Last time, the famous doctor Alexander Myasnikov spoke about the risk factors for intestinal cancer, as well as preventive measures that should be taken against this intestinal disease. Today - about the symptoms of cancer, which doctors do not always pay attention to, and in detail about the main study in the diagnosis of intestinal cancer - colonoscopy.
Doctors' recommendations for conducting preventive bowel examinations
In addition to diseases of the digestive tract, there is a danger of cancer. Colon cancer is the third most common cancer. Polyps that can grow in the organ cavity are considered potentially malignant. They are more often found in older patients, less often in women than in men. Based on these facts, colonoscopy for cancer prevention is indicated for everyone over 50 years of age. If no polyps or other diseases were found during diagnosis, then they will be further examined after 10 years.
If among close relatives there were cases of oncology or polyps of the gastrointestinal tract, intestines in particular, then such a patient is recommended to have a colonoscopy at the age of 40 and then every 5 years, when nothing was found at the first. Moreover, the age at which the formations were found and the degree of relationship are important. The risks are higher if such a case is recorded in brothers and sisters, father and mother under 60 years of age.
Doctors also recommend undergoing a colonoscopy at any age with a weakened immune system, digestive problems, chronic fatigue, anemia, and other symptoms of poor general health. Even poor skin and hair condition can signal problems in the intestines.
Attention! In order not to be tormented by doubts about the correctness of the results, you need to decide where to have a colonoscopy. Much depends on the capabilities of the equipment, and even more on the experience of the endoscopist.
Survey process
The examination consists of assessing the internal state of the final part of the digestive tract and large intestine. For more comfortable tolerance, local anesthetics are used or general anesthesia is injected.
Diet before colonoscopy
An endoscope (a long flexible tube) equipped with a video camera is inserted into the anus and slowly advanced down the rectum. During the process, air is supplied to expand the intestines.
The time range of the procedure is from 15 minutes to half an hour. If you experience discomfort after the procedure, you should take a sorbent agent and follow your previous diet for 2-3 days. Based on the results of the study, the patient is diagnosed and appropriate therapy is prescribed. Complications after the procedure are a tiny percentage. The most severe may be perforation (through disruption) of the intestinal wall.
Other undesirable consequences may include:
- excessively increased gas formation;
- pain in the anus;
- loose stool.
These symptoms are usually self-limited by the patient. If this cannot be done, you must seek medical help.
It is not the diagnostician who deciphers the results of the study, but the treating specialist.
Repeated examinations after polyp removal
Unfortunately, even with the modern capabilities of medical equipment, as a result of eliminating the formation, there remains the risk of re-growth of a new one in the same or another place. Therefore, after such a minor surgical operation, it is recommended to do a colonoscopy to make sure that there is no recurrence of the pathology. Depending on the type of polyp, they offer different time frames until the following diagnosis:
- Fibrous, inflammatory, hyperplastic and juvenile have a very low risk of malignancy, so after their discovery the patient is checked every 5 or even 10 years.
- Based on the removal of single (up to 2 pieces) adenomatous formations up to 1 cm in size, the next colonoscopy is recommended for the 6th year.
- Villous polyps, multiple up to 10 pieces or larger than 10 mm with a tubular structure, recur more often. Therefore, diagnostics are prescribed every 3 years.
- When removing various adenomas, “sessile” ones are especially dangerous, the risk of malignancy is very high. It is believed that cancer can be hidden in formations from 2-2.5 cm. Histology will reveal the presence of atypical cells, dysplasia and other potentially dangerous processes. After eliminating the adenoma, the patient is checked after 2-4 months, and the frequency of further examinations is determined by the attending physician.
Despite established recommendations, experts advise performing a colonoscopy in the first year after removal of polyps in the large intestine, since the causes of the appearance are not fully understood, but relapse is observed more often after 4-6 months from the removal of the predecessor.
Attention! After a colonoscopy under anesthesia, recovery is required not only from the procedure, but also from sedation drugs, which are often not recommended.
How can one suspect that there are already polyps in the intestines?
The appearance of a growth on the wall of the organ does not give any symptoms. However, over time, as the formation increases in size, it is damaged by passing feces and intestinal contractions. As a result, blood appears in the feces. It cannot always be detected visually, only with the help of a test or laboratory study. If the polyp is localized in the colon or higher, then the blood coagulates and becomes brown or black; if the growth is in the rectum, it is scarlet. Moreover, the formation can be located in the stomach, so sometimes a colonoscopy is done together with an FGDS at the same time.
Large formations of adenomatous, glandular or mixed type produce mucus, which can be seen in the stool. Causeless anemia is also considered an indirect sign, but this only indicates that there is bleeding in the body. Polyps are accidentally found during MRI of the abdominal cavity, CT scan, ultrasound, but already larger than 10 mm in size.
Attention! A video of how a colonoscopy is done can save you from having to repeat the examination. Sometimes you just need to show the disk to another specialist to study the results in detail in order to discover what was missed earlier.
Who should use this examination method?
Colonoscopy is sometimes irreplaceable
Colonoscopy is not necessary for all patients if they wish or if they experience minor gastrointestinal discomfort. For all invasive procedures there is a clearly limited range of indications.
It is primarily necessary to examine patients who present certain complaints and whose physical examination data alerts the doctor to the possible presence of cancer.
What situations can be included here?
- The appearance of blood on the surface of the stool in the absence of signs of anal fissure or hemorrhoids during digital rectal examination and rectoscopy using special mirrors.
- Severe anemia of iron or B-12 deficiency.
- Positive Gregersen reaction, indicating the presence of occult blood in the stool.
- Persistent melena (tarry black stool) in the absence of erosions, ulcers and cracks when performing fibroesophagogastroduodenoscopy.
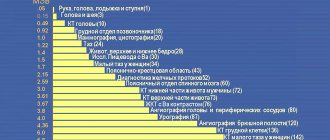
Patients are referred for this procedure after a certain set of preliminary examination methods. You may need fluoroscopy of the esophagus, stomach, assessment of the passage of barium suspension through the intestines, as well as ultrasound examination of the abdominal organs.
Frequency of colonoscopy for chronic intestinal pathologies
Crohn's disease, ischemic and ulcerative colitis, inflammatory processes - everything that affects the mucous membrane cannot be detected by other research methods. Therefore, in case of such problems, it is necessary to periodically perform a colonoscopy in order to assess the dynamics, effectiveness of treatment, etc.
Usually the timing of the diagnosis is determined by the doctor. If significant areas are damaged and the chronic process lasts from 8 years, then colonoscopy is done every 2-3 years. More often if necessary. A contraindication is the period of exacerbation of these diseases, when there is a risk of damage to the wall due to gas stretching or a risk of deterioration of the organ’s condition.
Who is it prescribed to?
The following symptoms are the basis for a colonoscopy:
- Blood in the stool (a typical symptom of hemorrhoids and many other diseases).
- Difficulty defecating – constipation or diarrhea.
- Intoxication of the body (expressed as loss of appetite, general impotence and loss of body weight).
- History of diseases of the rectum and colon.
- Polyps.
The undoubted advantage of the procedure is that it is almost impossible to miss hemorrhoids after a colonoscopy , since thanks to a special lighting device and optics, the device is able to recognize even just emerging nodes.
In addition, if the patient has minor hemorrhoidal bleeding, the colonoscope can immediately begin treating the hemorrhoids by performing cauterization.
The use of a colonoscope is contraindicated:
- In the early postoperative period.
- For acute paraproctitis, proctitis and chronic colitis.
It is also necessary to take into account general contraindications to medical procedures (for example, acute myocardial infarction in a patient, etc.).
The shortest interval between procedures
Doctors believe that 6 months is enough for recovery after cleansing the intestines with drugs, as a result of the removal of polyps, as well as for rehabilitation from the sedation used. After about the same time, it makes sense to check for recurrence of adenomas or evaluate the results of drug treatment for colitis or Crohn's disease.
Repeated colonoscopy is prescribed within a month to six months for acute indications. For example, a tumor was removed, histology confirmed that it was malignant, and an MRI revealed that fragments remained or the tumor had roots in the thickness of the wall.
Sometimes the procedure is prescribed after 1-2 months, if the patient did not prepare the intestines well for the previous examination, which prevented a full examination. Sometimes the procedure is interrupted due to severe pain during colonoscopy without anesthesia, then the diagnosis is repeated using sedation after a couple of months.
Attention! Proper preparation for colonoscopy increases its reliability significantly.
Preparation for the event
A high-quality colonoscopy is impossible without prior preparation of the patient. The walls of the organ must be clean so that the doctor can assess their condition and see the border between healthy and diseased tissue. There are two basic stages of preparation for the procedure.
Slag-free diet
A low-residue diet will help you prepare well for a colonoscopy.
A week before the procedure, you should exclude whole grain products, some fruits and vegetables (bread, grapes, cucumbers, tomatoes) from your diet. 3 days in advance - spinach, lettuce, paprika, mushrooms, onions. Nutrition before a colonoscopy should be easily digestible. Avoid flour, sweets, smoked foods, marinades.
It is better to take the last meal at lunchtime the day before the event. The time of the last drink should be agreed with your doctor.
Colon cleansing (enema, special laxatives)
To ensure a good view of the tissues, the intestines are first cleaned. This can be done with an enema or step-by-step administration of a special drug (Fortrans, Duphalac, etc.). A laxative to cleanse the intestines before surgery is taken not only to prepare the organ, but also to eliminate the slightest chance of triggering an inflammatory process after the intervention.
Advice: before a colonoscopy, you need to tell your doctor about all the medications you are taking and coordinate the intake with him. Often their components negatively affect a person’s condition during and after the procedure and provoke poor tissue examination (in particular, preparations containing iron).
During the procedure, the doctor must offer comfortable and safe conditions, taking into account the presence of concomitant pathologies (for example, hemorrhoids).
Why is intestinal diagnostics often not prescribed?
There are several reasons why it is not advisable to do the examination more often:
- Preparing the intestines with drugs before colonoscopy is a serious stress for the organ mucosa. In response, minor inflammation develops and the beneficial flora is partially washed out. As a result, the patient needs a week to a month of following a special diet to restore the intestines after a colonoscopy.
- Stretching the walls when pumping with gas is dangerous due to the formation of cracks in places where the mucous membrane is atrophied or damaged. With age, such areas become more and more numerous and, in general, the shell becomes thinner and loses elasticity.
- Risks include bleeding and organ perforation, which can be fatal.
- For most intestinal diseases, additional examination can cause an exacerbation of the process.
- The specified dates were chosen for a reason. They are based on many years of statistics from proctologists and the conclusions of scientific research. Therefore, more frequent colonoscopy is simply not necessary.
An experienced endoscopist is not able to harm the intestines. But if you turn to a non-professional, the procedure can end in disaster.
Diagnostic features
Compared to other methods of examining the intestines, colonoscopy has the following advantages:
- Credibility. Making mistakes is almost impossible - the fiber colonoscope is equipped with lighting and optical devices that allow a high-quality visual examination of the intestinal mucosa and assess its condition.
- Less traumatic. Despite the unpleasant sensations when air is supplied, which straightens the intestine and facilitates the advancement of the instrument, there is no injury to the mucous membrane.
- Multifunctionality. During the procedure, minor manipulations are performed for therapeutic purposes to avoid proctological surgery.
Colonoscopy is also performed in emergency cases - if internal bleeding is suspected, intestinal obstruction or the presence of a foreign object in the intestinal lumen
Colonoscopy is recommended for early detection of hemorrhoidal process. An endoscopist can take a biopsy sample - a piece of the intestinal mucosa, which is sent for laboratory testing to confirm or refute the diagnosis.
“The doctor doesn’t prescribe, but I’m not at ease, can I have a colonoscopy?”
If the patient is bothered by abdominal pain, diarrhea and constipation, or bloating, then it is permissible to do an unscheduled examination in a private clinic on your own a few months or a year after diagnosis. Indeed, sometimes such an intuitive approach allows us to identify problems that were not previously found. In addition, constant obsessive thoughts and anxiety can provoke any intestinal pathology, including polyps and cancer. Therefore, doctors say that it is better to undergo a colonoscopy and calm down.
The frequency of examinations depends on the indications, medical history, restrictions, age, general health and many other factors, which only a doctor can adequately assess. If one unscheduled procedure is not yet dangerous, then regular colonoscopies will lead to inflammatory processes, digestive disorders and other unpleasant and dangerous complications.
When is a preventative colonoscopy necessary?
This procedure must be done at least once a year, and even better, an examination every six months is what doctors say, this helps to identify possible intestinal diseases in the early stages of their development. But there is such a thing as preventive colonoscopy; this procedure should be carried out without fail by certain groups of people. For example, if a person has already been diagnosed with polyps once, then he will have to be examined with a colonoscope at least once every six months.
This examination will not cause any harm to health and the intestines, since a fairly long period of time passes between procedures, but the doctor will be able to see the pathology if it manages to develop during this period of time. Also, testing for preventive purposes is recommended for people with Crohn's disease and ulcerative colitis.
Today, many people die from intestinal cancer, since the disease is detected quite late; the thing is that this form of the disease develops slowly and unnoticed by a person. Often, oncology does not manifest itself at all, and symptoms begin to bother the patient already at a late stage of the disease. If the doctor detects this disease at an early stage, he will be able to prescribe effective treatment, especially since the first stages of cancer are remarkably treatable.
Almost six percent of the population can get bowel cancer, but if there is a person in the family who has suffered or has this disease, then the chance of getting cancer increases significantly. For this reason, it is so important to carry out an internal examination of the intestines; the procedure will not harm if done correctly, and also maintain a period of time for intestinal restoration. It is worth understanding that this examination cannot be carried out too often, as this can severely damage the intestines; first, the intestines are affected by the cleansing process, and then damage can be caused by the examination device.
In what cases is endoscopic diagnosis of the intestine indicated?
There are indications for the examination:
- Blood in the stool is obvious or hidden (according to the results of tests or tests).
- Prolonged, persistent diarrhea.
- Constipation.
- A sharp change in diarrhea and constipation.
- Severe bloating with abdominal pain.
- Assessment of dynamics in the treatment of Crohn's disease or other pathologies.
- MRI, CT, and irrigoscopy revealed polyps, or the results of these examinations are questionable, there is no clear picture.
- Iron deficiency anemia that cannot be treated.
- Tendency to tumors and polyps due to a family history.
- The need for a biopsy.
- Age from 50 years.
The risk group includes people who have harmful addictions - alcohol, smoking. And especially those who eat incorrectly, overeat, consume large amounts of flour, spicy, fast food, processed foods, etc.
Why might the colon endoscopy procedure be banned?
The development of health problems varies. It happens that a colonoscopy is contraindicated for a patient. In what cases does this happen and what needs to be done then, it is worth finding out in more detail. Thus, the period of pregnancy is unacceptable for intestinal examination, as are a number of other diagnostic methods. This can cause premature birth. You should also pay attention to Crohn's disease. In case of exacerbation, a copy cannot be performed, as well as in case of heavy bleeding. Indeed, due to the completely flooded space, the camera will not distinguish anything that can be considered normal or an anomaly in the digestive organ.
We must not forget about a number of complications that may develop directly during the procedure or upon its completion. Side effects include:
- pain as a result of the elimination of polyps and erosions;
- manifestation of nausea and vomiting;
- dizziness (consequences of anesthesia);
- in rare situations - intestinal perforation.
The latter case is life-threatening and requires immediate surgical intervention through surgery.
These are the features of the approach to colonoscopy taking into account the age limit. Here is the basic thing you need to know about when you should consider the procedure if a person is worried about the gastrointestinal tract or even if there are no obvious signs of concern.
Contraindications to colonoscopy
In some situations, diagnostics are prohibited temporarily or completely, since the risk to life and health is too high. The examination is prohibited in the following cases:
- Pregnancy;
- Exacerbation of colitis, Crohn's disease or paraproctitis;
- Infectious inflammatory process in the intestines;
- Depressed respiratory and cardiac function;
- Serious abnormalities in blood clotting;
- Anal fissure.
Elderly patients and young children undergo colonoscopy only in a hospital and according to strict indications. Since the wall of the digestive tract in such patients is very thin, there is a risk of perforation.
Attention! There are other ways to check the intestines for diseases, besides colonoscopy, but none of them gives such comprehensive results and functionality.
What should you not do after a colonoscopy?
After a colonoscopy, you cannot immediately leave the hospital - the patient remains under the supervision of medical personnel for several more hours, especially if anesthesia was used during the procedure. If you had local anesthesia, you can leave within an hour.
There are no restrictions on water and food intake, but the patient needs to follow the above nutritional recommendations for about three more weeks. As a rule, stool appears within 2-3 days after manipulation, taking into account that the patient is eating properly. If the diet is poor in fiber, then stool will appear in a few more days.
The appearance of pain in the intestinal area is due to the very nature of the procedure, however, you can take any painkillers only in consultation with your doctor. The same goes for laxatives. If flatulence bothers the patient for more than five days and the prescribed medications do not help, the air is pumped back out with an endoscope.
It is completely prohibited to take iron supplements (ferrumlek, sorbifer, actiferrin and others) and antiplatelet agents (aspirin and others) after colonoscopy because they inhibit the function of platelets, which are necessary for the healing of damaged intestinal mucosa. It is better to temporarily stop taking them after talking with the doctor who prescribed these drugs.
What to take with you?
For a colonoscopy, you need to take a minimum of things, as it takes place quite quickly and does not require much effort.
So don't forget:
- all necessary medical documentation - medical history, results of other tests, previous photographs;
- if there are chronic diseases, then a medical report on them;
- For older people, a recent cardiogram is necessary. And the doctor should warn you about this;
- socks to prevent your feet from getting cold during the session;
- slippers or disposable shoe covers;
- toilet paper or sanitary napkins in case you need to do additional bowel cleansing;
- a sheet, possibly disposable;
- For convenience, you can take a light robe with you.
That's it, you don't need anything else. And then, if you make an appointment at a paid clinic, then a disposable sheet, shoe covers, and toilet paper will be provided to you there.
How painful is the procedure?
Many people are interested in the question, is it painful to do a colonoscopy without anesthesia? No, you can only feel some discomfort during the injection of air into the intestinal flexures or the urge to defecate. You can easily get rid of the latter if you try to breathe deeply and slowly.
But for young children and patients with pathologies of the abdominal cavity or the presence of adhesions, colonoscopy is done under general short-term anesthesia, pain relief is administered intravenously, since diagnosis can be quite painful.
Colonoscopy, unfortunately, has a strong reputation as a procedure that is quite painful, which many patients cannot stand. Don't believe the rumors, this is absolutely not true. The professionalism of the specialist and the modern technical equipment of the device will allow you to experience minimal discomfort, that’s all.
Anesthesia
Local anesthesia - the patient is conscious, drugs based on lidocaine are used - ointments or gels, which are used to lubricate the skin in the anus area and treat the tip of the probe. Sometimes drugs are used for intravenous administration and pain relief.
During sedation, the patient is in a state of medical sleep. Colonoscopy in a dream involves the use of Midazolam or Propofol.
Colonoscopy under general anesthesia completely renders the patient unconscious for some time. It is associated with certain risks, therefore it has contraindications. But for children under 12 years of age, diagnosis is carried out only under general anesthesia, as well as for people with a high pain threshold, mental disorders, etc.
So, breathe freely and go to the procedure calmly. And then you will tell me whether it hurts and how much. But patient reviews today are significantly different from those a few years ago.
Absolute and relative contraindications
An absolute contraindication is the patient's condition in which the implementation of the study threatens his health or life.
Most often it becomes:
- peritonitis;
- perforation of the organ wall;
- intestinal abscess;
- advanced ulcerative colitis;
- significant internal bleeding;
- period of bearing a child;
- heart attack;
- collapse;
- severe angina;
- respiratory failure.
Relative contraindications represent a limitation of opportunities for colonoscopy, as well as conditions in which the study will not give the required results.
Anesthesia is used during the procedure, so you must first do allergy tests. If intolerance to the main drugs for anesthesia is established, the test must be replaced with another one.
It should not be carried out until the end of the rehabilitation period after surgery, a heart attack or stroke due to a possible deterioration in health.
You should not perform a colonoscopy if you have diverticulitis, since the pronounced stretching of the inner surface creates “blind” areas for the video recorder.
In case of a hernia, it is also undesirable to perform the procedure due to difficulties in passing the probe.
Colonoscopy is not necessary for elderly and senile people, as well as frail patients.
Restoration of intestinal microflora after the procedure
If painful sensations in the abdomen, flatulence, and stool disturbances become a manifestation of dysbacteriosis, it is necessary to conduct a course of restorative therapy to normalize the intestinal microflora.
For this purpose the following are used:
- probiotics (Hilak-forte, Bifiform, Linex, Bifidumbacterin);
- special diet.
Compliance with the diet directly determines how quickly the intestines can recover. Dietary nutrition excludes:
- foods high in fiber (legumes, brown bread, coarse cereals);
- carbonated drinks;
- whole milk;
- leafy vegetables, carrots, beets, cabbage.
During the first week, you can eat only light foods, including low-fat fermented milk products and bio-yogurt.
Strict adherence to all doctor’s recommendations will quickly shorten the time for intestinal recovery and eliminate unpleasant consequences after the procedure.
Colonoscopy results are normal
The following can be considered positive indicators of the study:
- Pale pink or yellowish color of the mucous membrane of all parts of the intestine. The presence of growths changes its shade.
- When exposed to light, the mucous membrane should shine; this indicator indicates normal mucus secretion. Dullness indicates the presence of pathological processes.
- The surface of the shell should be as smooth as possible. Lumps, protrusions, and growths are immediately noticeable during the procedure.
- Accumulations of mucus should not contain pus, fibrin or accumulations of dying tissue; in normal condition they are visible in the form of light-colored small lumps.
- The vascular pattern should be uniform and clearly visible throughout the entire intestine, have a uniform pattern.
Any deviation indicates a particular disease, which is determined by the proctologist.
What could be the consequences if contraindications are ignored?
When asked whether colonoscopy is dangerous, one can give a clear answer that it is a harmless and painless procedure.
The device for its implementation is made of soft elastic material, which allows it to be inserted into the patient’s anus and moved inside without the risk of injury. Its shape allows you to take into account all the features of the anatomical structure of the organ, without creating unnecessary risks during the study.
The device is equipped with a video recorder, which helps the proctologist to see the inner surface of the patient’s intestines with high resolution on the monitor screen.
Colonoscopy involves certain contraindications. They are both a categorical prohibition on its implementation and a recommendation to choose an alternative method.
It is very important to know the dangers of a colonoscopy. If you do not follow the basic requirements for the procedure, this can lead to complications.
Most often they become:
- Allergic reaction.
- Pain syndrome.
- Infection.
- Perforation of the ulcer.
- Hemorrhage into the organ cavity.
Therefore, it is very important to consider the absolute and relative contraindications for intestinal colonoscopy.
It is necessary to carefully prepare for the procedure to avoid complications.
In addition, you need to contact only public or reliable private clinics that have not only all the required equipment, but also highly qualified doctors.
Indications for a colonoscopy examination may include some visible symptoms, including:
- chronic loose stools
- presence of bloody stools after defecation
- black chair
- accumulations of mucus in the stool
- chronic anemia
- the presence of prolonged pain in the projections of the colon
- disruption of the passage of collected gases in the intestines
- prolonged constipation (obstruction) may indicate the presence of diverticula (pathological changes in the intestine, characterized by its thickening and protrusion)
An immediate examination should be carried out in the following cases:
- with erosive changes in the condition of the colon mucosa and its inflammation (for example, with Crohn's disease)
- in cases where polyps on the walls of the colon were identified during various medical procedures
- if there is a suspicion of the presence of neoplasms in the intestinal lumen (tissue biopsy is required)
- inflammation of the intestinal walls
It is imperative to undergo an examination if there has previously been surgical intervention in various parts of the colon, as well as for persons over 50 years of age.
There are a number of contraindications to colonoscopy. It is prohibited to conduct a colonoscopy examination when the patient:
- there are symptoms of inflamed intestines (peritonitis, colitis), as well as its possible rupture (perforation)
- low systolic pressure
- myocardial infarction
For what medical conditions may a doctor postpone a colonoscopy? The procedure is not prescribed due to the high probability of an incomplete examination:
- when the examination cannot be carried out in the presence of hernias (umbilical, inguinal)
- in some cases in the presence of diverticulitis
- after operations on the peritoneum (the colonoscope can disrupt the integrity of the sutures)
- if the patient has an artificial heart valve
- for internal bleeding in the colon
- in case of insufficient preparation for the examination (the presence of feces in the lumen does not make it possible to fully conduct the session)
Why and which doctor prescribes a colonoscopy?
Indications for use
Typical consequences and complications
Is it worth having a colonoscopy: arguments for and against
How much does the research cost?
Quite often it happens that a coloproctologist may prescribe a colonoscopy procedure, which allows you to fully examine the walls of the large intestine. Thanks to a colonoscope, it becomes possible to detect the formation of cancerous tumors and other diseases that can be prevented in the early stages.
Some indications for colonoscopy may directly indicate the presence of polyps, oncology and other pathologies that can be prevented in the initial stages of development. In this regard, the implementation of this procedure is mandatory, since human health depends on it. A colonoscopy session should not be neglected, as it allows for an accurate diagnosis of the condition of the intestine and avoids painful operations on the intestines, which are followed by a long recovery process with many restrictions in diet and lifestyle.
Using a colonoscope allows you to perform a number of manipulations:
- take damaged tissue for histological examination
- stop bleeding in the intestinal cavity, and also remove foreign objects
- identify the presence of diseases in the absence of visible symptoms
- restore full intestinal function in cases of obstruction (for example, when the intestinal lumen is narrowed)
To carry out the examination, an optical soft probe is used, which is equipped with a video camera with a special backlight that allows you to display the image on the display. Thanks to this, the coloproctologist can see what is happening on the monitor and assess the condition of the intestinal walls. The colonoscope is inserted peranally.
Patients often have a lot of questions: “Does it hurt to have a colonoscopy?” or “how long does the examination session last?” The session can be carried out under general anesthesia, and the patient will not feel anything during sleep. To improve the quality of the examination, a certain amount of air is supplied along with the colonoscope (during sleep the patient will not feel the sensation of intestinal distension), which allows the intestine to be increased in volume and smoothed out.
It is imperative to undergo an examination if there has previously been surgical intervention in various parts of the colon, as well as for persons over 50 years of age.
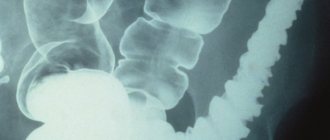
Often many patients are interested in the question: “what is more effective – irrigoscopy or colonoscopy?” Irrigoscopy allows you to see the intestinal projection and its size on an x-ray, as well as determine in which areas of the colon there are narrowings of the lumens.
To carry it out, the intestinal cavity is filled with a barium contrast solution, and then X-ray equipment is used to obtain an image. It clearly shows the anatomical features of the colon, as well as the presence of large tumors.
It should be noted that irrigoscopic examination does not provide a complete picture of the condition of the internal walls of the intestine, since polyps and inflammatory processes cannot be seen in the image. Therefore, colonoscopy is used to make a reliable diagnosis and timely detection of cancer.
source
Have you been struggling with JOINT PAIN for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure your joints by taking the product for 147 rubles every day.
The emergence of internal organs through natural and pathological openings located on the surface of the abdomen under the skin surface is called a ventral hernia. It usually penetrates through existing scars resulting from surgery. Its distinctive feature is its large size. Thus, the larger the scar present on the surface of the abdomen, the larger the protrusion will be.
This phenomenon, in addition to various cosmetic defects, also makes changes in the functioning of such internal organs as the stomach, intestines, diaphragm, and genitourinary system.
Our readers successfully use Artreid to treat joints. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
As mentioned above, a postoperative ventral hernia forms in the area of the scar that appeared after the patient recently underwent surgery. This phenomenon occurs as a result of weakening of the abdominal muscles. It is noteworthy that weakening is considered the most common cause of a hernia in a patient. According to statistics, ventral hernia is in second place in terms of frequency of occurrence after inguinal hernia.
A ventral postoperative hernia may occur a year or even two after surgery. This is due to the peculiarities of the recovery of the patient’s body. Once it appears, it can quickly worsen a person’s health. Most often it is characterized by severe pain.
- Causes of pathology
- Symptoms and diagnosis
- Classification of hernia by size
- Classification of hernia by clinical diseases
- Diagnostics
- ICD 10 code
- Treatment of postoperative ventral hernia
- Prevention of the appearance of a ventral incisional hernia
• The appearance of an inflammatory process in the wound and the penetration of infection into it;
• Presence of pus in the suture cavity. This reason appears extremely rarely. Its appearance depends on the age of the patient, the presence of pathologies and the severity of the infection;
• Failure to comply with a special diet and regimen during the rehabilitation period. The scar becomes denser 7-10 days after surgery, and it finally forms six months after surgery. During the entire rehabilitation period, the suture must be properly cared for;
• Development of diabetes mellitus and renal failure in the patient. They lead to an increase in the healing period of the suture;
• The appearance of atrophy in the abdominal muscles;
• The patient is overweight. Fat contributes to the disruption of blood supply in the abdominal area and is an obstacle to the normal healing of the scar. Also, excess weight increases pressure on the scar;
Possible consequences after the procedure
The only severe complications after CS are perforation of the intestinal wall (less than 1%) and bleeding (0.1%) that developed at the site of the removed polyp. The most common consequence is rectal injury when the probe is inserted.
Other undesirable consequences can be easily eliminated. These include:
- pain in the anus when a probe is inserted and throughout the intestine when air is pumped or at the site of tumor removal;
- flatulence due to air received as a result of manipulation;
- diarrhea caused by the use of laxatives in preparation for manipulation and irritation of the intestinal mucosa with a probe;
- the appearance of high body temperature after colonoscopy;
- consequences of anesthesia.
As with any invasive study, there is a possibility of acquiring viral hepatitis B, C, HIV, syphilis, and salmonellosis.
Isolated cases of splenic rupture have been recorded.
Intestinal perforation
Perforation of the intestinal wall most often occurs in the place of natural bends of the large intestine - in the hepatic and splenic angle. In these places, the ascending segment of the colon passes into the transverse colon (in the right half of the abdomen), and the transverse segment into the descending colon (in the left flank). This localization creates an additional threat to the patient’s life due to the vital organs adjacent to the intestine in this area: the liver and spleen. Often, as a result of perforation and penetration (perforation) into a neighboring organ, it has to be removed due to severe bleeding (spleen).
The following may contribute to the appearance of perforation:
- insufficient preparation of the patient - his restless behavior if the manipulation is not performed under general anesthesia;
- physician negligence;
- device malfunction.
When perforation occurs, a hole is formed in the intestinal wall. Through it, feces exit into the abdominal cavity. There is a sharp pain, which intensifies significantly with the slightest movement. A picture of an acute abdomen develops due to the appearance of peritonitis:
- asymmetry of the anterior abdominal wall and bloating;
- urge to vomit;
- severe tachycardia;
- heat.
In this case, urgent measures are necessary, since the rapid development of peritonitis can be fatal. The patient cannot rise; he is taken to the operating room and undergoes emergency surgery.
Bleeding when removing a polyp
Intestinal bleeding occurs extremely rarely. It may appear as a result of:
- perforation of the intestinal wall;
- polyp removal;
- performing a biopsy for histological examination;
- cracks or other superficial damage to the mucous membrane;
- an existing tumor that is damaged by the device during manipulation;
- infections;
- hemorrhoid injury.
After polypectomy, bleeding in most cases is not profuse and goes away quickly. It occurs rarely; age plays an important role. Most often it occurs in children and elderly adults due to a thinning intestinal wall. In other age groups, blood appears when there are errors in the manipulation: if the intestinal wall is captured more deeply with a loop electrode, to the damaged vascular layer.
Blood appears immediately during or after manipulation. Its isolation is possible 2-3 days after the study or during the first week.
With massive bleeding, which is extremely rare after polypectomy, the following is observed:
- a sharp drop in blood pressure;
- release of a large amount of scarlet blood;
- increasing weakness up to loss of consciousness;
- tachycardia.
In some cases, there is a gradual loss of small amounts of blood over a long period of time. This can lead to anemia. If the patient does not pay attention to traces of blood in the stool in the form of streaks, over time the anemia becomes severe and begins to manifest itself:
- severe weakness, unmotivated fatigue;
- dizziness;
- shortness of breath;
- heartbeat;
- deterioration of nail quality;
- hair loss;
- changes in the blood.
Do they do it for hemorrhoids?
Colonoscopy for hemorrhoids is prescribed in the following cases:
- to confirm the diagnosis previously made by a specialist;
- to identify the extent of the inflammatory process caused by hemorrhoids;
- to determine existing complications;
- to stop existing heavy rectal bleeding;
- as a preparatory study for the upcoming operation;
- to conduct a diagnostic assessment of hemorrhoids and existing tumors formed in the rectal cavity in the presence of characteristic symptoms in the form of sudden loss of body weight, signs of intoxication, changes in stool, etc.
- for the purpose of collecting tissues for further histological or microbiological laboratory studies.