Among the numerous methods of examining the breast, based on the use of the latest advances in diagnostic medicine, such as ultrasound, MRI and CT, mammography performed using X-ray radiation remains the most popular.
Since the negative impact of X-rays on a woman’s health is undeniable, one of the most important aspects of mammography is to obtain the maximum amount of information about the condition of the mammary glands with the least damage to the body.
Actually, the quality of the information received is a priority for any examination method, and it is this that determines the timing when it is better to do mammography, since the cyclic changes that occur in the female body affect all organs of the reproductive system, causing minor changes in the structure of breast tissue.
When are you referred for a mammogram?
Mammography is a non-invasive examination of the breast using X-rays (without instruments penetrating the skin), which allows the detection of malignant tumors at an early stage. Referrals for examination are issued by the following specialists: gynecologist, mammologist, endocrinologist, surgeon.
Experts cannot identify the exact reasons why tumors arise; they name the most common factors, including:
- hereditary characteristics;
- hormonal stress due to frequent abortions or pregnancies, as well as due to the use of oral contraceptives;
- bad habits (especially smoking);
- technogenic, environmental factors.
It is recommended to perform mammography in the following cases:
- after the age of 40-45 years or with early menopause regularly every year;
- with painful sensations and lumps in the chest or with discharge from the nipples, with changes in the color and shape of the nipple circles;
- in case of chronic diseases (gynecological, endocrine), with a genetic predisposition to tumors;
- for prophylaxis after tumor treatment or for evaluation of treatment.
Modern equipment produces minimal doses of ionizing radiation, close to the natural radiation background of the environment. This examination is considered conditionally dangerous and usually does not cause negative consequences, however, there are certain contraindications for mammography:
- pregnancy at any stage;
- period of breastfeeding and lactation;
- post-abortion period up to six months;
- inflammation or damage to the skin on the breasts and nipples;
- woman's age is up to 35-36 years.
This is due not so much to the supposed harm, but to the fact that during pregnancy and lactation the structure and shape of the mammary gland changes, so the examination results may be unreliable. If necessary, doctors individually decide on the appointment of this procedure; ultrasound mammography (ultrasound of the breast) is possible.
The description of the results of ultrasound diagnostics is subjective due to the variable structure of tissues and is greatly distorted by hormonal levels, the patient’s age and reproductive period, body weight and other indicators. There are problems with the unification of evaluation criteria for ultrasound examination - what is considered normal, acceptable or pathological condition.
Combination of X-ray mammography with other diagnostic procedures
Like any other radiation diagnostic methods, X-ray mammography causes some harm, increasing the risk of developing cancer by tenths of a percent after each procedure. Taking into account the need for annual fluorography, which carries twice the radiation load than mammography, cumulative radiation exposure to the thoracic region can lead to long-term negative consequences.
The risk of developing cancer is especially high in young patients, since all their metabolic processes occur at a relatively high speed, and when exposed to even minor mutagenic factors, the percentage of formation of malignant tumors is much higher than with a similar effect on patients over 50 years of age.
Despite the fact that the amount of radiation exposure is calculated based on the annual radiation exposure rate, that is, the total number of units affecting a person is taken into account, taking into account the background radiation that constantly accompanies it, it is not recommended to perform mammography and fluorography at the same time. The interval between procedures should be at least 3 months.
Taking all this into account, the doctor must determine when the diagnosis can be performed and which type of mammography is more appropriate to use, taking into account the patient’s age and the number of x-ray procedures available in the anamnesis.
Important! The restriction on the simultaneous use of mammography and fluorography does not apply to women with a diagnosed malignant neoplasm. In this case, comprehensive diagnostics allows us to identify the extent of spread of the malignant process, the presence or absence of metastases. Ultrasound mammography is performed like a regular ultrasound.
Types of breast examination
There are more effective and modern diagnostic methods compared to conventional x-ray mammography.
- Computer (digital) X-ray mammography – the results are displayed on digital media rather than on film, while the radiation dose is reduced. This technique makes it possible to more accurately determine pathology and everywhere replaces the usual film recording of results.
- Radiothermometric (microwave) mammography – determines the temperature of various parts of the breast. To do this, the skin temperature is measured at several points with a special device and a thermogram is built. Areas with elevated temperatures require special attention, as tumors may be detected there.
- Electrical impedance mammography - examines the resistance of breast tissue to electrical impulses. The breast moistened with water is exposed to an alternating low-power current, which is not felt by the patient. The attached sensor transmits a detailed image to the monitor, it is processed by a special program and, as a result, it is determined where the muscle, fat, connective tissue is, where there is fluid, and calcification deposits. This technique is completely safe, but does not guarantee accurate test results (pathology is detected in less than 80%).
- Magnetic resonance mammography - this technique does not use ionizing radiation, but affects the body through magnetic fields, therefore it is completely safe. This examination can be carried out using contrast agents, which indicate breast tumors in the earliest stages of formation. The patient first takes special drugs that tend to accumulate in tumor tissues, so the tumor becomes noticeable during examination. As a result, the doctor receives information about the size and location of the tumor, and the presence of metastases.
- Tomographic mammography – the obtained images of the mammary gland are combined into a three-dimensional image, from which the location of the tumor and other data about the disease can be determined. Tomosynthesis of the breast, which produces images in the form of thin sections, is increasingly being used. As in computed tomography, data for tomosynthesis is obtained by displacing the emitter.
- Tomographic laser mammography uses laser radiation in the infrared range. This produces three-dimensional images with very informative results. Literally every millimeter of tissue can be examined, and the diagnostic accuracy is quite high.
Quite expensive techniques are rarely used for routine examinations, but if a tumor is suspected, they allow a quick and accurate diagnosis.
Psychologist
Oddly enough, preparation for IVF, along with passing mandatory laboratory tests, sometimes needs to begin with a visit to a psychologist. Don't be surprised! The role of this specialist is greatly underestimated in our country, and part of the reason lies in the patients themselves, who neglect going to this specialist.
Oncologist
If you have a history of cancer and more than 5 years have passed since the end of treatment, you will need to consult an oncologist to authorize the IVF procedure and pregnancy.
Neurologist
Consultation with this specialist may be required if the patient has a history of neurological diseases or complaints indicating a possible neurological pathology.
Cardiologist
Cardiological pathology with good compensation may not have any clinical manifestations. Therefore, an ECG is a mandatory procedure. Changes in the ECG, examination by a therapist, and the nature of previous pregnancies may require consultation with a cardiologist.
Andrologist
An andrologist deals with problems related to male infertility.
- a relatively new direction in medicine, in which genetics, general and molecular biology, embryology, physiology and endocrinology intersect. Of course, the main specialization of this area is. Moreover, we are talking not only about the influence of medical and biological indicators, but also about the socio-psychological aspects of life.
Properly selected drug therapy in some cases of male factor infertility can significantly improve sperm parameters and optimize IVF results.
If there are no sperm in semen, testicular sperm retrieval (TESA) or epididymal sperm retrieval (MESA) procedures may be required.
Therapist
A consultation with a therapist is scheduled after receiving the results of blood tests and ECG. Questioning and examination allows us to identify hidden extragenital pathology in a woman. In the presence of chronic diseases, the therapist assesses risk factors and gives a conclusion that there are no contraindications to IVF and pregnancy.
Mammologist
Consultation with a mammologist is a necessary annual procedure for women over 18 years of age!
The mammary glands are a hormonally dependent organ, because changes in the structure of the mammary glands depend on the menstrual cycle, namely on the two most important female sex hormones - estrogen and progesterone. Various changes in breast tissue most often occur due to an imbalance of these two hormones.
A doctor who deals with the prevention and treatment of diseases of the mammary glands is called a mammologist.
.
How to consult a mammologist
Examination of the mammary glands is carried out from 2 to 10 days of the menstrual cycle, inclusive, to exclude hormonal effects on the glands, as mentioned above. If there is no menstruation, then any day.
Inspection
mammary glands is carried out in good lighting in two main positions:
- Standing, arms are lowered freely along the body;
- Standing, arms raised, palms behind head.
During the examination they evaluate:
- size of the mammary glands;
- contours;
- symmetry;
- condition of the skin (color, presence of swelling, rashes, ulcerations);
- condition of the nipple and areola (size, shape, location, discharge from the nipple, their nature).
Palpation
examination of the mammary glands is performed with the patient lying on her back and in a standing position (hands on her head).
During palpation, the following characteristics are assessed:
- consistency;
- elasticity;
- uniformity;
- sensitivity;
- the presence of space-occupying formations, their localization (location, size, shape, mobility, clarity of contours);
- axillary lymph nodes are palpated.
If any abnormalities are detected or even suspected, the mammologist will refer you for an ultrasound (ultrasound examination) or mammography (x-ray examination) to clarify the diagnosis.
Consultation with a mammologist before IVF
If you are entering into an in vitro fertilization protocol, you must be examined by a mammologist. Before IVF, this is not the only specialist you will have to visit. The conclusion of a mammologist for IVF, as well as a general practitioner, is necessary to determine possible contraindications to pregnancy or hormonal stimulation.
Before consulting a mammologist, it is advisable to first do an ultrasound of the mammary glands (if you are under 35 years old) or a mammogram (if you are over 35 years old). These studies allow you to evaluate the structure of the mammary glands.
If there are no problems, the doctor will issue a conclusion, and you can enter the IVF protocol. If a disease is discovered that is a contraindication to stimulation or pregnancy, you will first have to undergo a course of therapy, and only then engage in family planning.
You should immediately contact a mammologist in the following cases:
- painful sensations, a feeling of fullness, heaviness in the chest, especially if these sensations do not go away after menstruation;
- any changes in the shape, size and symmetry of the mammary glands;
- changes in the configuration of the mammary glands (retracted areas, protrusions);
- changes in the condition of the nipple and areola (dark area around the nipple): deformation, ulcerations, retracted areas.
- the presence of discharge from the nipple, if you are not pregnant or not a nursing mother;
- changes in the condition of the skin (redness, swelling, “lemon peel”);
- dilation of blood vessels;
- the presence of nodular seals, painful areas.
Breast ultrasound and mammography
Ultrasound is widely used in the diagnosis of breast diseases. The study is especially informative when examining young women (up to 35 years), and ultrasound is also informative for assessing the condition of silicone prostheses.
Ultrasound scanning allows you to obtain an image of all structures of the mammary glands. This method does not require special preparation, but it should be remembered that it is carried out in the first phase of the menstrual cycle (up to the 10th day of the cycle). The beginning of the cycle is counted from the first day of the last menstruation.
Mammography is a highly informative method for examining the mammary glands. According to various authors, diagnostic accuracy ranges from 60% to 90%. Mammography is contraindicated for women under 35 years of age, as well as during pregnancy and breastfeeding.
Regular preventive examinations - once a year, and for women 40 years of age and older - 2 times a year, are a timely detection of not only oncological, but also benign diseases of the mammary glands, which allows for high-quality treatment.
The mammologist may also prescribe the following studies:
Cytological examination of nipple discharge.
When discharge from the nipples appears outside of lactation, the mammologist prescribes a cytological examination of the discharge. After analyzing their composition, the doctor will conclude about the presence or absence of any disease and prescribe the appropriate treatment.
Blood test to assess hormonal status.
If a hormonal imbalance in the body is suspected, the mammologist must clearly know the ratio of estrogen, progesterone, prolactin and other hormones in order to make the right decision on treatment.
Obtaining a certificate for IVF from a therapist can turn into a long and unpleasant saga. After passing a series of tests, a woman who wants to undergo in vitro fertilization is sent to receive a certificate from a therapist, who makes the final decision - whether IVF can be performed for this patient or not.
The list of tests that need to be taken for IVF is quite standard - urine and blood tests, fluorography, ECG and ultrasound. The therapist may also ask for a certificate from a mammologist. If the patient has serious chronic diseases, the therapist may require a certificate from specialized doctors.
The problem of obtaining a certificate authorizing IVF from general practitioners is often associated with reinsurance. The doctor is afraid to issue a permitting certificate for fear of adverse consequences. And of course, no one has canceled the rudeness and sloppiness in Russian clinics. Long queues and, to put it mildly, not the most friendly atmosphere in them are a mandatory attribute of any queue to see a therapist.
All this leads to the fact that a woman caught in a bureaucratic labyrinth, already excited about the upcoming IVF procedure, begins to think: “Maybe I can buy a certificate from a therapist somewhere?” The woman is also pushed to this idea by the time limit - the IVF procedure is expensive and time-consuming. The entire course is calculated with an accuracy of one day and cannot be postponed. So the idea of buying a medical certificate is quite natural and we will help you in this matter.
Where can I buy a certificate for IVF from a general practitioner?
You can order a ready-made certificate from a therapist with permission for IVF from us. We process any medical documents with delivery throughout Moscow within one day. By contacting us, you have the opportunity to receive an official medical document without visiting doctors and even without undergoing tests.
The certificate will be issued on an official form. The diagnosis will indicate that there are no contraindications to the in vitro fertilization (IVF) program and pregnancy. The certificate is certified by the seal of the required medical institution and the signature of the doctor.
Ordering a certificate for IVF with delivery is very simple - just call us at the phone number listed on the website or send a request through the feedback form. Our operator will contact you shortly and clarify the details of the order.
Certificates for IVF from a mammologist
You can also buy a certificate for IVF from a mammologist from us. When obtaining this certificate, sometimes problems arise that cannot be resolved quickly, but time is running out and the issue with documents must be resolved quickly.
Just like a certificate from a therapist, this document is drawn up by professional medical professionals. experienced workers. We have a special group of specialists who have experience in working on these certificates in order to prepare all “female” certificates.
Delivery can be ordered to any place convenient for you in Moscow and even in the Moscow region. Our courier will deliver the certificate to central metro stations for free! Money is transferred to the courier only after checking that the document is filled out correctly. Processing and delivery time is one day. Contact us!
Examination of a man:
- spermogram (valid for 1 year)
- blood test for AIDS, hepatitis B and C (valid for 3 months)
- syphilis (valid for 1 month)
- blood test for herpes simplex virus antigens 1, 2 (valid for 3 months)
- microscopic examination of urethral discharge; trichomoniasis (culture), ureaplasmosis (PCR), mycoplasmosis (PCR), chlamydia (PCR); herpes simplex virus 1.2 (PCR), cytomegalovirus (PCR) (valid for 6 months)
Examination of a woman:
- blood test for the hormones FSH, LH, prolactin, testosterone, TSH, free T4, DHEA sulfate, 17-OHP, AMH (valid for 6 months).
- blood test for AIDS, hepatitis B and C (valid for 3 months).
- syphilis (valid for 1 month)
- (valid for 1 month)
- microscopic examination of urethral discharge for gonococcus (valid for 1 month)
- smears for infections: chlamydia (PCR), cytomegalovirus (PCR), mycoplasma (Mycoplasma genitalium PCR), herpes (PCR), HPV (PCR) (valid for 3 months)
- ureaplasma (Ureaplasma urealyticum) (culture), mycoplasma (Mycoplasma hominis) (culture) (valid for 3 months)
- (valid for 1 year)
- an. clinical blood (valid for 1 month)
- blood an. biochemical: creatine, bilirubin, total protein, ALT, AST, alkaline phosphatase, glucose (valid for 3 months)
- blood type, Rh factor (valid for 1 month)
- blood test for herpes simplex virus antigens 1,2 (valid for 3 months)
- blood test for IgG and IgM antibodies to rubella, toxoplasma, cytomegalovirus (valid for 3 months)
- hemostasiogram (valid for 1 month)
- general urine an. (valid for 1 month)
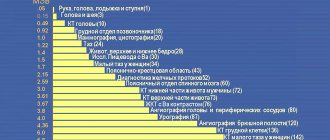
- ECG (valid for 1 year)
- Fluorography (valid for 1 year)
- physician's conclusion about the absence of contraindications for pregnancy and IVF (valid for 1 year)
- consultation and conclusion of a mammologist on the absence of contraindications for pregnancy and IVF (valid for 1 year)
- Ultrasound of the mammary glands (valid for 1 year)
- Mammography (women over 35 years old) (valid for 1 year)
Other studies, if necessary, as prescribed by a doctor:
- X-ray of the skull, CT or MRI
- laparoscopy
- Ultrasound of the kidneys, liver, abdominal cavity
- urine test for 17-KS
- genetic consultation
- karyotyping
- consultation with an andrologist, urologist, endocrinologist, therapist.
- other
Examination for a surrogate mother
- Blood group, Rh factor
- Clinical blood test
- Blood test for antibodies (to Toxoplasma, cytomegalovirus, IgG and IgM to rubella)
- Biochemical blood test (creatinine, bilirubin, total protein, ALT, AST, alkaline phosphatase, glucose)
- Blood test for hormones (TSH, free T4)
- General urine analysis
- Cervical and vaginal smear
- Cytological examination of the cervix
- Examination by a general practitioner + ECG
- Therapist's conclusion about the absence of contraindications to pregnancy and IVF
- Fluorography
- Examination by a mammologist + ultrasound of the mammary glands (from 6 to 12 days of the menstrual cycle). Conclusion from a mammologist confirming the absence of contraindications to pregnancy and IVF.
- Conclusion from a psychiatrist stating that he is “not registered”
- Marriage certificate
- Children's birth certificate
Screening for oocyte donors
- Blood test for AIDS, hepatitis B and C, syphilis
- Blood group, Rh factor
- Clinical blood test
- Blood test for AMH, TSH
- Blood test for coagulation (hemostasiogram)
- Blood test for herpes simplex virus 1 and 2
- Blood test for antibodies: toxoplasma, cytomegalovirus, IgG and IgM to rubella
- Biochemical blood test: creatinine, bilirubin, total protein, ALT, AST, alkaline phosphatase, glucose
- General urine analysis
- Karyotyping (medical genetic examination)
- Cervical and vaginal smear
- Microscopic examination of urethral discharge for gonococcus (Neisseria gonorrhoeae)
- Smears for infections: chlamydia (PCR), cytomegalovirus (PCR), mycoplasma (Mycoplasma genitalium PCR), herpes (PCR), HPV (PCR), ureaplasma (Ureaplasma urealyticum) (culture), mycoplasma (Mycoplasma hominis) (culture)
- Cytological examination of the cervix
- Examination by a general practitioner + ECG, a general practitioner’s conclusion about the absence of contraindications to donation.
- Fluorography.
- Examination by a mammologist + ultrasound of the mammary glands (from 6 to 12 days of the menstrual cycle). Conclusion from a mammologist about the absence of contraindications to IVF.
- Geneticist's conclusion
- Conclusion from a psychiatrist stating that he is “not registered”
An increasing number of couples are finding themselves infertile. Modern medicine gives them the opportunity to find the baby they want. The eco program in Russia has become free since 2009, thanks to which every married couple has a chance to have a baby.
Changes in the female body during different periods of menstruation
Progesterone, or the “pregnancy hormone,” is secreted by the ovaries and adrenal glands; it is necessary to prepare the uterus for conception, helps maintain pregnancy, and has a beneficial effect on the nervous system. This hormone determines the process of ovulation (the appearance of a mature egg from the ovary approximately in the middle of the menstrual cycle).
In a healthy state, progesterone levels in the first half of the menstrual cycle are relatively low. Further, the hormonal level rises depending on the phase of menstruation. After ovulation, if pregnancy occurs, the level of progesterone increases further, otherwise it decreases and menstruation begins.
Progesterone has a very strong effect on the mammary glands in the second half of the cycle, so mammography during or after ovulation is not very informative. It's best to do a breast exam in the first half of your cycle, before progesterone levels rise and ovulation occurs. During this period, the mammary glands are the most painless and soft against the background of increased estrogen levels.
Mammography and menopause
It has already been described above how hormonal levels affect a woman’s breasts every month, but what to do if menstruation stops and menopause occurs? If a woman is fifty years old, then she is close to the onset of menopause - the period of preparation for menopause. Menstruation stops, hormonal levels stop creating the usual “roller coaster” and stabilize.
On what day should I have a mammogram if I don’t have my period? Often women after reaching the age of 45-50 worry that hormonal fluctuations will distort the results. Doctors say that after menopause you can come for a breast examination any day; mammograms will correctly show the condition of your breasts.
In what phase of the menstrual cycle should you be examined?
The menstrual cycle depends on individual characteristics and can change during different periods of sexual activity. The following main types are distinguished according to cycle duration:
- Short menstrual cycle (lasts 21-28 days) - mammography is performed from the 3rd to the 7th day of the cycle.
- The average cycle (lasts 28-35 days) - in this case, you can do the examination from 5 to 12 days.
- A long cycle (longer than 35-36 days) is the most favorable period for mammography from 9 to 18 days.
In case of an irregular cycle, mammography is performed after the end of menstruation; upon the onset of menopause and the cessation of menstruation, it can be examined at any time. The procedure occurs in this way: a woman stands in front of a mammograph (X-ray machine), the breast is fixed between two plates, slightly squeezing.
Each breast is checked separately, this allows you to compare their anatomical condition and identify compacted nodes. An image is taken in two projections, from which the doctor determines the presence of tumor tumors. Sometimes there is a need to take photographs with additional projections in order to clarify the results.
Mammography in the first days of menstruation
To obtain reliable mammography results, it is important to correctly determine the day of mammography, since on different days and phases of the cycle, a woman’s breasts are in different states. Doctors, when asked whether it is possible to go for a mammogram during menstruation and 1–2 days before it, answer in the negative, since diagnosing a tumor during this period is problematic. Under the influence of progesterone, the glandular tissue of the breast swells and its structure becomes denser.
An additional factor that forces women to refuse to undergo the procedure in the first days of menstruation is intense pain and breast sensitivity. It is impossible to properly fix the gland between the plates of the device; the examination results are superficial and unreliable.
Even in the last days of menstruation, a woman’s breasts remain swollen; their tissues contain a lot of fluid, which is why, if a tumor is present, it goes unnoticed. If a mammography examination is urgent, then it is recommended to make an appointment with a doctor, waiting until at least the last critical day, but not earlier.
In a situation where a woman has not visited a mammologist before, and she has not had her period for several months, their unexpected arrival may indicate the presence of a tumor. It is important to immediately visit the clinic and undergo diagnostics, and then show the records of the examination to the doctor.
Possible test results
In a normal state, there are no visible compactions or darkening in the photographs, the tissues look uniformly dense, without foreign inclusions. Lymph nodes of normal size, vessels and milk ducts are visible.
The standard results of the description of the mammography performed depend on the presence of pathologies:
- zero category – incomplete assessment if the results are insufficient or questionable to make a diagnosis;
- Category I – negative, if the woman is healthy, no abnormalities are noticed in the breasts;
- Category II – a benign formation was detected;
- Category III – a benign formation has been identified, which requires clarification and additional testing; most likely, a repeat mammogram is required in six months;
- Category IV – a suspicious tumor, for which a biopsy is prescribed for an accurate diagnosis;
- Category V – a malignant tumor is highly likely to be found, so a biopsy is necessary;
- Category VI – established malignant tumor, confirmed by biopsy.
When determining the results, the specialist focuses not only on the images obtained, but also on the medical history and indicators of other studies. If benign tumors form in the breast tissue, they can be identified by the following signs:
- a darkened area of a more regular shape (round or oval);
- clear local contours;
- adjacent parts do not participate in the tumor process;
- slow growth of the tumor without germination into surrounding tissues (in dynamics there is an increase in the diameter of the tumor up to 10% within a year).
Signs of malignant tumors in the image:
- irregular shape of darkening (elongated, with noticeable constrictions);
- the contours of the darkening are unclear, blurry, intermittent;
- around the tumor the darkening is less intense (due to infiltration of surrounding tissues);
- the darkening focus can be connected to the skin or to the nipple;
- thickened skin in the tumor area;
- with cancerous tumors, the diameter of the tumor increases rapidly (approximately doubling in 10-12 months).
How to properly prepare for the procedure
In order for the mammography result to be as informative as possible, and not have to expose yourself to x-ray radiation again when taking a second picture, you should properly prepare for the procedure:
- When making an appointment for a mammogram, accurately calculate the day of your menstrual cycle;
- If you are undergoing the procedure for the first time, check all the details with your doctor;
- 1-2 days before the examination, stop consuming caffeine-containing products;
- if a woman is afraid that she will be in pain during the procedure, she can first take painkillers that will not affect the result (Ibuprofen);
- on the day on which the procedure is scheduled, you cannot use creams, talc, powders and antiperspirants, as they can affect the result of the study;
- Do not wear jewelry around your neck or remove it before the procedure;
- wear clothes that can be removed quickly;
- if this is not the first procedure, then you can bring previous images to your appointment with a mammologist;
- Before the procedure, the doctor needs to tell about all complaints and show the place where the lump is localized.
You need to be attentive to your health and if any lumps appear in your chest, immediately seek help from a specialist, because timely diagnosis gives a great chance of a complete cure.
How often can you get a mammogram?
Breast cancer ranks second (after lung cancer) among all cancers. Benign and malignant breast tumors can occur at any age; during menopause and menopause, the likelihood only increases. Tumors are diagnosed in every twelfth woman under 40 years of age, and with age this ratio gradually changes: in every tenth woman after 60 years of age.
More than 50 types of mastopathy (benign tumors) are known: lipomas, fibroadenomas, fibrocystic tumors and many malignant types. All tumors are more effectively treated in the first stages, so it is necessary to perform mammography annually after 40 years of age or more often when observing the first suspicious symptoms. To evaluate the treatment, mammography is prescribed repeatedly, even over the course of a month.
Read also: Why do breasts shrink?
Based on the above, several conclusions can be drawn: mammography is a mandatory annual procedure for middle-aged women after 40-45 years. Any complaints about pain, discharge from the breast, changes in color or shape should be referred to a specialist.
Constant self-diagnosis of the breast condition is necessary, but home self-medication is strictly contraindicated. Timely seeking medical help is the key to successful, effective treatment of any tumor.
Why is the procedure needed?
Before we talk about what day of the cycle to do a mammogram, let’s look at why it is needed and what it is.
Essentially, a mammogram is the same as an x-ray, during which the mammary glands are alternately pressed between glass plates to take an image.
Mammography is a more informative examination compared to ultrasound; it allows us to identify tumors that are not visible on ultrasound. Mammography is also indicated if ultrasound results are inaccurate.
The examination is recommended for all women over 40 years of age, and the older the patient gets, the more often mammography should be done, ideally once a year.
There are indications for mammography such as:
- Woman's age;
- Complaints of chest pain, weakness, increased sweating;
- If you need to supplement or clarify the results of the ultrasound;
- Monitoring the postoperative condition;
- Suspicions of breast cancer;
- Recommendations for undergoing mammography by a gynecologist.
The examination itself lasts from 10 minutes to half an hour. As a rule, the specialist asks you to hold your breath as standard while taking the picture to give it clarity and sharpness.
It must be remembered that in the life of every woman there are days and times that are most suitable for examination and when there is no need to do a mammogram.
Procedure right before or during menstruation
You should not have a mammogram before your period, just like during your period. This is due to the fact that the mammary gland swells during this period, and the density of its texture increases. This is a problem for research, since X-rays do not pass through well, and the result may be unreliable. Moreover, during menstruation the breasts are painful, diagnosis can cause severe discomfort. It will not be possible to fix the breasts in the desired position during menstruation; the woman will not be able to stand for the required amount of time in the desired position.
A factor in favor of refusing diagnostics before and during menstruation is that the breasts accumulate fluid at this point. It does not allow tumors and other neoplasms to be recognized.
The issue of irregular periods deserves special attention. If a woman has them 1-2 times a year or are absent for a long period of time, and then suddenly appear, a mammogram is scheduled for the nearest possible date.
What tests should I go to the doctor with?
You can go to the appointment without tests if you are healthy. An examination and, if necessary, an ultrasound and mammogram are sufficient. What tests should you go to a specialist for if you experience discomfort during menstruation or feel lumps? The following results will help make a diagnosis:
- blood test for hormones: ovarian (FSH, progesterone, estradiol) and thyroid (TSH, T3, T4);
- Ultrasound of female genital organs (ovaries, uterus);
- gynecologist consultations;
- cytology of nipple discharge.
If you come to the doctor without the results of these tests, the doctor will write a referral for the necessary examinations.
With this, we say goodbye and invite you to visit our website if new questions arise about women’s “weapons” - the breasts. Share interesting information with friends using the share button via social networks.
Types of research
Modern mammography comes in two types: film and digital. Film originates from the twenties of the last century. This is a common and fairly effective diagnostic method, but not without its drawbacks. These include:
- Difficulties in diagnosis for formations that are small or poorly contrasted.
- The inability to change any characteristics of an x-ray after the exposure has been taken.
- A technically labor-intensive and complex process of image processing.
- Premises and equipment for their storage and the creation of a special archive are required.
- It is not possible to transmit data digitally for consultation purposes.
And, although film mammography has been used for a long time and has proven itself, modern medicine requires a more informative research method.
Digital Research
Today, a worthy analogue of film mammography is the digital research method. It lacks the shortcomings of its predecessor. In addition, the method has additional advantages. The most important among them are the following:
- Economic feasibility of such screening.
- Reducing radiation doses.
- Increased efficiency of the method, the ability to detect the disease at an earlier stage.
- Using telecommunications to transmit digital images and receive consultations.
Unfortunately, digital devices are not currently available in all medical institutions, but over time they will finally replace film analogues. To carry out diagnostics on a modern device, it is also necessary to take into account the day of the cycle. Despite the greater information content and better visualization of breast formations, the principle of operation of the method remains the same. Tight compression of the organ is necessary to improve image quality, detailed examination of all structures and reduce radiation exposure to the gland.
Therefore, the same period remains optimal – days 5–12 of the patient’s menstrual cycle.
Alternative diagnostic methods
Doctors prescribe ultrasound (US) and magnetic resonance imaging (MRI) to patients to visualize tumors as an alternative to mammography.
If the X-ray image clearly shows changes in the tissues of the mammary glands, then the image obtained during an ultrasound also allows us to assess the condition of the regional (located nearby) lymph nodes. Ultrasound diagnostics makes it possible to preliminarily distinguish a benign tumor from a malignant one, as well as examine foci of pathology in places that are not visible on a mamogram (for example, if they are close to the chest).
MRI allows you to obtain volumetric layer-by-layer images, which visualize even the smallest changes in soft tissues. In this regard, this diagnostic method gives too many false positive results, which is why patients are needlessly subjected to many unpleasant tests, including biopsies.
In addition, examination with a magnetic resonance imaging scanner is long (more than 30 minutes) and expensive. Therefore, it is recommended to carry it out after mammography if a woman has alarming symptoms, but the doctor cannot make a diagnosis based on the X-ray images obtained.
In response to the question of whether it is painful to do mammography of the mammary glands, it should be said that it all depends on the individual sensitivity of the patient and her pain threshold. Women may feel discomfort when their breasts are squeezed between the plates of the X-ray machine, but only 15% of patients experience distinct pain.
As practice shows, pain occurs in those women whose mammary glands are very elastic. In isolated cases, pain persists for several hours after the examination. It is extremely rare for patients to have small hematomas on the surface of the breast after diagnosis. Therefore, there is no reason to be afraid of the examination.