Structure of the ovaries
Ideally, the ovaries in women are ovoid in shape, slightly flattened at the end, and the color of healthy tissue is blue-pink.
The surface of the organ is covered with scars, which are a consequence of the presence of corpus luteum in the ovaries and the passage of ovulation. Its weight ranges from 5-10 grams. The dimensions of the ovaries are about 25-55 millimeters in length and fifteen to thirty millimeters in width. Thickness is about 20 millimeters. Women's ovaries can change their location. They are attached to the pelvis by a ligament that suspends them and a ligament that connects to the uterus called the mesentery. Depending on the situation, the ovaries can change not only their location, but also their size.
Important! The ovaries have lateral and medial sides. The front side of the surface of the organ smoothly passes into the edge, which protrudes and is attached to the mesentery
The structure has a groove-like depression called the “ovarian hilum.” An artery and a nerve run through them, and veins and vessels emerge.
The top of the ovary is covered with germinal epithelium. Underneath it is white connective tissue with a higher density than the connective tissue. The stroma, which has a large number of elastic fibers, also consists of it. Parenchyma has two layers - outer and inner. The internal one is the medulla, which has a loose structure in which lymphatic and blood vessels are located. The outer one is the ovarian cortex; large vesicular and primary, small follicles are located on it.
At the edge of the organ there is a follicle, already ready for the ovulation process. Inside a mature, membrane-covered follicle there is a liquid, inside of which there is a granular layer with eggs and an egg-bearing tubercle located in it. This follicle reaches 2 centimeters in diameter.
Types of examination
Types of ultrasound of the ovaries in women have different information content and differ in the process of conducting:
- transabdominal - examination of organs through the anterior abdominal wall, for this the doctor smoothly moves the sensor over the skin, previously lubricated with gel;
- transvaginal - the most informative method, carried out by inserting a sensor into the vagina to a depth of 12 cm;
- transrectal - rarely used for diagnosing ovaries; for examination, the sensor is inserted into the rectum to a depth of 6 cm.
Ovarian volume 35 cm
Found (21 posts)
gynecologist August 23, 2011 / Olga / Novokuznetsk
...there was a laparoscopy (endometrioid cyst of the left ovary
and paraovarian cyst on the right).
Buserelin injections were prescribed... Ultrasound results on August 15: The right ovary is enlarged, volume
34 cubic meters.
cm
, clear contours, in the ovary there are 3 follicular cysts with a diameter of
35
, ... open
geneticist April 8, 2010 / Elena / Samara
... inflamed. Macroscopic examination of mucus: volume
sputum 1
cm
(norm 5-20 cm), outwardly dull... CA125 -4.0 u/ml, with a norm of up to
35
TSH - 1.600 m IU/l (0.150 -4.500) ... protocol due to lack of
ovarian
. It is proposed to carry out HLA typing based on ... open
infertility March 13, 2010 / Elena / 0
... inflamed. Macroscopic examination of mucus: volume
sputum 1
cm
(norm 5-20 cm), outwardly dull... CA125 -4.0 u/ml, with a norm of up to
35
TSH - 1.600 m IU/l (0.150 -4.500) ... protocol due to lack of
ovarian
. Thanks in advance for your help. Best regards... open
infertility December 8, 2009 / Angela / 0
..., thickness 25 mm, width 35
mm,
volume
19.2
cm
cubic.
, the structure is changed due to ..., thickness 12 mm, width 25 mm, volume
5.7
cm
cube, structure is not changed, ... conclusion was not identified - retention cyst of the left
ovary
, endocervical cysts (chronic cervicitis?)
At 22 … open
infertility October 10, 2009 / Anna
... the hormones were increased testosterone, prescribed to Diana 35
, which I drank for 3 years.
Already... volume – 2.3 ml. Isthmus 5 mm, total volume
9.9 ml, k=0.479 Dimensions and volume of the gland... *23*22 mm,
volume
8.1 cubic meters.
cm
.
Both ovaries
with anechoic inclusions 4-6 mm ... open
gynecologist October 5, 2009 / Valeria
... ovaries, hr. bilateral periodnexit. Right ovary: length 35
, thickness 23, width 25,
volume
... a month ago, according to ultrasound data,
the volume
of the right
ovary
was 5.3
cm
, the left ovary was 6.6
cm
. 3 M-echo also increased... tab - 2 times a day - 10 days, diane -
35
from the 1st day of men-tion 21 days ... open
gynecologist March 21, 2009 / Maria
Two years of unsuccessful attempts to have a child. Both my husband and I have children from our first marriages. I am not ovulating. I did AI (there was ovulation) - unsuccessfully. Latest… open
March 22, 2009 / Tatyana Borisovna Malanova
... 2. High ovarian reserve is assumed if: - the patient’s age is less than 35
years;
- FSH level at 2-3 d.m.c. less than 8IU/l; - number... 2-3 d.m.ts. more than 10 in each ovary; - ovarian
volume more than 12
cm³
; - high levels of anti-Mullerian hormone.
gynecologist December 7, 2007 / Irina
... 49 mm. Weight 60.7 g. Volume
: 57.8
cm
cu.
The contours are smooth. Echogenicity is normal. ... d= 45 mm Left ovary Dimensions: 35
* 25 * 24 mm.
Weight 10.6 g. Volume
: 10.1
cm
.
cube...: Uterine leiomyoma. Endometrioid cyst of the right ovary
. The ultrasound doctor said what needs to be done... open
endocrinologist February 10, 2005 / Alena
...at the end of 1999. ovarian cyst was discovered
, which increased during the year.
At the beginning of 2001... I completed 2 courses of treatment for 3 months each. Diana is 35
.
Menstruation is still irregular (23-... 200 to 2004, the volume
of the thyroid gland increased from 5 cubic
cm
to 7.5. Analysis of TSH-... open
endocrinologist February 22, 2002 / Larisa M.…
... - became smaller (by the way, I usually have a rather large menstrual cycle from 35
up to 40 days).
The ovaries themselves also worry me, the last ultrasound showed that the volume
of the left
ovary
reached 34
cm
cubic (Ultrasound on the 8th day of the month). What... open
Preparing for the examination
Preparing for an ultrasound scan of the ovaries and uterus does not take much time. When prescribing a diagnosis, gynecologists inform the patient about all the rules of procedures that must be followed before the study.
Transabdominal ultrasound
To obtain the most reliable results, it is necessary to prepare the internal organs of the pelvis for the procedure. To do this, you need to follow a special diet for 2-3 days, excluding gas-forming foods - legumes, cabbage, white bread, etc. Before visiting a doctor, you should empty your bowels naturally or with the help of a microenema.
The bladder should be full. An hour and a half before the ultrasound, a woman needs to drink up to one and a half liters of non-carbonated liquid. Tea, water or juice are suitable for this purpose. Insufficient fullness of the bladder makes it difficult to examine the appendages.
Transvaginal
To perform such an ultrasound of the ovaries and uterus, no preparation is required from the woman. First, you should thoroughly rinse the perineum using intimate hygiene products.
Infections during examination are excluded - to protect the patient, doctors use a disposable condom made for sensors. Some clinics ask clients to bring their own protective product, which can be purchased at the pharmacy.
If the ovary hurts during or after an ultrasound, you should immediately inform your doctor - this may be caused by some disease of the pelvic organs.
Transrectal
To carry it out, it is necessary to clear the rectum of feces. To do this, before visiting a doctor, you should empty your bowels naturally or with the help of a microenema. A few days before the procedure, gas-forming products should be eliminated.
Normal ovaries on ultrasound
The ovaries are homogeneous in structure, isoechoic in relation to the uterus and hypoechoic to the intestinal loops. Due to the vessels, the medulla can be hyperechoic compared to the cortex. Anechoic follicles are located in the cortex along the periphery. The dominant follicle usually reaches from 2.0 to 2.8 cm.
| Photo. A - A normal ovary has several anechoic follicles along its periphery. B - After menopause, the ovaries atrophy. They lack follicles and have reduced blood flow, making them difficult to detect. Menopausal women may have small cysts or residual follicles. A simple cyst less than 1 cm in a menopausal woman can be ignored. | |
Ovarian volume for different ages
The volume of the ovaries is calculated using the ellipse formula: 0.5 x length x width x height
| Age | Average volume cm3 | Maximum volume cm3 |
| 0-3 months | 1 | 4 |
| 3 months - 2 years | 1 | 3 |
| 3-15 years | 3 | 9 |
| Period of menstruation | 10 | 22 |
| Postmenopause | 6 | 14 |
| More than 15 years of menopause | 2 | 4 |
Changes in the ovary during the monthly cycle
Photo. A - Normal ovary on day 12 of the cycle. The dominant follicle is large in diameter and several small ones (2-5 mm). Why does one follicle from a cohort develop while the rest undergo atresia? Riddle... B - Before ovulation, the wall of the dominant follicle has a developed network of thin vessels, the blood flow in the wall is increased. B — Atretic follicle of preovulatory diameter
Note the thin and flaccid hyperechoic follicle wall. The wall of the atretic follicle is avascular
The large follicle is deformed due to small follicles along the periphery. With the growth of a healthy follicle, the increase in estradiol is significant, while the anovulatory follicle produces a minimum of estradiol.
| Photo. Record during ovulation (time shown below left). You can see how the fluid releases the follicle, the walls close and two thickened, slightly hypoechoic parallel stripes appear - this is the corpus luteum. |
The corpus luteum is an endocrine gland that regulates the menstrual cycle and maintains early pregnancy. The corpus luteum is formed from the cells of the wall of the preovulatory follicle. After ovulation, the volume of luteal tissue increases, increased vascular formation occurs, and the level of progesterone and estradiol increases. High blood flow in the corpus luteum is an indicator of metabolic activity. The corpus luteum remains unchanged until the 12th week of pregnancy and until the 23rd day of the menstrual cycle if pregnancy does not occur.
The corpus luteum may become filled with hypoechoic fluid, in which case it appears as a cyst. Fluid within the corpus luteum should be interpreted as a normal physiological phenomenon. Most often, blood and ichor leak from the vessels of the follicle wall after rupture. Fluid can be seen immediately after ovulation, and subsequently the volume may decrease or increase.
During the first week after ovulation, the corpus luteum can be traced to a rupture point on the outer edge of the ovary. If the break point is not visible, it is difficult to distinguish between a corpus luteum cyst and an anovulatory follicle. Therefore, the best time to identify the corpus luteum is soon after ovulation.
| Photo. A - Corpus luteum without a cavity (arrow). B, C — Corpus luteum of irregular shape with a thick, rugged wall and hypoechoic liquid contents (asterisk). |
| Photo. Neovascularization of the corpus luteum begins immediately after evacuation of follicular fluid. Within 48-72 hours, a vascular ring around the luteal tissue appears on ultrasound. As the corpus luteum develops, the ring of vascularization becomes more prominent. A, B - Blood flow around the corpus luteum on the day of ovulation. B - Blood flow around the mature corpus luteum. | ||
The corpus luteum can be seen throughout the luteal phase of the menstrual cycle. Once conception occurs, the corpus luteum will persist through the first trimester of pregnancy. In the absence of conception in the late luteal phase, degradation of blood flow begins in the corpus luteum and with the onset of the next menstruation, the corpus luteum will regress. As a result of regression of the corpus luteum of the previous cycle, a white body is formed. Sometimes several white bodies from previous menstrual cycles can be observed.
| Photo. A, B - The corpus alba is usually visualized as hyperechoic structures in the ovaries. | |
Take care of yourself, Your Diagnosticer!
Diseases, causes and symptoms
Ovarian diseases are divided into four types: 1. Diseases that arise against the background of hormonal imbalance. A characteristic symptom is menstrual irregularity, and the consequence can even be infertility. 2. Diseases associated with the occurrence of various neoplasms, most often cysts. Most of them are asymptomatic in the first stages. 3. Malignant ovarian tumor (cancer). In some cases, it also does not make itself felt for a long time and is detected only when metastases appear. 4. Inflammatory processes of the ovaries. The causative agent is bacteria from the cocci family, and sometimes the common cold. As a rule, the symptoms of all diseases are similar. These are: 1. Sharp or aching pain in the lower abdomen. 2. The occurrence of bleeding in the middle of the cycle. 3. Pain during sexual intercourse. 4. Vaginal discharge of various types. 5. Increase in temperature. 6. Pain when urinating. 7. Irregular menstruation or its complete absence. 8. Problems with conception. These are general symptoms that are characteristic of any disorder in the functioning of the ovaries. However, each disease also has specific symptoms that are specific only to a specific disease. Your doctor will tell you about them in detail during your examination.
Common causes of ovarian diseases are hormonal imbalance, untreated inflammation, hereditary predisposition, and the presence of damage by bacteria, viruses or fungi. In some cases, the cause of ovarian diseases may be a previous injury or taking a hormonal-based drug.
There are also factors that increase the risk of developing the disease. These include: 1. Failure to comply with the rules of intimate hygiene. 2. Self-medication using antibacterial agents. 3. Stress. 4. Uncontrolled sexual intercourse. 5. Weak immunity. 6. Unprotected sexual intercourse. 7. Abortion. 8. Some types of contraceptives. 9. Childbirth.
We recommend you learn: What are follicles in the ovaries
Preparation
If a diagnostic ultrasound is necessary, then it is advisable to examine the ovaries in the first half of the menstrual cycle, or more precisely on days 5-6.
In the case when it comes to identifying the dominant follicle and determining the moment of ovulation, the examination is carried out on days 8-12.
Depending on the type of study, the recommended preparation differs slightly:
- During the TA examination, it is necessary to fill the bladder. To do this, you need to drink 1 liter of water an hour before the test or simply not urinate for about 2-3 hours. The bladder is considered full when its volume is 300 ml, that is, when the first urge to urinate occurs.
- During a TV examination, you must first empty the bladder.
For a combined examination, you must come with a filled bladder, because first of all the doctor will perform a transabdominal examination. Next, after the bladder has emptied, transvaginal sonography will be performed.
Increased gas formation in the intestines can interfere with the examination, therefore, 2 days before the scheduled date of the ultrasound, you should follow a light diet with the exception of foods that contribute to flatulence.
Normal anatomy and physiology of the ovaries
The female gonads, the right and left ovaries, are bean-shaped. Their size depends on biological age: the average volume of the ovaries in girls before menarche is about 3 cm3, in menstruating women - 10 cm3, in postmenopausal women - 6 cm3.
The ovaries are located on the sides of the uterus. They are strengthened in their position by ligaments. The ovary is supplied with blood from two sources: the ovarian artery, arising from the aorta, and the ovarian branch of the uterine artery.
Every 4 weeks, a mature egg is released, ready for fertilization. Between the immature eggs there are intermediate cells that secrete the female sex hormone. Thus, the gonads produce reproductive cells and secrete sex hormones.
| Photo. If you cut the ovary and examine it at high magnification, you can see the medullary (medulla) and cortical (cortex) layers. The medullary layer is a number of round resting cells along the outer edge of the cortex - these are the primary egg cells, or follicles. Each newborn girl has 2,000,000 of these follicles. Only 200-300 of them will mature and form a mature egg. In the first 10 years of a girl’s life, the primary follicles remain dormant, and the formation of sex hormones occurs only in small quantities. With the onset of puberty, the size of the ovaries increases and intermediate cells begin to function, which secrete more sex hormone. By the end of the maturation period, mature eggs are formed, that is, capable of fertilization. | |
| Photo. The development of follicles occurs under the influence of pituitary gonadotropins - follicle-stimulating (FSH) and luteinizing hormones (LH). FSH stimulates the development of follicles in the ovaries. Follicles that were at rest divide once, then again. The last division is called the maturation division. It is of great importance for fertilization and the inheritance of parental qualities. About 10 follicles mature each menstrual cycle. Associated cells grow around the egg. Some of them are adjacent to the egg, surrounding it, while others form a graphite bubble, which is gradually filled with liquid. Only one Graafian vesicle becomes the dominant follicle and reaches a size of 2.0 to 2.5 cm. The vesicle squeezes to the surface of the ovary, its shell becomes thinner and thinner, and one day bursts. When the follicle matures, it releases estrogen, which stimulates endometrial growth. Close to day 14 of the menstrual cycle, high estrogen levels, through a negative feedback mechanism, cause the pituitary gland to stop secreting FSH and begin producing LH. 36 years after the LH surge, ovulation occurs. | |
| Photo. The follicular phase of the cycle ends with ovulation. During ovulation, the mature egg and surrounding cells are expelled into the abdominal cavity. The tentacle with fringed petals (the oviduct funnel) is so close to the ovary that under normal conditions it catches every released egg. The former follicle turns into a corpus luteum. During the luteal phase of the cycle, LH secretion promotes the development of the corpus luteum. The corpus luteum secretes estrogens and progesterone, which stimulate changes in the endometrium of the uterus to support early pregnancy. If pregnancy does not occur, then within 9 days the secretion of LH stops, and a scar forms in place of the corpus luteum - the white body. When the corpus luteum persists for a long time, overproduction of progesterone can delay menstruation or cause abnormal bleeding. |
What functions do these organs perform?
The ovaries are a functionally complex organ.
This is due to the fact that it has a fairly strong effect on the woman’s body. Functions:
- Initially this is a function of reproduction. In a woman’s ovaries, germ cells—eggs—are formed, which combine with sperm and the process of fertilization occurs.
- It is also a hormonal product. The most important hormones are formed in the ovary, these are estrogens and progesterone, and in small quantities these can also be androgens. They promote the development and functioning of the mammary glands, prepare the uterine cavity for implantation, and also influence many metabolic processes in the body.
From the first day of the menstrual cycle, the process of growth and maturation of follicles begins under the influence of estrogens. One follicle grows faster than the others. The egg matures in it, and it is called dominant. The growth of other follicles is slowed down. During ovulation, the follicle ruptures and the egg is released. The ruptured follicle transforms into the corpus luteum, which produces progesterone.
Under the influence of sex hormones, the reproductive function of a woman is ensured, and this is only possible with normal functioning of the ovaries. When the egg is fertilized, pregnancy occurs. If the egg is not fertilized, the menstrual cycle will end with menstruation.
A certain number of follicles are formed in the eggs of girls during intrauterine development. Over the entire reproductive period, hundreds of eggs mature, most of which remain unfertilized. When the supply of follicles in the ovaries is depleted, menopause occurs. Normally, menopause occurs at the age of 50.
In these dimensions, menopause can be compared to pathologies.
In women of reproductive age, the normal size of the ovaries has the following parameters:
- organ length – 20-35 mm;
- its width is 15-20 mm;
- thickness – 20-25 mm.
Both organs differ in size. This difference is considered normal. In a forty-year-old woman, the normal weight of one organ is 9.5 g.
The menopausal period has three stages, during which the ovaries change their size. The first stage is called perimenopause. It starts with the first symptoms of menopause - hot flashes, increased sweating, surges in blood pressure, excessive irritability and others. They are provoked by hormonal imbalance, which occurs due to the fact that the ovaries begin to produce fewer sex hormones.
How female genital organs change with age.
During premenopause, the menstrual cycle is disrupted. It becomes shorter or longer, and the number of critical days and the abundance of menstrual flow also changes. Delays are more common in women. First for a few days, and then weeks and months. The amount of menstrual flow decreases and lasts fewer days.
The first changes in the ovaries occur in premenopause against the background of decreased estrogen levels. The number of remaining follicles decreases with each menstruation. The cortex, which previously contained follicles, is replaced by connective tissue.
The ovaries begin to decrease in size to the following parameters:
- length does not exceed 25 mm;
- width no more than 15 mm;
- thickness within 9-12 mm.
The ovaries are constantly decreasing in size. After a few months, both organs become the same size.
During menopause, the last independent menstruation occurs. They can only be established retrospectively. Therefore, the diagnosis of menopause is made 12 months after menstruation, if there has been no menstrual flow. Throughout this year, the ovaries continue to decrease in size.
The following sizes of ovaries at menopause are considered the accepted norm:
- length is in the range of 20-25 mm;
- width – 12-15 mm;
- thickness – 9-12 mm.
Postmenopause is the final stage of the menopause. In postmenopause, menstrual function is completely absent. Many people are interested in what happens to the ovaries, the work of which is completely completed in the female body.
They continue to decrease in size. So, 5 years after the start of this stage, the volume of the ovaries will be approximately 2.5 cm3, and after 10 years - 1.5 cm3. The weight of the organ in a 60-year-old lady normally does not exceed 4 g.
By comparing the measured sizes of the ovaries with the norm, the doctor gives a tentative conclusion about the presence or absence of diseases. Signs of pathology are considered to be a significant increase in volume (it can be twice the normal value), a clear asymmetry in the location of these organs relative to the uterus, as well as a noticeable difference in their size.
Reasons for deviations in dimensions from normal values may be:
- the occurrence of an inflammatory process in the ovaries;
- formation of cysts (one or many, as happens with polycystic disease);
- the appearance of a benign tumor (fibroma, thecoma, adenocystoma and others);
- the presence of a malignant neoplasm (primary cancer or metastases of cancer of other organs).
If the ovaries are reduced, this is due to their depletion (age-related or premature).
By detecting diseases and pathologies in time, it is possible to prevent the occurrence of complications such as twisting of the cyst stalk, rupture of ovarian tissue. Often it is possible to eliminate the causes of infertility. Early detection of tumors and timely surgery can save the patient’s life.
Anatomical changes in the ovaries during the menstrual cycle
The results of ovarian ultrasound in women largely depend on what day of the cycle the study is carried out.
- Days 5-7 – early follicular phase. During this period, the ultrasound should show a white capsule surrounded by follicles. As already mentioned, the number of these same follicles may vary, but their size is more or less standard - about 6 mm.
- Day 10 – middle follicular phase. At this time, a dominant follicle is already noticeable, which stands out from the others, growing up to 15 mm.
- Day 14 – late follicular phase. The growth of the dominant follicle occurs particularly intensively and can reach several millimeters per day.
Factors influencing ovarian size
The function of the ovaries is to release an egg each menstrual cycle and produce two important hormones. At maturity, the eggs mature and are released for fertilization. The eggs reach the fallopian tube to be fertilized by sperm. If fertilization does not occur, it is discharged as blood through the vagina, forming the menstrual cycle. These hormones include progesterone and estrogen. The hormone estrogen is very important for the development of female sexual characteristics and the maturation of reproductive organs such as breasts.
As soon as the follicle increases to 18 mm, ovulation begins. The follicular capsule will burst and release the mature egg. Now, in its place, the so-called “corpus luteum” begins to develop, the main task of which is to block the development of other follicles.
- Day 15 – early luteal phase, size of the corpus luteum – 15-20 mm.
- Day 20 – middle phase. The newly formed body is actively growing and reaches 2.5-2.7 cm in diameter.
- Day 27 – late phase. The corpus luteum fades, decreases to one centimeter, and disappears completely with the onset of menstruation.
This is a standard picture of what can be seen on an ultrasound scan on different days of the month. As the follicle matures and then the corpus luteum grows and dies, the size of the ovary either increases or decreases again. But deviations from the script are also possible. In particular, they are inevitable if fertilization of the egg occurs. In this case, the body does not come out during menstruation, but remains in the ovary and begins to actively grow until the placenta takes over its functions.
Progesterone helps prepare the uterus for pregnancy and maintain a healthy endometrium. Two ovaries have a chance to release an egg every month. In case one of them stops functioning or is removed, the other will continue to supply an egg for each menstrual cycle.
How is an ultrasound performed?
The average size of the ovaries is the size of a Greek olive. You can determine the normal size of the ovary by ultrasound. Let's look at the size of the ovary according to different measurements. Conditions that affect the size of the ovaries. There are many ovarian diseases, such as ovarian cancer and ovarian cysts, that can cause the ovary to become enlarged. An ovarian cyst can cause the ovary to increase in size up to 6 inches in diameter. The size of the ovary may increase if women suffer from corpus luteum cyst, follicular cyst, hemorrhagic cyst or dermoid cysts.
Enlarged ovarian size in pregnant women is normal. The reason for this is increased blood flow in the pelvic area. Moreover, during this period, not only the normal size changes, but also the position of the paired organ - the uterus grows and the ovaries rise up.
What can you find out about the condition of the ovaries from ultrasound?
- Location. The ovaries are located in the abdominal cavity on either side of the uterus. Their location is rarely symmetrical and this is a variant of the norm.
- Form. The ovaries are visible on ultrasound as two oval tonsils. In healthy women they are slightly flattened.
- Size – length, width, thickness, volume. The size of the ovaries is individual for each woman and can change throughout her life. In many ways, these parameters depend on age, hormonal levels, general health, and the number of pregnancies and births. In addition, the ovaries can shrink and enlarge depending on the day of the menstrual cycle. That is why, if any disease is suspected, the doctor will most likely order not one ultrasound examination, but several on different days of the cycle in order to monitor how their size changes.
- Structure. The ovary consists of two layers: outer (cortical) and inner (cerebral). In the outer one, follicles mature, the number of which in the right and left ovaries may be different. On average there are about 12 in each. If the number of follicles is less than 5, there is a pathological deviation on the face.
- External contours. Normally, the surface of the ovary should be lumpy, which indicates the presence of follicles in the outer membrane.
- Echogenicity is the most important ultrasound parameter, indicating the ability of organ tissue to reflect high-frequency sound. It must be homogeneous, otherwise we can talk about the presence of inflammation.
Hormonal role of this organ
The ovaries produce several hormones. Let's look at most of them:
- Progestogens. The key hormone of this group is progesterone. It is produced by the corpus luteum, which forms at the site of a ruptured follicle during ovulation. During pregnancy, the placenta begins to produce progesterone in large quantities.
- Estrogens (estriol, estrone, estradiol). The most active of them is estradiol. These hormones are responsible for the development of the female genital organs, the maturation of the vaginal mucosa, increase the tone of the uterus, etc.
- Androgens. The most well-known androgen is testosterone. When this hormone is in excess, a woman begins to exhibit male sexual characteristics (male pattern hair, etc.).
The synthesis of hormones in the ovaries is controlled by the pituitary hormones according to the feedback principle, i.e. When the level of a certain ovarian hormone increases, the pituitary gland produces an antagonist hormone.
Range of ovarian sizes in healthy women
The size of the ovaries in women of childbearing age can vary within the following limits:
- length – from 20 to 37 mm;
- width – from 18 to 30 mm;
- thickness – from 16 to 22 mm;
- volume – from 4 to 10 cubic meters. cm.
If you carefully study the ultrasound report, you will notice that the sizes of the left and right ovaries may differ significantly from each other. This state of affairs is a variant of the norm. With age, when reproductive function begins to fade, the size of a woman’s uterus and ovaries decreases significantly. As a rule, by the time postmenopause occurs, both parts of the paired organ acquire the same parameters.
The normal sizes of the ovaries in women who have experienced menopause are in the following range:
- length – from 20 to 25 mm;
- width – from 12 to 15 mm;
- thickness – from 9 to 12 mm;
- volume – from 1.5 to 4 cubic meters. cm.
Genital cancer is the second most common cause of death among middle-aged women after breast cancer. Therefore, if you have symptoms such as periodic pain in the uterus and ovaries, discharge, or menstrual irregularities, you should not hesitate to visit an experienced gynecologist. The sooner a tumor in the ovary is detected, the higher the chance of recovery.
This means that the normal size of the ovaries in mm is 15 mm. On the other hand, the normal size of the ovaries in a cubic meter is about 5 cubic centimeters. Women go through a menstrual cycle when they cross the bridgehead of puberty. The menstrual cycle occurs each month when the ovary releases eggs, which travel through the fallopian tube to await fertilization by sperm. When this does not happen, the egg leaks out along with the endometrial lining every month. Thus, this results in a monthly bleeding cycle or periods.
An equally alarming indicator is the reverse deviation from the norm - to a lesser extent, especially for young women of childbearing age. This phenomenon is called “premature menopause” and this means that the ovaries have stopped working at full capacity. Most often, this problem is diagnosed in women 37-40 years old. Even if having children is no longer in your plans, it is dangerous to underestimate the seriousness of this problem. The ovaries are responsible not only for the maturation of eggs, but also for the production of a number of “female” hormones. Premature decline of the functions of this organ is fraught with serious hormonal disruptions in the body.
The ovaries contain an endless supply of eggs, which runs out after menopause
Therefore, they are the most important part of the reproductive system. Without their fertilization, conceiving a child would be impossible
However, ovarian size is not always a cause of concern for infertility issues. In this article, you will learn all about the normal size of the ovaries, their roles and functions.
The ovaries are located on either side of the uterus. They are located in the area of the ovarian fossa in the lateral wall of the pelvis. This region is present below the external iliac artery and opposite the ureter and internal iliac artery. The ovarian ligaments help connect the ovaries to the outer layer of the uterus.
Diagnostic methods
Ultrasound diagnostics with an additional Doppler method of vascular condition will help you find out what is happening to the ovaries. The following may also be carried out:
- CT scan;
- Magnetic resonance imaging.
But these methods are expensive and are not particularly effective, which is why they are used much less frequently than conventional ultrasound.
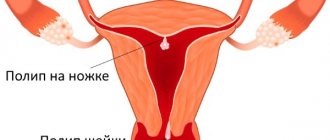
Malignant neoplasms are distinguished by a number of characteristic manifestations that contribute to the detection of a cancerous tumor during ultrasound, these are:
- increase in blood flow speed;
- bilateral localization of the lesion;
- polyp growth.
If an ultrasound examination reveals the presence of a neoplasm, a blood test is prescribed to determine the content of cancer markers. The obtained blood test results, in combination with ultrasound results, provide a more complete clinical picture, on the basis of which the subsequent treatment regimen is developed.
After surgical removal of a tumor in the ovaries, a histological examination of the extracted tissue is performed, on the basis of which a final diagnosis and further treatment are made.
Main functions of the ovaries
At the very beginning of the menstrual cycle, follicles begin to mature and grow. In the dominant follicle, the one that first reaches the required size, the process of maturation of the egg begins, and the development and growth of the remaining follicles slows down and gradually stops completely. At the moment of ovulation it bursts. The egg inside it and the liquid is poured into the peritoneum. It then enters the fallopian tubes. And a scar forms in place of the follicle. The ruptured follicle produces a corpus luteum.
If fertilization occurs, it begins to play the role of a gland. And after childbirth, the corpus luteum regresses and becomes white, and then connective tissue forms in its place. The surface in this place remains rough. If fertilization has occurred, the corpus luteum almost immediately regresses and dissolves.
Please note: It is worth highlighting two main functions of the ovaries - the reproduction of hormones and the maturation of germ cells. For obvious reasons, the main function of the ovaries is reproductive, it allows a woman to conceive and bear a child.
As for hormones, their level in the blood depends on the phase of the cycle. The ovary synthesizes hormones such as progestins, estrogens and androgens (in small quantities).
Despite the fact that women's ovaries are relatively small, their role in the reproductive system cannot be overestimated. The slightest malfunction can lead to serious health problems for the entire body.
We recommend you learn: About menstruation after ovary removal
Conducting research
The ultrasound is performed in the supine position and rarely takes more than 20 minutes. The following stages can be distinguished:
- It is recommended to free the examination area from clothing and lie down on a couch previously covered with a diaper.
- The examination begins with an examination through the abdominal wall, after which the patient should empty her bladder.
- Next, you need to lie on your back again and bend your knees.
- The ultrasound continues using a vaginal probe, onto which the doctor places a condom before starting the procedure.
- After a full examination and clarification of all questions of interest, the patient removes excess gel and awaits the result of sonography.
It is important to listen carefully during the ultrasound and follow the doctor’s requests - this will contribute to a better and faster examination.
How to prepare for an ovarian ultrasound
In the absence of any adverse symptoms, the best time to conduct a routine study is the 5th-7th day of the cycle, which, as a rule, occurs at the end of menstrual bleeding. To get a complete picture, the ultrasound will have to be repeated three times: on days 8, 14 and 22. Be that as it may, studying the ovaries alone is not enough. It is possible to draw up a complete clinical picture only after examining the entire reproductive system, in particular by establishing the normal size of the uterus.
How is an ovarian ultrasound performed? The patient can choose one of three methods.
- Transabdominal. The lower abdomen is lubricated with a special gel, and then a wide sensor is moved. It must be said that this is not the most informative method, since it allows you to see only obvious pathologies.
- Transvaginal. This method is more modern and informative. With its help you can see all the changes that occur in the ovary. To do this, the ultrasound machine sensor is inserted directly into the vagina, but not too deep, so that the uterine os remains intact.
- Transrectal examination. It is carried out through the rectum. This is the only way to examine the pathology of the ovaries in virgins without damaging the hymen.
In order for the ultrasound picture to be as complete as possible, the patient needs to prepare for the procedure in a special way. Thus, before a transabdominal ultrasound, it is necessary to follow a three-day diet, limiting the consumption of foods that cause fermentation in the gastrointestinal tract. This is especially true for cabbage, beans, black bread and soda. It will not be superfluous to take sorbents - Espumisan, Sorbex, activated or white carbon. An hour before the scheduled time of the ultrasound, you need to drink a liter of water, but you will be able to urinate only after the procedure.
Vaginal ultrasound also involves taking sorbent drugs, but the bladder, on the contrary, must be empty. You need to prepare for a transrectal examination even more carefully, getting rid of not only urine, but also feces. 12 hours before the ultrasound you will have to do an enema or use modern laxatives - Guttalax, Senade. Microkisms in the form of rectal suppositories (Norgalax) are suitable.
It happens that none of the above methods manage to see the ovary on the ultrasound machine screen. This can be prevented by severe bloating or severe pelvic adhesive disease. Another reason is the organ’s too small size, which indicates its premature depletion. It may also happen that the ovary will not be in the right place at all - it may be absent due to a congenital pathology or a surgical intervention. In any case, it is too early to draw any conclusions after one failed research attempt. Most likely, you will have to take a course of sorbents and visit the ultrasound room again.
Ultrasound methods
Depending on the reason for the examination, the doctor recommends when it is best to do an ultrasound of the uterus and ovaries: during, after or before menstruation.
Most often, the first examination is scheduled on days 5–7 of the menstrual cycle in order to examine not only the ovaries, but also the uterus. On days 5–7, the uterus has a minimum thickness of the endometrium, which makes it possible to see even minor abnormalities.
In the absence of menstruation, ultrasound diagnostics are performed any day. After the initial examination, repeat procedures may be required. In this case, which day of the cycle is best to do an ultrasound is decided on an individual basis.
For women who cannot become pregnant for a long time, ultrasound is performed every 2-3 days to monitor the maturation of the follicles. Before planned assisted reproductive technologies, ovulation and the state of the corpus luteum are assessed several times per cycle:
- at 8–10;
- at 12–14;
- on days 22–24 of the cycle.
Additionally, watch a video describing in detail an ultrasound examination of the ovaries:
Transabdominal
The transabdominal examination is carried out through the surface of the abdomen. The woman lies down on the couch on her back and frees her stomach from clothes. The doctor uses a sensor to examine the female organs through the anterior abdominal wall.
This method is suitable for initial examination, for screening preventive examinations, as well as for virgin girls. Compared to other methods, this one causes absolutely no discomfort.
Transvaginal
During a transvaginal examination, the sensor is inserted into the vagina, having previously protected it with a condom. The most convenient position for diagnosis is when the woman lies on her back with her knees bent to the sides. The sensor is small in size, so it does not cause much discomfort. Transvaginal examination allows better visualization of female organs.
The transvaginal method is shown more clearly in the video:
Transrectal
The examination of the female organs with a sensor inserted into the rectum is called transrectal. To facilitate insertion of the sensor, the girl should lie on her side and pull her bent knees towards her stomach and relax.
This method is rarely used and is an alternative when examining virgin girls.
Ovarian pathologies in women
To determine the pathological condition or deviations from the norm, the woman is sent for an ultrasound. If everything is normal and the body functions well, then the size of the uterus and ovaries should be within acceptable limits. If on an ultrasound the doctor discovered an enlargement of one ovary by two or more times, then this indicates serious disorders. Also, if there is a deviation in the volume of this organ by 1.5 centimeters or more.
Enlarged ovaries in women, shown on ultrasound, indicate the following diseases:
- Cyst.
- Polycystic disease.
- Benign tumor.
- Malignant tumor.
- Metastases.
In case of serious deviations, purulent condition and overlap, the doctor prescribes urgent surgical intervention. If the patient refuses the operation, then such an act can even lead to death. During an ultrasound, the presence and stage of the disease can be detected. If the tumor has reached significant parameters, then this can end disastrously for the patient. Very often, ovarian cancer can be accompanied by uterine cancer. Therefore, experts recommend regularly undergoing preventive ultrasound of the uterus in order to detect the disease at the initial stage and prevent its development.
Also, a sudden decrease in the reproductive organs of the uterus is not considered normal. Doctors call this condition “premature menopause,” which negatively affects the normal functioning of the reproductive organs. Most often, this pathology is observed in women aged 36-41 years. As for the size of the uterus, they also change slightly - they decrease, and the walls become thinner. Menstruation gradually begins to stop, and then menopause occurs. If this pathology is detected early on an ultrasound, it can be prevented by taking hormonal medications. After such therapy, a woman even has a chance of becoming pregnant.
Every woman is advised to pay attention to even minor changes or pain that may appear in the lower abdomen. If you begin to experience unpleasant sensations during sexual intercourse, you should immediately consult a gynecologist for advice, since the disease is easier to prevent than to treat at the last stage, which can also negatively affect reproductive function, especially at a young age.
Ultrasound of the prostate gland: advantages, types
How to prepare for an ultrasound of the pelvic organs: preparation, features, procedures
When is an ultrasound of the scrotum prescribed, preparation for the procedure, interpretation and risks
Ovarian cysts
One of the most common findings during ultrasound diagnostics of the ovaries. In the ultrasound photo, an ovarian cyst looks like a round, hypoechoic (dark) formation. Their contents can be very different. But the picture obtained by ultrasound cannot always be interpreted unambiguously, since there are several types of cysts, ranging from physiological ones, which disappear without a trace, to malignant cystomas.
The following types are found:
- Luteal and follicular cysts are physiological formations that most often disappear on their own. Only sometimes the rupture of a follicullin cyst can be accompanied by acute pain and requires the intervention of specialists;
- ovarian dermoid cyst - defined as a round-shaped formation with thick walls. Inside it, inclusions are visualized, which are cells of dermoid origin;
- endometrioid (chocolate) cyst, which developed as a result of endometriosis. Characterized by unilateral localization, uneven wall thickness, hyperechoic cyst contents (blood). During menstruation, hemorrhages may occur in the cyst, since the pathological endometrium also changes cyclically;
- polycystic ovaries - with this syndrome, an ultrasound examination of the ovaries reveals multiple cysts. More often detected in young women;
- The most serious finding during ultrasound examination of the ovaries is a malignant cystoma. It is impossible to make a definitive diagnosis using ultrasound. But if an ultrasound scan of the ovaries reveals signs that allow one to suspect the disease: multilocularity, the contents are poorly visualized, invasion into neighboring organs, free fluid in the abdominal cavity. If these stigmata are detected, a targeted examination is necessary - a biopsy.