Diagnosis of pancreatic diseases using magnetic resonance imaging reveals functional and organic changes, the condition of surrounding tissues and organs.
With MRI, in addition to the pancreas, which is located retroperitoneally, organs and tissues of the abdominal cavity are captured to assess the distribution and involvement in the process.
Based on the data obtained, a three-dimensional image is created in specified planes with the possibility of layer-by-layer study of images of pathological formations.
Operating principle of the tomograph
The human body consists of 63% hydrogen atoms, which is part of liquids and fats.
The nuclei of the hydrogen atom (protons) create a source of magnetic field. When a person is placed in an external magnetic field under the influence of radio waves, protons oscillate and reorient.
At the end of the effect, the protons return to their original state and emit a signal.
Based on the distribution of hydrogen atoms in different organs and tissues, the tomograph constructs a spatial image.
To visualize tissues and liquids with different physical properties, T1, T2, Stir, Tirm modes are used.
The image is obtained in three planes: longitudinal, transverse and frontal.
To obtain high-quality and clear images, MRI of the pancreas is performed on high-field devices with a power of 1.5-3 Tesla.
Diagnostic progress
Diagnosis of the pancreas using MRI takes place in a room where there is a tomograph. In some clinics, you are required to undress completely and do an MRI in a gown, which will prevent the occurrence of foreign images in the images.
The patient needs to lie down on the tomograph table, then the nurse will fix the limbs with straps. To fix the head, small pads are used. This measure is needed to eliminate involuntary movements, which during scanning will lead to the identification of blurred and unclear pictures.
If an MRI of the pancreas is performed using a contrast solution, then the nurse installs a catheter, which is connected to a machine that delivers the medicine under a specific pressure. The manipulation is performed with contrast medications, which are based on salts of the rare earth metal gadolinium.
It was found that gadolinium is not able to accumulate in cells and leaves the body through the kidney structures within 2 days. Gadolinium salts present in contrast medications help improve the quality of images obtained during the procedure. Using them, you will get a picture of formations of the smallest sizes, which would be impossible to see if contrast was not introduced.
MRI with and without contrast
The following contrast agents are most effective:
- Magnevist;
- Gadovist;
- Primovist;
- Prohens.
The drugs contain various combinations of gadolinium. Other products that have an iodine base are not suitable for MRI. These medications are manufactured to perform multislice computed tomography, which is performed on the basis of x-rays. MCT of an organ is performed if there are contraindications to the MRI procedure.
Magnetic resonance imaging is performed with 2 series of images.
- Before contrast injection.
- After administration of the drug.
The contrast disperses throughout the body in 2-3 minutes, while its accumulation is observed in the zone of the greatest intense blood flow.
The duration of the examination will depend on the type of tomograph. For example, when using a modern device, diagnostics are faster. Often the event does not last more than 40 minutes.
When performing an MRI of the pancreas, which shows manipulation in the natural position of the organ:
- homogeneous structure;
- smoothed and even contours;
- the shape is correct - it widens towards the head and narrows towards the tail.
getting results
When there is a painful phenomenon or swelling in the pancreatic gland, an MRI will show:
- heterogeneous structure;
- pancreatic tissue is swollen;
- there are foci of necrosis and inflammation;
- the organ is increased in size;
- fabrics have increased density.
Indications for examination of the pancreas
The diagnostic accuracy of MRI when examining organs of the peritoneal cavity and retroperitoneal space is 93.7%.
Tomography of the pancreas is prescribed in the following cases:
- constant arc-shaped pain in the upper abdomen, behind at the level of the lower rib, girdle pain;
- digestive problems: unstable stools, constipation, severe flatulence;
- inflammatory diseases of the pancreas (acute, chronic pancreatitis);
- destructive processes in the organ (pancreatic necrosis);
- stones in the ducts and parenchymal tissue of the gland;
- benign formations: cysts (teratoma, cystadenoma), lipoma, hemangioma, fibroids, neuroma;
- malignant neoplasms: adenocarcinoma, cystadenocarcinoma, pancreatoblastoma;
- developmental anomalies;
- for dynamic monitoring of the patient in the postoperative period, deciding on the technique of surgical intervention and assessing the effectiveness of therapy.
What a test can reveal
Using MRI, you can detect inflammation, cystic changes, tumors, reduction and enlargement of the organ.
Normal sizes and deviations
The most significant parameters are the length of the organ (15-22 cm) and the width of the head - from 3 to 7 cm. The body of the pancreas is approximately 1 cm smaller than the head, and the tail has an average thickness of about 2 cm. Weight in adult patients is 65-110 G.
Reduction in size (atrophy) is caused by general exhaustion of the body (starvation, tuberculosis, pituitary insufficiency), as well as age-related changes. The volume of the gland decreases by approximately 3 times due to a decrease in the number of functioning cells and their size in diabetes mellitus.
Also, wrinkling is caused by the replacement of working tissue with connective fibers as a result of chronic inflammatory processes. A peculiar type of weight loss is observed when a large amount of fat is deposited.
In the first stages of the inflammatory process, due to swelling of the iron tissue, it increases in size. It is most often associated with pancreatitis. There is a uniform increase in tissue volume. With a tumor, cysts, blockage of the duct with a stone or local suppuration, predominantly the affected part becomes larger than normal, the organ loses its normal structure.
Cysts
They are cavities filled with liquid. Appear as a result:
- injuries, hemorrhages;
- acute, chronic inflammation;
- disturbances in the outflow of pancreatic juice due to blockage of the duct.
Using MRI, you can clearly detect the shell of the cyst, its contents, and distinguish the fluid from the disintegrated tissue. With malignant degeneration, there is pronounced heterogeneity inside, and the shell loses its clarity. When suppuration occurs, the signal becomes uneven.
Diffuse changes
Normally, the structure of the tissue is homogeneous; with inflammation, there is an alternation of areas with different densities throughout the gland. In this case, cysts appear as foci with low signal intensity, and calcium deposits, small ulcers and areas of connective tissue growth appear denser.
Such heterogeneous areas are randomly scattered throughout the organ; there is no pattern in their location, unlike a tumor.
Cancer
A malignant neoplasm is characterized by the presence of a focus with a signal of low intensity or close to the gland tissue. Its contours are uneven and unclear. There is usually dilatation of the ducts. Without contrast, MRI detects tumors as small as 2 cm, and when used, tumors up to 1 cm in size can be detected at a very early stage.
Contraindications for tomography
Diagnostics has absolute contraindications, when the method is not used under any conditions, and relative contraindications, when the study is not desirable, but the benefits outweigh the possible risks.
Absolute contraindications:
- implanted pacemaker;
- electronic hearing aids installed in the middle ear;
- metal fragments, implants;
- endoprostheses, devices for transosseous osteosynthesis;
- hemostatic clips, stents in cerebral vessels;
- internal insulin injectors (pumps);
- abdominal vena cava filters;
- obesity with a body weight of 130-150 kg.
Relative contraindications:
- uncontrolled motor activity;
- first trimester of pregnancy;
- phobia of confined spaces.
When is an MRI not recommended?
MRI of the pancreas has certain contraindications, in the presence of which such diagnosis is not recommended, namely:
- The presence of metal parts in the body, these can be staples for fastening fractures, pollinated crowns on teeth, or a metal bridge, etc.
- Autonomous devices built into the patient’s body, such as a heart rate driver.
- Availability of various metal prostheses.
- First trimester of pregnancy.
- The presence of claustrophobia, that is, fear of closed spaces.
- Body weight exceeding 150 kg, because The diagnostic table of the tomograph is designed for less load.
If there are allergic manifestations to the administration of a contrast agent, an MRI of the pancreas can be performed without this, but the effectiveness of the examination will not be as high.
If there are the above-described contraindications for MRI, experts recommend being examined using diagnostic methods such as MSCT or CT.
How to properly prepare for a pancreatic diagnosis
The examination of the pancreas is carried out on an empty stomach in the morning. Two days before the tomography, gas-forming foods (cabbage, baked goods, beans) are excluded from the diet.
For preparation, a diet consisting of liquid, non-rich soups is indicated. A cleansing enema is given the day before and on the morning of the procedure.
2 hours before the MRI, antispasmodics (Drotaverine) are taken to reduce intestinal motility.
When performing a contrast-enhanced MRI, an allergy test is performed to the substance used.
A week before the procedure, blood is donated for a biochemical study to determine the level of creatinine.
If additional diagnostic methods are available (ultrasound, X-ray), the patient must provide results that will help to create a complete picture of the disease.
How to prepare for the examination
MRI of the pancreas is usually a planned procedure and requires some preparation. The examination is scheduled for the morning, but it is advisable to arrive a little earlier than the appointed time. If the manipulation is budgetary, paid for by medical insurance, then you need to take with you a classic set of documents: passport, policy and SNILS. Refers for examination by the attending specialist if there are clear indications for MRI of the pancreas. As a rule, such a referral is given signed by the medical commission of the clinic.
Before the procedure it is recommended:
- 72 hours in advance, adhere to a diet that does not contribute to gas formation in the intestines (do not eat cabbage, bread, legumes, carbonated drinks, sweet juices);
- do not drink alcohol during the day;
- if the examination is scheduled for the morning, then you should come on an empty stomach, if at later hours, then the fasting period should be at least 5 hours;
- first remove all metal jewelry from the body, including piercings;
- Tell your doctor if you have any allergies, especially to contrast agents if they have been previously administered.
When a procedure is scheduled during a hospital stay, preparation requirements may vary. This is due to the peculiarities of the internal regulations of the institution and the capacity of the tomograph. Sometimes a cleansing enema is sometimes prescribed or the contents of the stomach are removed through a tube. The latter must be done if there is stagnation in the upper parts of the digestive system. Proper preparation provides more accurate diagnostic capabilities of magnetic resonance imaging.
How is an MRI examination performed?
Before the procedure, the patient changes into clothing that does not contain metal, removes jewelry, watches, removable dentures, and hearing aids.
The laboratory assistant helps you lie down and take the correct position on the retractable tomograph table: on your back, with your head towards the magnet.
A torso coil is placed over the upper abdomen and secured to the table to prevent artifacts during breathing.
Place a pillow under your head and a cushion under your feet. To communicate with the operator, the patient is provided with a signal bulb or button, and the ears are covered with headphones.
The table is immersed in the tunnel of the apparatus, which is equipped with lighting and ventilation. The central laser beam is focused over the xiphoid process of the sternum.
To obtain a clear image, the patient remains motionless throughout the examination.
During the scanning process, commands are received from the operator to hold your breath for 20-30 seconds.
The duration of the procedure is on average 20-30 minutes. When using a contrast agent, the examination time is doubled.
Upon completion of the diagnosis, the doctor begins to decipher the images and draw up a research protocol, the results of which the patient will receive in 1-3 hours.
Carrying out the procedure
Many people are interested in what an MRI of the pancreas shows. This type of diagnostic examination is simple to use and can identify any organ pathology.
To carry out the diagnosis, the patient needs to lie down on a special couch. After this, the device will automatically push it into the large capsule. This happens if a closed procedure is carried out. In the open form of diagnostics, a spherical tube is placed above the person, inside which a tomograph is located.
When an MRI with contrast is performed, a catheter is inserted into the person. The solution will be supplied through it. If the patient has fears of closed spaces, then open equipment is more suitable.
Being in a closed capsule, the patient and the doctor will always have a connection. The person will not have to do anything. The main thing is to lie still and not move too much. The device is noisy. To prevent the patient from experiencing discomfort, he is asked to wear special headphones.
The study lasts from 30 to 60 minutes. Some clinics allow the presence of loved ones.
Applying Contrast
If there are indications for the use of contrast agents, a catheter and infusion tubes are installed for the patient for bolus or manual administration of the drug.
The harmless paramagnetic gadolinium is used as a contrast, which is eliminated from the body within 24 hours.
Based on contrast enhancement, the doctor obtains the best visibility of the pathology and norm of the gland parenchyma, identifies tumors and metastases, intratumoral foci of necrosis, and assesses the condition of the vascular bed.
Data analysis during scanning is based on contrast phases:
- arterial - occurs 25-35 seconds from the start of drug administration, while the aorta and abdominal arteries are filled;
- pancreatic - 45 seconds, the condition of the pancreas is determined;
- venous - 55-65 seconds, the condition of the liver parenchyma and venous system is assessed;
- delayed - 3-5 minutes, metastases are detected.
Methodology
Installing a tomograph requires the presence of a specially equipped room for it. The patient lies down himself or with the help of medical personnel on a special transport table, through which he is delivered to the field of operation of the magnetic chamber.
If it is a closed device, then the patient is completely hidden inside the spherical body. If this is a closed device, then the magnetic tube is fixed above the localization area of the organ being examined.
In order to introduce a special substance, a specialist connects the patient through a vein to a device that, under a certain pressure, pumps it into the lumen of the blood vessels. Currently, contrasts are used that are based on an element such as gadolinium. These include Prohens, Gadovist, Magnevist.
In these preparations, gadolinium is presented in the form of a compound with various components. But iodine-containing contrasts are not suitable in this case. They are effective only for those examination options where X-rays are used, for example, with computed tomography.
The specialist takes two groups of images. The first group is done before the administration of a contrast agent, the second group is done against the background of its passage through the vascular bed. Based on them, it is possible to assess the accumulation of contrast in pathologically altered structures of the gland.
Important! Usually everything takes about 40-45 minutes. During this time, the patient is strictly prohibited from moving. The only thing he can do is hold his breath, following the doctor's instructions. To prevent the noise produced by the device from interfering with contact with a specialist, the patient is equipped with headphones.
Signs of the disease based on tomography
What changes in the pancreas does it reveal?
Tomography visualizes areas of pathological signal emanating from lesions in the pancreas, assesses the location, shape, distribution and relationship with surrounding structures. What the pictures show:
- shape, size, position, structure of the organ;
- the condition of the fatty tissue surrounding the gland, the presence of inflammatory infiltrate and edema in it;
- condition and patency of the gland ducts, external compression, presence of stones, intraductal formations;
- in case of tumor diseases, the boundaries of the neoplasm, areas of purulent melting and disintegration, germination into vascular structures, and metastases are revealed;
- cysts, pseudocysts, gland abscess are detected, which are differentiated from tumors;
- post-necrotic changes in the organ (destruction of parenchyma, ducts);
- traumatic injury, rupture of the pancreas.
What is magnetic resonance imaging
This diagnostic method uses such properties of the magnetic field as its uneven reflection from various structural formations in the pancreas and adjacent abdominal organs. The tomograph is designed in such a way that the patient's body is located inside a magnetic field. The magnetic signal is reflected from hydrogen atoms, which are known to be present in every cell of the body’s tissues, and is processed by special computer programs, and as a result, the doctor observes a clear and three-dimensional image of the pancreas and its smallest details on the monitor screen.
The resolution of the tomogram, that is, the clarity and detail of the image of the organ, depends on the power of the equipment. Without going into technical details, we note that proper quality images can be obtained on a device with a power of 1.5 Tesla or more. Unfortunately, not all medical institutions in the country are equipped with such equipment. Therefore, if an MRI examination of the pancreas is prescribed to a patient using a lower-power tomograph, spending money on such a procedure is completely pointless, due to the impossibility of obtaining reliable examination results due to the low power of the equipment.
The second important factor that ensures the possibility of obtaining visualization of an organ with acceptable clarity and contrast is the introduction of a special substance that enhances the echo signal and affects the contrast enhancement. Failure to use this substance when examining an inflamed organ results in unreliable diagnostic results.
Alternative diagnostic options
If it is impossible to perform MRI, additional research methods are performed.
These include computed tomography and ultrasound diagnostics. Although these methods are inferior in terms of information content to MRI, they have diagnostic value.
CT has a high contrast resolution with the ability to localize the pathological process and identify the nature of changes.
CT scanning of the pancreas is preferable for detecting calcifications, protein plugs in the ducts, diffuse and focal changes, parasitic diseases, and developmental anomalies.
Ultrasound is one of the primary methods for studying pancreatic pathology.
Ultrasound scanning diagnoses structural disorders in soft tissues, neoplasms, and the spread of a malignant process.
With the help of contrast enhancement, vascular structures of focal changes in the organ are revealed.
How dangerous is pancreatitis?
Without the pancreas, food cannot be digested. And no other organ can take over its function. With pancreatitis, the pancreas turns into a terrible monster - it begins to digest itself with the development of pancreatic necrosis (tissue death). It is not surprising that this feast during the plague leads to death. Moreover, when the pancreas ruptures, a cocktail of enzyme juices and toxins enters the blood and quickly spreads throughout the body - such patients often do not even have time to get to the hospital.
How to protect yourself from pancreatitis? Get a preventive MRI and sleep well!
Cost of the study
The price of the procedure depends on factors:
- device power (price increases when diagnosing using high-field tomographs);
- use of contrast and anesthesia according to indications (additional fee applies);
- urgency of diagnosis;
- time of day for examination (discounts apply at night);
- professionalism and category of doctor.
The average cost of an MRI is 6,000-10,000 rubles, with contrast enhancement - from 14,000-16,000 rubles.
MRI takes priority in identifying diseases of the pancreas, due to its information content and the lack of radiation exposure to the body.
The use of tomography allows you to quickly obtain a detailed picture of the pathological process and make a decision on treatment tactics.
Research results
Due to a fairly wide range of capabilities, MRI allows you to obtain information about the state of the gland and its ducts. The image makes it possible to visualize the size, shape and clarity of the contours of the gland, stones that are located in the ducts of the gland.
When examining the body and tail of the pancreas, MRI accuracy is 97%. Carcinomas are most often localized in these parts of the gland. Tumors even with a diameter of less than 2 cm are detected.
Cystic and traumatic lesions
The cyst is located in the parenchyma of the organ; this formation is limited by the walls and filled with fluid. It is formed due to traumatic injuries or inflammation of the gland. In order to determine the size, the exact location of the cyst, and whether it is connected to the ducts, an MRI is performed along with other studies.
Tumors
Modern science has proven that the most accurate information when diagnosing a gland for cancer, and the earliest detection of cancer, is provided by MRI. This diagnostic method makes it possible to most accurately visualize an oncological tumor, establish its structure and structure, determine the boundaries of cysts and soft tissues, and detect the growth of a tumor into the tissue surrounding the gland and into adjacent organs (duodenum, spleen, renal fascia, etc.).
Pancreatitis
MRI, like cholangiopancreatography, is an accurate and informative way to study abdominal pathologies.
When using it, the following indicators are assessed:
- The performance of the gland and its general condition.
- Conditions of necrosis and accumulation of fluid masses in the retroperitoneal space.
- The most accurate picture of the state of the pancreatic and biliary tract, various pathological areas.
- Presence of stones in the ducts.
Visualization on MRI of signs of changes in the acute phase of pancreatitis has the greatest effect when screening the body and tail of the pancreas. High-level information content allows MRI to be among the most frequently used diagnostic methods.
Due to the accuracy of MRI studies, it is used to make diagnoses such as:
- Autoimmune pancreatitis. It is a chronic disease and lasts more than 6 months. The image reveals a change in the size of the diseased gland with a parallel narrowing of the lumen of the excretory duct.
- For various types of chronic inflammatory processes. Computed tomography sometimes cannot detect chronic pancreatitis, but MRI is more accurate and easily identifies this type of pathology.
Diffuse changes
MRI also shows diffuse changes. Among them:
- Cystic fibrosis. In the picture, the gland tissue in cystic fibrosis is inhomogeneous, there are fibrous and degenerative foci. The diameter of the cysts varies, and calcium deposits may be present. Over time, fatty degeneration and atrophy of the gland develop.
- Hemochromatosis develops when iron deposits occur in parenchymal organs. During diagnosis, a uniform diffuse compaction of the gland is revealed; no changes are observed in the contour and size.
- Lipomatosis occurs when excess fat deposits accumulate in the parenchyma of the gland. This occurs in chronic pancreatitis, cystic fibrosis, and excess body weight (obesity). It can develop in children due to a viral infection. In the photo, the iron is small in size, has low density and clear contours.
Cost of MRI of the pancreas in Moscow
All diagnostic centers in Moscow
MRI 24 on PaveletskayaTomograph: 1.5 Tesla device
6100 rub.
European Diagnostic Center for MRI and CT on NagatinskayaTomograph: 1.5 Tesla device
5500 rub. 5500 rub.
MRI 24 on KalanchevskayaTomograph: 1.5 Tesla device
6100 rub.
The importance of the pancreas for the body is difficult to overestimate. Only this organ is capable of producing insulin and producing pancreatic juice containing digestive enzymes. Therefore, for a full life, it is so important to take care of his health in a timely manner. Often pancreatic diseases can be asymptomatic. And the pain, if there is any, will have different localization, depending on which part of the gland is inflamed. And then Magnetic resonance scanning of the pancreas comes to the rescue.
Today this is the most informative, non-invasive, safe and painless diagnostic method. It shows the thinnest sections of tissue, displays all foci of inflammation and creates a three-dimensional projection of the organ.
Acute pancreatitis. Radiation diagnostics. CT and MRI signs
ACUTE PANCREATITIS - CAUSES
Gallstones and alcohol abuse are the most common causes of acute pancreatitis (60-80% of cases). Other causes include blunt abdominal trauma, iatrogenic trauma (postoperative trauma, endoscopic retrograde cholangiopancreatography), hypertriglyceridemia, drug-induced hypercalcemia; infectious processes (eg, mumps, cytomegalovirus), congenital anomalies (pancreas divisum, choledochocele), tumor of the rectal ampullary or pancreas, vascular abnormalities (atherosclerotic emboli, hypoperfusion, vasculitis), cystic fibrosis and Reye's syndrome. These causes account for approximately 10% of cases of acute pancreatitis. In approximately 10-25% of patients, no underlying cause can be identified.
SIGNS OF ACUTE PANCREATITIS
According to the Revised Atlanta Classification, a diagnosis of acute pancreatitis requires 2 of the following 3 features:
- sharp pain in the upper abdomen, radiating to the back
- Serum lipase or amylase levels are 3 or more times higher
- Imaging findings indicate classic signs of acute pancreatitis.
There are 3 degrees of severity of acute pancreatitis: mild, moderate-severe and severe.
- Mild: no pancreatic dysfunction; local as well as systemic complications. The episode resolves within a week, mortality is rare, and imaging of the pancreas is often not required.
- Moderate-severe: characterized by the presence of short-term dysfunction of the gland, as well as systemic complications and/or short-term pancreatic insufficiency. Morbidity and mortality are higher than for mild acute pancreatitis. The episode usually lasts no more than 2-3 weeks.
- Severe: characterized by persistent impairment of pancreatic function and local as well as systemic complications. Mortality among patients with severe acute pancreatitis that develops at an early stage is higher (36-50%). The development of necrosis significantly worsens the prognosis.
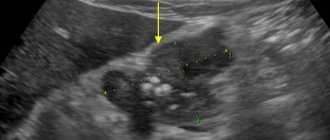
Acute pancreatitis - CT photo. Destructive pancreatitis involving the head of the pancreas. The head of the pancreas is enlarged, inflammation and exudation are detected around the gland.
Local complications of acute pancreatitis include accumulation of exudate, pseudocyst formation, abscess formation, pancreatic necrosis, hemorrhage, venous thrombosis, and pseudoaneurysm formation (see images below). A pseudocyst is a collection of pancreatic juice enclosed in a membrane of fibrous or granulation tissue. The pseudocyst has no true epithelial lining and often communicates with the pancreatic duct. A pancreatic abscess is a localized collection of pus within the abdominal cavity. It usually takes 4 or more weeks from the onset of acute pancreatitis for both pseudocysts and abscesses to develop. Pancreatic necrosis presents as focal or diffuse areas of nonviable pancreatic parenchyma; it is usually associated with necrosis of peripancreatic fat. Necrosis usually develops early in the disease.
RADIATION METHODS OF RESEARCH IN ACUTE PANCREATITIS
Contrast-enhanced computed tomography (CT angiography) is the standard imaging modality for evaluating acute pancreatitis and its complications. [9] Using non-contrast-enhanced CT, it is possible to establish the diagnosis and identify fluid accumulation, but it is not possible to detect pancreatic necrosis or vascular complications.
CT angiography allows complete visualization of the pancreas and retroperitoneum, even if it is covered by an ileum or band as a result of recent surgery. CT angiography can detect almost all of the major abdominal complications of acute pancreatitis, such as fluid collections, pseudocysts, abscesses, venous thrombosis, and pseudoaneurysms. Additionally, CT angiography can be used to perform percutaneous/endovascular procedures such as diagnostic fine needle aspiration or catheter placement. CT angiography is also possible for seriously ill patients, including intubated patients. Finally, CT angiography results can be used as a prognostic indicator of the severity of acute pancreatitis.
Get a CT scan of the pancreas in St. Petersburg
Other ancillary imaging modalities include ultrasonography (ultrasound), MRI, and angiography. Ultrasonography is especially informative in diagnosing gallstones and monitoring pseudocysts. This method can also be used to identify pancreatic pseudoaneurysms. The diagnostic performance of MRI is comparable to that of CT angiography, although MRI is more labor-intensive and expensive. Angiography is primarily used to diagnose vascular complications of acute pancreatitis.
Diagnostic fine needle aspiration is performed to distinguish infected pseudocysts from uninfected ones and to distinguish pancreatic abscess from infected necrosis. The aspirate should be immediately sent for Gram staining and subsequent aerobic, anaerobic and fungal culture. Treatment regimens for these organisms vary.
What is pancreatitis
Strictly speaking, pancreatitis means inflammation of the pancreas. But as a rule, this term is used for several dozen diseases, united by a common feature - damage to an internal organ - the gland located directly under the human stomach.
As the disease progresses, glandular tissue is replaced by connective tissue. As a result, failure develops and irreversible chronic changes in the gland are observed.
Over the past few decades, ultrasound has been widely used to diagnose the disease. But ultrasound had several significant drawbacks that affected the accuracy of the results. As a result, new methods were tried. Magnetic resonance or computed tomography can determine pancreatitis more accurately than ultrasound.