APTT is part of an extended coagulation test, a test designed to examine the speed and quality of blood clotting. The abbreviation can be deciphered as activated partial thromboplastin time.
The study is prescribed to patients regardless of health status, as a diagnostic or preventive measure. Any deviations are clearly interpreted as pathology. Bleeding disorders cannot be natural, they are an anomaly. Apart from a couple of cases. If the indicators are changed, diagnosis and treatment are the prerogative of the hematologist.
A course of therapy is prescribed at the discretion of the specialist. Using the same method, the doctor checks the quality of the correction. When necessary, it changes the recovery scheme taking into account the dynamics. If the pathology does not have a genetic basis, the prognosis is favorable.
The essence of the analysis and what the research shows
APTT (also APTT) is an auxiliary method of an extended coagulogram. They always study it. From the patient's point of view, there are no differences from a standard blood test. After the laboratory technician has collected the biomaterial, it is sent to a specialist.
How to work with a sample:
- The blood is divided into fractions. Doctors are interested in the liquid part, that is, plasma. She is low on platelets, which is exactly what she needs. Otherwise, the formed cells will disrupt the overall picture and affect the results. The main component remains in place: these are special proteins, fibrinogen and coagulation factors.
- Next, special chemical reagents are added to the clean sample. Calcium chloride, koalin and cephalin. This is a kind of provocative test that shows how efficient the clotting factors are. Ultimately, the sample should coagulate.
- APTT is calculated in seconds. Accordingly, when the blood completely changes compared to the initial state, then we can talk about the end of the analysis. The period from the introduction of reagents to the coagulation of liquid tissue is called APTT.
- Deciphering does not present any great difficulties if the reference values and counting methods are known. An increase in APTT means hypocoagulation: the time increases, the blood clots more slowly. It's liquid. A decrease in the indicator is hypercoagulation. The fabric reacts too quickly. It's thick. In the future, this condition almost guarantees thrombosis.
This study is rarely carried out in isolation. It's informative, but there are a few problems:
- As such, the indicator does not diagnose external coagulation disorders. That is, nothing is known about the work of platelets, their adhesion and aggregation. This is where the problem may lie.
- On the other hand, there are major differences in the methods that laboratories use. Therefore, there is no single normal meaning. This imposes certain requirements on the work of the doctor and the laboratory itself.
Specialists must indicate the ways in which they examine biomaterial. It doesn’t hurt for a hematologist to familiarize himself with the technology. Requires in-depth knowledge in diagnostics.
Basically, APTT is carried out in parallel with the study of prothrombin time.
What can distort the result
The common unit of measurement for the test is the clotting time in seconds.
In Russia, the standard range of values is considered
Reference values of the Invitro laboratory Invitro values are somewhat different from the standard ones, since the more modern equipment of this laboratory allows measurements to be taken with greater accuracy.
- Norm for APTT: 25.4-36.9 sec1
An increase in APTT time indicates a risk of bleeding, and a shortening indicates a risk of thrombus formation.
Influencing factors (reasons for incorrect results)
- Discrepancy between the volume of anticoagulant and the volume of plasma red blood cells;
- Insufficient filling of the vacuum tube with biomaterial (increases the indicator);
- Contamination of the patient's plasma with heparin (increases the rate);
- Violation of the rules of preparation for venipuncture, the process of blood sampling and storage of a biomaterial sample;
- The entry of tissue thromboplastin into the patient’s blood sample as a result of injury during venipuncture (reduces the indicator);
- Increased levels of lipids in the blood (may be associated with the patient’s diet);
- Therapy with very high doses of anticoagulants reduces the sensitivity of the activated partial thromboplastin time assay.
Important! The interpretation of the results is always carried out comprehensively. It is impossible to make an accurate diagnosis based on only one analysis.
Preparation and delivery of analysis
Before the procedure, you should follow simple recommendations.
- 5 hours before the test you need to refuse food. On an empty stomach, the results will be more accurate and the likelihood of errors will be much lower. This happens due to the dynamics in the bloodstream.
After a heavy meal, the liquid connective tissue thickens. This affects both prothrombin time and APTT. True, we are talking about short-term changes. But this is enough to distort the results.
- Under no circumstances should you smoke. How much? In about 3-5 hours. Nicotine is indeed harmful, but the main danger is caused by other substances. When tobacco and dye are burned, a lot of things are released: cadmium, arsenic, volatile carbon compounds, such as methane.
They enter the blood through the pulmonary system and inhibit the production of coagulation factors. And if the experience is long, then on the contrary - the liquid tissue quickly thickens, blood clots form. Smokers with “experience” would do well to abstain from cigarettes longer. 2-3 days. Because the body later returns to normal.
- You can't overexert yourself physically. Mechanical stress causes hypercoagulation. There are many clotting factors produced. And besides, during sports or exhausting work, a person loses water. The useful volume of liquid connective tissue decreases, but the amount of coagulation factors does not disappear.
It turns out that a smaller volume of blood in proportion is affected by more specific substances. This will definitely affect the analysis. There will be a serious deviation.
Of course, the body will quickly return to normal. But the study turns out to be false, and you will have to take the test again. The regimen needs to be adjusted 8-12 hours before the procedure.
- Stress is also excluded. Mental stress is no less dangerous. The fact is that after nervous tension, the adrenal glands begin to work actively. They synthesize cortisol, adrenaline, and trigger the release of norepinephrine.
These substances change the rheological properties of blood. The fabric becomes too thick. Coping with stress is much more difficult than giving up physical activity. It is enough to calm down an hour or two before the analysis.
You can take a herbal sedative tablet. For example, Valerian or Motherwort. But not alcohol tincture. Ethanol excites the nervous system, provokes blood thickening, the effect will be the opposite.
The patient will not notice any particular difference between a coagulogram, aPTT study and a simple CBC. All the same.
Biomaterial is taken from a finger or from a vein. This depends on the practice adopted in the particular laboratory. Then the tube is labeled and sent further.
Some centers assess clotting rates on site. But in the case of APTT in a coagulogram, this is quite difficult. Because it is necessary to purify the blood, isolate the liquid fraction and provoke a chemical reaction.
Typically, the patient receives results within 2-3 days.
Mechanism for performing APTT analysis
The test is based on the availability of reagents and the patient’s blood. Executing the test itself is simple:
1. 5-10 ml of blood is taken from a patient’s vein using a syringe.
2. The blood is poured into a test tube with sodium citrate, which binds calcium ions. The absence of calcium ions contributes to blood incoagulability and preparation of the sample for the test itself.
3. The blood is sent for centrifugation, resulting in plasma, which contains a small number of platelets.
4. To activate the mechanism of internal blood coagulation, kaolin or another reagent is added to the resulting plasma.
5. Next, a phospholipid, for example, cephalin, is added.
6. Add calcium chloride solution to enrich the blood with calcium ions and neutralize the effect of sodium citrate.
7. After carrying out all the manipulations, we note the time of formation of a blood clot.
Normal values
The question of what indicators can be called adequate is quite complex. Because clinics use different counting methods. Even doctors are confused. When deciphering, they take into account the research technique that the laboratory uses.
In adults and children
The normal APTT in adults is within 25-35 seconds. Then everything depends on the specific medical center.
Deviations up or down by 1-2 seconds are possible. In women, the cause is most often due to altered hormonal levels. Deviations depend on the menstrual cycle and its phase.
Anything that goes beyond this permissible error almost completely indicates pathology. You need to understand it in detail.
There is also no significant difference in APTT rates in children. The rate of coagulation with chemical provocation will be approximately the same. All other rules, such as deviations and the need for further diagnostics, are also valid.
During pregnancy
Gestation is a serious test for the circulatory system. Changes begin in the second trimester. At first, as a rule, there are no deviations. Approximate APTT values can be presented as follows:
| Trimester | APTT rate in seconds |
| I | 25-35 |
| II | 30-33 |
| III | 31-36 |
An increase in the indicator indicates that the blood is clotting more slowly than expected. It's too runny.
During gestation, other tissue properties and laboratory levels also change. Including fibrin, platelet concentration. This is fine.
However, too strong changes in the coagulogram, even if there is no connection with pathologies, do not bode well. Need treatment.
Attention:
When the APTT is at the border of 35-36, and even more so moves beyond these limits, the expectant mother needs to be helped. Because with natural resolution of childbirth, there is a high probability of fatal uterine bleeding.
Of course, hematologists are limited in their choice of drugs. Pregnant women should not take many medications. The problem is solved by a group of specialists.
APTT test during pregnancy
A hematologist and gynecologist can prescribe this test as part of a coagulogram if the expectant mother has a tendency to thrombosis or bleeding.
Pregnancy complications can occur due to natural processes:
- hormonal changes;
- the formation of the third circle of blood circulation (uteroplacental), which delivers oxygen and nutrients to the embryo;
- changes in the hemostatic system before and after childbirth.
Important! In pregnant women, the level of another coagulogram indicator, fibrinogen, increases, which reaches 6 g per 1 liter maximum (2 g more than normal).
At the same time, the APTT begins to decrease and reaches a normal value of 17-20 seconds.
When the thromboplastin time is shortened relative to the specified norm, the risk of developing thrombosis increases (the blood thickens). Thrombosis can affect the vessels of the placenta and cause its premature detachment. Also, APTT does not significantly deviate from the norm while taking iron supplements (prescribed to the expectant mother with low hemoglobin).
Prolongation of APTT in pregnant women (blood thins) can cause uterine bleeding, which threatens the life of the expectant mother and child.
Also, blood clotting disorders during pregnancy increase the risk of developing disseminated intravascular coagulation syndrome. In the 1st phase, blood clots are actively formed, and in the 2nd and 3rd phases the blood practically does not clot, which can cause severe blood loss.
To prevent the development of complications, it is necessary to do a coagulogram with APTT determination every trimester.
Unscheduled tests are prescribed for pregnant women in the following cases:
- presence of coagulation pathologies in the family history;
- liver dysfunction;
- diseases of the cardiovascular system;
- hypertonicity of the uterus (threat of miscarriage);
- hypertonic disease;
- proteinuria (presence of protein in urine);
- increased tissue swelling;
- gestosis (complication of toxicosis of the 3rd trimester).
APTT is higher - the norm, what does this mean and what are the reasons?
Provocateurs are always pathological. There are no natural factors here. Moreover, when the indicator is persistently increased over a long period of time. If we talk about specific points:
Hereditary and genetically determined disorders
For example, Hageman's disease. With it, the human body does not have enough coagulation factor XII. There are other options as well.
Regardless of the specific diagnosis, the essence is approximately the same. The quality and speed of coagulation decrease. In the most difficult cases, protein is not produced at all.
The reasons are inherited defective material from parents. It is difficult to effectively deal with such problems. We have to introduce the necessary substances artificially, from the outside. But it is impossible to radically help, because the problem is encoded in the foundation of the body.
Oncology
Especially malignant, neglected. When the tumor begins to disintegrate. The place where the neoplasia is located does not play a big role. What is more important is how quickly cells divide.
With rapid proliferation, they consume such an amount of nutrients that they die from “gluttony.” Other cancer cells don't have enough food. They die from hunger and lack of useful compounds.
In both cases, a huge amount of dead cytological structures enters the blood. They break down, leaving behind toxins. These toxic substances inhibit the synthesis of coagulation factors. Therefore, dangerous complications cannot be avoided.
Usually, by the time the tumor begins to disintegrate, the body is already exhausted. The bone marrow is working at its limit. The general asthenic condition of the patient makes the situation even worse.
Systemic autoimmune diseases
For example, lupus erythematosus. The reason for the increase in APTT is insufficient production of coagulation factors, a massive failure of all body systems. Without treatment, the pathology quickly leads to disability and then death. Coagulation disorders are part of a huge pathological picture.
Hepatitis
Liver inflammation of various origins. Most often, infectious, viral. Patients who abuse alcohol are also at risk.
Also those who receive extensive treatment for inflammation, cancer, etc. Since it is in the liver that the body synthesizes most of the coagulation factors, even the slightest deviations immediately affect the properties of the blood.
Cirrhosis of the liver
A much more dangerous condition. Another name is hepatonecrosis. That is, the death of organ cells. In a chronic course, the degree of impairment increases gradually, intensifying as the disease progresses.
Acute variants end in rapid breakdown. As a rule, there is no need to carry out analysis. Everything is obvious.
Hemophilia
A group of diseases of the circulatory system. In hemophilia, insufficient clotting factors are produced, and the aPTT increases. For what reason - you need to find out in each case separately.
Attention:
Genetically determined forms of the disease almost always occur.
Hormonal imbalances
Excessive activity of the thyroid gland, or problems with the pituitary gland as the basis for such deviations. The aPTT is elevated until the levels of specific substances return to normal.
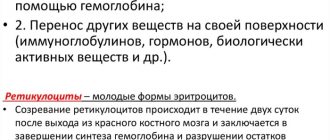
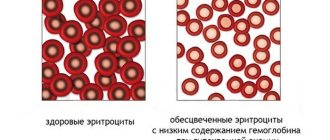
Problems occur with iron deficiency anemia.
There is perhaps one exception. The same effect develops if the patient takes anticoagulants. For example, heparin or other drugs. Strictly speaking, this is not a disease or pathology. More like a side effect of the medication.
As soon as the medication is discontinued, the blood condition is gradually restored. Although in some cases the coagulation rate does not return to normal on its own.
Especially if heparin was used for a long time or in large dosages. In this case, special assistance will be required. Hemostatic drugs are prescribed, and other methods are possible.
If the APTT level is higher than normal, it means the blood is too thin. Diagnosis is carried out by a hematologist. Treatment is etiotropic. Its task is to eliminate the factor provoking this disorder.
High aPTT rate
The time for blood clots to form during pregnancy is shortened
A high APTT means that clotting is taking longer than necessary. This condition in the mechanism of internal coagulation provokes hemorrhages in the internal organs, muscles and joints. Any injury, surgery, even a trip to the dentist can lead to irreparable consequences. The indicator is considered elevated when the clot formation time exceeds 40 seconds.
High levels pose a particular danger to pregnant women. The body of a woman carrying a child is preparing for the upcoming birth, so the process of blood clotting is significantly reduced over time. Normal aPTT values during pregnancy are 14-19 seconds. Thus, critical blood loss during delivery is eliminated. However, a low APTT is associated with a risk of blood clots, so clotting time is a very important indicator that should be carefully monitored.
Causes
The cause of prolonged aPTT is hemophilia
Most often, the reasons for prolonged clotting time lie in a decrease in the factors due to which this process is carried out. Main reasons:
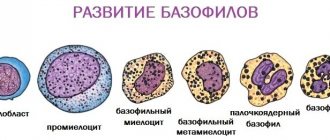
- Hemophilia A provokes a deficiency of antihemophilic β-globulin (clotting factor VIII);
- Hemophilia B causes α-globulin (factor IX) deficiency;
- Hemophilia C is accompanied by a lack of γ-globulin, a precursor of thromboplastin (factor XI);
- Lack of factors II, VII, IX and X due to vitamin K deficiency, since these factors are K-dependent;
- Damage to the liver, in which K-dependent coagulation factors are synthesized;
- Chronic diffuse glomerulonephritis is accompanied by excessive production of endogenous heparin, which inactivates factors II, IX, X, XI, XII;
- Taking anticoagulants (Warfarin, Heparin, vitamin K antagonists);
- Taking fibrinolytic drugs (Fibrinolysin, Stereptokinase);
- Neoplasms and sepsis provoke the formation of antibodies to factors V, VIII, IX.
Treatment
Treatment of elevated aPTT with vitamin K
Treatment is prescribed after identifying the cause of the increased APTT. Some forms of the disease (hemophilia A, B, C) are hereditary incurable pathologies for which maintenance therapy is carried out.
Lack of vitamin K is a common cause, as there are many factors that cause its deficiency. Insufficient formation of vitamin K in the intestines can be caused by antibiotics that cause dysbiosis. The use of vitamin K antagonists for thrombosis can lead to acute vitamin deficiency and an increased risk of bleeding. Blockage of the bile duct also leads to insufficient absorption of the vitamin. Thus, it is necessary to eliminate the root cause of low vitamin K levels; if improvement does not occur, the patient is prescribed Phytomenadione, Vikasol and a special diet.
Treatment of chronic glomerulonephritis includes anti-inflammatory drugs, hormonal agents, and diuretics. A mandatory element of therapy is a diet with limited protein, salt and liquid. Pathologies of the liver tissue can be caused by viral infections, in which case antiviral drugs and hepaprotectors are prescribed. Liver damage is often provoked by heavy alcohol consumption, so it must be eliminated first and then treatment aimed at restoring liver cells. Nutrition plays a key role in therapy.
Life forecast
Patients with congenital disorders should be seen by a physician
An increased APTT level caused by acquired factors can be corrected if detected in a timely manner. Treatment should only be carried out under the supervision of a specialist, as the clotting time should return to normal without reaching a reduced level at which there is a high risk of blood clots.
Inherited causes of high APTT, namely various types of hemophilia, are controlled by injections of a clotting factor that is lacking in the circulatory system. Today, therapeutic support for patients with hemophilia allows them to live a full life, in contrast to previous centuries, when patients, suffering from bleeding, died at a young age.
Modern medicine is constantly searching for new means to compensate for clotting factors. For example, in the UK, a drug based on gene therapy was successfully tested for the treatment of patients with hemophilia A. Patients forced to receive injections every 2 days now only need one injection to produce factor VIII. The product is based on a genetically modified DNA molecule, which carries the information of the necessary factor. The drug is under large-scale testing.
Prevention
The dosage of the drug is determined by a specialist
Preventive measures include avoiding drug overdose, timely treatment of diseases and periodic monitoring of the aPTT level. It is recommended to pay special attention to aPTT indicators at the stage of planning a child and during pregnancy.
Patients with hemophilia need to monitor not only the aPTT level, but also the possible formation of antibodies that destroy the clotting factors injected. Antibodies can form at any time, so tests must be taken regularly. Planning a pregnancy requires mandatory consultation with a geneticist and a full examination.
Reasons for the decline
When the level drops, the blood becomes thick. It is highly likely that the body produces a lot of specific proteins.
Why is this happening:
- DIC syndrome at the first stage. A condition in which liquid connective tissue begins to randomly coagulate directly in the vessels. The pathology is hereditary or secondary, caused by hormonal disorders. There are exceptions.
Hypercoagulation, and therefore low aPTT, is typical only at the very beginning of the disease. Then the disorder turns 180 degrees, everything becomes the other way around.
- Thrombosis.
- Thromboembolism. In both cases, the drop in the indicator is the result of a secondary pathological process. And sometimes there is no connection at all.
There are also natural factors. Although some of them can be called that very conditionally.
- Exercise stress. Why this happens has already been said earlier. Intense release of hormones, loss of water. The amount of functional blood volume decreases, and cortisol and other steroids accelerate the synthesis of coagulation factors. The result is hypercoagulation. But this is a temporary phenomenon. A healthy body solves the problem itself and quickly brings the system back to normal.
- Errors in nutrition. Substances such as caffeine and tannin have a negative effect on the condition of the blood and blood vessels. They are found in popular drinks. However, as in the previous case, this is not dangerous. At least for healthy people.
- Stressful situations. They provoke an active release of cortisol and adrenaline. It is impossible to completely get rid of nervous tension, because the body. Sometimes symptoms persist for years. It all depends on adaptive abilities.
- Smoking. Patients with considerable experience are especially at risk. The body adapts to the negative factor, but it only seems so. In fact, a person simply stops noticing problems.
- Alcohol is no less aggressive. Ethanol causes hypercoagulation and thickens the blood. The process is complex. When the patient drinks regularly, the disorder becomes persistent. Doesn't go away on its own.
If the aPTT is low, this means that the blood is too thick and this situation is ideal ground for thrombosis. Without treatment, everything can end in disaster.
Low – short time, high – extended
A low (or decreased) level of activated partial thromboplastin time (shortened clotting time and clot formation) indicates that the patient's blood is clotting too quickly (hypercoagulable).
Signs of hypercoagulation can be observed in pathological processes that form as a result of increased blood clot formation:
- Stage I (and only the first!) of disseminated intravascular coagulation (DIC syndrome);
- Thromboembolism of various locations (heart, lungs, spinal cord and brain, kidney, etc.), thrombosis (the lower extremities most often suffer; during pregnancy, thrombosis of the placental vessels, which leads to its detachment, threatening intrauterine fetal death).
However, a low APTT result can manifest itself not only due to the patient’s illness. Other factors may be to blame, which are sometimes quite difficult to avoid, for example, tissue thromboplastin getting into the sample when tissue is injured at the time of venipuncture, so there is no need to “torment” the vein too much if it is not possible to take a blood test right away.
A high level (extended clot formation time) of activated partial thromboplastin time is observed in conditions that disrupt the biosynthesis of factors and other pathological processes affecting the functioning of the hemostatic system. These include:
- Hemophilia of all types: A (antihemophilic globulin deficiency - FVIII), B (Christmas factor deficiency - IX), C - factor XI deficiency);
- The presence of factors inhibiting coagulation processes (inhibitory hemophilia);
- Hageman disease (defect) (factor XII deficiency);
- von Willebrand's disease;
- Stages II and III of DIC syndrome;
- Treatment with high molecular weight heparins;
- Serious damage to the liver parenchyma;
- APS (antiphospholipid syndrome).
Similar to a low APTT value, when technical errors intervene, a high activated partial thromboplastin time result can be obtained. This occurs if the volume of anticoagulant in the tube does not correspond to a high hematocrit value or an insufficient amount of blood is taken into the vacutainer (a special disposable vacuum tube).
How to increase APTT
To increase APTT, the following techniques are used:
Anticoagulant therapy:
- heparin medications, Pradaxa, Clexane;
Pradaxa
Clexane
- taking medications of the fibrinogen group - Warfarin;
Warfarin
- taking antiplatelet agents - medications based on acetylsalicylic acid to thin the blood - Aspecard and Aspirin.
Aspecard
Aspirin
A therapeutic anti-cholesterol diet is also recommended for the patient. Cholesterol plaques impede blood flow, and its slowdown, in turn, leads to increased coagulation and a decrease in aPTT. Vitamin-mineral complexes containing vitamins E, C, A and omega3 will also be useful.
Where can I get tested and how much does it cost?
If reagents and necessary equipment are available, any laboratory - private or public - can perform such a study. The cost of manipulation depends on what indicators need to be studied, what methodology and equipment is used for this.
Speaking on average, a regular coagulogram costs from 700 to 1300 rubles. To conduct an extended analysis, the patient will have to pay about 3,500 rubles. Although it is worth considering that such an analysis is mandatory for pregnant women, so for them it is usually free, just like under the compulsory medical insurance system.
How to lower APTT
To reduce aPTT it is recommended:
- coagulant therapy - Tranexam, Dicynon;
Tranexam
Dicynone
- vitamin therapy with vitamin K - Vikasol injections;
Vikasol
- treatment of underlying diseases;
- blood transfusion with an increased coagulation index.
A diet high in animal proteins will be beneficial. It is recommended to eat more lard, butter, fatty cottage cheese and sour cream, fatty cheeses and fish, eggs, red meat, red vegetables and fruits, legumes, and herbs.
What affects blood clotting
Emotional stress affects blood clotting
Normal blood clotting varies greatly throughout life. Factors that may influence it include:
- Hormonal background - in women, blood clotting depends on the phase of the menstrual cycle;
- Saturation of the diet with vitamins and macroelements (vitamin K, calcium);
- Intestinal health - vitamin K is produced in large quantities by the normal microflora of the colon;
- Psycho-emotional state - under stress, blood clotting increases significantly, as the body prepares for possible blood loss;
- Physical activity – excessive fatigue causes the same changes in the body as severe emotional stress.
Blood clotting is an important indicator for health, which only the doctor treating the patient can correctly assess.
How to prepare for research
APTT is usually determined as part of a biochemical blood test. Therefore, the general training requirements are the same. The norm for women by age is indicated on the same form as the obtained values.
In order to obtain correct results, the following rules must be observed:
- biological material is taken in the morning, on an empty stomach;
- before the test, the last meal is 8-14 hours;
- the day before it is necessary to avoid emotional and physical stress;
- you need to stop smoking 1-2 hours before;
- Drinking alcohol is prohibited 2-3 days before.
If the patient is taking anticoagulant drugs, she must notify the doctor in advance, since the aPTT values are significantly distorted. In agreement with the doctor, they are excluded in a few days.
Indications for analysis
Referrals for analysis are issued by doctors of various specialties. Information about the state of hemostasis (blood coagulation system) when making a diagnosis and for treatment is necessary for such specialists as a hematologist, resuscitator-anesthesiologist, surgeon, cardiologist, gynecologist, reproductive specialist, and therapist.
The APTT test is indicated in the following cases:
- frequent bleeding and hemorrhages of unknown origin;
- suspicion of congenital or acquired diseases of the blood coagulation system, the presence of a hereditary predisposition to the formation of blood clots;
- acute myocardial infarction;
- DIC syndrome;
- hypofibrinogenemia (low levels of fibrinogen in the blood);
- pregnancy;
- infertility;
- miscarriage;
- thrombosis in arteries and veins;
- systemic lupus erythematosus;
- antiphospholipid syndrome;
- hemophilia (deficiency of factors and weak ability of blood to form a blood clot when a vessel is damaged);
- laboratory monitoring during treatment with drugs that inhibit the coagulation process (Heparin, Hirudin);
- high level of lupus anticoagulant in the blood (formed during autoimmune pathology and in the body increases the risk of blood clots);
- stroke;
- Varicose veins;
- thrombophlebitis;
- pulmonary embolism.