What is osteoporosis?
Osteoporosis is a systemic disease that affects all bones of the skeleton. Due to the development of pathology, the number of osteocytes significantly decreases, bone mass begins to deteriorate, and all the minerals necessary for bone strength are lost.
All this leads to a high risk of bone damage , including fracture.
Attention! Women are most susceptible to this disorder. Despite the fact that the skeleton of both men and women is formed before the age of 25, female tissue, even in the mature, formed period, is 10–15% thinner than male tissue. The risk of osteoporosis especially increases after the menstrual break.
Diagnosis of osteoporosis: laboratory tests, markers, types of examinations and tests
Decreased bone density is a virtually asymptomatic disease in the early stages. The main task of an orthopedic traumatologist in diagnosing osteoporosis is to objectively assess the patient’s condition. The specialist identifies the fact of pathology, finds the cause of the disease and differentiates bone loss from other similar or concomitant diseases, and makes a prognosis for recovery.
At the doctor's disposal:
- possibility of clinical examination;
- hardware diagnostics (X-ray, ultrasound);
- laboratory diagnostics;
- genetic examination methods.
All of them are aimed at visualizing macro- and microarchitecture and identifying processes leading to a decrease in bone mineral density.
Clinical examination
At the clinical examination stage, the therapist can identify a group with an increased risk of osteoporosis. Among the symptoms of osteoporosis, the doctor can identify kyphotic deformation in the thoracic spine, a noticeable decrease in the patient’s height compared to the previous visit. Clinical markers of osteoporosis also include complaints of back pain. There is a chance to get an appointment with a traumatologist:
- in women with premature menopause;
- in people with a family history of osteoporosis;
- with frequent fractures under the age of 45;
- in patients with diseases that provoke secondary osteoporosis;
- after taking a number of pharmaceutical drugs;
- with extreme thinness – anorexia, exhaustion, congenital thinness with a BMI less than 20.
If a person has two or more risk factors, the likelihood of osteoporosis increases by a third, regardless of age.
Interviewing the client can help identify additional risk factors:
- calcium deficiency in food;
- lack of exposure to sunlight, and therefore a lack of vitamin D;
- problems with the stomach and intestines;
- drinking alcohol and smoking;
- treatment with glucocorticoids or hormones;
- diseases of the glands and internal organs, COPD;
- prolonged immobilization or low physical activity.
Patients with suspected osteopenia or osteoporosis are prescribed further in-depth examination. Often the disease is detected at a late stage by traumatologists in patients with fractures or neurologists in patients with pain in the spine.
An orthopedic traumatologist or neurologist differentiates osteoporosis from bone cancer, trauma, osteomalacia, fibrous dysplasia, Paget's disease, and peripheral neuropathy. Laboratory diagnostics becomes the main basis for decision-making in this case.
The following “clinical myths” serve as an obstacle to early detection of the disease:
Diagnostic methods
More than 70% of bone strength is provided by mineral density (BMD), the remaining 30% is redistributed between mineralization, metabolism, macro- and microstructure, and microdamage. It is important to identify all defects in the early stages of the disease. For this purpose, a number of methods for diagnosing osteoporosis have been developed.
Most often, osteopenia and osteoporosis are detected using conventional x-rays in the presence of bone fractures or spinal deformities. At this stage, more than a third of bone mass has already been lost. You can influence the process when we are talking about losses of up to 5%. Therefore, for the early detection of osteoporosis, there are more accurate methods:
- ultrasonic;
- isotope (mono- and biphoton absorptiometry);
- mono- and bioenergetic absorptiometry (DXA);
- quantitative computed tomography;
- blood chemistry;
- genetic studies of materials.
Rules for formulating the diagnosis of AP
Ultrasound
Analysis of the mineral composition of bones using ultrasound can identify areas of reduced density. This test for osteoporosis is based on the reflection of ultrasound beams from dense organs. The introduction of ultrasound devices into clinical practice makes it possible to assess the mechanical properties of bone tissue. Strength and elasticity create a hyperechoic image structure.
The testing site for ultrasonic densitometry (UD) is usually the heel bone and the tip of the index finger. Practice shows that this study is more suitable for screening. It is recommended to undergo it once every 5 years for early detection of the problem for women over 45 years of age and men over 50.
Radiodensitometry
An accurate diagnosis is established by examining certain areas of the skeleton using bioenergetic absorptiometry, which is considered the “gold standard” for diagnosing osteoporosis. Dual-energy X-ray absorptiometry aims to measure BMD. Diagnosis is carried out for the entire skeleton, vertebrae, paired sections or one bone. The device compares the received image with the reference ones and produces two indicators, T and Z.
The T-index indicates deviations from the peak bone density of an adult, and the Z-index indicates deviations from the norm for a given age. Normally T=1. Osteopenia is diagnosed at T from -1 to -2.5, lower mineral density is classified as osteoporosis. If the patient has a history of a fracture with a T less than -2.5, then osteoporosis is called severe. A one-unit decrease in BMD doubles the risk of fracture. The norm for the Z indicator is also equal to 1. Additional examinations are prescribed if there are significant deviations of Z to a greater or lesser extent. If measurements are carried out in several areas, then attention is paid to the worst and average indicators.
Bone loss affects the entire human skeleton, although unevenly. BMD is determined in places where fractures occur most often. This:
- lumbar vertebrae;
- femoral neck;
- distal forearm.
Postmenopausal women will likely have their vertebrae assessed, while older adults (over 65 years) will likely have their proximal femoral BMD measured. DXA is prescribed for the initial diagnosis of osteoporosis and evaluation of the effectiveness of therapy. The examination is repeated after a year.
The examination is not dangerous to health, since the radiation intensity is 400 times less than with a regular x-ray. The only contraindication may be pregnancy.
DXA does not require any special preparation. It is better not to take calcium supplements the day before. The physician is informed of recent barium examinations. After scanning the selected area, the patient receives images and a conclusion.
The DXA method has some limitations, which are compensated for by additional research.
CT densitometry
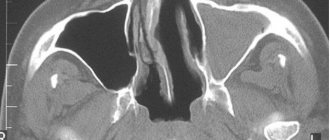
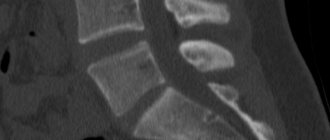
Using computed tomography, it is possible to determine reduced tissue density and obtain a three-dimensional image of the anatomical structure of a skeletal area. The study allows us to study the trabecular structure of the bone.
For examination using computed tomography, a peripheral scanner with a thin beam is used to determine the mineral composition of the tissue. The analysis is called CT densitometry and allows you to determine local changes in mineral composition.
MRI to determine bone density
Magnetic resonance imaging was discovered in 1946. The study makes it possible to obtain a three-dimensional image of organs by recording a radio signal, which is obtained due to the vibration of hydrogen atoms of aqueous tissues in a magnetic field. For this discovery, scientists received the Nobel Prize.
MRI is rarely used to diagnose diseases, although its possibilities are endless. The analysis allows you to see the trabeculae of the bones very clearly. This property was used to create densitometers - devices for determining the degree of osteoporosis.
Single publications in the literature indicate the high effectiveness of the study in determining the density of the bone structure. Obviously, MRI can be used to check the structure of organs. However, the test is rarely used due to the high cost of the procedure.
Laboratory research
The causes of bone loss, like osteoporosis itself, are not obvious. To identify them, you will need to conduct a biochemical blood test and genetic tissue studies. The first one is needed for:
- carrying out preventive measures in cases with metabolic disorders of bone tissue remodeling and resorption;
- predicting the rate of bone loss;
- assessing the effectiveness of therapeutic methods.
At this stage of diagnosing osteoporosis, osteomalacia, bone metastases, and hereditary diseases are excluded, the causes of secondary osteoporosis are identified, and metabolic features are established.
In this case, doctors use three groups of biochemical markers of pathology:
- Markers of bone tissue formation.
Sources used: spinazdorov.ru
Diagnostic methods
X-ray examination of osteoporosis can be done using several methods. To begin with, the specialist prescribes an image of the patient’s spine in three projections. After this, it is recommended to take an x-ray of the pelvic bones, cranial bone tissue, hand and feet . Such manipulations make it possible to assess the degree of transparency of the bone, and therefore its demineralization, as well as the shape of the vertebrae.
Attention! Most radiologists insist that simple images are not enough to make an accurate diagnosis . The study of the transparency of the resulting x-ray is a subjective assessment of a specialist. One can speak with complete confidence about the development of osteoporosis only when the shape of the vertebrae changes and there is a pronounced reduction in bone.
For better diagnosis, more accurate methods have now been developed to determine the degree of bone mass. These include: radionuclide radiography, the use of contrasts and absorption methods . These techniques are more invasive and expensive, but at the same time they give a comprehensive result after the manipulations.
Indications and contraindications for radiography
With osteoporosis, pathological changes occur in the body, which cause the development of symptoms characteristic of this disease. These signs are an indication for examination and diagnosis to confirm the diagnosis.
Indications for radiography for osteoporosis are:
- Pain in the lower back and bones, feeling of constant fatigue and pain when moving.
- Frequent fractures even after minor injuries and bruises.
- Thyroid diseases.
- Violation of the production of sex hormones.
- Stage of menopause.
- Decrease in human height.
- Deformities of joints and spine.
- Genetic predisposition to osteoporosis.
Contraindications to radiography:
- severe general condition of the patient;
- pregnancy;
- open bleeding;
- pneumothorax;
- active tuberculosis;
- severe damage to the liver and kidneys;
- decompensated diabetes mellitus.
Signs of osteoporosis in the picture
To diagnose the disease using X-ray, it is required that the bone tissue has lost at least 40% of the total amount. Such diagnostic difficulties are associated with the characteristics of the human body. The speed of detecting pathology is influenced by the thickness of the patient’s fat and muscle layer, the quality of equipment and consumables, as well as the qualifications of the radiologist.
Main features:
- Visible decrease in shadow intensity.
- The presence of increased transparency on x-rays.
- Bone necrosis.
- A noticeable decrease in the size of the periosteum.
- Reduction or absence of transverse striations of the spinal rings.
- Calcification of the aorta.
Attention! Even with a severe severity of the disease, x-rays are only the starting stage in diagnosing osteoporosis. For a more accurate diagnosis, other more highly specialized examinations are needed.
Benefits and Risks of Bone X-Rays
Advantages:
- Bone x-rays are the fastest and most affordable way to image and evaluate bone and joint conditions such as fractures and arthritis.
- X-ray equipment is relatively inexpensive and is available in most emergency departments, diagnostic centers, clinics and other institutions, making X-rays convenient for both patients and physicians.
- Since X-ray examination is quick and easy, it is particularly useful for the diagnosis and treatment of emergency conditions.
- After completion of the examination, no radiation remains in the patient’s body.
- When used for diagnostic purposes, X-rays do not cause any side effects.
Risks:
- With excessive exposure to X-ray radiation on the body, there is always an extremely small risk of developing malignant tumors. However, the benefits of accurate diagnosis significantly outweigh this risk.
- The effective dose of radiation for bone x-rays varies.
- A woman should always tell her doctor or radiologist about the possibility of pregnancy.
A few words about reducing the effects of radiation on the body
During an x-ray examination, the doctor takes special measures to minimize radiation exposure to the body while trying to obtain the best quality image. Experts from international radiological safety councils regularly review radiology standards and produce new technical recommendations for radiologists.
State-of-the-art X-ray machines allow you to control the dose of X-ray radiation and provide filtration, which minimizes beam scattering. In this case, the patient’s organs and systems that are not examined receive a minimal dose of radiation.
Up
The degree of manifestation of the disease in the image
Like any disease, bone tissue pathology has its own degrees of severity.
Today, experts distinguish the following degrees of pathology:
- 0 degree , which is accepted as a conditional norm, since it is impossible to identify existing possible deviations in the image;
- 1st degree , at this stage the bone tissue density already noticeably decreases and trabecular reduction is visible;
- 2 degree , in which the trabeculae are already greatly thinned, the bone tissue has thinned by 40–50%;
- 3rd degree , in which the bone has decreased in volume by more than 50%, the supporting platforms of the spinal bodies are clearly depressed, the vertebrae become wedge-shaped;
- 4th degree , characterized by advanced osteoporosis, due to the appearance of a large number of wedge-shaped vertebrae and a pronounced loss of essential bone minerals.
Attention! In addition to the signs in the image, the patient in life will face such unpleasant consequences of osteoporosis as severe back pain and concomitant pathologies of the lower and upper extremities. The chance of a bone fracture increases significantly, especially in old age.
Information content of X-rays for osteoporosis
Bone tissue is one of the most accessible for study using radiography. But if osteoporosis is suspected, changes can be detected in the image only if more than a third of the bone mass is lost. This is a fairly late detection of the disease.
For the initial detection of osteoporosis, standard radiography is not suitable, but it is mandatory if spinal fractures are suspected . Indications for examination are:
- the appearance of back pain after 50 years or in patients with other significant risk factors (use of prednisolone, diabetes mellitus, menopause);
- previously diagnosed osteoporosis;
- falling from one's own height;
- lifting weights;
- previous injury or illness with a long period of immobility;
- decreased growth;
- stoop, roundness of the thoracic spine.
Decreased bone density may be indicated by:
- disappearance of the bone pattern or its depletion;
- thinning of the cortical layer;
- contour contrast;
- symptom of an empty, glassy bone;
- growth of bone tissue along the edges of the vertebra, deformation.
The most distinct changes are noticeable in the porous (spongy) substance. You can set the sequence of their appearance. The first to resorb are those bone beams that are auxiliary. In this case, the main direction of loads (vertical) even acquires a reinforced pattern.
Mechanism of development, causes and classification of bone osteoporosis
“Osteoporosis of bones” is translated from Greek as “porous bones.” With the development of this pathology, the bones of the skeleton become thinner and become very fragile. Most often, this disease occurs in women during menopause and in elderly patients.
Mechanism of disease development
Women suffer from osteoporosis more often than men
A decrease in bone density and strength develops due to the loss of calcium, the main structural unit of bone tissue. As a rule, this condition occurs due to hormonal imbalances. With the restructuring of the endocrine system in the thyroid gland and adrenal glands (endocrine glands that regulate mineral metabolism), degenerative-dystrophic changes develop. As a result, calcium deficiency occurs in the blood (hypocalcemia), and it begins to be washed out of the bone tissue. Previously hard and dense bones become brittle and cellular, which is why they are no longer able to support a person’s weight. This disease is characterized by an asymptomatic course, and therefore its existence is often learned only after a fracture occurs. Osteoporosis is diagnosed much more often in women than in men. As a rule, this condition causes menopause, during which there is a sharp decrease in estrogen levels, leading to bone destruction.
Causes of the disease
- Improperly balanced diet (insufficient calcium intake).
- Treatment with glucocorticoids or radiation therapy.
- Physical inactivity, prolonged bed rest.
- Inability to absorb calcium in the gastrointestinal tract, associated with various pathologies of the digestive system.
- Genetic predisposition.
- Insufficient synthesis of vitamin D in the body.
- Also, the causes of osteoporosis include a lack of sex hormones (a condition that occurs in women during menopause).
- Aging of the body.
If, due to one of the listed reasons, there is a suspicion of the development of the disease, you should immediately consult a doctor. Not many patients know which doctor treats osteoporosis, and therefore, before seeing a professional, they have to visit many offices. As a rule, orthopedists and rheumatologists deal with this pathology. However, in order to find out the true cause of the development of the disease, a person requires a comprehensive, comprehensive examination, which involves the involvement of related specialists.
This condition develops when there is a lack of calcium and other minerals, and it can also result from a deficiency in hormone production and a lack of vitamin D.
Types of osteoporosis
Systemic osteoporosis is a skeletal disease characterized by a decrease in bone density and disruption of its micro-architecture. This condition leads to decreased bone strength and increases the risk of fractures. This pathology, as a separate nosological form, was identified in 1941. Together with osteomalacia, hyperparathyroid osteodystrophy and Paget's disease, it is included in the group of metabolic osteopathies. Today, more than 200 million people suffer from systemic osteoporosis. This is a social disease characteristic of a developed society. Moreover, the more developed it is, the higher the percentage of the likelihood of osteoporosis. In clinical practice, primary and secondary osteoporosis occurs. Primary forms of osteoporosis include postmenopausal, idiopathic, senile and juvenile osteoporosis. Secondary osteoporosis is a pathology that occurs against the background of some other disease, or develops after long-term use of certain medications. Most often, the disease affects people with chronic renal failure or hormonal disorders (diseases of the adrenal glands, thyroid and parathyroid glands). With long-term use of corticosteroids, steroid osteoporosis develops.
Note: this form of pathology can also be a consequence of diseases in which there is increased secretion of corticosteroids by the adrenal glands (Cushing's disease).
At the same time, the development of a secondary form of osteoporosis in some cases occurs while taking anticonvulsants, barbiturates and thyroid hormones. With the development of malignant neoplasms, diffuse osteoporosis of the spine very often occurs. This condition is characterized by severe bone pain, but pathological fractures do not always occur.
Primary osteoporosis
- Postmenopausal osteoporosis is one of the most common forms of the disease. At the present stage
Even minor injuries lead to fractures
Forms of bone loss in osteoporosis
Rarefaction of bone translated from Latin means rarefaction. This chronic process has no clinical manifestations in the early stages. When diagnosing osteoporosis, an X-ray image shows increased transparency of bone tissue. With diffuse changes, uniform bone transparency, thinning of the cortical plates and blurred trabecular pattern are observed. Against this background, spongy bones look denser. Patchy osteoporosis is the second form of bone loss. It is characterized by the presence of foci in which a decrease in bone tissue density is observed. Such areas have different shapes and sizes with characteristic blurred contours. In this case, the cortical layer does not change, and the trabecular pattern, unlike the norm, becomes more widely looped.
Note: bone size does not change in both diffuse and patchy osteoporosis.
Clinical manifestations
During the development of the pathological process, slow bone loss and deformation of the vertebrae occur. This condition can be asymptomatic for a long time. This is why in medicine osteoporosis is sometimes called the silent disease. In the case when compression of the vertebrae (one or more) occurs in the affected part of the spine, acute and intense pain appears. At the same time, the patient’s motor function is sharply limited, which leads to painful suffering, and often to severe depression. Very often the disease occurs against the background of rib fractures with characteristic pain in the chest area. Pain in osteoporosis occurs due to the formation of small bone micro-fractures and due to irritation of periostitis. Aseptic necrosis of the femoral heads (one of the most characteristic signs of osteoporosis) often leads to gait disturbance (duck gait). However, in patients suffering from osteoporosis, there is a decrease in height (from two to fifteen centimeters). In this case, there is an increase in thoracic kyphosis and anterior tilt of the pelvis is observed.
Diagnosis and classification of osteoporosis by radiological signs
The most common method for diagnosing the disease is a visual assessment of radiographs taken in various parts of the skeleton. According to radiological signs, osteoporosis is divided into small, moderate and pronounced:
- Mild osteoporosis is a condition in which there is a decrease in bone density, an increase in transparency is observed, an x-ray shadow is detected, and the vertical trabeculae of the vertebrae are roughly striated.
- Moderate osteoporosis is characterized by decreased bone density. In this case, the platforms of the vertebral bodies become biconcave, and a wedge-shaped deformity of one vertebra is also noted.
- Severe osteoporosis is accompanied by a sharp increase in transparency. At this stage, the vertebrae become “glassy” and a wedge-shaped deformity is noted in several vertebrae.
Note: Osteoporosis can only be accurately diagnosed using x-rays when twenty to thirty percent of bone mass has already been lost.
The qualifications of a radiologist play an important role in diagnosing osteoporosis.
Quantitative bone densitometry methods are currently used for early diagnosis of the disease. This technique makes it possible to detect osteoporosis even with a loss of 2–5% of bone mass. With the development of densitometry, specialists have the opportunity to assess the dynamics of the disease and the effectiveness of treatment. Densitometric examination of bones is carried out only when indicated. It is most often recommended for postmenopausal women (up to 65 years of age) who have a history of fractures, as well as men over 70 years of age (with characteristic risk factors), and patients who have suffered osteoporotic fractures (occurring with a low level of trauma). This study is indicated for people with low bone mass, as well as for those patients who experience significant bone loss while taking certain medications.
Sources used: znak-zdorovya.ru