By the end of 2020, there were 3,404,237 people in Russia with cancer (2.32% of the country’s population). Of these, 133,863 suffered from cancer (malignant neoplasms) of the respiratory system (3.9% of the total number of patients at oncology clinics). And although lung cancer was inferior in incidence to tumors of other locations (neoplastic tumors of the mammary glands, uterus, colon, hematopoietic system), the disease did not become less dangerous.
Lung cancer is one of the most common pathologies in the structure of oncological diseases
X-ray diagnostics is the most common method for detecting lung cancer, including in the early stages. But X-ray studies alone, even highly informative ones (CT), are not enough to make a diagnosis. Cancer of the lungs (and other organs) must be confirmed by histological examination. Therefore, x-ray is mandatory, but not the only diagnostic procedure recommended for suspected lung cancer. However, within the framework of this article, only radiological research methods will be considered.
Ways to get a picture of the lungs
X-ray examination is the study of the chest organs. This happens using X-rays. The image is captured on paper or film. The final image reflects the position of bone tissue, respiratory organs and mediastinum, their shape, and allows you to confirm or exclude pathology. For these purposes, the patient may be prescribed:
- fluorography;
- bronchography;
- radiography;
- scintigraphy;
- fluoroscopy;
- CT.
Fluorography is a preventive procedure that is recommended to be performed regularly by both adults and children. The image is transferred from a special fluorescent screen. The method is fast and affordable, but has several significant disadvantages.
Patients face high radiation exposure, and the anatomical dimensions of the organ being examined are distorted. Neoplasms smaller than 4 mm in size are often not visualized or cannot be read even by a specialist. Because of this, fluorographic examination is often replaced by other methods of lung radiography.
During bronchography, a contrast agent is injected into the patient's bronchi. The procedure is accompanied by unpleasant sensations and high radiation exposure. Additional problems arise if you have an allergic reaction to the contrast solution. This method is rarely used, and mainly only if it is not possible to conduct a CT scan of the chest.
During a survey type of chest x-ray, the condition of the chest organs is assessed. To begin with, a standard forward projection is performed. Additionally, other procedures may be prescribed; the doctor sometimes needs pictures of individual areas or in lateral reflection. The radiation dose with this method is minimal, the study is actively carried out to detect tuberculosis or cancer at the earliest stages of the disease.
When an X-ray of the lungs is performed, the rays are passed through the patient's body and illuminate the photographic film. The x-ray shows a pulmonary pattern consisting of gray, white and very dark spots. If the clinic has a modern digital device, the image is formed on a special receiver and displayed on the monitor.
We recommend reading! Follow the link: MSCT what is it
CT diagnosis of lung cancer
PREVALENCE OF LUNG CANCER AND RISK FACTORS
Lung cancer, a tumor of the bronchial epithelium, is one of the most common cancers in the world. Every year, more than 10,000 thousand people in Russia are diagnosed with malignant neoplasms of the respiratory system, and in the world this figure is even higher. Bronchogenic malignant tumors are one of the most common causes of death from cancer and the most common type of oncopathology of the tracheobronchial tree.
Risk factors for lung cancer include:
1) Living in environmentally unfavorable areas.
2) Work in industries associated with inhalation of dust particles, metals, paint fumes and active chemicals, even with protective equipment. The most unfavorable is inhalation of asbestos dust, then coal dust, as well as vapors of heavy metals, arsenic, chlormethyl ether, chromium, and mustard gas.
3) Tobacco smoking is the main predisposing factor for neoplasms of the tracheobronchial tree. In active smokers, the risk of developing cancer is up to 10 times higher than in non-smokers, and in passive smokers - up to 2 times.
4) Specific diseases. There is a direct connection between tuberculosis, asbestosis, silicosis, other diseases manifested by diffuse or local pneumosclerosis, and malignant neoplasms of the bronchi.
MANIFESTATIONS OF LUNG CANCER - WHEN CAN YOU SUSPECT THE DISEASE?
In order not to miss the first signs and symptoms of lung cancer, you must pay attention to the following changes in your health: the appearance of a cough with sputum streaked with blood, a sharp loss of weight for no apparent reason, an increase in body temperature, especially in the form of “peaks” accompanied by chills , increased sweating.
A direct indication for CT is the detection of a clearly focal shadow in the image during fluoroscopy or radiography. Of course, lung cancer on X-ray does not look very specific - after all, similar changes can also be caused by tuberculosis, other benign tumors, and even pneumonia. All these conditions can be differentiated using CT.
Get MSCT of the lungs in St. Petersburg
HOW TO DETECT LUNG CANCER?
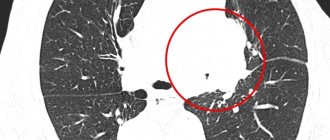
X-ray for lung cancer reveals a rounded shadow on the left. For the purpose of differential diagnosis (to distinguish lung cancer from tuberculoma, cyst or pneumonia), it is necessary to perform computed tomography - CT.
The most effective diagnostic method for lung cancer is multislice computed tomography (MSCT). In most cases, contrast is not necessary to see the tumor on CT scans. Contrast enhancement is used mainly in the diagnosis of central tumors in order to distinguish a small soft tissue node in the root of the lung from the pulmonary vessels located nearby. CT is an indispensable method for determining the size of the tumor, the extent of damage to the root of the lung, mediastinum and chest, and assessing damage to the lymph nodes. All these details ultimately determine the stage of the cancer process, so accurate analysis of the results of computed tomography is extremely important for prognosis.
Another tomographic research method, magnetic resonance radiography (MRI), is almost never used for diagnosing pulmonary tumors, as it poorly detects changes in lung tissue. The fact is that lung tissue contains a large amount of air, which does not give a signal on MRI.
Ultrasound examination (ultrasound) also cannot reliably diagnose changes in lung tissue, however, this method can be used to detect changes in the surrounding pleura.
X-ray and fluoroscopy can be used to detect pulmonary formations, but the isolated use of these methods does not allow a reliable diagnosis. Bronchography as a way to detect lung cancer is also a thing of the past.
Among the instrumental methods for diagnosing central tumors, fibrobronchoscopy (FBS) is very good - an endoscopic method, thanks to which you can not only see the narrowing of the bronchial lumen with your eyes, but also take part of the space-occupying lesion for histological examination.
HISTOLOGICAL CLASSIFICATION OF LUNG CANCER AND SURVIVAL PROGNOSIS
According to the histological classification of bronchogenic cancer of the latest revision (from 1999), 6 types of tumors of the tracheobronchial tree are distinguished:
1) Adenocarcinoma - detected in approximately 35% of all cases. Most often, this is a peripheral tumor that looks like a single (solitary) node of various sizes with typical signs of malignancy, with the presence of spicules - radiant edges, which are formed due to the growth of cancer along the lymphatic vessels; areas of necrosis, decay and hemorrhages in the tumor stroma. Adenocarcinoma metastasizes often and early. The prognosis is very variable, largely depending on how early the formation was detected.
2) Squamous cell non-keratinizing cancer is a common variant - up to 35% of all cases of lung tumors. It has the best prognosis and rarely metastasizes. In approximately 65% it develops in one of the central bronchi and causes a picture of atelectasis on CT and x-rays, in 35% it develops in the peripheral bronchi and looks like a solid single node, often with a decay cavity in the center, similar to an abscess.
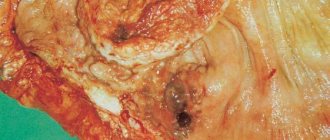
The patient was diagnosed with a cancerous node in the 6th segment of the lower lobe on the left. After resection, squamous cell lung cancer was verified by histological examination. Tomography in this case did not give a typical picture of a malignant neoplasm.
3) Small cell cancer is the most aggressive and most dangerous type; already in the early stages it can metastasize to the lymph nodes of the roots of the lungs and mediastinum. The life expectancy of patients with such neoplasms varies depending on the stage (TNM) and the possibility of surgical treatment. Frequency of occurrence up to 20%. It usually arises from the epithelium of large bronchi and causes a picture of atelectasis. Closely related to smoking.
4) Large cell undifferentiated cancer - rare, less than 5% of cases. It is usually presented by one solid peripheral node of large size. Almost always occurs in smokers. It metastasizes early - hematogenously and lymphogenously, the prognosis for it is unfavorable.
5) Large cell neuroendocrine cancer (carcinoid) - often central, with a characteristic feature - disintegration in the tumor, occurs in less than 5% of cases, metastasizes early to the lymph nodes, is aggressive, and has an unfavorable course.
6) Bronchiolo-alveolar cancer – up to 2%. It is a subtype of adenocarcinoma. Almost always peripheral. It manifests itself as a diffuse decrease in the density of the pulmonary parenchyma of the “ground glass” type, which simulates the picture of pneumonia. It also manifests itself as changes in the type of consolidation - diffuse compaction of the pulmonary parenchyma, which may look like a node. The prognosis for small node sizes is usually favorable.
WHAT DOES LUNG CANCER LOOK LIKE ON COMPUTED TOMOGRAPHY?
There are several options for the growth of a tumor node (according to Rosenstrauch):
1) Into the lumen of the bronchus on one side, narrowing it - endophytic type.
2) Into the lumen of the bronchus, circularly narrowing it - this is also an endophytic type.
3) Into the lumen of the bronchus and outwards from it - a mixed type of growth.
4) Along the wall of the bronchus, without narrowing its lumen - peribronchial type.
When a tumor grows into the lumen of the bronchus, it narrows, which leads to a violation of the ventilation of a certain area of the lung tissue. With a CT scan, you can directly notice the tumor node itself in the lumen of the bronchus - it looks dense (white). The lumen of the bronchus is narrowed in a circle, parietally, or “breaks off” at the border with the neoplasm. You can also see an increase in the density of the corresponding lobe (or segment, segments) ventilated by this bronchus. An increase in density can be caused by atelectasis - collapse of a section of lung tissue as a result of obstruction of the bronchial tube, distelectasis - partial collapse, as well as changes caused by pneumonia, most often of a stagnant nature, with abscess formation, as well as pneumofibrosis.
Get a CT scan of the lungs in St. Petersburg
There is also a division of lung cancer into peripheral and central - the classification of the latter is given above. Central cancer is clinically more severe due to the fact that it often gives complications in the form of atelectasis, massive pneumonia, abscess formation, and respiratory failure.
CT signs of central lung cancer: computed tomography reveals a volumetric formation of the soft tissue structure, in which the lumen of the lower lobe bronchus “breaks off”. The edges of the formation are tuberous, uneven, with spicules, and the shape is irregular.
Central lung cancer on CT. Note the differences in the width of the lumen of the central bronchi on the right and left. The lumen of the right upper lobe bronchus is not visible. Atelectasis of the upper lobe is visible. In the circle is the tumor itself, which caused atelectasis.
Peripheral lung cancer on CT looks like a focus or node located on the periphery of the organ far from the root. It usually has a homogeneous structure, in some cases with areas of necrosis, calcifications and hemorrhages into the parenchyma. The edges of a typical cancerous tumor are uneven, with multiple “spicules” due to lymphangitis. When located near the pleura, the formation deforms it and pulls it towards itself. Its dimensions vary - from the focus (3-10 mm) to the node (10-50 mm and more).
Typical peripheral lung cancer (adenocarcinoma) on MSCT. On the right, in the 6th segment of the lung, a dense soft tissue node with spicules was identified, deforming and pulling the interlobar pleura towards itself.
Much less common is primary multiple cancer, which must be differentiated from metastases and other diffuse and disseminated foci, including tuberculosis. There are also diffuse forms of tumors - bronchiolo-alveolar cancer (BAR), manifested on CT in the form of a total or subtotal decrease in pneumatization like “ground glass” - they need to be differentiated from pneumonia, pulmonary edema.
STAGES OF LUN CANCER ACCORDING TO TNM AND MOUNTAIN
Staging of lung cancer is necessary to determine whether the tumor can be removed.
At stages T1 and T2 according to Mountain, surgery is possible. Stage T3a means that the tumor may be resectionable (most often a pneumonectomy is necessary); stages T3b and T4 mean that it cannot be removed surgically.
In the absence of metastases to regional lymph nodes or in the presence of altered lymph nodes only on the affected side (TN0 and N1, respectively), surgical treatment is possible and the prognosis is most likely favorable. At stage N2, surgical treatment is possible after radiation and (or) chemotherapy; the prognosis is questionable. For N3, surgical treatment is not indicated. Detection of metastases to distant organs also significantly worsens the prognosis.
The table shows the classification of lung cancer according to the TNM scale (UICC, 1999).
| Stage ( TNM) | Criteria |
| T1 | A tumor node in the lung parenchyma up to 3 cm in largest size without signs of growth into the wall of the central bronchi. |
| T2 | An intrapulmonary tumor larger than 3 cm or a tumor infiltrating the wall of the main bronchus at least 2 cm below the bifurcation zone or a tumor growing into the visceral pleura. Atelectasis of a lobe or segment, but not total. |
| T3 | A tumor of any size infiltrating the main or intermediate bronchus less than 2 cm from the bifurcation or growing limitedly into the mediastinal pleura, mediastinum, or chest wall. Total atelectasis or obstructive pneumonia may be detected. |
| T4 | Tumor of any size with invasion into the mediastinum, pericardium, aorta, superior vena cava, brachiocephalic vein, bones, chest wall. Effusion into the chest cavity. Satellite foci (intrapulmonary metastases). |
| N0 | There is no damage to regional lymph nodes. |
| N1 | Damage to the root lymph nodes, bronchopulmonary lymph nodes on the side of the tumor. |
| N2 | Damage to the bifurcation, paratracheal, paraesophageal, para-aortic lymph nodes of the mediastinum on the side of the tumor. |
| N3 | Damage to the lymph nodes of the root, mediastinum on the side opposite to the tumor; damage to the axillary, sub- and supraclavicular, scalene lymph nodes. |
| M0 | There are no distant metastases. |
| M1 | Distant metastases (including intrapulmonary foci) were detected. |
An example of stage 4 lung cancer. Surgery is not indicated, only chemotherapy. Invasion occurs into the ribs and spine, as well as into the soft tissue of the chest wall. In the stroma of the tumor, multiple hypodense (dark) areas containing gas are visible - zones of decay.
CAN WE CURE LUNG CANCER?
Can lung cancer be cured? Yes, but only if detected early at stages T1 and T2. Unfortunately, the further the tumor is located from the large bronchi, the longer the time it can remain undetected, especially if the patient “forgets” about timely fluorographic examinations.
CT CT FOR LUNG CANCER AND SECOND OPINION
An important stage in the diagnosis of pulmonary oncological diseases is the analysis of CT results with the accurate identification of all signs that influence the staging of the tumor and the choice of surgical tactics. Given the high cost of error, such testing should be performed by a professional radiologist who specializes in diagnosing pulmonary diseases. Unfortunately, sometimes the interpretation of CT results is not at the proper level. In this case, the CT results recorded on a CD can be sent for review to a more experienced specialist and a Second Opinion can be obtained. In our country, any patient faced with the need to review the results of a computed tomography scan can turn to Second Opinion services, for example, the National Teleradiological Network.
Vasily Vishnyakov, radiologist
Read more about Second Opinion
Read more about telemedicine
Pavel Popov
Candidate of Medical Sciences, Member of the European Society of Radiologists
In what cases is radiography necessary?
In addition to preventive examinations, which should be carried out annually, X-rays of the lungs are prescribed if a disease of the organ is suspected. Various symptoms may alert the doctor.
These may be patients with the following symptoms:
- prolonged untreatable cough;
- prolonged low-grade fever (increase in body temperature 37-38C);
- profuse sweating at night;
- fever of unknown cause;
- copious sputum, sputum with blood;
- feeling of lack of air at rest, blue skin;
- receiving a chest injury the day before.
If necessary, after the initial examination, a repeat X-ray examination of the lungs may be prescribed, which will clarify or confirm the diagnosis.
Indications for the use of chest radiography
Suspicious symptoms associated with pathologies and diseases of the respiratory system, which require an X-ray of the lungs:
- fever;
- dyspnea;
- discharge of purulent sputum;
- persistent cough;
- confused, heavy breathing;
- accumulation of fluid in the space between the lungs and chest wall (pleural effusion);
- pneumonia;
- difficulty moving or lack of movement of the diaphragm due to lung disease or injury;
- difficulty moving air in the lungs (loss of elasticity of the lungs);
- emphysema;
- blockage (obstruction) of the bronchi;
- diagnosing injuries resulting from an accident (for example, broken ribs);
- control of disease progression (for example, cystic fibrosis);
- pneumothorax;
- heart failure;
- chest pain of unknown etiology.
How do you get pictures?
The special room is equipped with the necessary X-ray machines and is protected by anti-radiation screens that cope with radiation exposure. The patient enters the room only at the invitation of the radiologist. Before the procedure, any jewelry from the chest and neck is removed, and long hair must be pulled back into a ponytail. It is advisable to turn off your mobile phone.
X-ray of the lungs is usually performed according to the following scheme:
- The patient removes all clothing from the upper half of the body, exposing the chest.
- The reproductive organs and abdominal area are covered with a special protective apron.
- The patient is placed next to the beam tube and receiving device.
- At the doctor’s command, any movements are prohibited and breathing is held for a few seconds.
After the X-ray of the lungs, the protective apron is removed and the patient can get dressed.
Old type devices require some time to develop the image, and the result can only be obtained after a few days. Modern digital technology allows you to get an image instantly. With the image on the x-ray, the patient returns to the attending physician.
A standard x-ray of the lungs, the procedure is painless and takes a short amount of time. If there were no special instructions from the attending physician, the patient does not need specific preparation.
The difference between X-ray of the lungs and fluorography
The difference between X-ray of the lungs and fluorography is shown in the table.
| Key Features | X-ray | Fluorography |
| X-rays are directed through the patient's body to a special detector. | Yes | Yes |
| Photo research quality | High | Low |
| Preliminary preparation required | No | No |
| Impact on the human body | High | Low |
| The procedure does not take much time | Yes | Yes |
| What is it prescribed for? | To detect diseases | For screening |
It is not always possible to make an accurate diagnosis using a fluorogram due to the low quality of the study compared to x-ray data.
You can find out why you need to do radiography and fluorography, as well as what the difference between these procedures is from the video. Filmed by the Ilya Kr channel.
How often can a chest X-ray be performed?
According to current WHO recommendations, the maximum radiation dose per year should be within 1 m3v (1 millisieverts per hour [mSv/hour] = 0.1 roentgens per hour [R/h]). Indicators that are safe for health have not been determined, and the feasibility of research is determined by the doctor individually.
For prevention, adults are advised to have an X-ray of their lungs at least once every two years. There is also a certain “risk group” in which the frequency of examinations increases to twice a year. The shelf life of data on an x-ray is 6-12 months.
We recommend reading! Follow the link: MSCT of the chest organs
A current photograph is often requested from:
- living with pregnant women and newborn children;
- undergoing a medical examination when applying for a job,
- persons with chronic lung diseases;
- military personnel;
- medical staff;
- dispensary patients of narcology and psychiatry;
- patients with HIV infection;
- refugees and citizens without a fixed place of residence.
Sometimes a doctor needs to refer a patient unscheduled if he suspects:
- diseases of an infectious nature (pulmonary tuberculosis, sarcoidosis);
- inflammation in the bronchopulmonary system (pneumonia, pleurisy);
- oncopathology and mediastinum;
- pathologies of the heart and large vessels (chronic heart failure, PE);
- chest injuries.
If there are contraindications, doctors try to choose more gentle and safe methods to assess the pulmonary pattern.
Diagnosis of respiratory pathology
The condition of the lungs can be assessed in different ways: x-ray, tomography, radionuclide study, endoscopy, ultrasound, surgery (diagnostic thoracotomy). However, X-ray diagnostics are most widely used:
- Fluorography is a screening method for detecting lung pathology in the early stages, primarily tuberculosis and cancer. The study is carried out once a year for all categories of the population, with the exception of children under 14 years of age and pregnant women.
Fluorography room
- X-ray - obtaining an image of the chest organs in various projections: main - straight and lateral in a standing position, additional - posterior lying on the back, laterography lying on the side, anterior and posterior oblique. The lungs are clearly visible without contrast injection. The latter is used to visualize certain structures: vessels, bronchi, pleural cavity, mediastinum.
- Linear tomography – obtaining a layer-by-layer image of the thoracic cavity organs in longitudinal sections. The study is performed using a conventional X-ray machine. Unlike an x-ray, the method allows a more detailed examination of pathological formations and organs in the slice plane.
- Computed tomography is a highly informative method for diagnosing lung pathology. It is based on obtaining a layer-by-layer cross-sectional image of organs. Contrast when performing CT is used to study the vessels of the pulmonary circulation, as well as to assess the condition of the lymph nodes and the extent of cancer.
- Radionuclide research – registration of radiation from a radiopharmaceutical. Radionuclides are administered intravenously or inhaled as part of the breathing mixture. This study allows you to evaluate respiratory function and blood flow in the pulmonary circulation.
Radiation methods for diagnosing lung cancer
Thus, X-ray is not the only research method for lung cancer. It is often complemented by other diagnostic procedures, primarily CT. Among the methods not related to radiation, endoscopy is of greatest importance: bronchoscopy, thoracoscopy, mediastinoscopy. The role of ultrasound and MRI in the diagnosis of lung pathology is limited. Ultrasound examination is used to examine the pleural cavity, structures of the chest wall, heart and large vessels. MRI is effective in examining the roots of the lungs, pleura, and chest wall.
Lung cancer is a pathology that requires the use of several diagnostic methods, among which x-ray is used at the initial stage, but it is not enough to confirm the diagnosis.
Why can't you take an x-ray?
Despite the fact that an X-ray examination of the lungs is often the only way to assess the condition of the organ, in some cases patients will have to refuse the examination. Even minimal exposure to X-rays poses a danger to some categories of the population.
Clear contraindications include:
- childhood;
- serious condition of the patient;
- pregnancy;
- pulmonary pleural bleeding;
- lactation period;
- open wounds on the chest;
- open type pneumothorax.
Obtaining an image of the lung fields during a study using contrast solutions is undesirable in case of thyroid diseases or diabetes mellitus. A clear contraindication is also pulmonary tuberculosis in the active stage.
The norm in photographs in two projections
The norm in photographs in two projections is characterized by the following indicators:
- the width of the chest on a direct radiograph is twice as large as the transverse size of the heart;
- pulmonary fields are symmetrical on both sides;
- the spinous processes are located evenly in the vertical plane;
- intercostal spaces are uniform.
Deviation from normal values in photographs of the lungs in two projections during pneumonia is the presence of additional intense shadows on the frontal and lateral radiographs.
Venous congestion in the lesser circle will be characterized by a special shape of the roots, which in the image resembles “butterfly wings”. With edema, flaky, uneven darkening will appear in the lung tissue.
Changes in the heart on direct and lateral x-rays
Changes in the heart on x-rays of the lungs are combined with an enlargement of the right or left ventricles and atria. With an increase in size on the left, the roundness of the left border of the cardiac shadow will be visualized on the x-ray.
The image with expansion of the right contours of the heart will appear as an expansion of the shadow of the right ventricle. In this case, an increase in the shadow of the right ventricle is observed on the posteroanterior radiograph.
What the resulting image should look like
In appearance, an X-ray of the lungs resembles a peculiar pattern of various tones of gray, from almost white to deep black. The saturation of each shade depends mainly on the density of the tissue that “catches” a portion of the x-rays. They pass almost completely through the organ.
The image of the pulmonary fields looks like a dark-colored area of clearing. The roots of the organ, mediastinum and ribs are more dense, which is why the rays are delayed. They appear as lighter areas in the finished image. For them, doctors have the designation “shadow”.
The shadows that an X-ray of the lungs shows can be physiologically natural or represent pathological formations. For example, a healthy root of the lung looks like a clear, light “spot” with clearly defined edges. Single blurry shadows in the area of the lung fields are a sign that a disorder has begun. During diagnosis, doctors also pay attention to the degree of coloration of certain areas.
Types of radiography
Depending on the diagnosis, the doctor may prescribe one of the following types of radiography:
- overview;
- sighting.
Overview
Survey x-ray of the lungs - an x-ray in a direct projection of organs located in the chest area.
Such research allows:
- get an idea of the anatomical topography of structures;
- examine the condition of the costophrenic sinuses, heart and respiratory organs;
- assess the need for further research.
Sighting
A targeted X-ray image captures the area that includes a specific organ. With such a study, the X-ray tube is aimed precisely at the area under study, allowing a more detailed identification of the suspected pathology.
Tuberculosis on lung images
Most often, X-ray examination of the lungs is performed to identify inflammatory processes. During such pathologies, the tissues of the organ become flattened, and the disorder is clearly visible when the pulmonary fields are reflected. A number of diseases accompanied by inflammation pose a serious threat to human life.
We recommend reading! Follow the link: Why do a tuberculin test?
Pulmonary tuberculosis is one of the most common and dangerous diseases. It is clearly visualized on an x-ray. Foci of the inflammatory process are often discovered by chance, when a patient undergoes preventive fluorography.
The tuberculosis process can be local or affect the entire surface of the organ. There are several options for interaction between the pathogen and the human body. Doctors distinguish the following x-ray types:
- tuberculoma;
- primary focus;
- cavernous;
- focal;
- disseminated;
- infiltrative.
On an x-ray, a tuberculoma appears as a large single shadow. It is filled with lymph fluid and mucus, so the area looks quite dense in the picture. The primary tuberculosis focus is barely noticeable: it is visible with minimal contact of tissues and bacteria. The violation looks like a rounded fuzzy shadow, the size of which can reach 12 mm. The pulmonary pattern is disrupted due to the expansion of lymphatic vessels.
In the cavernous form, organ tissues are destroyed and noticeable cavities are formed. In the picture they look like a round focus of clearing, the walls are quite dense and reach a thickness of 1-2 mm. Focal pulmonary tuberculosis looks like numerous (from two to five) small shadows, the size of which reaches 5-6 mm. Most often they are localized in the upper segment of the lung.
An X-ray of the lungs with disseminated tuberculosis displays small shadows “scattered” over the surface of the lung fields. Fibrosis of the connective tissue septa occurs, which enhances the pulmonary pattern. Infiltrative tuberculosis on an x-ray is seen as a partial darkening of the lung fields. The infiltrate may contain areas of mineralization or decay cavities, which makes the shadow large and heterogeneous.
Decoding the result
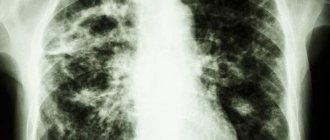
What does lung cancer look like on X-ray:
- Central cancer develops from the epithelium of large bronchi. It can grow into the lumen of the respiratory tract, towards the lung tissue, or be located around the bronchus, squeezing it from the outside. On an x-ray, the tumor appears as a shadow with an uneven contour located in the root of the lung. When the tumor spreads to surrounding tissues, rough cords resembling rays appear in the image. The disease is accompanied by external compression or closure of the lumen of a large bronchus due to the endobronchial nature of tumor growth. As a result, the airiness of part of the lung decreases, and with complete bronchial obstruction, this segment collapses (atelectasis occurs). In the picture, such an area looks like a triangular shadow with the apex facing the root of the lung. The airiness of neighboring areas increases due to compensatory hyperventilation. The mediastinum is often displaced in the direction of the pathological process. There may be elevation of the diaphragm on the affected side.
Central lung cancer on x-ray
- Peripheral cancer arises from the epithelium of small bronchi. In the photo it is visible as a shadow with radiant contours. A characteristic feature is a “path” from the tumor to the root of the lung - a manifestation of cancerous lymphangitis, inflammation of the lymphatic vessels. When the process spreads to large bronchi, their germination and compression, atelectasis and zones of increased airiness appear, as in the central form of cancer. The lymph nodes of the lung root are enlarged.
Arrows indicate the location of the tumor
- Disintegrating peripheral cancer. The tumor shadow is a cavity, sometimes with a fluid level. Unlike an abscess, the walls of such a formation are uneven, with radiant heaviness; you can find a “path” going to the root of the lung.
Radiographs of disintegrating peripheral lung cancer
- Pancoast cancer is a variant of peripheral cancer localized in the apex of the lung. In this case, there is often destruction of the posterior sections of the I-III ribs, the transverse processes of the vertebrae - lower cervical and/or upper thoracic.
Pancoast tumor
- With miliary carcinomatosis, multiple small and medium-sized shadows are found in the lungs.
- Mediastinal cancer affects the organs of the mediastinum. The main changes on the x-ray will be an increase and deformation of the median shadow. Enlargement of the lymph nodes of the lung root is often noted.
Signs of malignancy of a shadow detected on an x-ray are uneven contours, the presence of radiant strands, and a “path” to the root of the lung.
What is the basis for the research?
X-rays are similar to other forms of radiation such as light or radio waves. It has the ability to pass through most objects, including the human body. When used for diagnostic purposes, an X-ray machine produces a small beam of radiation that passes through the body and creates an image on photographic film or a special matrix for obtaining digital images.
X-rays are absorbed differently by different organs and parts of the body. Dense structures, such as bones, absorb radiation strongly, while soft tissue structures (muscles, fatty tissue and internal organs) transmit X-rays to a greater extent. As a result, on an x-ray, bone tissue appears white, air and air spaces appear black, and soft formations appear various shades of gray.
In a chest x-ray, most of the radiation is absorbed by the ribs, which appear white or light gray on the x-ray. Lung tissue absorbs X-rays weakly, and therefore the X-ray image appears dark in color.
Until recently, X-ray images were stored as copies on film, similar to photographic negatives. Nowadays, most images are available as digital files that are stored electronically. Such images are readily available and are used for comparison with the results of subsequent examinations to assess the effectiveness of treatment.
Up
Features of central and peripheral lung cancer on x-ray
There are specific features of peripheral and central lung cancer that every radiologist should know:
- Peripheral cancer quickly undergoes decay, therefore, when identifying suspicious shadows in the lung tissue, you should not hesitate, but immediately conduct a computed tomography scan.
- Cancerous nodes are most often localized in the central, cortical and median zones. About 70% of formations are located in the upper lobe. The frequency of their detection in the lower lobe is 23%.
- The lung cancer clinic is asymptomatic until the tumor grows into neighboring structures. In such a situation, not only an x-ray, but also an ultrasound will be able to determine the pathological focus in the lung tissue.
- Classic X-ray signs of peripheral cancer: a spherical formation with lumpy and unclear contours. Such radiological symptoms are caused by a formation greater than 3 cm in diameter. A small node often does not have a spherical shape, but acquires it during the process of growth.
- An important sign of peripheral cancer is unclear contours with a radiant corolla or “spikes”, which is caused by massive infiltration of surrounding tissues.
- The radial pattern of the “corolla” is gentle and differs from the rough scar cords in chronic diseases.
- When X-ray diagnosing a lung tumor, it is necessary to try to detect multinodularity, which is characteristic of cancer. The tumor consists of several small foci that merge into one conglomerate.
- Sometimes the contours of cancer can be clear, which does not exclude its malignancy.
- The intensity of the shadow is determined by the size of the node and the degree of its density. These indicators indicate the duration of the pathological process.
- The decay is manifested by enlightenment at the center of the cancerous formation. It is observed only in 30% of cases.
- Decay cavities can be multiple and single, small and large, regular and bizarre in shape.
- Rapid enlargement of the node is a sign of its malignancy.
Thus, radiological signs of lung cancer are quite numerous, but not specific enough. Radiography in frontal and lateral projections in combination with computed tomography helps to detect cancer in the lungs.
Effect of radiation on the patient
Ionizing radiation is one of the risk factors in the development of malignant neoplasms (cancer). According to regulations, a radiation dose of up to 1 MSv (millisievert) per year is considered safe, and the maximum permissible dose is 5 MSv per year.
Despite the use of modern equipment, fluoroscopy remains one of the relatively high-dose methods of radiation diagnostics. For just one such study, a patient can receive more than 1 MZv. It all depends on the medical equipment, duration of the procedure, and individual patient parameters.