Tuberculosis infection is an important social and medical problem. The cause of the disease is a mycobacterial infection, the provoking factor of which is low immune status. Damage to any organ is possible: lungs, bones, muscles, mediastinum, gastrointestinal tract. Pulmonary manifestations are predominantly detected.
Computed tomography (CT) allows you to identify tuberculosis of various locations - lungs, lymph nodes, bones, assess the extent of the process and monitor treatment. Previously, radiography (fluorography) revolutionized the diagnosis of this disease.
Tomographic methods have now further expanded diagnostic capabilities.
Indications for CT scan for tuberculosis
Computed tomography is performed when suspicious changes are detected on the x-ray that cannot be interpreted unambiguously.
- CT is used to detect tuberculosis of the mediastinal lymph nodes, which are difficult to evaluate with traditional radiography.
- Bone involvement is another indication.
Rarely, research is performed for mycobacterial infection of another location.
Benefits of CT Scan
Compared to radiography, CT allows you to get a holistic picture, simultaneously assessing lesions in the lungs, skeletal lesions, and changes in the lymph nodes.
- This research method has better resolution. CT reveals many more lesions than radiography.
- Small, loose lesions are visible, not even reaching a millimeter in diameter. Diagnostic accuracy improves.
CT is inferior to radiography (fluorography) in speed and widespread use. Although ideas for screening CT studies have recently appeared, all of them are far from being implemented. Radiography (fluorography) remains a tool for mass examination.
Attention: undergo fluorography annually. This study allows you to identify gross changes and orient yourself with further tactics. Most patients with pulmonary tuberculosis did not undergo fluorography for several years before pathological changes were detected.
Causes
This form of the disease appears due to re-infection of the body against the background of an incompletely eliminated primary infectious process or activation of mycobacteria in old pathological foci. In the first case, pathology develops during prolonged communication with a patient who has been diagnosed with an open form of tuberculosis.
Activation of Koch's bacillus in the body occurs when living in unfavorable social and living conditions, in regions where an unfavorable epidemiological situation has been recorded, or if there is no specific immunization of the population.
Focal tuberculosis in both cases appears against the background of weakened immune forces, which is facilitated by:
- stressful situations;
- overwork;
- poor quality nutrition;
- bad habits;
- pathologies such as stomach ulcers, diabetes, pneumoconiosis;
- taking immunosuppressants.
Focal pulmonary tuberculosis: contagious or not
The causative agent of the pathology is Koch's bacillus, which affects the lungs. It can be transmitted from a sick person as follows:
- by airborne droplets;
- when using clothes, dishes and other personal items of the patient.
Therefore, this pathology is considered contagious, transmitted from tuberculosis patients with an open form.
CT picture of tuberculosis
Findings found in tuberculosis
| Nakhodki | Description |
| Infiltration | Looks similar to pneumonia of a different etiology, the final diagnosis is established by examining sputum or by serological methods, for example, by enzyme immunoassay |
| Outbreaks | Round or irregular in shape, 1-10 mm in diameter, often with calcifications, cavities, usually in the upper lobes of the lungs |
| Caverns | Cavities of irregular shape, 1-10 cm, with walls 1-5 mm thick, filled with gas and (or) liquid; often combined with calcifications and fibrosis |
| Caseous necrosis | An area of cheesy (caseous) melting of lung tissue, an extremely severe complication of infiltrative tuberculosis |
| Fibrosis | Often fibrous changes (cords, adhesions) are combined with atelectasis, bronchiectasis, cavities, calcifications, tuberculomas, infiltration (a picture of cirrhotic lesions) |
| Tuberculoma | A volumetric formation, delimited by a dense capsule from healthy tissue, containing caseous masses in the center. Tuberculoma occurs due to the limitation of the infectious process |
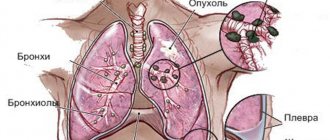
| Fluid in the pleural cavity | Liquid contents appear in the chest cavity due to irritation (inflammation) of the pleura. As the amount of fluid increases, it compresses the lung, leading to breathing problems |
| Lymphadenopathy | Enlarged lymph nodes of irregular, round or elongated shape, with a disrupted structure, without fatty gates |
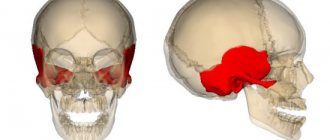
| Damage to bones, joints, muscles | Areas of bone tissue destruction, mainly in the vertebrae, with accumulations of pus in the soft tissues near the bones and joints |
| Damage to other organs | Lesions from the gastrointestinal tract and urinary system are rarely detected, mostly by chance |
Complications
Possible complications include:
- superinfection, such as fungal colonization;
- empyema - with tuberculous pleurisy;
- fibrothorax - replacement with fibrous tissue;
- fistulas - broncho-pleural, tracheo-esophageal;
- bronchiectasis - traction;
- pulmonary artery pseudoaneurysm.
Please note: complications are typical for advanced infection. If the pathology is detected in a timely manner, the risk of complications is minimal. Do fluorography in a timely manner.
Tuberculoma
Tuberculoma on chest CT is an encapsulated (having a dense wall) formation, most often more than 1 cm in diameter. Most often, tuberculomas are localized in the upper lobes, peripherally. The structure of tuberculoma is heterogeneous - a soft tissue component, caseosis or calcium inclusions can be detected in the center. Sometimes tuberculomas can be multiple. Differential diagnosis of tuberculomas must be carried out with hamartomas and peripheral lung cancer.
CT. Tuberculoma of the upper lobe of the right lung
Tuberculomas of various localizations identified by computed tomography
Variants of tuberculosis infection
Tuberculosis is diverse. The CT picture depends on:
- on the patient’s immune status;
- time since infection;
- type of pathogen;
- localization of the primary infection.
This disease must be differentiated from pneumonia of other etiologies, sarcoidosis, and tumors.
Please note: Tuberculosis can affect any organ, not just the lungs. Bones, joints, and the gastrointestinal tract are often affected.
Primary tuberculosis complex (PTC)
PTC occurs when a child or adolescent is initially infected with tuberculosis. A focus(es) or area of infiltration of the lung tissue is detected in combination with an enlargement of the mediastinal lymph nodes. Focal changes and lymph nodes in the mediastinum are connected by a “path” (lymphangitis).
Tuberculosis of mediastinal lymph nodes
Isolated lymph node involvement is rarely detected. CT scan reveals enlarged lymph nodes in the mediastinum.
- Their shape is round, elongated, or irregular.
- The transverse dimension often exceeds 10 mm.
- The structure of the lymph nodes may change; necrosis occurs in the center of the node, leading to a decrease in density. After contrast is administered, the center of the lymph node does not accumulate it.
Peripheral sections accumulate contrast in the form of a “rim”. When inflammation subsides, calcifications are found in the lymph nodes. Rarely, a calcified lymph node can pierce the wall of the bronchus, entering its lumen and causing obstruction.
Infiltrative form
Infiltration with mycobacterial infection resembles that with “ordinary” pneumonia. An area of compaction is detected in the lungs, against which the lumens of the bronchi can be traced.
The localization of the infiltrative process is specific - the upper lobes. Infiltration is often combined with lesions, cavities, and effusion.
Infiltrative pulmonary tuberculosis
The image (CT) shows multiple areas of infiltration in the upper lobe on the left (red arrows) against the background of tuberculous exudative pleurisy (blue arrow).
Miliary tuberculosis
This is a severe form with severe intoxication and high mortality.
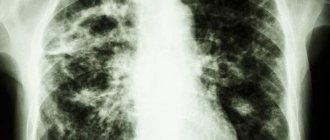
- Miliary tuberculosis on CT is characterized by multiple small foci (several millimeters in diameter) in all parts of the lungs.
- Lesions also appear in other organs, because the infection spreads through the bloodstream throughout the body, but the lungs are primarily involved. The prognosis in this case is unfavorable.
Disseminated variant
The term dissemination means spreading. Tuberculosis can spread through the blood or lymph.
The miliary and disseminated forms are similar, but in the first case the emphasis is on the size of the lesions, in the second on their widespread nature. Dissemination means a poor prognosis.
- CT scan shows multiple lesions of varying sizes scattered throughout the lung parenchyma.
- Calcifications, infiltrative changes, and pleurisy may be detected.
Cavernous variant
Cavern is a cavity formation formed as a result of decay and necrosis of lung tissue.
- The cavity is formed by cheesy masses from the inside, granulations and fibrous tissue from the outside.
- It occurs against the background of an infiltrative process or from tuberculoma during reactivation of the infection.
- It can be detected in isolation or in combination with other variants (infiltrative, focal).
Cavernous tuberculosis
Fibrous-cavernous tuberculosis
This option is characterized by the presence of a cavity (one or several) against the background of severe pneumofibrosis - adhesions, bands, traction bronchiectasis.
Often a consequence of massive infiltration. Usually indicates a more severe course of the initial process. Can be combined with other options.
Cirrhotic form
The final version with pneumofibrosis (multiple adhesions), bronchiectasis, emphysema, cavities, residual areas of infiltration, calcifications. The peculiarity is the preservation of the activity of the tuberculosis process.
Most often, pneumocirrhosis develops in patients with advanced lesions or when therapy is ineffective.
Tuberculoma
With successful treatment and normal immune status, the focus of mycobacterial infection gradually delineates. Tuberculoma is formed.
- It is a cluster of caseous masses delimited by a dense capsule. Calcifications are almost always found.
- Tuberculoma is not the target of therapy.
- If treatment is stopped, the infection may reactivate with the formation of a cavity.
- Under favorable conditions, tuberculoma decreases in size, its contents become denser, and calcification forms.
Damage to the trachea and bronchi
Specific inflammation of the respiratory tract caused by mycobacterial infection. It practically never occurs on its own and is always associated with damage to another location.
On the surface of the trachea and bronchi, areas of inflammation and ulcers form. Then fistula tracts may appear. This form may occur secondary to drainage of a tuberculous abscess.
Tuberculous pleurisy
Pleurisy is an inflammatory process that almost always leads to the appearance of liquid contents in the chest.
Pleurisy is a complication of any other variant of tuberculosis with localization of changes near the pleura. The volume of liquid ranges from a few milliliters to a liter or more. Intrapulmonary lesions are very often found.
Osteoarticular form
The vertebrae are predominantly affected, then large joints, such as the hip. Areas of destruction (melting) of bone tissue are identified along with pronounced deformation of the articular surfaces. In the soft tissues near the source of infection, an abscess (leap) is often identified in the form of an accumulation of low-density fluid with a denser rim.
Alternative diagnostic methods
To date, medical equipment development engineers (America) and Rentgenprom CJSC (Russia) have developed a new type of tomograph - tomosynthesis.
The uniqueness and value of this development for people with tuberculosis is:
- in the frequency of examinations and low radiation dose relative to CT, which is ~40-70 µSV per procedure. On new CT scans the dose is up to 4000 µSV, on old ones up to 20,000 µSV. The difference is obvious.
- in the low cost of the procedure relative to CT. Tomosynthesis is comparable in price to a fluorograph apparatus. The problem is that the devices are not widespread throughout the Russian Federation, and not everyone will be able to find it in their city.