In what cases is diagnostics needed?
Ultrasound in relation to the pancreas is considered a screening method, that is, it determines risk factors for the development of a particular pathology if the patient is at risk. So such research is a mandatory measure, and on a regular basis for those whose relatives suffered from similar oncology. Diagnostics is important when tracking pathological processes and detecting metastases.
Other indications for diagnostics:
- Pancreatic diseases. Moreover, only a doctor will be able to determine what exactly the vague or, on the contrary, clear symptoms of the disease are. Diagnostics opens up opportunities for early detection of the disease and prompt treatment.
- Recurring pain in the hypochondrium, right, above.
- Symptoms of tumors and cystic neoplasms.
- Loss of body weight, both slight and dramatic.
- Jaundice develops.
- The process of bowel movement is disrupted.
- Diabetes is suspected.
- In case of injury to the gland.
Ultrasound may also be prescribed as an additional measure to confirm laboratory, x-ray and other types of diagnostics.
The main task of ultrasound is to determine primary indicators. These include the shape and size of the gland. Next, parchenima and the presence of neoplasms are necessarily checked.
Causes of tumor appearance
The causes of pancreatic tumors have not been fully determined. Therefore, it makes sense to talk about factors that increase the risk of developing the disease. These include:
- long-term chronic pancreatitis;
- hereditary diseases (cystic fibrosis, hereditary chronic pancreatitis);
- genetic predisposition - in blood relatives the risk increases by 3-18 times;
- chronic hepatitis B and carriage of the Hbs antigen;
- diabetes;
- Smoking increases the risk by 2-3 times, depending on the length of smoking and the number of cigarettes smoked per day;
- food containing large amounts of fried and smoked foods rich in carcinogenic substances;
- excessive consumption of strong coffee;
- harmful industrial carcinogenic chemicals - gasoline, benzidine, dyes, solvents, pesticides;
- lack of vitamin D3.
Hereditary chronic pancreatitis is transmitted in an autosomal dominant manner. Starts at a young age. Half of patients develop cancer by the age of sixty.
Research has found that about 30% of pancreatic cancer cases are associated with smoking. Quitting this bad habit reduces the risk of disease by 30%.
Diseases that ultrasound can detect
Using ultrasound, you can identify a number of diseases that are dangerous to human health. Moreover, diagnosis will be effective at different stages of the disease and will help to find out what impact the pathology has had on the organ.
Pancreatitis
In the acute form of this disease, it manifests itself as inflammation. It can develop as a result of injury, intoxication, or independently. The symptoms of the acute form are quite strong. Obvious signs include:
- Defecation disorder.
- Nausea and/or vomiting.
- Pain in the umbilical area and ribs on the right.
The patient's condition does not improve.
On ultrasound, such a phase will be shown as a heterogeneous echostructure of the organ, its edges will be unclear. There will be fluid areas around it, and the duct is dilated. Diffusion changes will be noticeable in the pancreas. Next, cysts will develop, they will show themselves as rounded neoplasms with liquid inside.
There is also chronic pancreatitis, discomfort in the organ occurs from time to time, but regularly. Symptoms during an exacerbation are as follows:
- After eating, aching pain occurs.
- Periodic abdominal bloating.
- Time after time, nausea occurs.
When carrying out ultrasound diagnostics, the uzist will see the contours of the organ blurrier, its structure will also be heterogeneous. There will be diffuse changes, the duct is dilated more than 2 mm. In the chronic course of the disease, stones may form. On an ultrasound it will be visible as a round spot.
Cystic neoplasm, abscess
With these pathologies, excess fluid will accumulate in the organ. An abscess also causes fluid to transform into pus. It will feel like heaviness in the stomach, pain. When pressing, the cyst can be palpated if its location is superficial. In addition to the fact that an ultrasound will clearly show a neoplasm with hyperechoic contours, changes will also be noticeable in the tissues of the organ.
Different malignant neoplasms may manifest themselves differently on ultrasound. This will largely depend on the stage of the disease and its location. There are a number of symptoms that indicate a cancerous tumor, including:
- Cancer of the head of the pancreas will manifest itself with regular nausea and vomiting, and the gallbladder will be enlarged. As a result, jaundice will develop.
- If the tumor is localized in the middle part of the pancreas, the patient will feel a dull pain almost all the time, there will be nausea and vomiting. Appetite decreases, weight decreases sharply.
- With cancer of the tail, there will be aching pain, with varying strength, which depends on the position of the patient's body. Subfrontal tumor provokes weight loss of 15% or more.
A common symptom that will manifest itself regardless of location will be pathological changes in the parenchyma, which affects the acoustic structure that the doctor sees on the monitor. The acoustic structure may vary and is often hypoechoic and heterogeneous.
An indirect indication of cancer can be an increase in pancreatic parameters in the area where the tumor is located, or a change in the diameter of the duct.
Lipomatosis
This disease manifests itself as the growth of fatty tissue. During this process the following changes occur:
- The structure of the organ becomes nodular.
- Tissues can transform into diffuse ones.
- In some cases, the tissue structure will be diffusely nodular.
Lipomatosis is considered a benign pathology, but it is irreversible. The correct functioning of the pancreas depends on how advanced the disease is. Fat cells grow when organ cells die.
Clinical symptoms do not appear immediately, but only at the second stage of development. For the most part, they manifest themselves like any gastrointestinal disease: there will be heartburn, bloating, flatulence. It is quite difficult to detect lipomatosis using ultrasound, since the size of the organ does not change, and the echogenicity is almost within normal limits.
Conclusion. Most diseases of the pancreas can be diagnosed using ultrasound. Moreover, based on the data obtained, it is possible to determine the stage of development of the disease and prescribe treatment.
Ultrasound diagnostics refers to the traditional method of identifying various formations in the peritoneum. Pancreatic cancer on ultrasound is detected as a tumor of a heterogeneous structure formed in the tissues. The disease is highly malignant. About 20% of patients live after surgery for an average of 5 years. In case of early detection of pathology, life expectancy increases by 2 years. Treatment of organ cancer is performed surgically, with the addition of radiation, hormonal and immune therapy.
How to check the pancreas for cancer
If the above symptoms appear, you should consult a doctor. A full range of examinations will help identify pancreatic cancer as early as possible.
Treatment started at an early stage increases its effectiveness and improves prognosis.
How to diagnose
Diagnosis begins with the collection of complaints and information about the dynamics of well-being. Risk factors are identified. Much attention is paid to family history. It is important for a doctor to know what illnesses close blood relatives had. Analysis of this information will suggest the hereditary nature of the disease. If necessary, genetic testing is prescribed.
The next stage is inspection. The doctor assesses the patient’s general condition, nutrition, skin color and visible mucous membranes. Body temperature is measured, lymph nodes and abdomen are palpated.
During a medical examination, signs of low nutrition, jaundice, increased temperature, swollen lymph nodes, and abdominal pain on palpation are revealed. Sometimes it is possible to palpate the enlarged pancreas. With metastases to the liver, its enlargement is detected.
The doctor prescribes the necessary tests:
- a general blood test reveals an increase in ESR;
- a biochemical study reveals an increase in alpha and gamma globulins, an increase in enzyme activity (alkaline phosphatase, GGTP, ALT, AST);
- imaging methods – ultrasound, CT, ERCP;
- aspiration biopsy of gland tissue verifies the tumor and establishes its morphological variant.
Using imaging methods, the location, size, density of the tumor, metastases, and involvement of lymph nodes, vessels, and neighboring organs are determined.
What does it look like on an ultrasound?
The following ultrasound diagnostic methods are used to diagnose pancreatic cancer:
- Transabdominal ultrasound of the abdominal organs. The classic method of examination is through the anterior abdominal wall.
- Transesophageal ultrasound. The endoscope is inserted into the esophagus through the mouth. The method is more informative and is indicated for determining the condition of the stomach, duodenum, and head of the pancreas.
- Three-dimensional reconstruction of ultrasound images in 3D mode. Small malignant foci are detected in the gland tissue. They examine the damage to the vessels that supply it. The anatomical location of the tumor in relation to nearby organs is determined.
Cancer on ultrasound looks like a space-occupying formation in the structure of the organ. It can appear in the area of the head, body or tail. Ultrasound visualizes the size, shape and density of the tumor. With cancer of the head, its enlargement is noted. It takes on a round shape. The spread of the malignant process to neighboring organs, tumor germination into nearby vessels, and the appearance of metastatic foci in the lymph nodes are detected.
Pancreatic tumors on ultrasound
Tumor markers
Tumor markers are substances secreted by malignant tumor cells. When cancer occurs, they appear in the blood. The larger the size of the tumor, the higher the level of tumor markers. Ideally, each type of cancer should have a specific tumor marker. Only in this case will the diagnosis be accurate and specific.
In addition, tumor markers are used to assess the effectiveness of treatment and detect tumor relapses.
It has been established that with pancreatic cancer in the blood the content of:
- CA 19-9 – carbohydrate antigen;
- CEA – carcinoembryonic antigen.
To check for pancreatic cancer, it is advisable to examine both tumor markers simultaneously.
Standard values for CA 19-9 do not exceed 40 IU/ml. With a malignant tumor of the pancreas, the concentration increases to 550 IU/ml or more. For distant metastases – above 1000 IU/ml.
CA 19-9 does not increase early in the disease and is therefore not useful for early cancer detection or screening.
The specificity of CA 19-9 is low, since it also increases in tumors of other organs - liver, colon, stomach.
In pancreatic cancer, CEA increases more than 10 times. However, its specificity is even lower. An increase in CEA is observed in cancer of the colon, lungs, breast, stomach, esophagus, thyroid gland, ovaries, cervix, and nasopharynx.
Oncology research centers are conducting research to find new highly specific and reliable markers. The first results are already there. Perhaps in the near future there will be methods for the early detection of this terrible disease.
Possible symptoms
Due to the peculiarities of the placement of the pancreas, which is in contact with all digestive organs and has a direct working relationship with them, the development of pronounced symptoms of the disease indicates a painful process that has already gone quite far.
The signs of a pancreatic tumor are somewhat different, it all depends on the location of the organ damage. Regardless of the location of common cancer formations, the following symptoms appear:
- pain syndrome;
- depression;
- yellowing of the skin;
- body weight is lost.
Painful discomfort sometimes does not have a clear localization, but is often detected in the epigastric region, under the left and right ribs, radiating to the back.
The area where the symptom of pain is formed depends on the area of the gland damaged by the formation:
- in blockage of the common bile duct or Wirsung canal;
- peritoneal phenomena due to exacerbation of the concomitant inflammatory process that develops in nearby tissues;
- in compression of nerve trunks.
As pancreatic tumors form, dyspeptic disorders increase.
- There is no desire to eat.
- It makes me feel nauseous.
- Belching of air appears due to bloating.
- Vomiting begins.
- Abnormal stool – diarrhea, constipation.
The main early symptom of pancreatic cancer is rapid weight loss. The victim loses a lot of weight as a result of changes in the digestive process and cancer poisoning, which is determined by the decomposition products of the formation. Atypical, rapidly dividing cells of the formation lose their activity without producing enzymes. Since the Wirsung canal or common bile duct is compressed by the expanding formation, the duodenal canal ends in entry.
- Digestive juice with enzymes and their breakdown of carbohydrates, fats, proteins.
- Bile, in the presence of which fats are broken down.
At the last stage of pancreatic disease, tumor manifestations progress and new ones appear. With cancer of the body and tail, vascular thrombosis is observed, which develops more often than cancerous damage to the head.
As cancer develops, symptoms change and may develop:
- diabetes;
- decreased glucose levels;
- pancreatic stool;
- yellowing of the skin and mucous membranes.
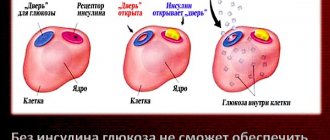
If the patient has not previously experienced diabetes, the disease affects the organ when the cancer covers the tail part of the gland. This is combined with the large distribution of the islets of Langerhans in this zone with beta cells that produce glucose, and alpha cells that synthesize the insulin antagonist - glucagon.
Due to inadequate insulin production, the formation of glycogen from glucose is disrupted, which subsequently leads to the development of diabetes mellitus.
Diabetes, a consequence of cancer, is characterized by a number of symptoms.
- Headache.
- Inability to concentrate.
- Increased fatigue.
- Increased amount of urine excreted.
- Dry mouth.
- The occurrence of hallucinations.
- Loss of mind.
- Inappropriate behavior.
- Presence of seizures.
- Development of coma.
If you have diabetes, you need to pay attention to your health and be monitored by a doctor.
Pancreatic stool is characterized by the following manifestations:
- gray color of stool;
- greasy shine;
- stinking smell;
- emptying up to several times a day.
Jaundice forms as the cancer spreads. The patient's skin, sclera, and mucous membranes turn yellow, excrement becomes discolored, urine darkens, and dilation of the bile ducts is also observed. The increase in hysteria is formed from the development of pathology. The patient complains of excruciating itching, which intensifies at night, and severe pain. These symptoms may develop in later stages when tumors grow into the hilum of the liver.
In pregnant women and children, symptomatic signs require treatment, which will be constantly monitored by a doctor. Cancer therapy requires the development of an individual regimen.
When carrying a child, treatment is selected depending on the week of pregnancy and the stage of the tumor. If cancer is detected in the thirty-first week, symptomatic therapy is carried out to eliminate pain, the main treatment is carried out after the birth of the child. Before 12 weeks of cancer detection, the woman is offered to terminate the pregnancy.
In case of cancer development, the gland needs diagnostics to confirm the diagnosis. Ultrasound examinations are prescribed. As an additional diagnosis, tests are taken for pancreatic cancer, blood and urine parameters are examined, and X-ray and other diagnostic methods are prescribed.
The main task of ultrasound is to identify primary indicators. This is the size of the pancreas, the shape. The parenchyma and the presence of cancer are then checked.
What will the study show in the case of cancer?
No specific preparation is required for ultrasound diagnostics. To better view the organ, the doctor asks you to inflate your stomach and hold your breath for a while.
If patients experience bloating, they are advised to follow a slag-free diet for 3 days before the ultrasound and drink adsorbent drugs. This is activated carbon, taken 2 pills 3 times a day. You should not have dinner before the ultrasound. The last meal takes place 7 hours before the examination.
When performing diagnostics, an ultrasound scan of the pancreas shows:
- with a single tumor localization, there is one cancer focus;
- in case of progression, a tumor of a dense structure is visible.
Basically, research is carried out not only on the glands, but also on the entire digestive system - the abdominal cavity, pelvis, soft tissues of the organ.
A type of ultrasound is Dopplerography, during which a sonologist evaluates the characteristics of blood flow using a special sensor. If tortuous vessels are detected on ultrasound, this indicates cancer.
In addition to cancer, ultrasound reveals a number of diseases.
Instrumental techniques include CT and magnetic resonance scanning. Multispectral tomography can detect metastases of pancreatic cancer. Laparoscopy is a surgical method of examination that can detect cancer in the peritoneum. During the procedure, a cancer biopsy is performed for subsequent histological analysis.
Risk factors
- Cholelithiasis
- Diabetes
- Alcoholism
- Excessive consumption of meat (animal fats contained in meat have an adverse effect)
- History of chronic pancreatitis
- Smoking
- Having either of your parents with pancreatic cancer (i.e., a hereditary risk factor)
Heredity is one of the risk factors for cancer pathologies
- Coffee abuse
- Occupational risk for industrial workers when interacting with nitrosamines and cholanthrene. As a rule, these are employees of dry cleaners and gas stations.
- Patients undergoing radiation therapy.
If you have several risk factors at once, then you should be especially careful, because the summation gives a higher percentage of the likelihood of pancreatic cancer.
Ultrasound signs
The tumor on the ultrasound machine monitor is visible as a voluminous neoplasm, having an irregular shape and uneven edges. Changes in pancreatic tissue of low echogenicity are observed. Formation of a heterogeneous structure. Difficulties often arise in differentiating a formation from a pseudotumorous form of pancreatitis, which is why a thorough examination of the pancreatic canal is required. During the disease, the main pancreatic duct appears dilated, and its diameter is uneven along its length. When there is cancer, the canal widens only below the tumor.
Also, thanks to ultrasound, it is determined whether surgery is needed. To do this, the doctor assesses the location of the cancer for vessels of significant size.
- Inferior vena cava and portal vein.
- Aorta.
- Superior mesenteric artery.
In the case of close contact with one or several vessels at a considerable distance, then surgical treatment of pancreatic cancer is impossible or there are certain difficulties in its implementation.
If cancer is suspected in an organ, an ultrasound scan looks to see if there are tumors in the liver or lymph nodes. The formations have a round shape. A clear symptom of metastasis is determined by the absence of an echo-negative border in a circle. Cancerous lesions of the lymph nodes are round neoplasms with clear contours, located near the aorta and organ.
The ultrasound conclusion is not considered a diagnosis. To confirm cancer, a CT scan is performed and a tissue sample is taken. Histological examination confirms cancer.
Pancreatic cancer can be detected by ultrasound in the early stages of the disease. But, as a rule, this does not happen: due to the mildness or absence of symptoms, patients rarely consult a doctor in the initial stages of the pathology. A pancreatic tumor is detected accidentally when a patient visits for another reason. When performing an ultrasound, not only the primary tumor is determined, but also metastases with secondary foci.
Surgical methods
Surgical examination methods are those diagnostic methods in which the integrity of the skin is disrupted. Such methods of detecting cancer are highly accurate, and it is on the basis of some of them that one can assert the malignancy of the process and the spread of metastases in the body.
Laparoscopy
Diagnostic laparoscopy is used to examine the abdominal cavity to identify metastases in it.
The instrument is inserted through a small incision on the abdominal wall, all data is displayed on a computer monitor and the doctor can assess the condition of the internal organs under high magnification. If necessary, during laparoscopy, a biopsy specimen and ascitic fluid are taken for histological examination.
Angiography
Angiography is a complex x-ray method that involves injecting a contrast agent into the femoral artery. With the blood flow, the contrast moves to the pancreas and shows a number of changes.
During the malignant process, deformations of the arteries, displacement and asymmetric narrowing of the vessels of the organ are mainly detected. If high-quality equipment is used, tumors with a diameter of less than one cm are detected.
Angiography is usually prescribed as an addition to other examination methods, in particular CT.
Methods for diagnosing pathology
To determine the malignancy of the pancreas, laboratory and functional diagnostic methods are used. The latter can be invasive (performed with violation of the integrity of the skin) and non-invasive. Ultrasound examination of the abdominal organs and retroperitoneal space (ultrasound of the abdominal cavity and retroperitoneal space, echography) is a safe diagnostic method, has no contraindications, is prescribed immediately to exclude gross pathology, is screening, and is effective in the initial and later stages of the disease. It is based on the use of ultrasonic waves.
Using this method, you can find out:
- pancreas shape;
- the size of the organ as a whole and its component parts;
- parenchyma density;
- the presence of neoplasms and their distribution within the gland and beyond its borders.
The sensitivity of ultrasound is 73.8%, the specificity is 75%, and the accuracy is 74.3%. Enlarged regional lymph nodes during ultrasound examination are detected in 30-47%, upper abdominal and retroperitoneal lymph nodes - in 78.9%, liver metastases - in 46-74% of cases.
In 30% of cases, ultrasound may not provide diagnostic results due to the patient’s:
- obesity;
- ascites;
- special topographic location of the organ.
For a more detailed study, checking ultrasound results and clarifying the diagnosis, other methods are used:
- MRI;
- CT;
- ERCP (endoscopic retrograde cholangiopancreatography);
- MRPHG;
- biopsy with further microscopic examination of tissues taken for analysis.
MRI and CT with contrast are more highly sensitive diagnostic methods. CT, compared to MRI, is a more dangerous procedure due to the high radiation dose. For MRI, which is performed in a magnetic field, there are some limitations (the presence of metal implants in the body). Using this method, tumors as small as 2 centimeters are detected.
ERCP is dangerous due to complications, so it is used less frequently.
Life expectancy
The prognosis depends on the stage of the disease. If the operation is performed in the early stages and a full course of chemotherapy is given, then about 30% survive the 5-year postoperative mark.
Unfortunately, 80-90% of patients seek help when the cancer has already spread and metastasized. In the later stages, the disease cannot be treated, and the life of patients is limited to several months.
Today, the 5-year survival rate after complex treatment is only 5-10%. On average, the prognosis for life after surgery is limited to 1.5-2 years.
Postoperative mortality is high - up to 30%.
Improving the situation comes down to solving the following problems:
- search for markers of early detection of the disease;
- increasing the availability of informative examination methods (CT, ultrasound) to detect the disease at the preclinical stage;
- dispensary observation of persons from risk groups;
- development of effective cytostatics;
- promotion of healthy lifestyles.
Symptoms of the disease
Due to the peculiarities of the location of the gland, which is in direct contact with all digestive organs, and the close functional connection with them, the appearance of pronounced clinical symptoms indicates an advanced pathological process.
The clinical manifestations of pancreatic cancer vary slightly depending on the location of the organ lesion. But regardless of the location of the tumor, the following occurs:
- pain symptom;
- dyspepsia;
- jaundice;
- weight loss.
The pain sometimes does not have a clear localization, but is most often determined in the epigastrium, left or right hypochondrium, and radiates to the back. The location where the pain symptom is determined depends on the area of the gland affected by the tumor. The cause of pain is:
- blockage of the common bile duct or Wirsung duct;
- peritoneal phenomena due to exacerbation of concomitant inflammation developing in tissues adjacent to the tumor;
- compression of nerve trunks.
As the disease progresses, dyspeptic disorders increase:
- lack of appetite;
- nausea;
- belching air due to flatulence;
- vomit;
- stool disorders - diarrhea, constipation.
An important symptom of the disease is sudden weight loss. The patient is progressively losing weight due to digestive disorders and cancer intoxication caused by tumor decay products. Atypical tumor cells that quickly divide lose their functions - they do not produce enzymes. As a result of compression of the Wirsung duct or common bile duct by the growing neoplasm, the entry into the duodenal lumen stops:
- pancreatic juice with enzymes and their breakdown of proteins, fats, carbohydrates;
- bile, in the presence of which fats are broken down.
In addition, obstructive jaundice develops - one of the main diagnostic criteria for pancreatic head cancer. Its appearance is associated with obstruction of the common bile duct or metastases that have penetrated into the gates of the liver. If the bile duct is damaged, this sign may appear in the early stages of tumor development. Bile accumulates in the lumen of the gallbladder due to compression of the common bile duct. An enlarged bladder is detected, which can be palpated due to its significant size. In addition to icterus of the skin, mucous membranes and sclera, painful skin itching appears due to the entry of bile acids into the blood and skin.
At later stages, symptoms progress and new ones appear. They are defined:
- location of the tumor;
- tumor size;
- penetration of the pathological focus into nearby and distant organs;
- the nature of the spread of metastases.
With a tumor of the body and tail of the pancreas, vascular thrombosis is detected - they develop 4 times more often than with cancer of the head. If there are large tumors in the body or tail, they can be identified by palpation. Splenomegaly may develop, which is associated with tumor metastasis to the spleen, portal vein vessels, or the formation of blood clots in them.
Early symptoms and signs of pancreatic cancer
At the beginning of its development, pancreatic cancer may be asymptomatic. Signs of the disease that appear at different stages are often ignored due to their nonspecificity: as a rule, they are mistaken for symptoms of pathology of other digestive organs.
At the beginning of the development of the disease, epigastric discomfort appears. It can be expressed by:
- unclear pain without clear localization;
- dyspepsia (nausea, sometimes vomiting, constipation or diarrhea);
- disturbance of food perceptions;
- decreased appetite.
Secondary signs of pancreatic cancer
Over time, as the disease develops, changes increase. May develop:
- diabetes;
- hypoglycemia;
- pancreatic stool;
- obstructive jaundice.
Diabetes mellitus, if the patient has not previously suffered from this disease, develops when a tumor affects the tail of the pancreas. This is due to the predominant location of the islets of Langerhans with beta cells that produce insulin and alpha cells that synthesize the insulin antagonist, glucagon. With insufficient insulin formation, the formation of glycogen from glucose is disrupted with the subsequent development of diabetes mellitus.
Glucagonoma is formed from α-cells of the pancreas; with their uncontrolled division, diabetes mellitus also develops with all its symptoms (constant dry mouth, excruciating thirst, frequent urination, further progressive damage to important organs). This occurs due to excess secretion of glucagon, which can increase blood sugar levels by breaking down glycogen found in the muscles and liver. The tumor can become malignant over time, causing it to begin to grow uncontrollably.
Hypoglycemia occurs when a tumor arises from the β-cells of the islets of Langerhans: the insulinoma begins to intensively produce insulin (insulinoma). In cases of insulinoma development, 70% are adenomas, 30% are aggressive, rapidly growing adenocarcinomas.
Pancreatic stool has a characteristic appearance: gray in color, with a greasy sheen (difficult to wash off) and a foul odor. Repeats several times a day.
As the process progresses, obstructive jaundice develops, accompanied by:
- positive Courvoisier's symptom (enlarged, painless gallbladder due to impaired bile outflow);
- icterus of the skin, sclera and mucous membranes;
- acholic (discolored) feces;
- dark urine.
As the disease progresses, icterus increases, and painful itching appears, worsening at night. At the same time, the pain becomes more intense. This can occur in later stages due to the growth of metastases into the portals of the liver.
As the size of the tumor increases, a person quickly loses weight, even with a normal amount of food eaten, due to disruption of its absorption processes.
Treatment
The most effective method is surgical removal of the tumor and metastases. However, at the time of detection of the disease, the number of operable cases is no more than 15-16%. Then patients are prescribed chemotherapy and palliative symptomatic treatment. Its tasks are:
- Reducing pain with analgesics, antispasmodics, celiac plexus blockade, palliative radiation therapy.
- Restoration of bile outflow. If conservative treatment is planned, with obstructive jaundice and an increase in total bilirubin to 250 µmol/l, bile unloading surgery is indicated.
- Restoring the patency of the duodenum by stenting or bypassing anastomoses between the stomach and the lower parts of the small intestine.
- Treatment of diabetes mellitus.
- Enzyme replacement therapy for excretory insufficiency.
In some cases, patients are prescribed radiation therapy - exposure of the tumor to low doses of ionizing radiation. New methods of radiation treatment have been proposed, for example, “cyberknife”. The method is considered as an alternative to surgical removal of the tumor. High doses of radiation are applied pointwise, directly to cancer cells. Negative side effects are kept to a minimum.
Chemotherapy
Treatment of cancer with cytostatics is used in inoperable cases or as adjuvant therapy after radical surgery. Chemicals kill cancer cells or slow their growth.
Prescribing chemotherapy after surgery increases survival and reduces the risk of relapse. Chemotherapy is often used in combination with radiation treatment.
A type of chemotherapy is targeted therapy. It involves targeted delivery of cytostatics to tumor cells. In this case, the effect of the drug on healthy tissue is excluded.
The use of cytostatics causes a decrease in tumor size. Unfortunately, the effectiveness of chemotherapy is no more than 28%.
Surgery to remove the tumor
Surgery is the only effective treatment for pancreatic cancer. The type of surgical intervention depends on the stage of the malignant process, the size of the tumor, and the involvement of neighboring organs and tissues.
- For head cancer, standard gastropancreaticoduodenal resection is performed. The head of the pancreas, part of the stomach, common bile duct, duodenum, and nearby lymph nodes are removed. An anastomosis of the pancreatic remnant with the jejunum is formed.
- If the cancer affects the body or tail, the distal parts of the gland and regional lymph nodes are removed.
- If the tumor spreads along the pancreatic duct or several tumor foci are identified in the gland, its total resection and removal of regional lymph nodes are performed. Resection of part of the blood vessels improves long-term treatment results. In some cases, the common bile duct and pyloric part of the stomach must be removed.
Tumor involvement of regional lymph nodes worsens the prognosis. If the process involves the celiac trunk, superior mesenteric and common hepatic arteries, the case is considered inoperable.
Do folk remedies help?
Folk remedies are used as auxiliaries. They improve well-being, promote bile secretion, and have a beneficial effect on digestion. In folk medicine the following are used:
- herbal infusions containing oats, sedum, fennel, centaury, wormwood;
- antitumor preparations based on forest mushrooms, the main component is the stitch mushroom.
Oncologists consider cancer treatment with herbs and mushrooms not only ineffective, but also unsafe. Instead of starting full treatment as quickly as possible, the patient tries to be treated with folk remedies. This takes days, weeks and even months. Meanwhile, the cancer progresses and becomes incurable, that is, incurable.
If suspicious symptoms are detected, you must immediately contact a medical institution and see a therapist, who, if necessary, will refer you to an oncologist.
Ultrasound signs of a pancreatic tumor
Due to the peculiarities of the topography of the pancreas and the asymptomatic course of the malignant tumor in the initial stages, the pronounced clinical picture in which the patient seeks help appears late - at the final stages of the disease, when treatment is no longer effective. Therefore, diagnostic detection of pancreatic tumors at the stage of minimal manifestations of the disease is especially important.
When performing an ultrasound, you can see a characteristic echo sign of a cancerous tumor - a significant increase in a separate part of the gland or a bulging of its contour. In 50-80% of cases, the head of the pancreas is involved in cancer. Even a small tumor is clearly visible at the head end on ultrasound. This is due to the following reasons:
- clearer visualization of the head of the gland compared to its other parts;
- relatively rapid compression of the common bile duct, accompanied by the appearance of changes in sonography in a short time.
An oncological process in the form of a small tumor in the tail is detected on ultrasound much less frequently. The presence of a neoplasm of this localization is indicated by the signs described in detail in the ultrasound transcript (its protocol). Research may show:
- impaired form of the pancreas;
- increased dimensions of the tail section.
The tumor may affect the entire pancreatic tissue - multicentric growth. The picture, which is visualized on ultrasound, resembles diffuse edema in acute pancreatitis.
With pancreatic cancer, the contours of the organ change: they become unclear, but, unlike chronic pancreatitis, they do not have irregularities or jagged edges. At the location of the tumor, bulges are visualized that penetrate into the surrounding tissue in the form of tongues. All this is described in detail in the ultrasound report.
Basically, pancreatic cancer is hypoechoic and does not contain internal echo structures. But there are tumors with diffusely defined echo signals or high-intensity echo signals in the center of the node in the absence of them at the periphery of the tumor. The border between the altered tumor and the rest of the gland tissue may be unclear, but is always approximately visible due to the difference in echogenicity of normal and pathological tissue. Despite the similarity of the tissue structure of the formation (especially if it lacks areas of structures with increased density) with a cyst, ultrasound, using the effect of distal enhancement, makes it possible to differentiate a malignant focus from a liquid formation.
Acute pancreatitis on ultrasound
Acute pancreatitis is a severe complication of gallstone disease or a consequence of toxic effects, such as alcohol.
Mild pancreatitis is not visible on ultrasound (CT is a more sensitive method). Severe pancreatitis is easily detected by ultrasound. When an unusually clear and contrasting pancreas stands out from the surrounding tissue, edema of the parenchyma and surrounding fatty tissue can be assumed. If a thin layer of free fluid is visible around the pancreas, along the stomach, at the hilum of the liver and spleen, pancreatitis can be confidently diagnosed.
| Photo. Acute pancreatitis on ultrasound: A - Swelling of the pancreatic parenchyma (p), the contour of the pancreas is unusually clear, a small accumulation of fluid along the border (arrows). B, C - Accumulation of fluid along the contour of the body of the pancreas, a thin rim of fluid along the splenic vein (arrows), the parenchyma is heterogeneous, the surrounding tissue is hyperechoic - swelling and inflammation, the common bile duct is dilated (B). In this case, gallstone disease must be excluded. | ||
Almost all pancreatic tumors are hypoechoic compared to the normal pancreas. It is impossible to distinguish between focal pancreatitis and pancreatic tumor using ultrasound alone. A tumor and pancreatitis can be combined.
| Photo. Acute pancreatitis on ultrasound: The pancreas is unusually contrasted against the background of hyperechoic surrounding tissues, a thin strip of fluid along the contour (A), a hypoechoic focus in the tail (B), fluid in the hilum of the spleen (C). A hypoechoic tail can be mistaken for a tumor. | ||
In severe cases of pancreatitis, pancreatic fluid digests surrounding tissue, forming pseudocysts. Such cysts can be single or multiple. They may increase in size and rupture.
On ultrasound, pseudocysts are defined as oval or round hypoechoic formations with clear contours. In the early phases of cyst formation, it is a semi-liquid formation and has a complex echostructure with internal reflections and unclear contours. Later, due to autolytic processes and sedimentation of a suspension from blood and pus, clear signs of liquid contents appear and a false capsule with smooth walls is formed. Infection of pseudocysts often occurs, then internal echo structures or thin delicate septa can be detected. When a cyst is detected, it is important to trace the connection of the cyst with the duct, as this is important for determining treatment tactics. When a pseudocyst is more than 10 cm in size, difficulties arise in determining its source.
| Photo. A - Large pseudocyst between the head of the pancreas and the liver after pancreatitis. B, C - Severe necrotizing pancreatitis longitudinal (B) and transverse (C) sections: extensive necrosis, melting of the surrounding fat in the tail area, accumulation of fluid around the gland. | ||
Can an ultrasound show pancreatic cancer?
In most cases, having only the results of ultrasound of the pancreas, it is difficult to unambiguously determine the presence of a tumor, its invasion into neighboring or distant organs, and also to differentiate small-sized (up to 3 cm) cancer tumors from areas of local inflammation of the pancreas. According to published research data from some authors, the sensitivity of ultrasound for detecting pancreatic tumors is more than 90%. Other works provide the following values for diagnosing pancreatic cancer:
- Ultrasound – 84%;
- CT – 88%;
- consistent use of ultrasound and CT – 97%.
In the presence of a tumor in the head of the pancreas, data from the dilated Wirsung duct are analyzed: with cancer, smooth and non-compacted walls are revealed, in contrast to their changes in chronic pancreatitis. If the diameter of the main excretory duct is equal to approximately half the thickness of the pancreas itself, this is one of the signs of a malignant process.
Dilatation of the common bile duct and smaller intrahepatic ducts is possible.
The expansion of the common pancreatic and Wirsung canals also occurs in the presence of a formation that compresses them in the circumference of the duodenal papilla of Vater.
Ultrasound can diagnose compression and displacement of nearby vessels - the inferior vena cava and mesenteric vein. This is observed both in chronic pancreatitis and in tumors, but in the case of a malignant tumor it is more pronounced. When the tumor is localized in the head of the pancreas, the superior mesenteric vein shifts in the ventral direction, and when the node reaches a large size, the head itself shifts.
Examination algorithm using ultrasound
Based on ultrasound data, a general examination algorithm has been created for accurate diagnosis of pancreatic cancer:
- transcutaneous research in B-mode in real time - used to detect tumors and is a screening method with which the examination of the patient begins;
- color Doppler scanning or ultrasound in B-mode using CO2 as contrast - for differential diagnosis of malignancy and inflammation of the pancreas;
- color Doppler scanning in the color Doppler mapping (CDC) or EDC (power Doppler mapping) mode - establishes the relationship of the tumor with nearby vessels.
Transcutaneous B-mode imaging
Transcutaneous ultrasound in B-mode is the most common method for studying parenchymal organs. Provides a two-dimensional, two-color image of the organ being studied on the screen. Allows you to see:
It is one of the screening methods for pancreatic pathology.
Real-time B-mode ultrasound for pancreatic cancer is based on detecting direct and indirect signs of the disease. Direct signs are the identification of a single focus or cavity with a clear boundary of heterogeneous density between the tumor and normal tissue. Changes in the parenchyma of the pancreas are the main sign of an existing neoplasm; they are observed with ultrasound in 80% of cases. Based on the intensity of signal reflection, a tumor (its echogenicity) can be:
- hypoechoic;
- hyperechoic;
- isoechoic;
- mixed.
Indirect signs are:
- expansion of the common bile duct and pancreatic duct (more than 3 mm);
- a significant increase in the size of the pancreas in the area of the neoplasm.
Dilatation of the bile ducts in the liver is possible in the presence of a tumor in the head of the pancreas or lymph nodes in the area of the hepatoduodenal ligament.
Depending on the size of the formation, the size of the gland may be unchanged or locally or diffusely increased.
Color Doppler scanning
To diagnose pancreatic cancer, a method with the Doppler effect, named after the Austrian physicist who discovered it, is used. In this case, a color image of the reflected ultrasonic signal is obtained. Unlike conventional ultrasound, this method is based on the reflection of ultrasound by moving objects, for example, blood cells in the vascular bed - red blood cells. Due to the changing frequency of the signal reflected from them, vascular pathologies are identified, the differences between benign neoplasms and malignant tumors are determined, and the following is assessed:
- speed;
- direction of flow;
- blockage of blood vessels;
- collaterals.
This procedure has no contraindications, no side effects are observed, the patient is not exposed to radiation - it is absolutely safe. With the help of color flow, a color image of the blood flow is displayed, any circulatory disorders in the organ are visible.
Color Doppler scanning using Color Doppler or EDC modes
An additional method for the differential diagnosis of a malignant process and inflammatory changes in the pancreatic parenchyma is the use of color Doppler examination in the Color Doppler and EDC modes.
When using the methods, it is determined:
- presence and patency of blood vessels;
- the nature and speed of blood circulation in them.
If pancreatic cancer is suspected in a patient during duplex scanning, the following is noted:
- absence or sharp decrease in blood flow through the vessels inside the tumor;
- the presence of collateral vascular networks with arterial blood flow.
EDC is essentially a more advanced color Doppler mapping. Its difference from Color Doppler, in which the color-coded frequency shift of the Doppler signal is visualized on the screen, lies in the display of numerous signals from moving objects (red blood cells) - this method maps the energy characteristics of the signals.
What other pathologies can be detected using ultrasound?
It is necessary to differentiate the echographic image of cancer from diseases of the pancreas or other organs of the digestive system, which may give a similar clinical or ultrasound picture. They can be suspected or detected during sonography:
- local forms of pancreatitis;
- cancer of the major duodenal papilla;
- pseudocysts;
- lymphoma;
- metastases.
It is tactically important to take into account clinical and laboratory data in combination with biopsy results.