What diseases does blood indicate?
Blood in the stool is a sign of intestinal damage.
Normally, there are no red blood cells in feces. The presence of these blood cells indicates damage to the blood vessels. The most common cause is hemorrhoids. It can also disguise a more serious pathology (intestinal cancer). The presence of this symptom should force the sick person to see a doctor and get examined. If the source of bleeding is located in the stomach and small intestine, clotted blood may be released in the feces. It is dark in color and appears in the form of clots.
Blood in the stool of women and men can be visible to the naked eye or detected during laboratory tests.
There are many reasons for this pathology. Not all of them are associated with intestinal pathology.
How to determine the presence of blood in stool
During the study, chemical substances are used that, upon contact with a red blood cell, change color due to oxidation. Gregersen's method allows you to see even small amounts of hemoglobin. Benzidine turns iron blue.
Taking into account the speed of staining and its intensity, a weakly positive (+), positive (++ or +++) and strongly positive (++++) reaction is established. When using benzidine, it is possible to establish blood loss in excess of 15 ml/day, which often gives false positive results.
Immunochemical analysis of stool is considered more accurate. It uses antibodies to human hemoglobin, so there is no need to follow a diet. The test is highly sensitive; it will detect 0.05 mg of hemoglobin per gram of stool (at 0.2 ml/g of stool the test is considered positive).
This method allows you to detect tumor formations in the large intestine, but does not detect bleeding from the esophagus or stomach. In 3% of cases, tests give a positive result in the absence of a tumor in the large intestine.
Causes of blood
Blood in the stool in an adult: causes
Finding blood in the stool of an adult is quite frightening.
The reasons can be completely different, because blood is just a symptom of the disease. If the bleeding stops after a certain period of time, this does not mean at all that the disease went away on its own; in any case, it is necessary to find out the main cause by contacting a specialist.
Let's look at why stool with blood can appear in adults or children, what symptoms accompany the main diseases that cause bleeding, and what can be done to alleviate the patient's condition.
Common diseases
It is not surprising that blood in the stool of an adult is a symptom of diseases of the gastrointestinal tract and various parts of the intestines.
First of all, you need to be checked for intestinal cancer, since this is the most serious disease, the treatment of which directly depends on the time of visiting a doctor. The sooner, the greater the chance of saving the patient.
- if blood occurs, if you have never had problems with this before;
- you need to call an ambulance quickly when the bleeding continues for more than 10 minutes;
- if the victim is over 40 years old;
- there is a hereditary predisposition to intestinal cancer;
- other problems such as discomfort and pain in the abdomen, elevated body temperature, dizziness;
- if the person has already had bowel cancer or has undergone radiation therapy.
blood in the stool of an adult is a symptom of diseases of the gastrointestinal tract, various parts of the intestines
Infectious diseases
In other cases, it is also necessary to take blood in the stool seriously. The causes may be infectious. Bacteria can enter the body through food or dirty hands. One of the most dangerous diseases of this type is dysentery.
The lining of the large intestine is affected. This also includes amoebiasis and salmonellosis. The main manifestations of intestinal infections are: frequent loose stools, which contain mucus and blood in the stool, fever, chills, severe abdominal pain, vomiting.
False urges to go to the toilet also usually occur.
Infectious diseases can provoke other complications, so you should not treat them yourself; it is strongly recommended to consult a specialist in such cases. They are also often contagious, so it is imperative to disinfect the room after the patient to avoid re-infection.
To avoid poisoning, the simplest prevention is necessary, which includes:
Carrying out diagnostics
Seeing a doctor is a mandatory procedure for a patient who has discovered bloody discharge and mucus in his stool. As a rule, the proctologist prescribes diagnostics, instrumental or laboratory, which includes the following activities:
- Stool analysis.
- Rectal diagnostics.
- Examination of the anus.
- Sigmoidoscopy.
If after these diagnostic procedures the problem is still unclear, then the patient should undergo an ultrasound examination of the intestines, as well as an x-ray of the gastrointestinal tract. Also, if necessary, a specialist can prescribe a colonoscopy for the patient. It would be useful to consult with a gastroenterologist, who requires a gastroscopy to clarify the cause of the appearance of blood in the stool.
The main methods of treatment for the appearance of blood in the stool
If blood begins to appear constantly, you need to contact a proctologist or coloproctologist. Treatment options will depend on the cause of the bleeding.
If bleeding occurs in the rectum, it is necessary to undergo a colonoscopy, and a rectal examination is also required. You should tell your doctor in detail about the symptoms that are accompanied by bleeding: the consistency of the stool, the nature of the pain, constipation. If there is a feeling of incomplete emptying, the doctor may suspect a tumor formation.
If you have bleeding in the rectum, you should not walk, stand or sit, because during movements the blood flows to the pelvic veins, which may subsequently increase the bleeding. You should not drink fatty, spicy, or alcoholic drinks. The patient should lie down on a sofa or bed. Remember, self-medication in this situation is dangerous, you need to urgently go to the hospital.
At home, you must adhere to the following recommendations:
- Lie in bed and on your side.
- Take a cold heating pad and apply it to the perineum. Using cold, you can narrow the vessels of the perineum and stop bleeding. The heating pad should be kept on for 20 minutes. Then rest for 5 minutes and apply the cold heating pad again.
It is life-threatening for the patient if, in addition to bleeding, a malignant tumor develops in the hemorrhoids or in the intestinal region.
For example, an experienced proctologist talks about a case that he encountered in his medical practice: “A 25-year-old man came to me, he had complaints of pain in the anus and blood in his stool. After I examined him with a proctoscope, an erosive bleeding internal hemorrhoid was discovered. Above, I saw a stenotic tumor. After interviewing the patient, I learned that at first he was bothered by a feeling of discomfort in the lower abdomen, most often on the left, then bloody stool appeared, and only then hemorrhoids began to fall out. The patient did not want to see a doctor; he thought that everything would go away just like that. The situation turned out to be dangerous, so an operation was scheduled to remove the primary tumor and create a colostomy. In the future, the patient needed consultation with an oncologist.”
This case suggests that if you notice even a little blood in your stool, you should immediately go to the doctor. Do not think that hemorrhoids are a harmless disease that is constantly laughed at. It leads to serious consequences.
Remember that all bleeding in the rectum is pathological. The sooner the cause is determined, the better. The main thing is to prevent or detect the appearance of a malignant tumor in a timely manner. What will happen if this is not done? The patient may die because the doctor can no longer help with an inoperable tumor.
Thus, blood in the stool is always not only an unpleasant, but also a dangerous symptom.
There can be many reasons; it is very important to find out about the disease that caused the bleeding. Quite often, bleeding is caused by an infectious disease or inflammatory process.
Treatment methods
Detection of blood and clear or colored mucus in feces is a reason to immediately begin treatment. Treatment tactics should ideally be determined by a group of specialists, which includes a proctologist, hematologist, infectious disease specialist, oncologist and surgeon.
Attention! If during treatment a sharp increase in the amount of blood in the stool is detected, an emergency team should be called. Massive bleeding threatens the patient's life; his emergency hospitalization can save his life.
Emergency care
The treatment method for the causes of blood and mucus in the stool is determined by the nature of the disease. Therapy is prescribed by a doctor whose profile is responsible for bleeding. So, if blood and mucus in the stool are the result of cancer, the person is referred to an oncologist. If bright red clots are an indication of a fissure in the anus, then treatment is carried out by a proctologist.
When consulting with a doctor, it is worth not just listing the complaints, but also indicating the external signs of mucus in the stool. This is a condition under which it is possible to guarantee an accurate reconstruction of the clinical picture, which is the key to a well-designed examination plan and prescribed treatment. Most of the pathologies in which inclusions in stool are detected are chronic, so the condition without proper treatment will only worsen over time.
Colon polyps
Rectal polyps are benign spherical or branched formations that exist asymptomatically for a long time. The appearance of mucus and blood in the stool indicates that the process is neglected and requires immediate surgical treatment, otherwise malignant oncopathology may develop in place of benign polyps. In more than 50% of cases, polyps develop into cancer within 10 years.
The reasons for the growth of polyps are varied, but more attention is paid to hereditary predisposition and age over 50 years. In addition to bleeding, these benign formations can cause diarrhea, constipation and abdominal pain.
Detection of polyps during colonoscopy
Treatment
After correct diagnosis, the doctor prescribes treatment for the adult to prevent the appearance of viscous contents in the stool. One of the first measures is a diet that excludes the consumption of coarse fibers, suggesting a balanced diet. The prescription of the medicine depends on the disease:
- treatment of hemorrhoids - suppositories, tablets to relieve inflammation, stop bleeding;
- for irritable bowels - antispasmodics, medications for constipation;
- to get rid of parasites - tablets for their removal.
If the cause of the appearance of mucous contents is oncology, radiation treatment and chemotherapy are prescribed. Medications that help cope with the problem in adults include:
- Furazolidone – intestinal infections with loose stools;
- Viferon – viral lesions;
- Amphotericin B – fungal pathologies, candidiasis;
- Interferon - ingestion of mucus during the flu;
- Bifiform – dysbacteriosis;
- NO-spa – inflammation, spasms in the rectum;
- Contrical - pancreatitis.
Prevention of gastrointestinal bleeding
Prevention of diseases of the digestive system consists of a healthy lifestyle, proper nutrition, and giving up bad habits. It is necessary to take medications only as prescribed by a doctor, and do not self-medicate. You should avoid spicy seasonings, canned foods, and eliminate alcohol. The diet should include quite a lot of fermented milk products. Regularly, at least once a year, you should undergo preventive medical examinations.
Prevention of bleeding also consists of timely diagnosis and effective treatment of chronic gastrointestinal diseases. Particular importance is attached to eradication (destructive) antiulcer therapy aimed at eliminating Helirobacter. The European Society for the Study of this bacterium has proposed a treatment regimen:
- omeprazole or lansoprazole;
- clarithromycin, amoxicillin.
Drugs of the first group belong to proton pump inhibitors, new pharmacological agents that suppress the secretion of hydrochloric acid in the stomach. Clarithromycin and amoxicillin are antibiotics with a wide spectrum of antimicrobial activity. Eradication therapy is prescribed for 10 days to patients with gastric and duodenal ulcers during remission to prevent exacerbations and bleeding.
Diagnosis of pathology
Blood in the stool is a very ambiguous and rather alarming symptom that should not be taken lightly. The fact is that this sign can indicate both diseases that are not life-threatening, and rather serious pathological conditions that require emergency medical care.
Causes in an adult
In an adult, the appearance of unchanged scarlet blood on the surface of the stool (this could be streaks of blood in the stool, mucus with blood) most often indicates bleeding from the lower parts of the large intestine, in particular from the rectum.
Such bleeding may be due to the presence of hemorrhoids, anal fissure, polyps and diverticula, as well as rectal cancer. Rare causes include endometriosis and vascular abnormalities. Blood clots may be present in the stool in Crohn's disease and ulcerative colitis.
If bleeding occurs in the upper parts of the gastrointestinal tract (esophagus, stomach, duodenum), the blood becomes tar-black in color under the influence of gastric juice and digestive enzymes.
But bleeding is not always so massive that it can be seen with the naked eye. Hidden blood in the stool can appear due to ulcerative, tumor and other lesions of the gastrointestinal tract, and there are special laboratory tests for its detection. This makes it possible to detect even minor bleeding, usually at an earlier stage of the disease.
Causes in children
- In a child, the appearance of streaks of blood and mucus in the stool is usually associated with stool disorders - constipation, diarrhea, which can accompany various diseases, including dysbacteriosis and food allergies.
- If the stool takes on the appearance of raspberry jelly against the background of the child’s expressed anxiety and cramping abdominal pain, intussusception of intestinal loops can be suspected - a very serious condition that requires urgent surgical intervention.
Other reasons that change the color of stool
The appearance of black stool and even red inclusions does not always indicate bleeding. Sometimes this is associated with the use of certain foods and medications:
- semi-digested remains of eaten berries (blueberries, currants), tomatoes may look like blood clots;
- when eating red beet dishes, the stool may turn crimson;
- food colorings included in various desserts and drinks can change the color of stool;
- the use of activated carbon and iron supplements leads to the appearance of black stools.
However, it is better to be overly vigilant than to miss a terrible signal. Each person needs to periodically examine their stool and, if suspicious impurities are detected, consult a doctor who will promptly prescribe the necessary tests and make a diagnosis.
Diagnosis of possible diseases
After the doctor examines the symptoms of the disease, he begins to examine the patient. When examining surgical patients (with hemorrhoids, suspected ulcer bleeding, appendicitis, etc.), a mandatory digital rectal examination is performed.
Additional laboratory tests:
- coprogram
- examination of stool for helminth eggs,
- fecal occult blood test (Gregersen test),
- coagulogram (clotting system),
- clinical blood test (low hemoglobin with anemia).
Invasive diagnostics
Fibroesophagogastroduodenoscopy (FGDS). A procedure that involves inserting an endoscope, or flexible tube with a small camera at the end, through the mouth and down the esophagus into the stomach and duodenum.
Used to find the source of blood loss in the upper gastrointestinal tract. During EGD, samples are often taken for biopsy. Colonoscopy. A diagnostic method in which an endoscope is inserted through the rectum.
This means that the large intestine is examined. Colonoscopy is not without pain, which is why it is often performed under anesthesia. Barium X-ray. Since hollow organs are not visible on x-rays, to take an x-ray of the digestive tract, a contrast agent must be injected. During an X-ray of the stomach, barium is drunk; during irigography, it is injected into the rectum.
Capsule endoscopy. A new diagnostic method in which the patient swallows a small capsule with a video camera, and the doctor behind the monitor can observe all changes in the intestinal mucosa. It is used for suspected Crohn's disease, celiac disease, intestinal polyps, anemia of unknown origin and other conditions. The capsule passes through all parts of the gastrointestinal tract and exits naturally.
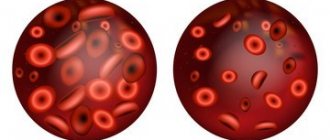
Color of blood in stool
During the analysis, laboratory assistants must pay attention to the color of the blood. If bleeding has opened in the sigmoid colon, the rectum, it will be bright red.
Burgundy or dark red blood appears when there is bleeding in the transverse and rectum.
If there is bleeding in the anus, black blood may appear in the stool. In this case, the feces have a resinous consistency and an unpleasant odor. This type of stool is called melena. In this case, blood accumulates in the intestine for a long time. Melena may indicate bleeding in the upper stomach (duodenum, small intestine).
Red blood in your stool indicates that you have hemorrhoids. In this case, blood is released without clots after defecation. It is worth considering that scarlet blood can be a sign of a malignant tumor in the rectum.
You should call emergency services immediately if you have black, loose stools. It indicates severe bleeding in the stomach or intestines. Most often, this symptom is provoked by an ulcer, gastric erosion, varicose veins, and cirrhosis of the liver.
What if mucus comes out with blood?
Blood entering the stool in the gastrointestinal tract turns the feces dark. This is due to the breakdown of hemoglobin, which is converted into iron. The blood turns black, and so does the stool. Also, these processes become symptoms of such diseases:
- Varicose veins of the esophagus. This is a component of portal hypertension syndrome, which occurs when diagnosing liver cirrhosis. Black stools, vomiting, chest pain after eating and increased heart rate are the main signs of this pathology. If a vein in the esophagus ruptures, a probe must be inserted to compress the veins and stop the bleeding.
- Stomach ulcer, duodenal ulcer. The feces become tar-colored, liquefy, nausea leads to vomiting, and the vomit contains blood clots like “coffee grounds.” To solve the problem, surgery is required.
- Perforation of the ulcer. The patient complains of acute pain in the abdomen and chills. Covered in cold sweat, in some cases even loses consciousness. The main way to urgently help a patient is resection of the stomach and duodenum.
- Stomach cancer. The patient experiences an aversion to food, especially to meat products. Blood tests show anemia. A person who has lost a lot of weight becomes weak. The breakdown of tissue provokes bleeding, which can be determined by the admixture of blood in the stool.
- Bowel cancer. The main symptom of this pathology is alternating constipation with diarrhea, constant rumbling in the stomach. Defecation does not bring satisfaction. The urge to have a bowel movement is often false. The character of the stool is ribbon-like, thin, and in the later stages of the disease there are noticeable traces of blood in it.
Interesting! Blood in the stool can be a sign of not only diseases of the internal organs. This can be a sign of stomatitis and nosebleeds. When impurities are detected during defecation, it is necessary to conduct a comprehensive assessment of the body's condition.
Blood may be a result of intoxication. Thus, poisoning from rat poison or some poisonous plants can be so severe that internal bleeding occurs. Sometimes bloody bowel movements become a side effect of drug therapy using Aspirin, Diclofenac, Xarelto or Heparin. Use of these medications should be discontinued if such problems are detected.
Possible complications of the disease
Constant blood loss in small quantities often leads to serious and even irreversible consequences. Moreover, the effectiveness of treatment largely depends on the patient’s age, his state of health and the presence of other pathological processes in the body. On average, recovery time after serious illnesses ranges from 2 to 12 months.
During the treatment period, it is extremely important to follow the doctor’s recommendations and not break your diet. In my practice, I have encountered a patient suffering from ulcerative colitis
To avoid recurring bleeding, the patient should not drink alcoholic beverages or fried foods. On his birthday, the man violated his diet, which led to extremely unpleasant consequences. Due to the abundance of spicy and fatty foods in combination with wine, damage to the vascular wall occurred in the lower intestines, which resulted in massive bleeding. The victim was urgently operated on, as a result of which complications were avoided.
Unpleasant consequences of the disease:
- Anemia, or anemia. This is a dangerous disease that develops against the background of constant blood loss. The number of red blood cells and hemoglobin, a protein involved in the transport of oxygen to tissues, decreases in the body. This leads to disruption of many physiological processes in the human body. The nervous system suffers from nutritional deficiencies, as a result of which patients with this disease often lose consciousness.
- Disturbance of iron metabolism in the body. Problems with the gastrointestinal tract affect its ability to absorb various components. Due to constant blood loss, iron supplied with food is absorbed much worse and cannot be used in the body's metabolic processes. This pathology is manifested by severe impaired hair growth, brittle nails and fragility of the skeletal system.
- Hypovolemic shock. With massive blood loss in the human body, the balance between the volume of circulating fluid and the vascular bed is disturbed. There is not enough blood to fully start the heart, as a result of which the patient falls into a prolonged faint, gradually turning into a coma.
Possible diseases
Let's talk about common pathologies in which blood comes out in the stool. First, let's discuss a disease such as hemorrhoids.
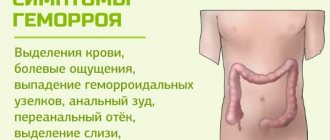
Haemorrhoids
Hemorrhoids are a common disease based on varicose hemorrhoidal veins. Most often, the disease affects people who lead a sedentary lifestyle. The increasing computerization and motorization of society as a whole explains why the disease is gaining momentum in its prevalence every year. But despite this, few people are ready to talk openly about their problem, and even fewer people understand what the reasons for the development of this pathology are.
The following factors can serve as a catalyst in the development of hemorrhoids:
- chronic constipation;
- long sedentary work;
- lifting weights;
- poor nutrition, in particular, abuse of spicy foods;
- bad habits, such as alcoholism;
- anal sex;
- pelvic inflammation;
- pregnancy and childbirth;
- neoplasms;
- long periods of standing.
Blood discharge is present in the stool, on linen or toilet paper. Sharp and unbearable pain appears in the anorectal area. To restore the act of defecation and the consistency of stool, a diet is prescribed. It is important to monitor the amount of liquid you drink. This can be not only natural water, but also vegetable and fruit juices.
Therapeutic exercises are also carried out, medicinal baths, ointments, and suppositories are prescribed. The basis of drug therapy is phlebotropic drugs. They normalize blood flow and microcirculation, and also increase tone. In severe cases, surgery is indicated.
Anal fissure
An anal fissure is damage to the skin of the anal canal. On the back side of this channel in the middle, the skin is not sufficiently protected. There is also insufficient blood supply to this area. Cracks can appear in a person at any age. People suffering from chronic constipation are at risk. Due to stool retention, trauma to the anus occurs.
Anal fissures can be a consequence of colonoscopy, sigmoidoscopy, and surgical interventions. Sometimes the appearance of such a symptom can signal the development of more serious pathologies, namely:
- tuberculosis;
- chlamydia;
- cancer;
- gonorrhea;
- syphilis;
- sepsis;
- herpes;
- nonspecific ulcerative colitis.
Fresh blood in the stool occurs with anal fissures.
The pathology is accompanied by the appearance of blood in the stool and painful sensations during the act of defecation. Patients develop a fear of going to the toilet “in a big way”, which is why they can restrain the urge to defecate.
Important! Cracks can form from hard feces.
To relieve sphincter spasm, nitroglycerin ointment, warm manganese baths, as well as suppositories and ointments with an analgesic effect are used. Methyluracil and sea buckthorn oil will help relieve suffering. The most important condition for the success of the treatment process for anal fissures is dietary nutrition.
Its main task is to activate the intestines and facilitate bowel movements. The menu must include dairy and plant products. The diet should be varied and balanced. Spicy foods and alcoholic drinks will have to be completely avoided.
Crohn's disease
This is a chronic disease in which there is inflammation of the mucous membrane of the large intestine. It is characterized by a progressive course. Crohn's disease can cause serious complications, including perforation, sepsis, and bleeding. The formation of pathology is associated with ongoing immunological processes in the body.
Essentially, the body perceives the intestines as a foreign organ and produces protective antibodies against it. This leads to damage to the organ and the formation of pathomorphological changes. The following factors can trigger the onset of Crohn's disease:
- hereditary predisposition;
- bacterial and viral infection;
- dysbacteriosis;
- bad habits: smoking, alcohol abuse;
- influence of harmful production and environmental pollutants.
The first symptom of the pathological process is the appearance of bloody discharge along with feces. Over time, false urges to defecate with mucus and blood appear. Patients complain of stool incontinence. If only the rectal segment is involved in the process, the patient will be bothered by constipation.
If the process involves the descending part of the colon, on the contrary, diarrhea is a concern. When the entire intestine is completely damaged, bloody diarrhea and cramping pain in the lower abdomen occur. General well-being is also affected. There is an increase in body temperature, tachycardia, and a drop in blood pressure.
During an exacerbation, therapeutic fasting is indicated in the first two days. For diarrhea and dyspeptic disorders, it is recommended to consume large amounts of protein, while fats and carbohydrates are reduced. All medications for Crohn's disease are used under the strict supervision of a physician.
Intestinal bleeding
Excessive blood loss can occur with traumatic injuries, diseases of the gastrointestinal tract (GIT), endocrine pathologies, and infectious processes. Symptoms of internal bleeding include:
Pain in the lower abdomen after defecation
- change in color of stool;
- stomach ache;
- weakness, pallor;
- iron taste in the mouth;
- vomit;
- diarrhea with blood.
If a person complains of a frequent urge to defecate and has loose, dark stools, this indicates heavy blood loss. A blood clot and scarlet mucus in the stool most often indicate moderate or heavy bleeding. The presence of blood streaks indicates minor loss of biological fluid.
Dark stool indicates damage to the large intestine. Bright stool may indicate pathology of the small intestine. A scarlet stream of blood after a bowel movement is a clear sign of hemorrhoids. In case of heavy blood loss, the patient should be laid on a flat surface, put cold on the stomach and call an ambulance. It is strictly forbidden to eat, drink hot drinks or take a bath.
Rectal cancer
A malignant tumor appears as a result of hypertrophy of intestinal cells. The pathology is more typical for older people. The first signs of direct food cancer may be frequent hemorrhoids and constipation. Experts identify factors that can lead to the development of a tumor process:
- lack of balanced nutrition;
- polyps. These benign neoplasms have a tendency to degenerate;
- human papillomavirus;
- anal sex;
- obesity;
- sedentary lifestyle.
With rectal cancer, blood bleeds during bowel movements.
The photo shows 4 stages of the tumor process. In the early stages of the tumor process, the following symptoms may appear:
- frequent urge to defecate;
- pain in the anal area;
- constipation causing bloating;
- discharge of blood before the appearance of stool;
- exhaustion, weakness;
- incontinence of feces and gases;
- loss of appetite;
- temperature increase.
Important! During tumor processes, blood may appear in the stool without pain.
Treatment directly depends on the location of the tumor and the stage of the process. In general, complex therapy includes surgery, chemotherapy and radiation. With timely treatment, a five-year survival rate is observed in sixty percent of cases.
Colitis
Colitis is an inflammation of the large intestine. It manifests itself in the form of stool failure, flatulence, as well as pain of different localization in the abdominal area. Feces acquire an unpleasant odor. Colitis can be acute or chronic. The first option is characterized by a stormy and fast current. A chronic process develops over a long period of time. Depending on the method of exposure, the disease is divided into the following groups: ulcerative, ischemic, infectious, medicinal.
Proctitis
With proctitis, the mucous membrane of the rectum is affected. The causes of the disease can be intestinal infections, parasites, injuries, syphilis, tuberculosis. Surgery, anal sex, and poor nutrition can damage the rectum. Pain sensations are localized not only in the intestines, but also in the perineum. In women, they radiate to the labia and vagina, and in men, to the genitals and scrotum.
The disease causes a disturbance in general well-being. The signs of chronic proctitis are less pronounced. This process is characterized by a wave-like course, in which periodic exacerbations are replaced by periods of remission. Nutritional adjustments play a major role in the treatment process.
It is important to exclude foods that irritate the rectal mucosa, these include fatty, hot, spicy, and sour foods. During the acute process, fruits, berries, sweets, and vegetables should be excluded. It is important to follow the correct regimen and give the body moderate physical activity. It is not recommended to sit for a long time.
Diverticulosis
The disease is characterized by the appearance of diverticula, that is, protrusions in the form of pouches, on the intestinal wall. The leading role in the development of the pathological process is played by dystrophic changes in the muscular and vascular wall of the organ. Diverticulosis can also occur due to an unhealthy diet, which does not contain enough fiber, as well as a sedentary lifestyle.
Blood in stool may be a symptom of Crohn's disease and ulcerative colitis
Often the disease is asymptomatic and is discovered completely by accident during a diagnostic examination of the intestines. The presence of diverticula may be indicated primarily by abnormal bowel movements. Mostly patients are concerned about constipation. A large amount of foul odors are released. In approximately thirty percent of cases, diarrhea with blood appears.
Pain may occur in the left side of the abdomen. Patients complain of abdominal rumbling, bloating, nausea and vomiting. They become irritable and get tired quickly. In asymptomatic cases, the treatment process as a whole is based on nutritional adjustments. Products containing coarse fibers are excluded from the diet: raw cabbage, radishes, persimmons.
You will also have to give up legumes, grapes and watermelon, as they cause bloating. Drug therapy includes the use of broad-spectrum antibiotics, as well as drugs that restore intestinal microflora. If complications occur, surgical treatment may be required.
Helminthiasis
Blood in the stool can appear in advanced forms of helminthiasis, when there are a lot of worms in the intestines. In this case, not only the worms themselves come out along with the feces, but also blood is released due to numerous lesions.
Attention! Some types of worms have the ability to gnaw through the intestinal wall, causing internal bleeding.
Helminths can simultaneously cause a number of seemingly unrelated symptoms:
- neuroses;
- allergy;
- bloating;
- anemia;
- weight loss;
- temperature increase;
- weight loss;
- increased gas formation;
- bleeding from the anus.
Helminthiasis is another reason for the appearance of blood streaks in the stool
Internal hemorrhoids
With internal hemorrhoids, enlarged hemorrhoids are located inside the rectum and are not visible when examining the anus. During defecation, the nodes can be injured and light blood streaks remain on the surface of the feces. Hemorrhoids are also characterized by other local symptoms: itching in the anus, pain during defecation, constipation, distension in the anal area outside of defecation.
The causes of hemorrhoids vary, but most often they are regular constipation and a sedentary lifestyle. Inflammation of hemorrhoids often occurs in pregnant women, which is associated with an increased load on the vessels, including the hemorrhoidal veins.
Diagnosis of internal hemorrhoids is carried out by examining the anal area and performing rectoscopy (endoscopic examination of the rectum).
Symptoms
Blood during defecation will be accompanied by various symptoms, they will depend on the root cause of the pathology. With hemorrhoids, a person will feel pain, burning and itching near the anus, while the hemorrhoids will also be bothered when walking, which causes a lot of discomfort. With oncology of the digestive organs, heartburn is often a concern, problems with stool appear, it is painful to defecate, and discomfort often radiates to the lower back. Feces can be solid or liquid, the blood is dark, sometimes instead of feces, pus and mucus come out of the intestines along with blood inclusions.
Sometimes traces of blood on toilet paper can be the first symptom of intestinal cancer.
Often, with oncology in the initial stages, the act of defecation occurs without pain, and there may be no blood or it may be present, but not much. But even a drop should alert you and become a reason for a visit to a proctologist, since many serious diseases in the initial stages do not have pronounced signs. Blood on paper is sometimes evidence of the onset of the disease, so you should not ignore this sign.
With infectious pathologies, women and men develop indigestion, fever, severe abdominal and lower back pain, and sometimes diarrhea is accompanied by nausea and vomiting. Blood in the stool is bright, pink, indicating damage to the intestinal mucosa and the development of internal bleeding. The first thing to do in this case is to immediately go to the hospital and immediately begin therapy.
What can cause mucus?
There are many reasons why the body begins to produce mucus. The most common ones are listed below:
- Sudden change in diet plan.
- Using raw water from a source.
- Severe constant hunger.
- Intestinal dysbiosis.
- Treatment of concomitant diseases using antibiotics.
- Infectious respiratory diseases.
- Using a large number of decoctions in the diet.
- Chronic constipation.
In addition to these reasons, mucus in the stool can be a consequence of severe hypothermia in the pelvic organs. If you sit on a cold surface for a long time or swim in a body of cold water, the body will react with the appearance of jelly-like discharge.
Causes of blood in stool
Factors influencing the appearance of red spots in the stool of an adult are divided into two categories depending on whether they are male or female. This allows you to subsequently prescribe a more effective recovery course and eliminate relapses.
In men
The causes of bloody stool in an adult man can be a wide range of infectious pathologies. The most common ones should be considered:
- salmonellosis;
- shigellosis;
- Escherichiosis.
Associated with the presented category of factors is the pathological influence of helminths. Parasites or protozoan microorganisms may well affect the excretion of blood in feces in men. Quite often, the cause of such discharge is aggravation of the general condition due to ulcerative lesions of the stomach or duodenum. The nonspecific form of ulcerative colitis is another provoking factor for the appearance of blood in the stool in men, the symptoms of which are quite aggressive.
We should also not forget about the likelihood of the presence of neoplasms of various origins in the digestive system. Each of the presented factors requires prompt treatment and subsequent prevention.
Among women
The causes of blood in a woman’s stool may be a simple failure to comply with the diet. In the early stages of pregnancy, female representatives experience a craving for food products that are unusual for her. In addition, in the early stages, feces with blood during pregnancy can be provoked by toxicosis and concomitant diseases of the digestive system (for example, gastritis).
In the first trimester, there is a serious hormonal change in the body, which is associated with a worsening of the immune system. As a result, problems in the gastrointestinal tract may appear. At later stages (at the very end of the third trimester), diarrhea can be caused by the female body preparing for the upcoming birth. If stool with blood in a woman in late pregnancy is not associated with painful symptoms and is an isolated case, the use of medications can be abandoned. This may be the result of a burst vessel.
However, the causes of diarrhea can be more serious, since pregnant women have reduced immunity. For example, any infections can cause a large amount of blood in the stool during pregnancy, as well as frequent diarrhea. Only a specialist can determine the exact causes and prescribe treatment.
Fecal occult blood test
Testing feces for occult blood will help identify various diseases.
At first glance, blood in fecal waste is bad. But if you look at the situation from the other side, then detecting blood in the stool will help identify the presence of pathologies in the gastrointestinal tract, and throughout the body in general.
However, there are also cases when a person has health problems, but he does not notice blood in his stool. If there is no blood outside the stool, this does not mean that it is not in it at all. That is why it is necessary to periodically take an occult blood test.
Read: Stool analysis for Helicobacter pylori: features of the procedure
The occult blood test is carried out in a very unique way. The purpose of the analysis is to detect hemoglobin in fecal waste. To get accurate results, you must strictly follow all preliminary recommendations and rules, because Meat eaten the day before may give false results and the analysis will have to be repeated.
To avoid such misunderstandings, you should exclude all foods that contain iron from your diet. It is necessary to exclude products for a period of 4 days before undergoing analysis. You will also need to stop taking medications that increase hemoglobin.
If the test result is positive, then there are some diseases in the gastrointestinal tract. This result may indicate the presence of pathologies in the gastrointestinal tract or cancer. That is why a person is sent for a repeat occult blood test.
Thus, doctors want to play it safe and make sure the results obtained are correct. Only after undergoing a re-analysis the doctor will make a final conclusion and prescribe treatment. Occult blood can act as an indicator for the following diseases:
- Stomach and duodenal ulcers
- Malignant neoplasms
- Ulcerative colitis
- Polyps in the intestines
Don't be ashamed of yourself. Health comes first. Get tested periodically, get examined, because this is the key to your long and happy life.
People whose age exceeds 50 years are recommended to undergo such an analysis annually.
Colon diseases
Unchanged, that is, scarlet blood in the stool indicates damage to the lower intestines: the sigmoid or rectum, possibly the anal area.
Fecal masses are covered with scarlet streaks, since they reach the surface after the formation of feces:
Fissures in the anus and lower rectum. The occurrence of cracks may be a consequence of constipation, which is chronic or often recurrent. The appearance of blood in the feces means that the process has worsened. Treating this condition is quite simple if it is not in a complicated form. A diet is prescribed to normalize stool and local medications to heal cracks.
- Haemorrhoids. Occurs due to chronic constipation and increased intra-abdominal pressure. Blood in the stool in women as a symptom of hemorrhoids occurs during pregnancy and gradually subsides after the birth of the child. Men “get” this disease as a result of heavy lifting. Treatment is carried out using conservative and surgical methods. For uncomplicated hemorrhoids, drug therapy using oral and topical medications is used. Severe or advanced forms require surgical intervention.
- Oncological processes in the sigmoid and colon can cause blood clots in the stool. The treatment is quite complex and specific.
- Nonspecific ulcerative colitis. The disease is caused by immunological changes, which are characterized by lesions of the colon mucosa with the occurrence of an inflammatory process. In a state of moderate to severe severity, bleeding occurs with an admixture of mucus and blood - “raspberry jelly” stool. If these symptoms occur, treatment with corticosteroids and sulfonamides in the form of oral and local agents (suppositories and enemas) is prescribed.
- Crohn's disease is a pathology with symptoms similar to ulcerative colitis, plus blood clots in the stool. But the localization of the lesion is slightly higher. And the origin of the disease is autoimmune in nature against the background of genetic predisposition.
We should not forget that any damage to the mucous membrane of the lower intestine can occur with inflammation. And at the same time, infectious microflora may join, which will make the treatment process more difficult and longer. Also, some conditions (ulcerative colitis or Crohn's disease, for example) can develop into oncology if treated untimely or incorrectly. By the way, patients with these pathologies are forced to take medications almost for life in order to avoid relapses. Diet is also necessary.
Interesting fact. The etiology of the origin of nonspecific ulcerative colitis and Crohn's disease has not yet been fully studied. They talk about the hereditary factor and the influence of the psychological state. Severe stress can trigger an autoimmune failure and trigger the process of self-destruction.
Mucus in a child's feces
The predominance of mucous discharge in a newborn baby is normal. Since the intestinal tract of the baby is not yet populated with a sufficient number of representatives of normal microflora. Beneficial microorganisms settle in the baby’s intestines along with mother’s milk. After colonization of the intestines and adaptation of the newborn, the mucous secretion gradually disappears from the feces. If this does not happen, then you should pay attention to:
- the diet of a nursing mother may be unbalanced;
- sterility of breast milk. If it is not sterile, pathogenic microorganisms enter the child’s body, which negatively affects his health. To clarify sterility, you can conduct a study - culture of breast milk;
- allergy to lactose in infants;
- the possibility of developing thrush in a child, which was transmitted to him by the mother during childbirth;
- changing artificial formula for nutrition;
- early introduction of complementary foods is irrational.
White mucus in a child’s stool is detected due to dysbacteriosis. This is especially true in the first years of life, when the baby tastes various objects that may be unwashed. Among the pathological causes, the following should be highlighted:
- acute stage of an infectious disease of various etiologies;
- helminthic infestation;
- Crohn's disease;
- development of neoplasms in the gastrointestinal tract;
- intestinal obstruction;
- colitis;
- allergic food intolerance.
You should take into account the baby’s incorrect diet, medications and the possibility of hypothermia.
How to get tested
A therapist, oncologist, surgeon, or gastroenterologist can prescribe the test. Before taking the test, preliminary preparation is required. Doctors give the following recommendations. 72 hours before the test, exclude iron-containing foods from the menu, as well as tomatoes and green vegetables and fruits. You should not eat meat or fish, as they contain hemoglobin.
For a week, stop taking medications such as aspirin, laxatives, iron tablets, non-steroidal anti-inflammatory drugs. If it is not possible to stop drug therapy, then you need to inform your doctor about the medications you are taking.
Do not consume foods that change the color of stool. The collection of material should be carried out before diagnostic manipulations in the digestive tract. It is not recommended to do an enema or take laxatives to speed up the collection of a sample for analysis.
The sample should not be collected during menstruation. If X-ray diagnostics were performed, the analysis can be taken only after 2-3 days.
If the subject has periodontal disease, in which there is severe bleeding of the gums, then the day before collecting stool, it is not recommended to brush your teeth, since blood that gets into the stomach can give a positive result.
You need to take material from three different sides of the stool. An unreliable answer is likely if water or urine gets into the sample. In order to eliminate this, it is recommended to lay oilcloth on the toilet. The test sample must be placed in a plastic container (can be purchased at a pharmacy) and brought to the laboratory within the next 2-3 hours.