Causes of pulmonary edema
Swelling of the main organ of the respiratory system is a consequence of many diseases from the fields of cardiology, urology, pulmonology, and neurology. In women, the clinical syndrome accompanies diseases of the reproductive system.
What diseases cause pulmonary edema:
- bronchitis, asthma, lobar pneumonia, tumors (cancer), emphysema, pneumosclerosis;
- heart defects, hypertension, infectious inflammation of the inner lining of the heart, acute myocardial infarction, replacement of cardiac muscle tissue with connective tissue, valve deformation;
- infections that cause severe intoxication (viral diseases) - influenza, whooping cough, measles, diphtheria, scarlet fever, polio;
- failure of kidney function, acute impairment of glomerular filtration, nephrotic syndrome (high protein content in the urine);
- liver cirrhosis, acute pancreatitis, intestinal obstruction;
- stroke, cerebral hemorrhages, tumors, infectious meningitis, encephalitis, craniotomy;
- poisoning with caustic substances, alcoholic beverages, narcotic substances, and medications.
Classification of pulmonary edema
Depending on the mechanism of development, pulmonary edema is divided into:
- cardiogenic, or cardiac, hydrostatic, hemodynamic;
- non-cardiogenic – develops in severe respiratory distress due to increased permeability, acute lung injury or respiratory distress syndrome, including in newborns with organ immaturity;
- mixed.
The described types of pulmonary edema have different causes; different treatment regimens are used for their treatment, but due to similar clinical symptoms, it is difficult to differentiate them.
In healthy lungs, the movement of fluid and proteins occurs through small spaces between endothelial cells. These substances are filtered from the circulation not into the alveoli, which have a dense structure, but into the alveolar interstitial space. After penetration into the interstitial areas, the fluid enters the peribronchial space, from where it is removed through the lymphatic system and enters the bloodstream. In this case, the hydrostatic pressure in the pulmonary capillaries is approximately equal to the force that is responsible for plasma filtration.
As the pressure in the capillaries increases, transvascular filtration of fluid intensifies. This occurs due to an increase in pulmonary vein pressure due to increased diastolic pressure in the left ventricle and atrium. Under the influence of these forces, a liquid with a small amount of proteins overcomes the epithelium of the lungs and fills not only the intercellular space, but also the alveoli. This is how cardiogenic edema develops.
Non-cardiogenic edema is caused by an increase in vascular permeability of the lungs, resulting in fluid being directed into the pulmonary interstitium and air spaces. At the same time, it contains a significant amount of proteins due to the greater permeability of the vascular membrane for the release of plasma proteins.
According to the course of the pathological process, the following types of edema are distinguished:
- acute – develops within 4 hours, in most cases ends in death (occurs with traumatic brain injuries, anaphylaxis, heart attack);
- subacute - the graph of symptoms resembles waves, signs of swelling either increase or subside, diagnosed with intoxications of various natures;
- fulminant – develops in a few minutes, the person dies before resuscitation begins;
- protracted – development period from 12 hours to 3-5 days, symptoms erased, occurs in patients with chronic diseases of the respiratory and heart organs.
First aid
When the first signs of the disease appear, you should immediately call an ambulance.
Before her arrival, it is necessary to provide first aid to the person:
- Place it in a reclining position, with your legs down (horizontal and vertical positions are strictly prohibited).
- It is recommended to immerse the patient's feet in hot water.
- Provide access to fresh air into the room.
- To avoid increased blood pressure and increased blood flow to the right atrium, it is necessary to tighten tourniquets on both thighs. They are applied for 15-20 minutes; they cannot be tightened too much. After time, the tourniquets must be removed, gradually loosening them. The pulse must be constantly monitored.
- If alcohol is present, the patient must inhale its vapor.
- If you have Nitroglycerin in your medicine cabinet, 1 tablet should be placed under your tongue.
- It is recommended to give the patient a diuretic (for example, Lasix).
While transporting the patient to a medical facility, he is given artificial ventilation and Morphine is administered (for severe pain).
Diagnostic Basics
X-rays and laboratory tests take first place in the diagnosis of pulmonary edema. The examinations take place simultaneously with emergency care.
Changes in blood gases are studied. First, hypocapnia develops—carbon dioxide (CO2) deficiency. Then the oxygen tension (O2) drops. At the late stage, the amount of CO2 increases rapidly and O2 values decrease. Alkaline substances accumulate in the blood and tissues.
Biochemical screening is also carried out to determine the causes of the pathology - total protein, urea, creatinine are assessed, liver tests, and a coagulogram are performed.
When examining the heart on a cardiogram, signs of ischemia of the heart muscle, arrhythmia, and enlargement of the left ventricle may be detected.
When using non-invasive research methods, if diagnostic discrepancies arise, it is necessary to quickly determine the cause of the developed condition and prescribe adequate treatment, then resort to catheterization of the pulmonary artery.
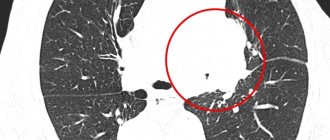
X-ray for pulmonary edema is the main examination method for making an accurate diagnosis. In the center of the image there is a pronounced darkening in the form of a symmetrical “butterfly” (the main feature).
The image allows you to timely identify the stage of development of swelling, assess the dynamics, and determine the mechanism of the occurrence of pathology.
Prevention
People suffering from chronic diseases are primarily at risk. To reduce the likelihood of complications such as pulmonary edema, it is necessary to visit your doctor twice a year and, if necessary, undergo a preventive course of treatment. This is especially true for people suffering from various disorders of the cardiovascular system.
In addition, dietary adjustments are required. Salty, fried, fatty, smoked foods should be excluded from it, as they contribute to fluid retention in the body. When cooking, it is recommended to use salt in minimal quantities.
Moderate physical activity is also indicated.
Compliance with these rules does not exclude the occurrence of pulmonary edema, but significantly reduces its likelihood.
What signs of pulmonary edema can be seen on x-ray?
The following signs of pulmonary edema are visible on x-ray:
- the boundaries of the roots of the lung and heart are expanded;
- darkening in the root system of the organ;
- changes in the arteries, the vascular network is lubricated;
- diffuse focal fusion;
- infiltration (compaction) of tissues;
- strengthening of the pulmonary pattern in acute edema.
Expansion of the peribronchial space
Due to swelling of the walls of the bronchial tree, the peribronchial space expands, peribronchial couplings appear - thickening of the vascular walls. The diameter of the vessels and bronchi increases, and the contours blur and become unclear. At the same time, the clearance decreases.
Pleural effusion
The accumulation of edematous fluid contributes to the thickening of the pleura and the appearance of pleural effusion. Initially it appears on the right, and then is observed on both sides.
With pulmonary edema, a typical sign is observed in the X-ray photo - thickening of the layers of the interlobar pleura, located horizontally. This is clearly visible in forward projection.
Kerley lines types A, B, C and septal bands on a radiograph
One of the radiological signs is the appearance of Kerley lines (linear darkening in the parenchyma). The symptom is caused by compaction of the stroma (the framework of the lung made of connective tissue).
With swelling, type B lines are most often found - they are located parallel along the periphery of the organ, along the border between the lobes. Length – no more than 1 cm. They come into contact with the pleura, most often localized in the costophrenic angles.
Type A Kerley lines, 2 to 6 cm long, are found less frequently and only together with other lines (B, C). They have no branches and run diagonally from the main bronchus to the periphery.
Curley C lines are extremely rare. They appear in the form of reticular striations over the entire area of the organ.
Air bronchogram
In case of pulmonary edema, the X-ray image shows an air bronchogram - air-filled bronchi. In parallel, pulmonary consolidation is observed - the alveoli are filled not with air, but with liquid. The image shows infiltration and opacity of the tissue.
The air bronchography symptom is the most important criterion in differentiating hydrostatic edema and edema resulting from a violation of the integrity of the capillaries. The X-ray picture of damaged vessels is not so dynamic. Changes in the lungs are detected on the second or third day and progress over several days. With such edema, there are no Kerley lines or peribronchial couplings.
Pulmonary edema x-ray: x-ray picture and description
The disease is a pathological condition accompanied by an increase in fluid levels in the pulmonary interstitium.
The causes of the condition are varied, but there are two main ones: left-sided heart failure and structural damage to the alveoli during adverse effects on them. Edema is often a consequence of pulmonary hypertension.
Signs of pathology
Signs of pulmonary edema are easy to see on x-ray. As a rule, they have a pronounced character. These symptoms include:
- Expressiveness of the drawing in the photograph.
- Blurred contours of the vascular network.
- Increased size of the heart shadow.
- The appearance on x-ray diagnostics of long and short lines in the central and transverse areas of the image.
- The presence of infiltrates in the peribronchial parts.
- The silhouette of a bat appears in the photo.
- Presence of patchy shade areas.
Having studied the X-ray picture of pulmonary edema, a specialist can easily make an accurate diagnosis. Often, the description of this pathological process includes changes in the size of the pulmonary artery, heart, and significant redistribution of blood in the lungs. This picture can be easily seen in an X-ray image. We see an example of an X-ray image of the lungs in a state of edema in the photo.
Folk remedies
irinazaitseva.ru
Treatment of pulmonary edema is carried out in the intensive care unit (ICU) under constant monitoring of oxygenation and hemodynamics. Unfortunately, in some cases, pulmonary edema can be fatal.
In addition, even after successful relief of the pathological process, complications such as congestive pneumonia, pneumosclerosis, pulmonary atelectasis, and ischemic damage to internal organs may develop.
The key to a favorable outcome is the timely identification of the underlying disease that caused the development of pulmonary edema, as well as the earlier initiation of pathogenetic therapy.
In addition, it is necessary to promptly diagnose and subsequently treat diseases that, in the absence of specialized treatment, can lead to the development of pulmonary edema. That is why it is strongly recommended not to self-medicate at home, but to immediately seek help from a qualified specialist.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Diagnostic Basics
As a rule, these symptoms appear against the background of a sharp decrease in blood pressure. If the x-ray picture confirms the primary diagnosis, the doctor additionally listens to the chest to identify irregular, dull tones in the heart. By listening to the sounds, the specialist can easily identify bubbly, dry rales in the lower parts of the lungs.
During an exacerbation of interstitial pathology, the patient experiences arrhythmia and coronary insufficiency.
To clarify the picture, the doctor prescribes a number of additional examinations, including:
- Ultrasound of the heart and lungs.
- Blood test to detect acidity levels.
- Other necessary studies, in the opinion of the doctor.
Curley lines of different types - why they appear
Kerley lines are of three types (A, B, C) and appear in the following diseases:
- Heart failure with blood stagnation;
- Pneumofibrosis with the proliferation of fibrous tissue in the lungs;
- Carcinomatosis (cancerous lesion);
- Deposition of heavy metals;
- Kerley bands type B characterize chronic diseases (fibrosis).
The most common are Kerley type A bands. Interstitial pneumonia often manifests itself on an x-ray with precisely these x-ray symptoms.
Acute pulmonary edema
Pulmonary edema is one of the most serious and frequent complications of severe injuries, surgical interventions, many diseases, allergic conditions and poisonings According to GR
Cameron (1948), based on the results of 500 postmortem studies, pulmonary edema in skull fractures is observed in 63%, multiple skeletal injuries in 61%, pulmonary embolism in 31% of cases.
The development of pulmonary edema is usually associated with a violation of the water-electrolyte balance, causing the liquid part of the blood to sweat into the interstitial tissue of the lungs and alveoli. The following factors are of decisive importance: a rapid increase in hydrostatic pressure in the capillaries of the pulmonary circulation, increased permeability of the vascular wall, a decrease in colloid-osmotic plasma pressure and decrease in intrapleural pressure
Source: https://MedikTest.ru/issledovaniya/rentgen-kartina-oteka-legkih.html
Severity
Depending on the severity of symptoms, the disease has 4 degrees of severity:
- First. Another name is pre-edema. Signs of the disease usually go unnoticed. Slight shortness of breath appears and breathing quickens.
- Second. It is characterized by increased shortness of breath, wheezing is clearly audible when breathing.
- Third. Wheezing and shortness of breath intensify so much that they can be heard at a considerable distance.
- Fourth. Other symptoms of pulmonary edema are added: general malaise, increased sweating, rapid heartbeat, pale skin, etc.
CT diagnostics of lung damage due to covid-19. lecture for doctors
One of the most life-threatening conditions for a person is pulmonary edema. This condition occurs as a result of the release of blood from the vessels through the capillary wall into the airborne part of the pulmonary system.
The main cause of the development of edema is acute left gastric failure. This condition can be identified by clinical symptoms. But to complete the picture, doctors prescribe x-rays of the lungs for edema.
What is interstitial fluid?
One of the types of intercellular fluids is interstitial; its other name is tissue.
It makes up approximately 25% of the total human body weight and is a solution containing mainly nutrients and metabolic end products.
At normal levels of tissue fluid pressure, its volume does not change significantly. When pressure increases or under the influence of other factors, the amount of fluid increases significantly, which leads to edema.
Mechanism of disease development
Obstructive (
) lung diseases are characterized by a chronic course and similar symptoms with a wide variety of x-ray patterns. Smoking is one of the main factors that lead to this group of diseases. As a result of the lack of oxygen and chronic inflammation, connective tissue develops in the lungs, which is also called pneumosclerosis.
Diseases that have an obstructive component include:
- chronic obstructive pulmonary disease;
- Chronical bronchitis;
- emphysema;
- bronchial asthma and some others.
Diagnosis of this group of diseases using X-ray of the lungs is carried out first, but it is not always the only one.
Thus, in case of bronchial asthma, doctors confirm the allergic component of the disease using special tests.
Particular attention is paid to functional tests, since airway obstruction significantly reduces the ability to inhale and exhale sufficiently.
Chronic obstructive pulmonary disease is an inflammatory disease, which is accompanied by a violation of the passage of air through the bronchi and is manifested by chronic cough, shortness of breath and sputum discharge.
Impaired bronchial obstruction consists of several factors, including increased mucus production, spasm of the muscle wall, and swelling of the mucous membrane. Chronic obstructive pulmonary disease is distinguished by a number of radiological signs:
- in the initial stage of the disease, significant changes in the lungs and bronchi may be absent, but a slight increase in the pulmonary pattern is determined;
- subsequently, a narrowing of the lumen of the bronchi and a simultaneous thickening of their walls appears;
- the lungs increase in volume, on x-ray this is reflected in the clearing of the lung fields;
- the diaphragm occupies a lower position - at the level of the seventh or eighth rib;
- the difference in the area of the lung fields in the image during inhalation and exhalation is almost invisible;
- the diameter of the pulmonary arteries in the region of the lung root is increased (right artery - more than 17 mm, left - more than 27 mm);
- the pulmonary pattern becomes reticular in nature due to pronounced fibrosis of the vascular walls;
- in the late stage of the disease, deformations of the walls of the bronchi (so-called bronchiectasis) are detected.
Chronic obstructive pulmonary disease develops very slowly and often unnoticed by the patient, but it is dangerous because it provokes a large number of complications, both local and general. Chronic obstructive disease may cause pneumonia, emphysema, pulmonary hypertension, respiratory failure, and heart failure.
Emphysema is a pathological condition in which the alveoli of the lung expand due to deformation of the walls. Emphysema is one of the complications of chronic obstructive pulmonary disease. Inflammation of the terminal sections of the respiratory tract is accompanied by the release of enzymes that destroy the alveoli.
At the same time, they stretch due to the fact that the mucus that fills the lumen of the bronchi acts as a valve - air enters the lungs when inhaling, and when exhaling it remains blocked in the alveoli. As a result, the lung tissue is stretched, and expansions of various shapes and sizes are formed.
The following types of pulmonary emphysema are distinguished:
- acinar emphysema – the alveolar part of the lung (acinus) is affected;
- uneven (irregular) emphysema - appears in the area of scar changes in the lungs;
- bullous emphysema - combines several acini into large saccular expansions - bullae.
On x-ray, emphysema is characterized by extensive clearing of the pulmonary field. The pulmonary pattern is weakened, the dome of the diaphragm is lower than usual, and it is inactive during breathing.
The ribs are located almost horizontally, due to the fact that the chest is increased in volume. The mediastinum and cardiac shadow are narrowed.
Computed tomography (CT) with good resolution can detect bullae and septal deformities in the lung tissue.
Bronchial asthma, like obstructive pulmonary disease, is characterized by impaired bronchial patency due to swelling of the mucous membrane, spasm of the muscular wall of the bronchi.
However, in bronchial asthma this phenomenon is observed as a result of an allergic reaction.
In asthma, the bronchial wall is extremely sensitive to contact with allergens such as pollen, wool, and molds.
Bronchial asthma is diagnosed using a set of procedures, the main one of which is the study of external respiratory function.
Unlike chronic obstructive bronchitis, in bronchial asthma the functional volumes of the lungs increase when the allergic component is removed by inhalation of medications.
In addition, a series of allergy tests are performed to determine allergens.
X-ray examination for bronchial asthma is carried out, first of all, to exclude other diseases, mainly of an inflammatory nature (pneumonia, acute bronchitis).
In patients with bronchial asthma, X-rays show an increase in the transparency of the lung fields on X-rays. If an x-ray is taken during or immediately after an asthma attack, shadows may be found in the image that quickly disappear.
They are accumulations of mucus in narrowed areas of the bronchi.
Pneumosclerosis can develop due to various reasons:
- pneumonia;
- chronic obstructive pulmonary disease;
- inhalation of toxic and poisonous substances;
- hemodynamic disturbances in the pulmonary circulation;
- some hereditary diseases.
X-ray examination allows you to detect morphological changes in the lung tissue, identify the prevalence, nature and degree of pneumosclerosis. Pneumosclerosis can be local or diffuse. Focal pneumosclerosis is observed with lobar or segmental pneumonia, infarction of a portion of the lung.
Source: https://cordiacardio.ru/rentgen/rentgenologicheskaya-kartina-oteka-legkih.html
Treatment
Interstitial pulmonary edema is a serious disease for which the patient requires intensive care. All treatment measures are carried out only in a hospital setting under the constant supervision of doctors.
Treatment for interstitial pulmonary edema includes:
- use of an oxygen mask;
- increased blood pressure (with a significant decrease);
- normalization of heart contractions;
- elimination of pain syndrome;
- intravenous administration of diuretics;
- infusion of blood plasma into the patient (if protein levels are low);
- taking glucocorticosteroids (for bronchial spasms);
- antibiotic therapy (if an infection is detected in the body, for example, sepsis).
Depending on the results of a comprehensive examination, all measures and medications are prescribed individually, and each patient has his own treatment regimen.
With a quick diagnosis and timely action, the patient is usually cured and discharged from the hospital after about 3 weeks.
Mechanism of disease development
The pulmonary interstitium is a connective tissue that is the basis of the entire respiratory system. Normally, the interstitial space allows up to 20 ml of fluid to pass through it every hour. It does not enter the alveoli, which is due to the anatomical structure of the lungs. The end products of metabolism are eliminated from the body thanks to the work of the lymphatic system.
Thus, interstitial and alveolar pulmonary edema are not independent diseases; they develop against the background of existing pathologies in the body.
As a rule, symptoms of interstitial pulmonary edema appear at night, when a person is asleep. During the daytime, a weak cough periodically occurs, to which attention is often not focused.
A few hours later, the patient’s condition worsens significantly:
- the skin turns pale;
- shortness of breath appears, which does not subside even when the person is at rest;
- it becomes difficult to take deep breaths, up to the impossibility of taking them;
- due to hypoxia, headaches begin to bother;
- sweating and saliva production increases;
- cyanosis appears in the area of the nasolabial triangle;
- wheezing can be clearly heard when breathing;
- tachycardia occurs.
If you contact a medical facility in a timely manner, the chances of a successful treatment outcome increase significantly. Delay or unwillingness to receive qualified help threatens the transition of the disease from the interstitial to the alveolar form, which increases the risk of death.
Regarding bedridden patients, their signs of the disease are less pronounced.
Often patients complain of:
- lethargy;
- drowsiness;
- shortness of breath;
- rapid breathing;
- lack of air.
The situation is complicated by the fact that the horizontal position does not allow inhaling large volumes of air, due to which blood circulation worsens. In addition, accumulating sputum provokes the development of an inflammatory process. In such cases, pneumonia may occur.
Pulmonary hypertension
Pulmonary hypertension is an increase in pressure in the pulmonary artery caused by pathology of the cardiovascular system or lung diseases (for example, chronic obstructive pulmonary disease). Chronic obstructive pulmonary disease (COPD) is accompanied by emphysema with disruption of the structure of the lungs, a significant decrease in the number of alveoli due to their destruction, the formation of bullae, fibrosis, and a decrease in the surface area for gas exchange in the lungs (see article “X-ray: Chronic obstructive pulmonary disease”). As a result, a reflex spasm of small arteries occurs, with further development of connective tissue in their walls, which leads to obliteration (closure, fusion) of the lumen of blood vessels.
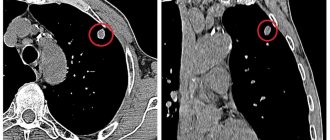
The X-ray picture of pulmonary hypertension is characterized by dilation of the main and hilar pulmonary arteries (see article “Radiography: Chronic obstructive pulmonary disease”, Figure 1, 2). Closer to the periphery of the lungs, the caliber of the vessels decreases sharply - a so-called “jump in caliber” of the pulmonary arteries is noted. Due to the expansion of the left and right pulmonary arteries, the roots of the lungs expand (Figure 8, 9), while the structure of the roots is preserved, the outer contours are clear and even (in contrast to the “lumpy”, polycyclic roots with lymphadenopathy, and non-structural roots with stagnation in the small circle of blood circulation). Due to the “jump in caliber” of the pulmonary arteries, the roots of the lungs look “chopped off”. Often there is a “bulging” of the pulmonary trunk arch along the left contour of the heart (see Figure 10).
Figure 8. Pulmonary hypertension in cardiac pathology. A – radiograph in direct projection: the image shows the expansion of the left and right pulmonary arteries with a smooth, clear contour, and the expansion of the hilar arteries. There is also a significant expansion of the cardiac shadow. B – radiograph in the right lateral projection: the shadows of the aortic (see arrow) and mitral (see index) valve prostheses are determined
Figure 9. Severe pulmonary hypertension with long-standing myocardial atrial septal defect: there is a significant expansion of the roots of the lungs due to the pulmonary arteries
As a method of diagnosing pulmonary hypertension based on X-ray signs, measuring the diameter of the descending branch of the right pulmonary artery . On a radiograph taken in a direct projection, this measurement is carried out at the level of the intermediate bronchus, which is determined in the body of the right root in the form of a clearing strip medially from the pulmonary artery (Figure 10). If the dilatation of the descending branch of the right pulmonary artery is more than 20 mm, this is a sign of pulmonary hypertension. Normally, the width of the descending branch of the right pulmonary artery in women does not exceed 16 mm, in men - no more than 18 mm.