How to correctly interpret lung x-rays
X-ray of healthy lungs
X-ray of the lungs is presented by photographs in two projections, which clearly show: lung tissue, ribs, collarbones, shoulder girdle, domes of the diaphragm, cardiac shadow and shadows of the mediastinal organs, vascular bundle, spinal column and sternum, which overlap each other.
To correctly interpret an x-ray, it is important to know what normal looks like on an x-ray. The lungs are an air organ.
Even slight darkening, clearing or asymmetry of the pulmonary pattern may indicate a serious pathology at an early stage of development. In this case, it is important to notice changes in time and begin the necessary treatment in a timely manner.
In the photography technique, it is important to avoid situations where the result may be distorted:
- position of the patient’s body - uneven location of the lung fields due to incorrect placement of the screen, x-ray tube or tilt of the patient, violation of the patient’s positioning (opening of the shoulder blades, moment of the respiratory act);
- additional artifacts - shadows of various jewelry (pendants and pendants, piercings, etc.), which can obscure pathological foci or disrupt the integrity of the image perception;
- completeness of the image - cutting off the apexes, fields, diaphragmatic sinuses on the radiograph due to improper placement of the screen;
- the clarity and contrast of the x-ray image is determined by the strength of the x-rays; the selection of the “Thin”, “Medium”, “Full” modes is made by the doctor. Based on the individual characteristics of a person (with greater body weight and pronounced fat deposits, it is necessary to increase the dose of X-rays for a clear image), using digital analysis it is possible to enhance or weaken the contrast.
Healthy lungs (positive image)
Healthy lungs (negative photo)
Take advantage of the consultation of our radiologists in the “Image Expansion” section
Forecast
The prognosis and life expectancy for pulmonary fibrosis depends on the disease against which it developed, the degree of progression of the fibrosis itself, its extent and the degree of involvement of the bronchial tree (meaning the formation of bronchiectasis, which aggravates the course of the disease). Among the prognostic criteria, the main one is the type of formation of pulmonary fibrosis.
Favorable types include fibrous changes in the form of cords in the central and peripheral interstitium of the lungs, as well as the atelectatic type of fibrosis. The latter is formed in places of organized pneumonia or at the site of long-term collapse of lung tissue as a result of closure of the bronchi. The occurrence of these types of pulmonary fibrosis does not affect perfusion and diffusion in the lungs and does not lead to the development of respiratory failure. Unfavorable types include changes in the form of acinar fibrosis and honeycomb lung, which always lead to impaired perfusion and severe respiratory failure. It is this factor that reduces the patient’s life expectancy.
Honeycomb lung and its significant prevalence are considered the most unfavorable prognostic sign. At the same time, importance is attached to the size of the “honeycombs” - large “honeycombs” or a mixed type of structure with alternating small and large cysts are considered more unfavorable. As for their localization, the lower zonal location is considered unfavorable.
The natural history of idiopathic fibrosis is associated with gradual changes in lung tissue and progressive fibrotic damage, which at the final stage takes on the appearance of a “honeycomb lung”. Increasing fibrosis progressively worsens the patient's condition and affects life expectancy.
It is difficult to answer the question of how long people live with this disease, since it depends on the state of pulmonary function. Terms can range from 2 to 6 years. Thus, in acute cases, patients live no more than 2 years, in subacute cases - from 2 to 4 years, and in chronic cases - from 4 to 6 years. The situation is aggravated by concomitant diseases that arise with age. Death is caused not only by the development of acute respiratory failure, but also by ischemic heart disease, pulmonary embolism or lung cancer .
With slowly progressing silicosis, the prognosis for life is positive, since the process of transition from one stage to another can last decades. There are cases when the progression of fibrosis is not detected at all - in such cases the prognosis for life is favorable. A severe complication of silicosis is spontaneous pneumothorax , but it is very rare in modern forms of silicosis. tuberculosis develops against the background of silicotic fibrosis , then the course of the disease is unfavorable and, in general, the prognosis depends on the severity of tuberculosis and silicosis, and the form of tuberculosis.
Radiograph description protocol
Any therapist can decipher an X-ray of the lungs and see gross pathology, but a detailed conclusion is provided by a radiologist, based on a special protocol.
For convenience, the protocol contains a special analysis algorithm, which includes the following points:
- the exact name of the study (the doctor indicates the anatomical area of the image, projections: direct, lateral);
- the symmetry of the pulmonary fields is assessed;
- the presence of pathological shadows (focal, infiltrative, diffuse) or clearing in the area of the lung tissue is detected;
- strengthening of the pulmonary pattern: a violation indicates pathology of the pulmonary vessels;
- condition of the roots of the lungs - there is a violation of the structure of the lymph nodes, a study of the pathology of large bronchi, the lymphatic system (lymph nodes);
- description of the shadow of the mediastinal organs (important for diagnosing heart diseases): arch of the ventricles of the heart, aorta, pulmonary artery;
- the condition of the diaphragm and pulmonary-phrenic angles (sines): the symmetry of the position of the diaphragm, the angle of the sinus, its fullness (the presence of effusion in pleurisy) is assessed.
Encapsulated exudative pleurisy
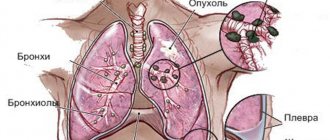
Description of the oncology image
Compaction syndrome.
Infiltrate. Cancer. Cancer on radiography or fluoroscopy looks like “plus tissue” - a pronounced darkening of an area of the lung field.
The contours are fuzzy and blurry, as the cancer grows in all directions and affects healthy tissue. The presence of rounded shadows may indicate screening out metastases.
In the second stage, local lymph nodes are affected, which looks like a violation of the structure of the root of the lungs. Lymphoid tissue increases in size and metastases form.
Severe stages of oncological pathology are accompanied by an increase in pulmonary pattern, since the tumor requires intensive blood supply and nutrition, which is why it actively grows, this can lead to the formation of signs of hypertension.
Signs of pleurisy are often observed: the appearance of a contour of the pleura (it is sclerotic under the influence of prolonged inflammation), the level of fluid in the sinuses is determined - pathological transudate.
Oncology is confirmed in the presence of symptoms of the disease: rapid loss of body weight, signs of cachexia, intoxication syndrome (fever, lethargy, weakness, fatigue, drowsiness, apathy). The disease often occurs in smokers.
Features when analyzing pulmonary fields
For the convenience of describing the localization of pathological shadows in the fields, they are usually divided into segments. In the description of the radiograph, the doctor indicates the serial number of the segment and the exact size of the formation.
Digital code
In the right lung it is customary to distinguish 10 segments, in the left, since its field is smaller due to the overlap with the cardiac shadow - 9. The principle of division into segments is based on the study of the branching of large bronchi. One segment is formed by one large bronchus.
Traditional methods of treatment
You can supplement the treatment prescribed by the doctor with folk recipes. One of the most preferred methods of treatment is inhalation of garlic vapor .
Garlic contains special components that have a detrimental effect on many pathogens. To prepare, take several large cloves of garlic, peel them and grate them. The resulting pulp is poured into a small jar and inhaled in pairs for 5-10 minutes. In this case, you need to alternately breathe through your nose and mouth. This procedure must be carried out several times a day.
To strengthen general immunity, the patient can take a mixture of aloe leaves, lemon and honey. To prepare the medicine, take 5 large aloe leaves, keep them in the refrigerator for 3-4 days, then twist them together with one lemon and add 1 glass of honey. Mix everything thoroughly and take 1 teaspoon 3 times a day.
Before using any traditional methods of treatment, you must consult a doctor!
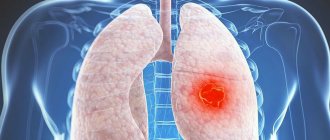
If treatment is started on time, the prognosis is good, especially if there is an inflammatory form of the disease. Oncological diseases of the lungs are initially asymptomatic, so the diagnosis may be made late . To exclude late diagnosis, you need to make it a rule to undergo fluorography once a year.
What can you see in a photo of a smoker?
Chronic obstructive pulmonary disease is the main pathology that occurs in smokers. In the picture, COPD looks like obstructive bronchitis: the pulmonary pattern is enhanced, especially in the lower sections, and there are compensatory clearings - signs of emphysema.
At the same time, the intercostal spaces expand, the diaphragm lowers, the domes are smoothed, and the costophrenic angle turns from acute to straight.
Clinically, with an increase in tissue volume, signs of hypoxia and insufficient ventilation are observed. Lung tissue loses its function.
Classification of fibrosing alveolitis
Currently, idiopathic fibrosing alveolitis is considered only one of the forms of a single spectrum of diseases united by the concept of “interstitial pneumonia”. This spectrum includes several clinical and morphological types (patterns) of the disease: idiopathic pulmonary fibrosis, nonspecific interstitial pneumonia, cryptogenic organizing pneumonia, desquamative interstitial pneumonia, respiratory bronchiolitis - idiopathic lung disease, lymphocytic interstitial pneumonia and acute interstitial pneumonitis (Hamman-Rich syndrome) . What all these conditions have in common is that they all have underlying inflammation of the pulmonary interstitium, with characteristic manifestations on computed tomography.
Inflammation or tuberculosis on x-ray
Compaction syndrome.
Low to medium density lesion. Tuberculosis. Inflammatory diseases are often differentiated from pulmonary tuberculosis. Tuberculoma is most often localized at the tops of the lung fields. The shadow is round, often with clearing in the center - the focus of destruction. Expansion of the roots of the lungs is observed.
Pneumonia or inflammation is clearly visualized on x-ray and looks like an infiltrative shadow against the background of an intensified pulmonary pattern; around the lesion there are often clearings - local compensatory emphysema.
X-ray diagnostics is the “gold standard” in the diagnosis of respiratory diseases. Due to the airiness of the lung tissue, radiography well visualizes inflammatory changes, bronchial obstruction and the growth of the pathological substrate of oncology or tuberculoma. The simplicity and low cost of the technique allows it to be used to monitor dynamics during therapy.