red bone marrow. They are responsible for:
- blood clotting and, consequently, stopping bleeding and restoration of damaged tissue areas;
- blood purification due to the removal from the bloodstream of immune complexes (killed particles of viruses and other antigens associated with antibodies) produced during inflammatory processes;
- nutrition of blood vessels, transportation of a number of biologically active substances.
Therefore, any deviations in platelet levels from the norm are a sign of disturbances in the functioning of the body.
The role of platelets in the human body:
Additional examinations
Ancillary measures are aimed at establishing the origin of the pathology.
Among the techniques:
- Oral interview with the patient.
- Anamnesis collection.
- Ultrasound of the digestive tract.
- MRI as needed.
- Blood and urine tests: general, biochemical. For hormones.
- Coagulogram.
This is a basic diagnostic checklist. Based on its results, specialized examinations are prescribed at the discretion of the doctor.
Blood test for platelets and how to prepare for it
To test for PLT, blood is taken from a finger, or less commonly from a vein. Blood must be donated in the morning, on an empty stomach, at least eight hours after the last meal. Before taking blood, you can only drink water.
It should be taken into account that the number of platelets increases with stress, pain, smoking, and physical activity. This means that on the eve of donating blood, you need to stop smoking, drinking alcohol, exercising, and stop taking certain medications - this will avoid distorting the results.
Treatment
Regarding symptomatic correction:
With elevated platelets
It is necessary to eliminate the primary cause of the pathological process. These are the diseases that were described earlier. There is no need to fight the platelets themselves. The task is to remove the primary factor. It is better to address this question to a specialized specialist.
Symptomatic correction is to prevent the formation of blood clots. Anticoagulants or antiplatelet agents are prescribed.
At low
The same. Etiotropic treatment is necessary. Fighting the primary cause.
Diseases due to deviations from the norm
An increase in platelets above the permissible norm is thrombocytosis. It entails the risk of blood clots and, as a consequence:
- stroke;
- heart attack;
- blood flow disturbance.
A decrease in indicators is characteristic of a disease called thrombocytopenia. It is accompanied by fragility of the vascular walls, impaired blood clotting, which, in turn, causes bleeding. This does not exclude the presence of infectious diseases, anemia, and leukemia in the body.
Both pathologies pose a real threat to the health and life of the patient.
Trying to understand the research results on your own will not be successful. Deciphering the tests is the prerogative of a specialist, since only a qualified doctor can determine the cause of deviations from the norm by assessing the clinical picture and other indicators of a general blood test.
Prevention
Preventive measures are extremely simple. It is enough to follow simple recommendations:
- Regularly undergo inspections. Every six months or a little less often.
- Eat well. To prevent the development of anemia and deficiency diseases.
- Treat pathologies of any profile in a timely manner. Even an old source of infection can present an unpleasant surprise.
- Eliminate alcohol from your life.
- Do not self-medicate.
PLT stands for platelet, which means platelets in English. The indicator is informative, but it needs to be clarified by other methods. This way you can quickly detect health problems.
Deciphering a general blood test: what are platelets - video
Thus, PLT is an important indicator of a person's health status. Deviation from the norm may indicate the development of diseases, the treatment of which is carried out by diametrically opposed methods. Therefore, you should not self-medicate. Only a doctor can determine the exact cause by analyzing the remaining results of the OAC and the present symptoms.
- Author: Maria Voronina
A copywriter with an active lifestyle. I specialize in writing articles on medical topics. Rate this article:
- 5
- 4
- 3
- 2
- 1
(13 votes, average: 4.6 out of 5)
Share with your friends!
Classification
It is not entirely correct to talk about the typification of microcytosis as such. A generally accepted method has not yet been developed, and it would not have sufficient information content.
The division is carried out on such a basis as the features of the provoked changes in general. Accordingly, we can talk about the following types of pathological process.
Iron-deficiency anemia
Classic disorder. It is typically caused by insufficient iron intake or weak, poor absorption as a result of disorders of the digestive system or other reasons.
The question is secondary in the context of the situation. The point is different. Due to an insufficient amount of iron, the concentration of hemoglobin drops, therefore, the normal synthesis and maturation of red blood cells is disrupted. As the previous sizes are no longer needed, they are reduced in volume in order to save money.
Only after eliminating the disorder does everything return to normal. Read more about IDA and its treatment methods in this article.
Thalessemia
A genetically determined type of pathological process. The result of the disorder is a dual symptomatic complex. Both manifestations are equally dangerous to health and life.
- The first characteristic sign is a natural (in the context of a clinical case) drop in hemoglobin production. The result is a problem with cellular respiration. There are several types of thalesemia, they are determined precisely by the degree of deviation and the severity of the disorder.
- The second typical symptom concerns the synthesis of red blood cells. They decrease in size (microcytes), and in addition, as a result of an abnormal reaction of the body, they begin to die in large volumes. Which also leads to a reduction in quantity.
The pathological process has many variations. Not everyone is so dangerous. Sometimes the patient does not even suspect that he has any health problem.
Attention:
There are also situations that lead to stillbirth or early death of children. In the very first days from birth. This is a hereditary or mutational abnormality.
Hypochromic anemia
Accompanied by a violation of the size of formed blood cells. On the other hand, there is an insufficient concentration of hemoglobin in their structure.
Cytological units are not able to transport oxygen, which leads to ischemia, hypoxia and unpredictable consequences in the long run. It is necessary to begin treatment as quickly as possible.
Read more about hypochromic anemia in this article.
There is also the opposite phenomenon. When red blood cells are smaller than normal in size but contain an abnormally large amount of hemoglobin. It carries no payload, typically. Because they still cannot tolerate it normally.
There are rarely exceptions. The origin of both this and that state is always secondary. That is, it is caused by other violations. To eliminate anemia, you need to deal with the source of the problem.
Hypochromia and microcytosis are the most common ligaments and are as widespread as the pathology associated with iron deficiency. Special diagnostics help to put an end to the issue of nature.