Ultrasound of the ovaries in women is one of the mandatory methods for diagnosing diseases and pathologies of the reproductive organs. Everyone knows that the ovaries are small glands located in the pelvic area. Their main purpose is to produce a hormone responsible for a woman’s reproductive health.
There are quite a few ways to determine the shape, size and presence of a pathological process occurring in the ovaries, but the most popular is ultrasound diagnostics.
Description
Ultrasound examination is one of the most informative types of diagnostics. Ultrasound allows you to assess the condition of the ovaries, their functionality, and possible pathologies. The procedure is carried out during population screening, routine medical examinations and when gynecological diseases are suspected.
A woman is examined with a sensor emitting ultrasonic waves in a hospital setting. During the procedure, the doctor determines the condition of the organs from the image obtained on the monitor screen. Using an ultrasound machine, measurements of all sizes and examination of individual tissue areas are taken. If necessary, the image is enlarged. The average time for an ultrasound is up to 15-20 minutes.
Why do you need an ultrasound scan of the ovaries?
The ovaries are sex glands that perform many different functions in the female body. They are responsible for puberty, sexual activity, and reproductive health. They also maintain a regular menstrual cycle and affect the general condition of women’s bodies.
Ultrasound examination is the best way to determine the condition of these organs and determine their performance. Using ultrasound you can determine:
- size and shape of the female reproductive glands;
- clarity and evenness of their contours;
- state of the follicular apparatus (number of ripening follicles).
The state of the female ovaries constantly changes during the monthly cycle - follicles mature, one becomes dominant, ovulation occurs (egg release), and the corpus luteum develops. All these processes can be clearly seen using ultrasound. This allows you to assess the condition of the reproductive system and timely recognize any pathologies of the gonads.
Indications for ultrasound of the ovaries in women
An examination is indicated for suspected infertility or lack of conception. To do this, you should check the ovaries and uterus. The latter are initially examined completely; later, if pathologies are detected or functions need to be monitored, only the affected organs are subject to examination.
To obtain complete information about a woman’s reproductive health, she should additionally undergo blood tests for hormonal levels, vaginal smears for microflora and infections.
Indications for ultrasound of the ovaries in women:
- suspicion of infertility;
- irregular menstrual cycle;
- lack of conception for more than a year with regular unprotected sexual intercourse;
- heavy or scanty menstruation;
- pain in the lower abdomen;
- diseases of the mammary glands;
- hormonal imbalance;
- routine gynecological examination.
Regular consultations with a gynecologist will ensure timely detection of diseases of the ovaries and other genital organs. Early treatment is highly likely to preserve a woman’s reproductive function. Pathologies are often diagnosed in their final stages - this is due to the frequent asymptomatic course of diseases of the appendages.
Transvaginal ultrasound and color Doppler ultrasound for ovarian tumors
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
A number of physiological and pathological processes occurring in the ovaries are accompanied by an increase in their size: maturation of the follicle, the appearance of various cysts, the presence of endometriosis, inflammatory processes, benign and malignant tumors. In most cases, patients require surgical treatment. Clarification of the diagnosis before surgery is necessary to determine the scope of surgical intervention, the nature of preoperative preparation and the necessary qualifications of the surgeon.
Cysts represent the most common volumetric pathology of the ovaries and are retention formations that arise as a result of excessive accumulation of tissue fluid in the previous cavities. The development of cysts is observed mainly during reproductive age. In most cases, these are functional formations, the size of which does not exceed 4-5 cm. In the postmenopausal period, cysts occur in 15-17% of patients.
Tumors originating from the surface epithelium account for about 70% of all ovarian tumors. Among them, benign variants (serous and pseudomucinous) occur in 80% of patients. Benign ovarian tumors (excluding hormone-producing ones), regardless of their structure, have much in common in their clinical manifestations. The early stages of the disease are asymptomatic and even when the first symptoms appear, patients often do not consult a doctor, or the doctor does not recommend surgical treatment, preferring dynamic observation. Malignant ovarian tumors are detected in 20% of all neoplasms of the female reproductive system.
The most common complaint of patients with ovarian tumors is dull, aching pain in the lower abdomen, sometimes in the groin areas. Acute pain occurs only with torsion of the tumor stalk and with hemorrhages in cases of capsule rupture. As a rule, pain is not associated with menstruation. They arise as a result of irritation or inflammation of the serous membranes, spasms of the smooth muscles of the genital organs and as a result of circulatory disorders in certain organs. The second most common complaint is menstrual irregularities such as dysmenorrhea, oligomenorrhea or hyperpolymenorrhea.
Early diagnosis of ovarian cancer is one of the main problems in gynecological oncology. Despite the variety of diagnostic methods used, about 80% of patients are admitted to specialized hospitals with advanced stages of the disease. This is determined by the peculiarities of the clinical course of ovarian cancer: the absence of symptoms of the disease in the early stages, late seeking medical help, as well as the lack of oncological alertness among general practitioners, therapists, and antenatal clinic doctors.
For several decades, ultrasound diagnostics has been successfully used to differentiate tumors of the uterus and appendages. A comparison of echography data and morphological examination indicates a high accuracy in identifying tumor-like formations of the ovaries and determining their internal structure. However, in a number of cases of benign neoplasms of the appendages, especially in pre- and postmenopausal patients, transvaginal echography does not allow differentiating the nature of tumor growth. The possibility of differentiating benign and malignant ovarian formations using color Doppler mapping (CDC) is a promising direction in ultrasound diagnostics.
The main achievement of CDK in the diagnosis of tumor processes is the visualization and assessment of the blood flow of newly formed tumor vessels, which have their own characteristic features. The tumor vascularization system is represented by many small, very thin vessels, abnormal in shape and location, randomly scattered within the tumor tissue. The blood flow in these vessels is characterized by extremely low vascular resistance, high speed and varied direction. The peculiarities of blood flow are due to the transformation of blood vessels into wide capillaries or sinusoids, devoid of smooth muscle, the presence of precapillary drainages and multiple arteriovenous anastomoses with very low vascular resistance, which provide high kinetic energy of blood flow and wide variability in its direction. As a result of numerous studies by J. Folkman, it was revealed that the described type of blood circulation is a feature of primary malignant tumors of the uterus and ovaries, which confirms the hypothesis that all fast-growing malignant neoplasms produce their own vessels to ensure further growth.
Blood flow in benign tumors has a different character. The vessels involved in the vascularization of benign formations of the uterus and ovaries are a direct continuation of the terminal branches of the uterine and ovarian arteries. Doppler characteristics of blood flow in these vessels are the constant presence of a low diastolic component, low velocity and high values of the resistance index. According to most authors, peripheral, with single vessels, tumor vascularization should be associated with benignity, and the presence of multiple vessels in the central part, on the septa and in papillary growths is a sign of malignancy.
Due to the commonality of echographic manifestations, two types of intratumoral blood flow have been identified
- in 41.7% of patients, variously expressed peripheral blood flow
of ovarian formations with an average level of resistance in the vessels was registered; - In 58.3% of patients, neovascularization
of the ovarian tumor was detected: intense central and peripheral intratumoral blood flow with a low level of peripheral resistance of newly formed vessels.
Peripheral intratumoral blood flow with an average level of vascular resistance is observed in various types of cysts and in serous cystomas.
With borderline cystomas and malignant transformation of the ovaries, neovascularization is recorded: intense central and peripheral intratumoral blood flow with low resistance index values in newly formed vessels.
Patients with peripheral intratumoral blood flow
In patients with ovarian cysts and cystomas, the most common complaint is pain in the lower abdomen, as well as in the lower back, sometimes in the groin areas. The pain was not associated with menstruation and was dull, aching in nature. Irregular menstrual cycles are observed in 31.3% of patients. Chronic inflammatory processes of the uterus and appendages are observed in 43.8% of patients.
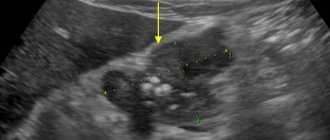
With transvaginal echography of cysts, true tumors are visualized as single-chamber thin-walled formations of a round shape, located in the lateral sections of the small pelvis, with an acoustic effect of distal amplification. The internal and external contours of the formations are smooth, the contents are homogeneous and echo-negative. The size of the cysts is 4-9 cm.
In a patient with a paraovarian cyst, the ovary is visualized on the side of the tumor-like formation.
Color Doppler sonography records single color signals from vessels located in the capsule of the formation with an average level of resistance index (IR min = 0.57+0.09 and 0.54+0.09).
In patients with endometrioid cysts, a characteristic symptom is progressive pain, especially pronounced in the premenstrual period and during menstruation. In most patients, pain is accompanied by symptoms of peritoneal irritation due to microperforation of cysts and spillage of their contents into the abdominal cavity. The cysts are located on the side and behind the uterus; due to the pronounced adhesive process, they formed a single conglomerate with the uterus. The size of endometrioid cysts varies depending on the phase of the menstrual cycle and is 6-8 cm.
Transvaginal echography reveals a unilateral formation with a thick wall having a double contour. The contents of the cyst are represented by an immovable fine suspension.
Color Doppler sonography records “poor” peripheral blood flow in the vessels of the neoplasm with an average level of resistance (IR min = 0.59+0.03).
Patients with neovascularization of tumor formation
Patients with borderline ovarian cystomas complain of dull, aching pain in the lower abdomen. In 83.3% of cases, an increase in abdominal volume was noted. The size of the tumors varies widely: 7-20 cm in diameter. All tumors exhibit a characteristic decrease in sound conductivity. It is not possible to judge the duration of the disease, since patients have been noticing certain symptoms of the disease for quite a long time, but do not seek medical help, or the doctor does not recommend surgical treatment.
Papillary cystadenomas are visualized by echography as formations with a clear and even outer contour, but along the internal contour there are multiple papillary formations in the form of echo-positive parietal structures.
Mucinous tumors are characterized by multilocularity and the presence of septa of unequal thickness. The contents of the chambers are represented by a spongy mass of increased echogenicity.
Color Dopplerography allows to detect neovascularization of the tumor: multiple color signals from vessels in the parietal growths, on the septa and in the tumor capsule with a low level of resistance (IR min - 0.40+0.07).
In patients with malignant ovarian tumors, the clinical course of the disease in the early stages of the disease is characterized by the absence of severe symptoms. In later stages of the spread of the process, women complain of pain in the lower abdomen, a feeling of malaise, weakness, and fatigue. In the small pelvis, dense, lumpy, painful formations with spiky outgrowths in the rectovaginal tissue are palpated, inactive, fused into a single conglomerate. Early-appearing ascites leads to an increase in abdominal volume, muscle tension in the anterior abdominal wall, and shortness of breath. The vast majority of patients are admitted to a specialized oncology hospital with stages III and IV of the disease.
When echography of serous malignant tumors, large pathological formations are detected (13-20 cm in diameter), occupying almost the entire abdominal cavity. The uterus is involved in the tumor conglomerate and in some cases is not visualized separately. The borders of the tumor in most cases have a bumpy contour and are not traced throughout.
Mucinous cystadenocarcinomas are characterized by the presence of multiple chambers of varying diameters (1-4 cm), some of them are filled with fine-mesh structures of medium echogenicity.
With color Doppler mapping, neovascularization of the pathological formation is recorded: intense central and peripheral blood flow in the septa and parietal growths, with a low level of resistance of the newly formed vessels. IR min - 0.36+0.06. The accuracy and sensitivity of IR min = 0.36+0.06 was 76.9%, specificity - 78.6%.
An increase in angiogenic activity and diffusely high capillary density corresponds to foci of proliferation and malignancy. Therefore, it is necessary to focus on the minimum index of resistance of intratumoral vessels, as an indicator that more accurately reflects the processes occurring in the tumor.
Ultrasound examination makes it possible to detect the presence and determine the structure of tumor-like formations of the ovaries in almost 100% of cases. However, the use of the gray scale as an independent method today is irrational, since it does not allow assessing the nature of tumor growth and identifying patients at risk.
Color Doppler mapping allows preoperative, non-invasive assessment and differentiation of tumors by the degree of changes in their vascular wall, by location and number of vessels, being a unique measure for assessing the malignancy of ovarian tumors. Comparison of echography and Dopplerography data leads to a real increase in the accuracy of diagnosing ovarian tumor formations.
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
When is the best time to do an ultrasound of the ovaries and uterus?
The day of the examination is determined by the attending physician depending on medical indications. The first ultrasound examination can be performed on any day of the cycle, with the exception of the period of menstrual bleeding - in the presence of chronic or acute diseases, the disease is easily diagnosed in any phase of the cycle. Experts recommend doing an ultrasound of the ovaries on days 5-7 or 22-24 of the cycle - the exact time is determined individually.
To obtain a complete picture of the functionality of the ovaries, ultrasound is performed several times during the menstrual cycle. The first time it is done on days 5-7, then on days 8-9, 13-14 and 22-24. This study is called folliculometry and is necessary to monitor ovulation by monitoring the growth of follicles on ultrasound and their subsequent rupture in the ovaries for the release of the egg. This type of diagnosis is prescribed to women with suspected infertility.
On what day of the cycle can an ovarian ultrasound be performed?
Most often, an ultrasound is performed after the end of the cycle. However, it is necessary to take into account its duration, since not every woman has it as a classic option. It is considered the most optimal to carry out diagnostics depending on the following cycle duration:
- With a cycle of 28 days, the optimal option for performing an ultrasound is the 7th day after the end of menstruation. During this period of time, new follicles have not yet begun to grow, and the thickness of the endometrium is the least important;
- with a 21-day cycle, the best day for ultrasound diagnosis is considered to be 3-5 days after menstruation. With such a cycle length, ovulation may already occur on day 7, accompanied by thickening of the endometrium due to the activity of progesterone;
- with a long cycle of 35-40 days, ultrasound is performed at a later date, which is calculated by a specialist in each specific case. The 7th day after the end of menstruation is considered normal for ultrasound.
If there is a need to track ovulation and the formation of the corpus luteum, ultrasound is performed dynamically from days 8 to 10, from days 12 to 14 and from days 22 to 24, that is, the process of follicle maturation is monitored throughout the entire cycle.
Types of examination
Types of ultrasound of the ovaries in women have different information content and differ in the process of conducting:
- transabdominal - examination of organs through the anterior abdominal wall, for this the doctor smoothly moves the sensor over the skin, previously lubricated with gel;
- transvaginal - the most informative method, carried out by inserting a sensor into the vagina to a depth of 12 cm;
- transrectal - rarely used for diagnosing ovaries; for examination, the sensor is inserted into the rectum to a depth of 6 cm.
How is ultrasound performed at SM-Clinic?
The study is performed in three ways, including:
- Transabdominal. This is a superficial examination that is carried out through the abdominal wall using a sensor.
- Transvaginal. This is an informative method in which the examination passes through the vagina. In this case, the doctor receives the most accurate results.
- Transrectal. This diagnostic method is rarely prescribed, only in cases where it is impossible to examine the condition of the ovaries by other methods for a number of reasons.
During an ultrasound examination using any of the above methods, a woman does not experience pain or discomfort. The procedure lasts approximately 10-15 minutes, the doctor’s conclusion is issued immediately.
Preparing for the examination
Preparing for an ultrasound scan of the ovaries and uterus does not take much time. When prescribing a diagnosis, gynecologists inform the patient about all the rules of procedures that must be followed before the study.
Transabdominal ultrasound
To obtain the most reliable results, it is necessary to prepare the internal organs of the pelvis for the procedure. To do this, you need to follow a special diet for 2-3 days, excluding gas-forming foods - legumes, cabbage, white bread, etc. Before visiting a doctor, you should empty your bowels naturally or with the help of a microenema.
The bladder should be full. An hour and a half before the ultrasound, a woman needs to drink up to one and a half liters of non-carbonated liquid. Tea, water or juice are suitable for this purpose. Insufficient fullness of the bladder makes it difficult to examine the appendages.
Transvaginal
To perform such an ultrasound of the ovaries and uterus, no preparation is required from the woman. First, you should thoroughly rinse the perineum using intimate hygiene products.
Infections during examination are excluded - to protect the patient, doctors use a disposable condom made for sensors. Some clinics ask clients to bring their own protective product, which can be purchased at the pharmacy.
If the ovary hurts during or after an ultrasound, you should immediately inform your doctor - this may be caused by some disease of the pelvic organs.
Transrectal
To carry it out, it is necessary to clear the rectum of feces. To do this, before visiting a doctor, you should empty your bowels naturally or with the help of a microenema. A few days before the procedure, gas-forming products should be eliminated.
How to prepare for an ultrasound?
Ultrasound of the ovaries requires preparation so that the doctor can thoroughly examine all female organs. Excessive gas or stool in the intestines may limit visibility.
- A few days before the diagnosis, give up foods such as milk, legumes, fruits, vegetables, baked goods, and carbonated drinks. They enhance gas formation processes, which can complicate visualization during examination.
- 3 days before the ultrasound, eat only light food. It is better not to eat at least 4–6 hours before a transabdominal ultrasound of the ovaries.
- Before the examination through the abdomen, you need to drink 1 liter of water 1–1.5 hours in order to fill the bladder. For other methods, the bladder does not need to be filled.
- Before transrectal ultrasound, it is necessary to cleanse the rectum with an enema.
If an ultrasound examination is performed during menstruation, make sure you have a diaper and hygiene products.
How to do an ultrasound of the uterus and ovaries
The examination stages of the procedure itself do not differ from each other. The main differences lie in the area of the body through which the examination is carried out.
Transabdominal
The patient lies on the couch on her back with her legs straightened. A special gel that conducts ultrasonic waves is applied to the previously exposed lower abdomen. The sensor is moved over the lubricated area, assessing the condition of the internal genital organs. Visualization is difficult when the bladder is not full or when gases form in the intestines.
Transvaginal
The woman lies on the couch on her back, with her legs bent and slightly spread. A condom is put on the sensor, the latter is lubricated with a special gel. The device is inserted into the vagina and gently moved within it for a complete examination. This method is the most informative due to the absence of other organs that may interfere with the examination and the close proximity to the appendages.
Transrectal
The patient lies on the couch on her side, bending her knees and clasping them with her arms. The sensor with a pre-applied condom is inserted into the anus. This method is used very rarely and is relevant only when transvaginal scanning is impossible or examination through the abdominal wall is uninformative.
In girls and virgins
For girls and women who have not been sexually active, the transabdominal or transrectal method is used. Examination by inserting a probe into the vagina is not possible due to the risk of damaging the hymen. After the start of sexual activity, patients are recommended to undergo a transvaginal ultrasound for a more detailed examination of the organs.
Decoding the testimony
A description of the data obtained is carried out by a functional diagnostics doctor, but only a gynecologist can assess their significance for making a diagnosis.
Normal for girls and women
The size of the ovaries depends on age, and in girls and women with an established cycle they change slightly depending on its phase. For diagnostics, not only the value of length and width, thickness, but also volume (the product of the obtained parameters) is taken into account. The latter indicator is considered a more reliable sign of normality and deviations.
| Age, years | Ovarian volume, cm3 |
| 1 | 1 |
| 2-6 | 0,67 |
| 7-10 | 1,2-2,3 |
| 11-12 (or until menstruation appears) | 2-4 |
| From the beginning of a stable cycle | 2,5-10 |
| Menopause | 1,5-4 |
Follicles can be found already in a newborn. They look like small cavities with liquid. Formed under the influence of matter hormones. After 2 years and up to 12, they are found in half of the girls.
In women, the ovaries have a lumpy surface consisting of maturing follicles. The organs are abundantly supplied with blood, their density (echogenicity) is almost the same as the uterus. There should be at least 10-12 follicles in two ovaries with a size of about 4-7.5 mm. Before ovulation (approximately the middle of the cycle), one large one appears, reaching 20 mm. An egg is then released from it, and then a corpus luteum is formed, which produces progesterone.
Watch the video about ultrasound of the pelvic organs in women:
Norms for ovarian size
One ovary in a woman is always slightly larger than the other - this is due to the peculiarities of their work. The dominant organ is large due to the constant production of eggs, the second in most cases is responsible only for the production of hormones. Therefore, identifying different sizes of appendages should not frighten the patient.
Normal ovarian size on ultrasound in adult women:
- length – 20-37 mm;
- width – 18-30 mm;
- thickness – 16-22 mm;
- volume – 4-10 cubic meters. cm.
During menopause, the maximum ovarian volume is 4 cubic meters. see - this is due to the natural cessation of their functionality.
Minor deviations can be considered normal. If the appendages are excessively large, their inflammation, the presence of neoplasms and other pathologies are diagnosed. Small ovaries are not the norm - such organs most often have low functionality, cause infertility or signal the onset of menopause.
Hemorrhagic ovarian cysts
A complex hemorrhagic ovarian cyst is formed by bleeding from a Graafian follicle or follicular cyst. On ultrasound, hemorrhagic cysts appear as single-chamber thin-walled cystic structures with the presence of fibrin strands or hypoechoic inclusions, with good permeability to ultrasound. On MRI, hemorrhagic cysts are characterized by high signal intensity on T1 FS scans, while on T2 WI they give a hypointense signal. With Doppler ultrasound, there is no internal blood flow; the component accumulating contrast inside the cyst is not detected on CT or MRI. The wall of a hemorrhagic cyst has variable thickness, often with the presence of vessels located in a circular pattern. Despite the fact that hemorrhagic cysts usually manifest with acute pain symptoms, they can be an incidental finding in a patient who does not present any complaints.
Sonograms reveal a hemorrhagic cyst with a blood clot simulating a neoplasm. However, Doppler ultrasound did not reveal internal blood flow in the cyst, and its permeability to ultrasound was not reduced.
MRI picture of a hemorrhagic ovarian cyst: in the T1 VI mode without fat suppression, a complex cyst is determined, characterized by a hyperintense signal, which can be caused by both the fatty component and the blood. On T1 fat-suppressed imaging, the signal remains hyperintense, allowing confirmation of the presence of blood. After administration of gadolinium-based contrast, no contrast enhancement is observed, which allows us to confirm the hemorrhagic nature of the ovarian cyst. In addition, it is necessary to include endometrioma in the differential diagnostic range.
Ultrasound reveals a soft tissue (solid) component in both ovaries. However, ultrasound permeability on both sides is intact, suggesting the presence of hemorrhagic cysts. Dopplerography (not shown) shows no blood flow in the formations.
How to distinguish a hemorrhagic cyst on MRI? In T1 mode, a component with high signal characteristics (fat, blood or protein-rich fluid) is detected in both formations. With fat suppression, the signal intensity does not decrease, which generally makes it possible to exclude a teratoma containing adipose tissue and confirm the presence of hemorrhagic fluid.
Changes in the appendages during the menstrual cycle
The appendages themselves are always the same size.
Changes occur in the follicles and corpus luteum necessary for conception. The first contain an egg that is released on days 14-16 of the cycle for fertilization, breaking the outer shell. The corpus luteum is formed at the site of the burst follicle - it is necessary for the production of the hormone progesterone, which promotes the movement of the egg through the fallopian tubes and the implantation of the fertilized egg into the walls of the uterus. Changes in follicle size by day of the cycle:
- 5-7 days – formation of several dominant follicles up to 6 mm in diameter;
- 10-11 days – clear identification of a dominant follicle measuring 14-16 mm;
- 14-15 days - the follicle reaches its maximum size of 18-22 mm, after 1-2 days it will rupture and the egg will be released, i.e. ovulation.
The days of the cycle are indicated taking into account its duration of 28 days; in women with a longer or shorter menstrual cycle, changes in the appendages occur at other times.
After ovulation occurs, the corpus luteum matures:
- 15-16 days - the corpus luteum is determined to be up to 20 mm in size, free fluid in the uterus from a burst follicle;
- Day 20 – the corpus luteum actively produces progesterone and reaches a size of 25-27 mm;
- 26-27 days - regression of the corpus luteum - its diameter is 1 cm, with the onset of menstruation it disappears.
These changes are considered normal - they are present in all women who do not have health problems.
Diagnosis of ovarian cancer
Transvaginal ultrasound (trusound) and determination of the CA 125 marker in blood serum are used as diagnostic methods. The combination of these two methods has high specificity for diagnosing ovarian cancer.
Additional research methods such as magnetic resonance imaging (MRI) or positron emission tomography (PET) can provide additional information, but are not necessary studies in routine practice during preoperative preparation. If the results of TRUS are questionable, the use of MRI can help us in correctly diagnosing ovarian tumors (malignant/benign tumor). The final diagnosis of ovarian cancer is made only after a morphological (examination of cellular/tissue composition) examination.
CA 125 (carbohydrate antigen 125) is the main marker of ovarian cancer. Normal levels in blood serum are up to 35 IU/ml. In most cases of ovarian cancer, its concentration increases 5 times or more. The concentration of CA 125 in the blood serum can also increase in various non-tumor diseases: inflammatory changes in the abdominal cavity, pelvis, menstruation, benign tumors of the female reproductive system (ovarian cysts). However, in most of these cases, the concentration of CA 125 in the blood serum does not exceed 100 IU/ml.
Decoding the results
The condition of the organs is determined by several parameters that are recorded on the diagnostic sheet. Using some values, you can independently decipher the results of an ultrasound scan of the uterus and ovaries, and the presence of any abnormalities in their functioning.
Location
Normally, the ovaries are located on both sides of the uterus, on the side walls of the pelvis.
They may be slightly shifted relative to the uterus - with a slight change this is not considered a deviation. In most cases, the norm of location is determined individually - for some women it may differ slightly from the established standards. This is explained by the anatomical features of the internal organs.
What can be seen with a gynecological ultrasound?
Ultrasound of the ovaries can reveal various pathologies:
- Anovulation as a probable cause of infertility.
- Volumetric formations of the gonads: cysts and tumors.
- Inflammatory diseases of the uterine appendages.
- Ectopic pregnancy.
- Anomalies of appendage development.
An ultrasound scan helps to find the cause of the pathological process and select the optimal treatment.
Gynecological ultrasound can also detect diseases of the uterus and fallopian tubes. The technique is actively used in the diagnosis of various conditions during pregnancy.
Question to the expert
Tell me, on what day of the menstrual cycle is an ultrasound of the uterus and ovaries performed? The doctor advised me to undergo an examination, but the date was not indicated in the direction.
Ultrasound of the uterus and ovary is done by default on the 5-7th day of the cycle, unless the doctor gives other instructions.
Other features noticeable during ultrasound
During the examination, not only the size and structure of the organs are determined, but also the degree of their functionality. Sometimes quite rare pathologies are diagnosed.
Why the ovary may not be visible or clearly visible
Most often, the appendage is not clearly displayed on the monitor screen during a rectal or transabdominal ultrasound. In this case, visualization is hampered by an overproduced bowel or an unfilled bladder. The study should be repeated in compliance with all preparation rules.
An ultrasound does not show the ovary even when it is depleted or there are adhesions. If it is difficult to make a diagnosis, magnetic resonance imaging of the organs should be performed - this type of diagnosis is considered much more informative than ultrasound.
Increase in size
A slight increase in appendages is noted when the follicles reach large sizes. If there is a strong deviation from the norm, an inflammatory process or cystic formation is diagnosed.
Lack of follicles
Indicates a violation of the reproductive function of the ovaries. The study must also be carried out for the next menstrual cycle - most women do not ovulate 1-2 times a year for natural reasons.
Follicles are not detected during examination at the time of ovulation - during this time the corpus luteum has not yet had time to form, and the doctor may make a false diagnosis.
Increased echogenicity
Stroma is the lining of the appendage containing many blood vessels. Its high echogenicity indicates the course of polycystic disease or an inflammatory process.
What does ovarian cancer look like on an ultrasound machine?
Oncology in the ovaries is determined by ultrasound in the form of a multilocular cancerous tumor and papillary growths. Such formations have thick walls; in the final stages they can reach enormous sizes.
Other violations
Other types of diseases that can be detected by ultrasound of the ovaries:
- endometriosis – adhesions of the uterus, fallopian tubes, formation of endometrioid cysts on the appendages;
- ovarian pregnancy - attachment of the embryo near the appendage or to its walls;
- calcifications in the ovaries by ultrasound are defined as the deposition of calcium salts in the organ;
- rupture of the appendage or its cyst is accompanied by acute pain, which forces an examination.
Ultrasound of the ovaries is necessary for every woman to undergo regularly to prevent the development of gynecological diseases. Carrying it out 1-2 times a year ensures timely diagnosis of pathologies, and early treatment accelerates the recovery process. The ultrasound examination method is considered completely safe and does not harm health.
What does an ultrasound show?
An ovarian ultrasound will help detect the following pathologies:
- Cyst (round echogenic formation with fluid inside).
- Multifollicular ovaries (slight enlargement of the organ, multiple small follicles in the absence of a dominant one).
- Polycystic ovaries (ultrasound shows an increase in the size of the organ, uneven contours, increased echogenicity, a large number of follicles).
- Inflammatory process (increased echogenicity of the ovarian stroma, blurred indistinct contours, increased size).
- Ovarian apoplexy (ultrasound shows signs of ovarian rupture and blood clots).
- Adhesions (immobility of the organ, atypical location).
- Neoplasms (changes in the shape and size of an organ, multi-chamber fluid formation).
- Ectopic pregnancy (the right or left ovary in which the embryo is located is enlarged).
- Calcifications (ultrasound signs of calcium deposition in an organ).
Video shows ovarian cancer:
Sometimes the organ may not be detected. The absence of an organ indicates premature aging of the ovary, developmental abnormalities, and adhesions. Sometimes the ovary is not detected on ultrasound due to the accumulation of gases in the intestines. Watch the video to see what it looks like:
Ultrasound is performed not only when gynecological pathology is suspected, but also for preventive purposes. For example, to assess ovarian reserve. This indicator indicates the health of the reproductive system and the ability to become pregnant.
It is imperative to control the size of the organ upon the onset of menopause. Normally, the size of the ovaries in women according to ultrasound is reduced during menopause, as natural aging of the body occurs. Dimensions:
- length: 20–25 mm;
- width: 12–15 mm;
- volume: no more than 4 cubic meters. cm.
Features of the study
For folliculometry, a conventional ultrasound device is used. The study consists of several procedures. Each of them complements the overall picture, but performs individual tasks. To obtain an accurate result, ultrasound is performed on strictly defined days.
The first ultrasound examination is carried out on days 7-10 of the cycle. You need to calculate the day using the cycle calendar at least six months in advance or based on the results of other tests. The first ultrasound examines not only the ovaries, but also the uterus and fallopian tubes, which allows you to assess the condition of the genital organs and readiness for conception. The first procedure will immediately exclude or confirm the presence of concomitant pathologies. If there is a danger, the organs are examined during each ultrasound.
In parallel with folliculometry, the hormonal blood level is determined. Functional tests are performed to calculate the day of ovulation. On the day of ovulation, the level of female sex hormones in the blood changes. Other signs of ovulation: disappearance of the predominant follicle, formation of the corpus luteum, accumulation of fluid behind the uterus in the abdominal cavity.
Scheme of folliculometry
- At the end of menstrual flow. Since menstruation itself is the first phase of the cycle, during this period 2-3 follicles of 5-9 mm in diameter begin to mature in the ovaries. The level of progesterone decreases, and a new one forms in place of the dead endometrium. After menstruation it is thin, without inclusions. The thickness reaches 2-3 mm.
- Between days 10 and 11 of the cycle. It is during these days that the predominant follicle is determined. It is noticeably larger than the others, reaching 10 mm. Its subsequent growth: 2-4 mm every day. If the dominant follicle is not identified during the second folliculometry, the ultrasound course is stopped. If there is no dominant follicle, the woman will most likely need ovulation stimulation. On these days, the endometrium begins to prepare for conception, the basal layer increases, and cells actively multiply (proliferation phase). At the end of the phase, the endometrium thickens to 4-5 mm, and the follicle reaches 15 mm in diameter.
- Between days 12 and 13 of the cycle. The dominant follicle is almost ready to ovulate (release an egg). Its dimensions are 22-23 mm. The endometrium matures in the uterus, the three-layer structure is clearly visible. The normal width for this period is 8-12 mm. Without three layers and sufficient width, the uterus will not be able to accept the embryo and securely implant it. Even if it gets caught, there is a high chance of miscarriage. If it does not take hold, it can leave the uterus and take root elsewhere, turning into an ectopic pregnancy. The fourth ultrasound is performed only if there are signs of future ovulation.
- A day later for the third ultrasound. At this stage, ovulation should take place: the release of the egg, the transformation of the follicle into a body with curved edges. If ovulation has not occurred, the examination is repeated daily until the egg is released or discharge begins.
- Between 15 and 17 days. Ultrasound at this stage is necessary only during ovulation. The previously dominant follicle becomes the corpus luteum, which produces the hormone progesterone. It will protect and nourish the embryo until the placenta is fully formed at the beginning of the second trimester. The corpus luteum has a characteristic star-shaped shape. The width of the endometrium reaches 13 mm, three layers turn into one.
- Between 21 and 23 days. During this period, the endometrium should be homogeneous and wide. The corpus luteum continues to grow. The fertilized egg is just moving into the uterus and trying to gain a foothold. The condition of the endometrium must be monitored carefully, because the success of fertilization depends on it.
Causes of ovarian failure
Today, there are three theories for the development of exhausted ovarian syndrome:
- chromosomal abnormalities;
- autoimmune diseases;
- iatrogenic factors.
Under the influence of each of the factors, ovaries with an insufficient number of follicles are formed, the regulation of cyclic processes in the hypoalamus is disrupted, and germ cells die.
Almost every second patient with the syndrome has menstrual irregularities in close relatives. Delayed sexual development, complete or partial absence of menstruation, and early menopause in the mother can be observed.
Ovarian wasting syndrome is also often associated with autoimmune hypothyroidism and other autoimmune diseases, suggesting a role for the immune system in the development of the pathology. In addition, gestosis, extragenital pathology of the mother, and the use of certain medications during pregnancy are important. Acting during the period of intrauterine development of the fetus, these factors damage the follicular apparatus. After birth, ovarian wasting syndrome can be caused by viral diseases - rubella, influenza, mumps, streptococcus, excessive psycho-emotional stress, fasting, and vitamin deficiency. Often the disease develops after surgical interventions on the ovaries, conservative treatment of fibroids, or surgery for an ectopic pregnancy.
Thus, the main role in the development of exhausted ovarian syndrome is played by the following points:
- Hereditary predisposition in the female line (early or premature menopause in the grandmother, mother or sisters).
- Autoimmune diseases (eg, autoimmune hypothyroidism).
- Infectious, iatrogenic factors (that is, effects on the ovaries during treatment of any disease) that can affect the organ at different periods of life (for example, even in utero, the ovarian tissue of the fetus can be damaged if the pregnant woman took drugs with a teratogenic effect, or had rubella in childhood, chemotherapy in adulthood).
- Adverse effects of environmental factors - hunger, vitamin deficiencies, stress.
- History of surgical removal of part of the ovary (for example, during resection of a cyst or tumor).
Prognosis and prevention of pathology
Unfortunately, specific preventive measures to prevent the syndrome have not been developed. The main preventive measures are:
- proper nutrition;
- timely treatment of viral infections;
- avoiding contact with harmful substances;
- elimination of psycho-emotional and physical stress;
- treatment only under the supervision of a physician;
- correct selection of IVF protocol;
- regular preventive examinations.
A woman's diet should be balanced in both calories and nutrients. It is strongly not recommended to use strict diets for the purpose of rapid weight loss. If necessary, a diet should be developed by a doctor.
Viral infections should be treated in a timely manner, carefully following the doctor's recommendations. This applies to both medication and regimen. Contact with hazardous substances at work should be kept to a minimum. It is imperative to use personal protective equipment. To avoid excessive physical activity, you should review your daily routine and occupation. If it is impossible to completely eliminate overload, you need to properly plan your work and rest schedule. It is also advised to reconsider your attitude towards stressful situations. Taking hormonal medications should only be started on the recommendation of a doctor. Before starting therapy, you should undergo a complete laboratory and instrumental examination.
The in vitro fertilization protocol should be selected only taking into account the individual characteristics of the organism. Women should undergo preventive examinations with a gynecologist at least once a year, and patients at risk - once every six months. The Altravita clinic successfully treats women with exhausted ovarian syndrome. If you want to get pregnant and give birth to a child, assisted reproductive technologies using donor eggs are used.