Combinations of coprogram analysis results
Starch is a complex type of carbohydrate that enters the body mainly from plant foods.
Under the influence of salivary enzymes and pancreatic secretion, starch is converted into glucose, which is easily absorbed by the body. Starch elements may appear in feces due to malfunctions of the digestive system when the breakdown process is disrupted.
Normally, a small amount of starch grains in the stool is acceptable, but a large amount of them is an alarming symptom and is called amilorrhea.
Amilorrhea can occur in young children, adults, and the elderly. To understand the reasons for the occurrence of an alarming sign, you need to understand how starch is absorbed by the body.
The breakdown process begins in the oral cavity under the influence of amylase, a digestive enzyme found in saliva.
Passing further through the gastrointestinal tract, starch continues to be digested in the small intestine, where, under the influence of secretions secreted by the pancreas, it must be broken down into glucose. In the small intestine, the absorption process must be completed.
Small amounts of starch grains in feces can be detected when:
- a person eats too much food of plant origin - starch may not be fully absorbed;
- starch-containing preparations were taken the day before;
- disturbances in the functioning of the gastrointestinal tract develop. For example, with diarrhea caused by poisoning.
During diarrhea, the beneficial substances simply do not have time to be completely absorbed, and therefore starch is not completely absorbed.
The causes of severe amilorrhea can be:
- inflammatory processes in the intestines (enteritis);
- pathologies of the pancreas (pancreatitis or atrophy);
- diarrhea of various etiologies;
- fermentative dyspepsia;
- different types of gastritis.
There are different types of starch. By determining which one was found in the stool, you can roughly identify the location of the problem.
Fruits and vegetables contain so-called intracellular starch, which is located inside the cells and is protected by a membrane that breaks down during digestion, releasing the carbohydrate.
Its presence in human feces indicates that food is not digested enough and passes through the gastrointestinal tract too quickly.
Extracellular starch detected in feces suggests problems “at the level” of the stomach (decreased quantity or quality of gastric juice) or reveals a lack of amylase in saliva.
How to donate stool?
Test results largely depend on proper sample preparation and collection. So how to donate feces? There is nothing complicated in the procedure. To collect samples, it is recommended to purchase a special plastic container with a lid. Such containers are sold in almost any pharmacy. They are equipped with a convenient spatula for collecting feces.
Before the procedure, you should wash, otherwise during the study, uncharacteristic bacterial organisms, epithelial cells, and chemical compounds may be detected, which, naturally, will affect the further diagnostic process. The collection is carried out immediately after defecation.
According to laboratory technicians, a complete analysis requires one teaspoon of material. Smaller samples may not be sufficient to perform all tests. Feces should be sent to the laboratory as quickly as possible - no later than 5-7 hours after collection. The longer the biomaterial is stored, the less likely it is to obtain accurate results, because under the influence of environmental factors (light, temperature, air) some chemical components of feces are destroyed, which leads to distortion of information. It is best to store the sample container in the refrigerator.
If a coprogram is carried out on a baby, then parents are not recommended to collect feces from the diaper - it is better to first place a clean diaper under the baby. If a special plastic container is not available, samples can be placed in a glass jar, but it must first be sterilized.
Causes of amilorrhea
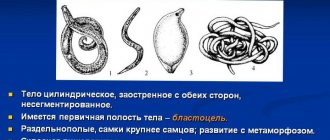
Starch is a complex carbohydrate that enters the body mainly with plant foods. Its breakdown begins already in the oral cavity at the time of chewing food, under the influence of the amylase enzyme contained in saliva. Further digestion of starch continues in the small intestine, where amylase from pancreatic juice acts on it. Ultimately, starch is broken down into simple sugars, which enter the blood.
Normally, stool should not contain starch, however, its appearance does not always indicate a disease.
The reasons for the appearance of starch in stool in children and adults can be:
- significant consumption of starch-rich foods;
- diarrhea (in this case, starch does not have time to break down into glucose due to the too rapid movement of chyme through the intestines);
- acute or chronic enteritis;
- acute or chronic pancreatitis;
- pancreatic atrophy;
- fermentative dyspepsia.
Vegetables and fruits contain starch inside their cells. When chewed and in the stomach, under the influence of gastric juice, the cell membranes are destroyed, which promotes the release of starch grains to the outside.
The detection of extracellular starch in the stool indicates amylase deficiency or too rapid movement of the bolus of food through the intestines. The presence of intracellular starch in the feces of an adult or child indicates possible pathologies of the stomach, which are accompanied by a decrease in its secretory function.
Normal indicators
Only the attending physician can establish normal values for the content of detritus in feces. At the same time, the isolated use of a criterion or coprogram to establish a final diagnosis is unacceptable. A comprehensive examination, in addition to laboratory diagnostics, should be accompanied by ultrasound of the abdominal organs and gastroscopy.
In most cases, detritus in the coprogram is also detected normally, which explains such a wide spread of acceptable criterion values in the analysis results from small to significant. As a rule, healthy children and adult patients show a moderate content of detritus in the biomaterial being studied.
A complete digestion process involves the release of undigested and digested remains of the food bolus. At the same time, representatives of the intestinal microflora are also isolated, which is a variant of the physiological norm.
Connective tissue in stool
Not detected – During normal digestion, connective tissue is not detected in the stool.
Detected - The presence of meat food residues indicates insufficient function of the digestive glands, or an excess of meat in the diet. The connective tissue may visually resemble parts of helminths, thick mucus, or a fungal infection. Microscopy gives an idea of the structure of connective tissue fibers. Children who receive meat feeding before the age of one year have a large amount of undigested muscle fibers in their feces.
general description
The smallest particles of processed food, altered cells and bacteria are called detritus. Looking at them under a microscope, you can see structures of different sizes and completely shapeless. They resemble grains, their contours are unclear. The nature of the appearance of detritus cannot always be determined.
With normal digestion, stool will always have a few small particles. Their appearance, processing and crushing are facilitated by microorganisms living in the intestines. Detritus is also the remains of epithelial tissue that exfoliate from the intestinal walls, blood cells and mucus clots. Each of these elements changes and becomes similar to the others. If a person adheres to a balanced diet, then the feces will contain a large amount of detrital formations. With loose stools, there will be few small particles.
Detrital matter is formed under the influence of secretory secretions produced in the digestive system. Many have not encountered such a concept as detritus. What is it? In simple terms, these are the smallest remnants of food digested by the body, thanks to which one can judge the well-coordinated functioning of the digestive system.
Diagnosis of amilorrhea
The presence of undigested starch grains in stool is detected during a general stool analysis. In a normal coprogram, starch, as well as leukocytes, red blood cells, proteins, bilirubin and mucus, should be absent.
Amilorrhea is not an independent disease. Its appearance can be caused by many factors. For example, the presence of undigested starch in children of the first years of life (1-2 years) is explained by the physiological immaturity of their digestive system, therefore, in this case, amilorrhea is not a pathology.
If older children and adults eat too many vegetables and fruits, as well as other foods rich in starch (jelly, baked goods, cereals), they also often have undigested starch grains in their stool. And in this case, this is not immediately considered as an unambiguous sign of pathology.
- repeat general stool analysis;
- bacteriological examination of stool;
- stool examination for dysbacteriosis;
- ultrasound examination of the pancreas, liver and gallbladder;
- FEGDS (fibroesophagogastroduodenoscopy);
- determination of gastric juice acidity.
When collecting stool for testing for starch content (as part of a coprogram), it is important to follow the rules for preparing, collecting and storing the material. Their violation can cause false results, as a result of which the correct diagnosis of diseases of the digestive system is difficult and the prescription of appropriate treatment is delayed.
Amilorrhea is not an independent disease. As a rule, pathology is a complication of an existing disease.
As such, amilorrhea indicates changes in the functioning of the gastrointestinal tract and is a specific diagnostically important sign.
By identifying it in a stool analysis, a specialist, based on the symptoms combined with amilorrhea, can make a diagnosis and, if necessary, prescribe treatment.
Starch grains in feces are detected during a scatological examination - scatology.
Coprology is a type of analysis that allows you to collect a large amount of information about the functioning of the digestive tract in a short time, based on studying the characteristics of feces.
This is a routine test that is performed for diagnostic purposes to identify or differentiate new symptoms.
Scatological tests determine the presence of starch, blood elements, infection, signs of parasites in the body, and much more. The doctor conducts a visual examination of the stool and checks its characteristics using certain techniques.
The stool should not contain mucus, undigested food elements, drops of blood, bilirubin, proteins, white blood cells or starch. The pH reaction is normally neutral.
These are standard parameters checked by a laboratory assistant during a scatological examination, but sometimes there is a need to place emphasis in order to clarify the diagnosis.
For example, if tests are taken to examine stool for carbohydrates, then the specialist not only notes the presence of starch in the stool, but also studies whether the starch belongs to a certain type.
In adult stool, starch is usually a serious symptom of developing diseases.
Research methods
Microscopic analysis of stool
Analysis of stool - a coprogram is carried out by microscopy, the fragment is ground between glass slides and its composition is assessed. If the feces are too thick, add a small amount of water or sodium chloride solution and grind it with a glass rod until a smooth consistency is obtained.
To identify iodophilic microflora, crystals of fatty acids, drops of neutral lipids, staining reagents are used that change the color of the pathological component.
In microscopic analysis of feces, detritus constitutes the main background and is a mass of granular components. The more complete digestion of food occurs, the more detritus there will be and the fewer differentiated elements there will be.
When decoding the results of the coprogram, organoleptic and physico-chemical indicators are indicated. Based on the data obtained, the doctor evaluates the properties of feces, identifies pathological inclusions indicating the development of any disease of the intestinal tract, changes in acidity, microflora and the total volume of digested food fragments.
Muscle fibers are unchanged
Not detected - Normally, with sufficient activity of the digestive glands, muscle fibers are absent in the feces.
Found – Insufficient activity of gastric juice or pancreatic enzymes does not allow the gastrointestinal tract to digest muscle fibers (meat). The presence of unchanged (striated) fibers is a symptom of acute pancreatic insufficiency, for example, with pancreatitis. Children who receive meat feeding before the age of one year have a large amount of undigested muscle fibers in their feces, since at this age the pancreas is not yet fully formed.
Few detected - Normally, with sufficient activity of the digestive glands, muscle fibers are absent in the feces. With an excess of meat food in the feces, altered muscle fibers may be present in small quantities and the normal activity of the digestive glands is maintained.
Many were found - Insufficient activity of gastric juice or pancreatic enzymes does not allow the gastrointestinal tract to digest muscle fibers (meat). With partial activity, altered, unstriated muscle fibers, partially digested, are found. This indicates the preservation of the pancreas, but may indicate the presence of inflammation (pancreatitis).
Physical characteristics of feces: what do deviations indicate?
Before starting to study the chemical composition of feces, the laboratory assistant must study and enter physical characteristics into the questionnaire. They are no less important for creating a high-quality coprogram.
By the way, the patient can only note some disorders independently. For example, there are average statistical norms for the daily amount of feces. For an adult, this is 100-200 g. Naturally, we are talking about those cases when the patient follows the correct diet:
- the release of less than 100 g of excrement per day is observed with constipation of various origins;
- more than 200 g often indicates inflammation of the intestinal mucosa, accelerated evacuation of food masses, and insufficient supply of bile;
- If a person excretes more than 1 kg of excrement per day, this indicates serious pancreatic insufficiency.
Another important factor is consistency. Feces are 80% water. With diarrhea, this figure increases to 95%, but constipation is accompanied by a decrease in the amount of fluid to 70-65%. Normally, the stool of an adult is formed and has a dense consistency. What the analysis can tell you:
- abundant semi-liquid feces with oily impurities may indicate impaired absorption of fat in the intestines;
- pasty stool appears when there is insufficient amount of bile and secretion disorders in the pancreas;
- loose, mushy excrement indicates increased fermentation processes, colitis, enteritis;
- liquid feces appear when digestive processes in the small intestine are disrupted;
- solid feces of a ribbon or spiral shape are observed with constipation, hemorrhoids, as well as with the formation of tumors in the colon;
- semi-liquid, foamy feces are characteristic of fermentative colitis and irritable bowel syndrome.
An important factor for diagnosis is the color of the stool:
- light brown stool indicates accelerated evacuation of intestinal contents;
- reddish feces are observed with inflammation and ulceration of the mucous membrane of the colon;
- with disorders of motility and digestion in the small intestine, patients often note that the stool becomes yellow;
- white stool may indicate blockage of the bile ducts;
- With diseases of the pancreas, stool may acquire a gray or yellow-gray tint.
As for other signs, they also pay attention to the smell. Naturally, it depends primarily on food and the amount of protein foods consumed. This is a subjective factor, although it should not be ignored. For example, the presence of a sour odor may indicate fermentative dyspepsia.
It is worth understanding that physical characteristics directly depend on nutrition. That is why, a few days before the test, it is recommended to switch to simple, healthy foods. Overeating, a strict diet, the use of dyes and preservatives - all this can distort the results.
After studying the physical parameters, the laboratory assistant proceeds to study the chemical composition of feces. So, what should not be present in human excrement and what pathologies can be detected using this analysis?
- A bad sign is the presence of protein in stool samples. Its presence may indicate enteritis, dysbacteriosis, ulcerative lesions of the digestive tract, gastritis, cancer, rectal fissures and hemorrhoidal formations.
- Hemoglobin is a component of red blood cells that is absent in healthy human stool. The test for occult blood is positive for ulcers, bleeding in any part of the digestive tract (including the oral cavity), the formation of polyps and hemorrhoids, and hemorrhagic diathesis.
- Stercobilin is a substance that is formed during the breakdown of hemoglobin molecules. A decrease in its amount indicates pancreatitis, hepatitis, cholangitis, and liver damage. But its increased content in feces is observed in hemolytic anemia.
- Bilirubin is found in the stool of an adult in severe forms of dysbiosis, as well as increased intestinal motility. By the way, this element may be present in children in the first year of life.
- The presence of leukocytes indicates an inflammatory process, in particular ulcerative colitis, dysentery, cancer, and tuberculosis of the large intestine.
- The presence of mucous impurities in the stool sometimes indicates the presence of an infection in the intestines.
- If the stool contains a large number of muscle fibers, this may also indicate a number of pathologies, including dyspepsia, constipation, ulcerative colitis, impaired bile flow, and failure of the digestive processes.
- Digestive disorders in the small intestine, insufficient supply of bile, putrefactive and fermentative dyspepsia are accompanied by the release of fatty acids along with feces.
In addition, stool analysis helps diagnose parasitic diseases. Feces may contain eggs, larvae or segments of helminths, as well as Giardia, dysenteric amoebas and other pathogenic microorganisms.
Treatment of amilorrhea
It is worth fixing the problem based on the existing problems. Amylorhea itself is not dangerous, but only suggests that pathological processes are occurring in the body and that beneficial substances in the gastrointestinal tract may be absorbed in insufficient quantities.
First of all, it is worth dealing with the root cause that caused the alarming symptoms. If pathologies of the digestive system have become a negative factor, then the emphasis in therapy will be on treating the underlying disease.
Thus, the course of therapy depends on the primary pathology - pancreatitis, dysbiosis, gastritis, dyspepsia or any other disease identified by the doctor.
Since in children of the first years of life the presence of starch grains in the stool is a variant of the norm, no treatment is prescribed for them.
If amilorrhea is caused by an excess of carbohydrate foods, then the patient is prescribed a therapeutic diet. Products with a high starch content are excluded from the menu:
- legumes;
- cereals;
- nuts;
- pasta;
- potato;
- all types of baked goods;
- jelly.
In addition, it is necessary to limit the consumption of the following vegetables: carrots, beets, pumpkin, zucchini, eggplant, cauliflower, apples, melon, strawberries.
The recommended diet includes milk and dairy products, eggs, cucumbers, tomatoes, white cabbage and lean meat.
It should be taken into account that some unscrupulous manufacturers use starch as a thickener in the production of dairy products (yogurt, sour cream, ice cream). Therefore, if a child or adult is diagnosed with a severe malabsorption of starch, then it is better to refuse to purchase these products in stores and prepare them yourself.
Amylorhea may be caused by a diet containing large amounts of starchy foods.
Drug treatment is prescribed only when amilorrhea develops against the background of pathology of the digestive system. Therapy is aimed at treating the underlying disease that caused insufficient absorption of starch. Depending on the indications, the patient is prescribed drugs of the following groups:
- enzyme agents;
- eubiotics, pro- and prebiotics;
- Acidin-pepsin;
- antidiarrheals;
- anthelmintic drugs;
- bacteriophages.
In addition to drug treatment, diet therapy is indicated.
Reasons for changes in detritus indicators
Deviations in detritus levels in feces can result from:
- production of gastric juice in insufficient quantities;
- introducing unusual foods into the diet;
- decreased immunity;
- an increase in the population of pathogenic microorganisms in the gastrointestinal tract;
- diarrhea;
- infectious diseases;
- constipation;
- inflammatory processes occurring in the gastrointestinal tract.
The amount of detritus may change due to the development of diseases such as pancreatitis, ulcerative colitis and gastric ulcers, cholecystitis, the presence of gallstones, enteritis, Crohn's disease, gastritis or dysbiosis.
Soap
Not detected – Normal
Soaps, digestible fiber, unchanged muscle fibers, modified fibers, starch, bilirubin, neutral fat, fatty acids - Soaps in combination with unchanged and modified muscle fibers, fiber and starch are a sign of accelerated passage of food through the gastrointestinal tract, for example, in case of intestinal infection, poisoning , enhanced peristalsis.
Soaps, fatty acids, neutral fat - Lack of normal activity of the pancreas, a decrease or absence of bile secretion leads to the appearance of neutral fat, fatty acids, and soaps in the feces.
Deviation from the norm
What changes in the indicator under consideration indicate pathology? If the amount of detritus is of no diagnostic value, then its qualitative characteristics are of decisive importance and indicate various diseases of the gastrointestinal tract. Examples of deviations from the physiological norm:
- a large amount of undigested fiber in combination with detritus indicates a disruption of the biliary tract and the act of digestion in the small intestine, often accompanied by constipation;
- mucus or in detritus - a sign of an infectious disease or dysbacteriosis (disturbance in the composition of normal intestinal microflora);
- the predominance of destroyed bacterial and epithelial cells is observed in acute inflammatory processes;
- the absence of detritus in combination with diarrhea indicates disturbances in the absorption of nutrients in the intestinal tract;
- an abundant content of detritus, represented by fatty molecules, indicates pathologies in the functioning of the pancreas or liver.
Indigestible fiber
Not detected – In the absence of plant foods in the diet, there is no fiber in the feces.
Discovered – Plant fiber can only be partially digested by the human gastrointestinal tract, under the influence of enzymes from intestinal microorganisms. Fiber is mainly excreted unchanged in feces. Indigestible fiber is the coarse fibers of plants and the cell walls of their membranes.
Not detected – During normal digestion, digestible fiber is not detected in the feces.
Found in small quantities - A variant of the norm, a small content of digestible fiber in the form of individual cells not connected to each other is acceptable.
Found in large quantities, starch, foamy feces, acidic reaction – The appearance of digestible fiber in the feces in large quantities indicates insufficient activity of the pancreas and the accelerated movement of chyme through the digestive tract.
Coprogram in a newborn and infant: norm, interpretation
When examining children's feces, many indicators are taken into account, which helps to assess the health of the gastrointestinal tract. To determine whether any pathology occurs, you should know the norms of coprogram in children under one year of age
:
| Indicator name | Newborn, 1-8 months (breastfeeding) | Newborn, 1-8 months (artificial feeding) | 9-12 months |
| Form | Unformed. | Unformed. | Decorated. |
| Consistency | Pasty, viscous. | Thicker consistency. | Formed soft feces. |
| Color | Yellowish, sometimes with greenish tints. | Golden yellow, light brown. | Brown. |
| pH (acidity) | |||
| Muscle fibers | Not detected. | Not detected. | Not detectable, or may be present in very small quantities and only digested. |
| Neutral fat | Absent or drops. | Absent or there is a small amount. | Absent. |
| Fatty acid | Crystals in small quantities. | Not detected. | |
| Soap | Yes, in small quantities. | Yes, in small quantities. | |
| Cellulose | Digestible is not detected, indigestible may be a small amount. | Digestible is not detected, indigestible may be a small amount. | |
| Starch | Not detected. | Not detected. | Not detected. |
| Iodophilic flora | No, or in minimal quantities. | No, or in minimal quantities. | |
| Slime | Not detectable (or in very small quantities). | Not detected. | Not detected. |
| Leukocytes | No, or just a few. | No, or just a few. | Not detected. |
| Red blood cells | Not detected. | Not detected. | Not detected. |
| Hemoglobin | Not detected. | Not detected. | Not detected. |
| Squirrels | Not detected. | Not detected. | Not detected. |
| Bilirubin | Revealed. | Revealed. | Not detected. |
| Stercobilin | Revealed. | Revealed. | Not detected. |
For the accuracy of all indicators, the correct collection of material and timely delivery to the laboratory are very important.
What does detritus in the coprogram indicate in a newborn and infant?
Detritus
- these are all kinds of small particles that represent various residual products of processed food, epithelial cells of the digestive tract and some bacteria. It is formed under the action of enzymes and intestinal microflora.
In the feces of newborns and infants, the amount of detritus can vary in different quantities. It is believed that the more it is, the better, because the presence of detritus indicates the correct functioning of the children's digestive tract.
It is worth noting that the presence of a large number of components other than detritus in the feces (mucus, blood, and so on) may indicate serious pathologies.
Deviations from the norm in the coprogram
Knowing the normal indicators of stool analysis of a child up to one year old, the doctor can judge the health of the gastrointestinal tract.
| Deviation | Possible reason |
| Change in stool consistency | Constipation, increased secretion, colitis, pancreatitis, dyspepsia, food poisoning, allergies. This also happens when teething. |
| Changes in acidity | In case of disturbances in the digestion processes, the acidity shifts to the alkaline side, and in case of dyspepsia - to the acidic side. |
| Mucus in stool | |
| Blood in the stool | The appearance of scarlet blood is a sign of bleeding from the rectum, anal fissures. Blood streaks indicate the presence of infectious diseases (for example, dysentery). With stomach bleeding, the stool usually takes on a very dark, almost black hue. |
| Increase in stercobilin | Hemolytic anemia, increased bile secretion. |
| Decreased stercobilin (stool becomes light-colored and acholic) | Hepatitis, pancreatitis, cholelithiasis, blockage of the bile duct. |
| Increased number of muscle fibers | Gastritis, pancreatitis, dyspepsia, increased peristalsis. |
| Leukocytes in feces | Infectious diseases, colitis, enteritis, errors when collecting material. |
| The appearance of bilirubin in stool | Long-term treatment with powerful antibacterial drugs, dysbacteriosis, increased motility. |
| Presence of proteins in stool | Foci of inflammation and bleeding in the digestive tract, dyspepsia (putrefactive). |
| Appearance of starch | Gastritis, pancreatitis, dyspepsia. It is also observed when the excretion of intestinal contents accelerates (in such cases, this carbohydrate does not have time to break down). |
| Lack of soaps | Pathologies of the liver and pancreas, malabsorption, dyspepsia. |
Mothers should definitely monitor the health of their baby: pay attention to the color, consistency of stool, impurities, as well as the presence of other symptoms. In case of any deviations, it is better to consult a doctor as soon as possible, who will prescribe a coprogram and other tests. This is important for timely diagnosis and treatment of many pathological conditions.
Natalya Korol, pediatrician, especially for the site
Reasons for the appearance of starch in stool tests
Not detected - Starch must be digested completely under the action of salivary and pancreatic amylase, enzymes of the intestinal flora.
Found in large quantities, amilorrhea – Starch found in stool indicates a lack of pancreatic or small intestinal enzymes. With normal enzyme levels and gland activity, starch may remain in the stool due to accelerated movement through the intestines. This happens with disorders of intestinal motor function or intestinal infections.
Small amounts of starch grains detected – Partially undigested starch may be present in the stool due to its excessive amount in food. In this case, they speak of relative enzyme deficiency. This requires diet correction and balanced nutrition.
Iodophilic flora
Not detected - Normal intestinal flora should consist of more than 90% lacto and bifidum bacteria. Iodophilic flora is not detected in feces.
Discovered – Iodophilic intestinal flora are bacteria that are stained dark with iodine preparations. These are cocci, rods, yeasts, which are responsible for the processes of rotting and fermentation in the intestines. Normally, they make up less than 10% of the intestinal flora. When the ratio of lactobacilli, bifidumbacteria and iodophilic microorganisms changes, the digestive processes in the intestine are disrupted.
Iodophilic flora was detected, muscle fibers were changed, the reaction was alkaline, the color was dark brown - Insufficient activity of the digestive glands leads to the fact that incompletely digested chyme enters the intestines, which creates favorable conditions for the development of iodophilic flora. Excess animal protein in the diet and insufficient digestion provokes the development of putrefactive flora.
Iodophilic flora, digestible fiber, starch, acidic reaction were detected - The processes of carbohydrate breakdown were disrupted as a result of insufficient activity of the pancreas. Undigested or partially digested fiber and starch, and excess simple carbohydrates create an environment for the proliferation of iodophilic flora.
Detritus in a smear for flora in women
A gynecological smear is taken from the urethra, vagina and cervix. In this case, only representatives of the normal microflora of the woman’s vagina should be diagnosed in the detritus. In case of inflammation of the internal genital organs, infectious infections or vaginitis, pathogenic species of bacteria or abundant unnatural secretion of normal microflora are detected. Normally, the cervix and urethra are completely sterile. In this case, a moderate number of epithelial tissue cells is allowed in the analysis results.
Prescribed to determine the condition and function of the digestive organs. Such a stool examination helps to identify the presence of inflammatory and infectious lesions of the digestive system in a child. Also, using a coprogram in the stool, you can detect hidden blood (to diagnose internal bleeding) and worm eggs.
Mucus in stool
Not detected - Normally, mucus in stool is not detected as a separate structure, but is completely mixed with it.
Detected - With increased mucus secretion, it is detected in the stool as streaks and plaques of light yellow or white color. This can happen with an intestinal infection, benign or malignant formation in the intestine.
In children under one year of age, excess mucus in the stool is normal, since the intestines are still adapting to work. An increase in the amount of mucus can occur when the balance of microflora is disturbed, and when complementary foods are introduced for which the child is not yet ready.
Preparing for coprogram
Proper preparation determines the accuracy of the research data obtained. The biomaterial for analysis is feces, which must be collected naturally. It is allowed to take feces from the surface of the baby's diaper. For children - from a previously washed (without chemicals) potty. Adults collect feces that have not touched the bottom of the toilet.
For 2 days, it is necessary to exclude medications that affect intestinal motility (laxatives, prozerin ®, vasopressin ®, belladonna ®) and the color of stool (carbolene ®, iron).
The biomaterial is collected in a special sterile container, which can be purchased at the laboratory or pharmacy. Temperature optimum for storage is from +2 to + 8° C (refrigerator).
Epithelium in feces
Not detected – Normal
Found in small numbers – Normally, a small number of squamous and columnar epithelial cells may be present in the stool. This occurs as a result of the mechanical effect of feces on the walls of the digestive tract.
Found in large quantities, brown feces with red deposits, red blood cells - With an increased number of epithelial cells, one can judge the inflammatory process of the gastrointestinal tract. Squamous epithelium enters the stool from the lower rectum. Usually, red blood cells or blood are present along with the epithelium in this case. This can happen with constipation, hemorrhoids, fissures.
Found in large quantities, mucus, digestible fiber, altered fibers, starch, foamy feces, semi-liquid consistency, liquid consistency, mushy - With an increased number of epithelial cells, one can judge the inflammatory process of the gastrointestinal tract. The detection of columnar epithelium indicates inflammation in the upper intestines; the level of inflammation helps determine other changes in the coprogram.
Norm
To be able to decipher the coprogram, you should know what characteristics of the stool are being examined and what their normal values are. Note that in a small child, the type of feeding affects the characteristics of feces.
| Index | Breastfed infants | Formula-fed infants | Children over one year old |
| Quantity (grams per day) | From 100 to 250 | ||
| Yellow, possible greenish or mustard tint | Brown or yellow | Brown | |
| Consistency | Pasty | Putty-like | Decorated (sausage-shaped) |
| A little sour | Pronounced, putrid | Specific fecal, but not harsh | |
| pH value (acidity) | From 4.8 to 5.8 (slightly acidic) | From 6.8 to 7.5 (slightly alkaline) | From 6 to 8 (slightly alkaline) |
| May be detected in low quantities | |||
| Leukocytes | May be isolated | May be isolated | Single |
| Stercobilin | From 75 to 350 mg per day | ||
| Bilirubin | Must be missing | ||
| Ammonia (in mmol/kg) | Not determined | Not determined | |
| Muscle fibers | Can be detected in small quantities | Can be detected in small quantities | Not detected |
| Not detected | Not detected | Not detected | |
| Soluble protein | Not detected | Not detected | Not detected |
| In small quantities | In small quantities | In small quantities | |
| Connective tissue fibers | Not detected | Not detected | Not detected |
| Digestible fiber | Not detected | Not detected | Not detected |
| In different quantities | In different quantities | In different quantities | |
| Not detected | Not detected | Not detected | |
| Fatty acid | In low quantities, represented by crystals | Not detected | |
| Neutral fat | In the form of drops | In small quantities |
Leukocytes in stool
Not detected/single – Single leukocytes in the stool may be present in a healthy person.
Single leukocytes, mucus, brown feces with bright red coatings - Changes are characteristic of inflammation of the rectum, hemorrhoids.
Found in large numbers, columnar epithelium - The presence of a large number of leukocytes indicates acute or chronic inflammation of the digestive tract. Columnar epithelium indicates that most likely the source of inflammation is in the duodenum or upper parts of the small intestine.
Found in large numbers, squamous epithelium, mucus - A large number of leukocytes and the presence of squamous epithelium indicates inflammation of the rectum, possibly a tumor or the presence of polyps.
Rules for taking the analysis
It is advisable to collect stool in the morning. Prepare a clean container for the laboratory and a vessel for defecation in advance. The genitals are washed with soapy water and boiled water. The bladder is first emptied. The sample is transferred to a container for transportation and carefully closed.
Leukocytes in the stool of an adult appear during infectious diseases, dysbacteriosis, against the background of intoxication, and during allergic reactions. To eliminate the unreliability of the result, it is recommended to exclude fish and meat, tomatoes and all types of greens from the diet 3 days before the test.
The presence of fatty acids in the stool of a child under 3 years of age indicates steatorrhea and impaired digestion. To normalize the condition, it is necessary to adjust the diet and not introduce “adult” foods into the diet. Recommendations for patients with mature flora are given by the doctor based on the results obtained.
Red blood cells in feces
Not detected - normally absent
Changed red blood cells were found in large quantities, black stool - The presence of changed red blood cells in the stool is a consequence of gastric bleeding or bleeding from the duodenum. The amount of blood detected indicates the intensity of bleeding. Thick black stool indicates an emergency condition, intense bleeding.
Red blood cells are found in large quantities, the stool is dark brown, red-brown - When bleeding in the small intestine, the red blood cells/blood in the stool manage to partially change, acquiring a dark red or brown color.
Unchanged red blood cells were found in large quantities - In case of bleeding from the large intestine and rectum, red blood cells remain unchanged in the stool.
Table with norms for children
The main (obligate) microflora in adults makes up 90% of all intestinal microorganisms, in children - 99%. When deciphering a coprogram in a baby, age characteristics are taken into account:
Stool analysis in children is carried out according to the same rules as in adults. For young patients, a special diet and abdominal massage help relax the intestines.
Red blood cells in the stool, regardless of age, indicate hidden and open bleeding. Minor inclusions can only be identified through chemical testing. During inflammatory processes in the large intestine, blood fragments can be seen on the surface of the feces, in the upper sections and stomach - the color of the stool changes to tarry, black.
A general stool analysis - coprogram - allows you to clarify the diagnosis. For example, a change in color may have harmless causes. Coloring changes when consuming foods with dyes, certain types of antibiotics and other medications, greens and beets, chocolate and iron supplements.