Diagnosis of lung cancer using FLG
Lung cancer is detected by fluorography images only in some cases.
- Significant size of formations. The images clearly localize the problem area, which usually indicates the last stages of the presence of cancer or the aggravated condition of the patient’s body.
- Location of cancer formation on the surface.
Important! Detecting lung cancer in the early stages is not an easy task, due to the almost complete absence of symptoms. At the initial stage, the disease manifests itself only by the germination of oncological formations of the bronchi, pleura, and blood vessels (or the tumor, due to its growth, begins to compress the tissues surrounding it)
Therefore, the patient does not seek medical help until a clinical picture begins to emerge.
At the initial stage, the disease manifests itself only by the germination of oncological formations of the bronchi, pleura, and blood vessels (or the tumor, due to its growth, begins to compress the tissues surrounding it). Therefore, the patient does not seek medical help until a clinical picture begins to emerge.
Features of detecting tuberculosis using FLG
In fluorography images, pulmonary tuberculosis lesions appear as darkening and compaction with a clearly defined pattern
The doctor pays attention not only to their size and quantity, but also to the characteristic contour of the shadows. Depending on the degree and type of disease, the picture shows:
Photo 2. Photo of pulmonary tuberculosis on fluorography. Foci of infection are located in both lobes.
- Many small darkened lesions with clear contours and a diameter of up to 2 mm, located throughout the entire area of the lung in large quantities. These signs define disseminated tuberculosis.
- Focal tuberculosis. It is determined if the dark spots have a round or oval (less often) shape, with one or more dark areas, 1-2 cm in diameter. The intensity in this case is low, the lesions in the image may merge.
- Infiltrative tuberculosis. It is distinguished by focal darkening of a widespread nature, with the same consistency of formations and uneven edges.
- Caseous pneumonia. This is the most severe form of tuberculosis. It is classified by extensive darkening of a large part of the lung, and sometimes its entire part. At an early stage, it has a homogeneous structure, which changes to a stronger darkening with emerging foci of clearing.
- Cavernous tuberculosis. A decay cavity is defined when there is a visible gap in the center of the darkening.
- Lung cancer and tuberculosis; they can be detected using fluorography if the lung tissue is changed. However, such a diagnosis in any case requires laboratory confirmation using tests.
How does pneumonia differ from tuberculosis in fluorography images?
In medicine, there is a golden rule, known at the beginning of the last century, that distinguishes tuberculosis from pneumonia.
- Ascultative findings in tuberculosis are mild in nature, combined with extensive pulmonary damage, which is visible on X-ray diagnostics.
- Radiologically, pneumonia is a unilateral process that is characterized in certain segments of the lung. The changes are infiltrative in nature.
- Tuberculosis is a bilateral process; it is often localized in the right lobe of the lung. In the image, the lesions are clearly expressed (unlike pneumonia), with visible foci of dissemination and destruction.
Treatment
To diagnose tuberculosis, in addition to a visual examination and history taking, radiography and a tuberculin test, as well as bacteriological culture of sputum, are performed. An antibiotic is initially prescribed for a course of 10 days. and conduct a re-examination. If the results do not change, then tuberculosis is diagnosed.
Medication method
Since the nature of the disease is bacterial, the main method of treatment is antibiotic therapy, which is carried out, depending on the severity of the disease, for 6 months. up to 2 years. Several common drug regimens are used:
- Three-component. With this technique, 3 drugs that have activity against mycobacteria are used simultaneously. The oldest and most proven scheme, but today it is almost never used;
- Quadruple. By the end of the 20th century, the Dutch scientist Karel Stiblo developed a 4-component scheme that made it possible to treat the disease with greater efficiency, since new resistant strains of mycobacteria had appeared;
- Five-component. It is used in many treatment centers and consists of adding fluoroquinolone derivatives to the previous regimen. This scheme is even more effective, but is the most expensive and has a number of side effects.
In addition to antibiotics and anti-tuberculosis drugs, immunomodulators, glucocorticoids, vitamin complexes, non-steroidal anti-inflammatory drugs, and hepatoprotectors are used in complex treatment. Enhanced nutrition is of particular importance - the body requires additional resources to absorb medications and neutralize toxins.
ethnoscience
There are many recipes recommended for the treatment of tuberculosis. However, you should not rely only on them - mycobacteria are very resistant to any influence and often continue to destroy the body even when treated with medications. Therefore, it is better to use traditional remedies as a supplement:
- Mix 1 tbsp in a glass container. l. pine pollen with 150 g of linden honey. Take for 2 months. 1 dec. l. 3 r. a day before meals;
- 30-40 g of dried mole crickets are ground in a mortar and mixed with honey or chilled porridge. Take 2-3 tbsp. l. shortly before meals 3 p. in a day;
- Pour 1 tbsp into a thermos. l. chopped chicory root and motherwort herb, pour 400 ml of boiling water and leave overnight. The strained broth is drunk over the next day, and a new one is prepared in the evening;
- Take 2 tbsp. l. seal fat before meals 3 r. per day, and also cook food on it. The course of treatment is 3 months. Seal oil can be replaced with badger oil;
- Boil oatmeal jelly for an hour. Use bran or oats. The broth is filtered and brought to the required thickness. Drink instead of a drink, maybe with honey;
- 5-7 clean iron nails are inserted into an apple for a day. Afterwards the nails are pulled out and the apple is eaten. The goal of treatment is to saturate the body with iron;
- Insist 1 tbsp. l. birch buds in 400 g of vodka in a cool, dark place. When the tincture takes on the color of cognac, take 1 tbsp. l. 3 r. a day before meals;
- Dried leaves (feathers) of garlic are ground into powder and taken 3 rubles on the tip of a knife. a day before meals. The course of treatment is 30 days. , break – 14 days. , after which the treatment is repeated.
Fibrous-cavernous form
Is evidence of a chronic tuberculosis process. Deformation of the tissue of the lung and upper respiratory tract (trachea, bronchi) occurs. This course of the disease is characterized by alternating exacerbations (with cough, hemoptysis, shortness of breath) and remission, when nothing bothers the patient.
The description of images of tuberculosis in the fibrous-cavernous form has the following features:
- a cavity with a thicker and more pronounced wall than in cavernous tuberculosis;
- displacement of the trachea towards the formation of a cavity;
- deformation of the pulmonary pattern;
- placement of cavities in the upper sections.
Nuances of diagnostics
The effectiveness of the procedure depends on compliance with all the rules for conducting the study, as well as the correct interpretation of the results.
Fluorography consists of the following stages:
- To begin with, a person must expose his torso. All jewelry must be removed, and hair must be secured with an elastic band or hairpin.
- A lead apron is hung on the belt. This is done to minimize the impact of radioactive rays.
- The doctor adjusts the screen according to the patient's height. He, in turn, presses his chest tightly against him with his shoulders brought forward.
- Do not breathe or move while the device is operating. The specialist warns when to freeze, after which the person returns to his usual rhythm.
- Next, the patient gets dressed. The diagnostic result is obtained by the doctor in a few minutes or days, depending on the device. Based on it, a conclusion is drawn describing the state of the respiratory system.
Following the technique of the procedure makes it possible to obtain the most accurate result. Otherwise, you can observe image distortion and a blurry picture, which requires repeating digital fluorography. This fact is undesirable, since large doses of radiation are dangerous to human health.
If the patient has concomitant diseases or disabilities, the procedure becomes more difficult. It all depends on the individual characteristics of the body and the health of the person being examined. In cases where the patient constantly coughs and cannot stabilize the chest, the effectiveness of the procedure is sharply reduced.
Types of X-ray examinations
Digital X-ray
During the research process, the result is displayed on a computer; the main advantages of the method are:
- minor radiation exposure;
- accuracy;
- approved for use in children;
- low level of spoiled photos;
- low price achieved due to the absence of consumables;
- thanks to special programs you can get an accurate image;
- maintaining information in an accessible form;
- You can print the photo on regular photo paper;
- the ability to calculate the radiation dose received in a certain period of time.
The method has a number of disadvantages:
- worse than film radiography in resolution;
- in many countries, at the legislative level, it is not customary to consider a digital medium a legal document;
- it can only be used to diagnose pulmonary tuberculosis. It is impossible to control the benefits of the therapy used using the method.
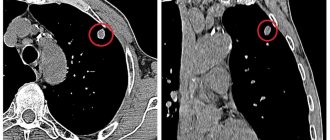
CT scan
The advantages of this lung examination for tuberculosis:
- highest accuracy, information content and resolution;
- three-dimensional image;
- speed of implementation;
- allows you to assess the condition of nerves, soft tissues, lymph nodes, bones, blood vessels, lungs;
- allows the use of a contrast agent;
- allows you to determine the presence of complications and the location of changes;
- widely used when examining children when other methods do not work due to the child’s age;
- allows for differential diagnosis;
- ease of evaluating results;
- ease of data transfer and storage.
Disadvantages of the method:
- Expensive;
- difficulties in carrying out research for people with claustrophobia or mental illness;
- children at an early age are diagnosed only under anesthesia;
- high radiation exposure.
Digital X-ray and computed tomography are effective research methods.
Often prescribed as an additional diagnosis when tuberculosis is suspected.
How often can you do it, and are there any mistakes?
Modern FLG devices have high resolution and are quite compact. They are located in specially equipped stationary rooms or in mobile laboratories (based on vehicles). The latter are used to implement anti-tuberculosis preventive raids so that all employees of the organization, residents of an entire locality, or generally everyone can undergo examination.
There are two types of fluorography:
digital – a more modern look. With this method, there is significantly less radiation exposure to the subject, since more modern equipment is used. The radiation dose per session is 0.03 millisieverts. In addition, the quality of the signal and image, despite the reduced picture area, is high;
film - traditional look. With it, the subject receives a dose of radiation almost fifteen times greater - 0.5 millisieverts
This figure does not exceed the permitted values, but when prescribing the procedure, it is important to take into account contraindications
Recording the results of the study on a digital medium is a huge advantage; this makes it possible to show the image to several doctors even remotely, and there will be no need to go through the procedure again.
In the absence of corresponding symptoms, experts advise adults to undergo such an examination no more than once a year. The certificate obtained as a result of the study is valid for twelve months.
It is possible to detect tuberculosis using fluorography with almost one hundred percent accuracy. However, medical errors, the so-called “human factor,” should not be completely ruled out.
In addition, there have been cases where the images do not show tuberculosis, but there are symptoms characteristic of this disease.
Alarming signs of this disease are difficulty breathing and shortness of breath. If such symptoms appear, you must immediately seek medical help from a doctor who will prescribe appropriate examinations.
You should be wary of those manifestations of the disease that cause less discomfort, but are important when making a diagnosis. This is a sudden loss of weight and appetite, a slightly elevated temperature, and a cough with phlegm that lasts more than three weeks.
In later stages, there is a cough that coughs up blood.
There are also contraindications to performing FLG even if tuberculosis is suspected. These are the cases:
- pregnancy;
- oncology;
- radiation sickness;
- inability to assume a vertical position;
- presence of chest pain and severe cough.
The procedure is not recommended for children under fifteen years of age. Prescribing this form of examination to children is determined only by the impossibility of establishing a diagnosis by other means. Monitoring of the incidence of tuberculosis among minors in the Russian Federation is carried out using the annual Mantoux test.
If this procedure is prohibited, tests are prescribed: sputum, urine, blood.
In any case, it is more reliable to undergo additional tests, since the question of whether fluorography always detects the disease remains open. Incorrect results of the procedure may result in equipment failure.
Description, varieties, advantages of the technique
The essence of the fluoroscopy procedure is as follows: a person needs to remove all outer clothing, press tightly against a special glass, take a deep breath, hold his breath and exhale. During the period of holding your breath, the physician leaves the room where the device is located and takes a picture.
Today there are two types of diagnostics – film and digital. The second method is considered more accurate; it immediately shows whether there is fluid or abnormal changes in the organ.
This diagnostic technique is popular and in demand, among its advantages: a high level of accessibility, a minimum radiation dose during the process, and the ability to choose the type of procedure. But the main advantage is complete safety for health and life.
Fluorographic examination is available to city residents and people living in remote villages - they do not need to go to the city for examination; a car with a mobile device comes to the countryside.
The purpose of the analysis is the prevention of respiratory diseases transmitted by airborne droplets and contact.
What is it for?
When conducting a comprehensive examination of the patient, many specialists conclude that fluorography needs to be done. The operating principle of this technique is based on the ability of X-rays to penetrate tissue structures, which allows one to visualize the condition of the body.
The first mentions of the use of this technology appeared at the end of the 19th century, when scientists were looking for a more gentle alternative to the classic options for radiographic examination. Due to its high accuracy and accessibility, it was actively used for diagnosing organs of the respiratory system in order to determine all kinds of pathologies. Among them:
- Inflammatory processes.
- Oncological diseases.
- Infectious pathologies.
There are other problems that require fluorography. Thus, modern specialists prescribe it for intractable or chronic colds. The key object of examination is the chest area, which allows us to study the condition of the lungs, heart, mammary glands and bones. The technique is effective in the early stages of dangerous pathologies that have mild symptoms. These include:
- Tuberculosis.
- Pneumonia.
- Malignant formations.
As a preventive measure, fluorography of the lungs is performed for the following groups of people:
- Citizens who are over 16 years old. The optimal frequency of diagnostics is at least once every 2 years. If a person works in a hazardous enterprise and receives a high dose of radiation exposure, he is prescribed fluorography once a year.
- Patients of medical centers who came for an initial examination.
- Citizens living with a pregnant woman or newborn child.
- Diagnosed with HIV.
An unscheduled study of the lung is necessary if there are symptoms of the following pathologies and diseases:
- Various forms of pneumonia, pleurisy and inflammation in the lungs and other organs of the respiratory system.
- Tumor formations.
- Tuberculosis.
- Lung diseases.
In this X-ray examination, rays pass through the human body. An image of 256 shades of black and white appears on the screen, which reflect the condition of the chest and nearby organs.
Understanding the importance of fluorographic examination, you need to pay attention to the following features and advantages:
- Availability. Every medical facility has equipment for chest X-ray examination. To quickly detect lung cancer, bronchitis, tuberculosis and other dangerous pathologies, powerful installations are used that ensure high accuracy of the examination. On-site diagnostics are also practiced, which allows us to reach a larger number of people.
- High execution speed. The average duration of a lung study session for tuberculosis, bronchitis and other diseases is no more than 5-7 minutes. During this time, the doctor sets up the equipment and records the results. To make an accurate diagnosis, the patient needs to undress to the waist and stand in front of the matrix. The remaining actions are corrected by a specialist. After a couple of seconds, a picture of the lungs appears on the screen.
- Painless. Since the procedure is non-invasive, the patient does not feel pain or discomfort during it. This allows you to see any pathologies without negative effects on the skin.
- Information content. The technique provides accurate results and qualitatively displays the inflammatory focus.
Contraindications
Checking the respiratory system through fluorographic diagnostics is safe and harmless. This technique does not harm the human body, since the radiation dose remains minimal. In this case, the radiation quickly leaves the body, leaving no traces.
Under high loads, the likelihood of developing pathological processes at the cellular level, which are fraught with cancer, increases.
The use of this diagnostic technique is contraindicated for:
- Children under 15 years of age. To identify fibrosis of lung tissue or other manifestations of tuberculosis, it is enough to evaluate the body’s reaction to the Mantoux vaccination.
- Pregnant women and breastfeeding women.
- Bedridden patients who are unable to hold the body in an upright position.
- Patients with respiratory failure.
If there are such contraindications, other examination options are used, and pregnant women are allowed to undergo fluorography only after the birth of the child.
Definition of disease
This is the name of the tuberculosis type of intoxication. It is diagnosed mainly in children of school and preschool age, as well as adolescents.
This type of tuberculosis includes complex primary tuberculosis lesion. It includes the site where the infecting bacteria enters the body or the site of the disease and the lesions on the lymph nodes inside the chest.
In turn, pulmonary tuberculosis, according to the degree of spread and severity of the course, can be:
- Miliary. It is a dangerous form of tuberculosis, in which the formation of tuberculous tubercles is observed in various organs and tissues. Also characteristic is the absence of a pronounced lymphogenous period.
- Disseminated. A clinical type of tuberculosis, accompanied by the formation of many focal inflammations in the lungs due to hematogenous transport of the bacterium.
- Focal. A form of tuberculosis, which is characterized by a limited spread of infection, mainly in the lungs.
- Infiltrative. It is characterized by the formation of exudative-pneumatic formations with caseous destruction in the middle.
- Cavernous. Tuberculosis, accompanied by the formation of cavities.
- Fibrosis-cavernous. It is characterized by the formation of light cavities in the cavity, which are equipped with dense walls of fibrosis.
- Cirrhotic. This type of tuberculosis is the final stage of pathology development and is characterized by a large amount of pneumocirrhosis, which predominates over specific damage to lung tissue.
It is customary to highlight separately:
- tuberculoma;
- caseous type pneumonia;
- tuberculous inflammation of the pleura;
- pleural empyema;
- sarcoidosis
The following lesions are distinguished as non-pulmonary forms of tuberculosis:
- brain in the spinal column;
- meninges;
- gastrointestinal organs;
- lymph nodes;
- articular elements and bones;
- organs of the reproductive system;
- urinary system;
- skin.
Tuberculosis is an infectious disease caused by mycobacteria and characterized by specific changes in the lungs. These lesions are caused by chronic inflammation, in which irreversible changes occur in the tissues that impair ventilation of the lungs.
When a pathogen enters the body, it is subjected to a massive attack by cells of the immune system. If the immune system is strong, then the bacteria are safely destroyed without any signs of illness.
However, in the case when, for certain reasons, a person’s defenses have a small margin of safety, the pathogen first penetrates into the tissues of the lungs, entering the blood from there. Thus, the digestive organs, bones and joints, genitourinary and nervous systems, skin, and eyes can be infected.
The causative agent of the pathology is the tuberculosis bacillus. A distinctive feature of the bacterium is its shell, which protects the microbe from changing environmental conditions and the effects of medications.
The tuberculosis bacillus develops very slowly, so diagnosing the disease can be difficult. Microorganisms are usually transmitted through the air: when a patient coughs, sneezes or talks. When drops containing components of the tuberculosis bacillus dry, even smaller particles are formed that remain in the air for a long time and do not settle down under gravity. From the air, the pathogen penetrates the mucous membranes of the human nasopharynx and into the respiratory tract.
Tuberculosis actively develops in people suffering from infectious and chronic pathologies:
- HIV;
- renal failure;
- diabetes mellitus;
- oncological diseases.
The risk category for tuberculosis infection includes children under 5 years of age, people living in poor living conditions, and the elderly.
Diagnosis of tuberculosis using this method
Today there is an opinion that tuberculosis is a disease of people who have low social status. Unfortunately, this is just a stereotype. Anyone can become infected with tuberculosis, regardless of their social status.
Tuberculosis is a disease that is transmitted by airborne droplets. It was discovered back in the eighties of the nineteenth century. The causative agent of the disease is Koch's bacillus. It is dangerous because it has a very high threshold of resistance to external environmental factors.
The tuberculosis bacillus can persist for a long period on food, furniture or dust. It should be remembered that tuberculosis poses a threat to all people on the planet. It can be contracted in any area by simply inhaling dust or particles of saliva from a sick person.
The fluorography method can show the disease in the early stages. This facilitates quick and effective treatment, reduces the risk of infecting others and developing an epidemic. X-ray diagnostics are performed without preliminary examination of the person. Regular chest examinations significantly reduce the risk of disease.
If a person goes to the hospital, he is required to undergo fluorography - today, X-ray diagnostics are simply irreplaceable in identifying a disease such as tuberculosis. If a person has any violations, the device will immediately detect them. It has a high throughput and quickly transmits data on the condition of the chest organs. This data is displayed on the screen, which is viewed by a specialist. Also, using the image, you can establish a final diagnosis.
Forms of tuberculosis in photographs
There are several types of tuberculosis in photographs:
- focal pulmonary tuberculosis - in the picture this disease appears as small spots in the form of lesions. Their localization is in the upper part of the lung and under the collarbone. Chagas can spread over the entire surface of the organ. Without proper treatment, the disease leads to fibromatosis;
- infiltrative pulmonary tuberculosis – relapse, which was the result of focal tuberculosis. It is complicated by the fact that it leads to tissue death and elimination through coughing and sputum. Sputum contains bacteria that can infect other people. Infiltrative tuberculosis has an open form and appears on photographs as dark spots of uncertain configuration;
- fibrous-cavernous chronic tuberculosis - with this form, dark spots will be visible that cover the entire surface of the lungs. The disease progresses to a stage when fibrosis and bleeding begin to develop. It also affects the larynx and intestines.
If X-ray diagnosis occurs in the later stages, then the disease is often accompanied by complications:
- tuberculosis of the larynx;
- intestinal tuberculosis;
- tuberculosis of the genitourinary system.
All complications are quite severe and can be seen very clearly in the photographs. Timely treatment can prevent the development of these diseases.
Decoding the results
The result obtained during the chest examination must be deciphered. There are special tables that set standards for each disease. Experienced specialists know that the image of diseased lungs has a non-uniform color. Some organs do not absorb X-rays well, so there may be dark areas in the image.
After the X-ray diagnostic procedure, the doctor must give a description.
First of all, tuberculosis on fluorography manifests itself in:
- different intensity of the image in the image;
- increasing the size of blood vessels;
- various spots and lesions;
- shadows;
- sealed sinus.
Description of the image may take several days. It all depends on the qualifications of the doctor and the quality of the equipment.
There are several reasons why lung fluorography should not be done. It is contraindicated:
- people with radiation sickness;
- patients with cancer;
- children under 15 years old.
It allows you to quickly and accurately identify all the problems that arise with the chest organs.
https://youtube.com/watch?v=933X_E9oi-s
Risk of errors
During a fluorographic examination of the human chest organs, there is always a risk of misdiagnosis of tuberculosis. This is influenced by several different factors, among which it is worth highlighting the following:
- malfunction of the hospital's technical equipment;
- the presence of rare pathological processes in the lungs;
- low doctor competence;
- non-compliance with diagnostic techniques.
In order to be 100 percent confident in the examination results, it is additionally worthwhile to undergo other diagnostic methods.
General information about the disease and the specifics of the procedure
Despite unlimited access to information, society still believes in erroneous stereotypes. One of them is associated with tuberculosis. Some still believe that it is a disease that only affects those of lower social status. This is wrong. The infection is not selective to the wealth of the person into whose body it enters.
Any person has a risk of contracting tuberculosis; it is transmitted through airborne droplets, during normal household contact from a carrier to a healthy person.
However, there are people who are more at risk of getting sick:
- elderly;
- military;
- prisoners;
- persons without a fixed place of residence;
- persons with unhealthy habits;
- those with serious immune problems.
The causative agent of tuberculosis is Mycobacterium Koch bacillus. It was identified back in the eighties of the century before last. The danger of infection is that it is extremely resistant to environmental conditions. The microorganism can remain alive for a long time on food, furnishings, even on dust particles. Tuberculosis can be contracted simply by inhaling dust containing saliva from an infected person.
The lack of necessary treatment leads to death, since mycobacteria gradually fill the entire space of the respiratory tract, destroy them, and the patient suffocates.
Fluorography is a method of x-ray examination of the lungs and chest organs. Allows you to identify hidden pathologies in this area. It is the main form of preventive tuberculosis diagnosis (it detects even initial specific changes) and an alternative to radiography. It is usually prescribed instead of repeated x-rays. Early detection of tuberculosis allows you to prescribe timely treatment, increases its effectiveness, protects others from infection and prevents an epidemic.
Fluorography is a mandatory examination. When a patient goes to a clinic (no matter what specialist he is referred to), he must do a “flux test”.
This type of radiographic examination was discovered by American and Italian scientists in the late nineteenth and early twentieth centuries. But the method became more widely used in Brazil, several years before the outbreak of World War II.
The whole procedure boils down to the following simple steps.
- The subject takes off all items of clothing and jewelry and remains naked to the waist.
- Then the patient walks to the device, stands facing the screen, and presses his shoulders and chest against it as tightly as possible.
- After this, the doctor gives the command “Don’t breathe,” and the patient holds his breath for a few seconds. This is necessary so that at the time the picture is taken, breathing movements do not “blur” the picture.
Usually the procedure does not take much time. If the patient is being tested with limited mobility, special accommodations will likely be required. For children, restraint straps are used, or the parent must hold the child and his arms in an elevated position.
Symptoms of tuberculosis
Pulmonary tuberculosis can occur in any person without exception. It appears due to infection with Koch's bacillus. A distinctive feature of this pathogen is that it can remain in the open air for a long time, being resistant to environmental influences.
Before doing chest fluorography, a person needs to know what symptoms may indicate infection with Koch's bacillus. First of all, you should pay attention to such possible signs of the disease as:
- Dyspnea. Most often with tuberculosis it occurs even with minor physical exertion.
- Cough. If it occurs continuously over a long period of time, you should definitely visit a medical facility.
- Wheezing. They are a sign of the presence of an infiltrate in the lungs or any other pathological changes in the structure.
We recommend reading! Follow the link: X-ray examination method
It is also necessary to pay attention to the occurrence of low-grade fever in the range of 37-37.3 degrees Celsius. If you have several of the above symptoms, you should definitely make an appointment with a pulmonologist or TB specialist.
Detection of tuberculosis in an image
Using fluorography, the doctor can determine the presence of damage by Mycobacterium tuberculosis, as well as assess the characteristics of the course of the disease.
The study makes it possible to identify the following forms of the disease:
- Focal tuberculosis. It has a local character. Darkening is observed in the upper part of the lung. The size of the lesions often does not exceed 2 cm. The main complication of this form of the disease is fibromatosis, which affects the entire organ.
- Recurrent infiltrates. In most cases, they form against the background of focal forms of pathology. Advanced cases are fraught with necrosis of lung tissue, as well as hemoptysis. The image shows shadows with unclear contours, round or oval in shape, the size of which ranges from 2 to 4 cm. This is a dangerous type of disease for the health of the patient and the people around him, since the risk of infection is very high.
- Chronic form. After performing the study, the resulting image shows small dark spots that are located over the entire surface of the lungs. In the presence of a closed type, lack of treatment can lead to the development of scars and bleeding, as well as the spread of bacterial agents to other organs through the vascular system.
- Disseminated type. The photo shows multiple lesions up to 2 millimeters in size, which extend to the entire lung.
In the picture, healthy tissues have smooth edges and color, while damaged tissues have darkening and irregular shape. There is also a change in the vascular apparatus of the lungs. Doctors use special tables to decipher the results. With their help, they create the most accurate picture of the pathology.
The role of fluorography in preventing the development of the disease is very great, since this mass diagnostic method is available in all territorial areas.
However, the study is not able to identify the causative agent of tuberculosis, but only demonstrates the consequences. To detect mycobacteria, doctors use sputum bacterial culture and antibody testing. Also, the examination cannot detect disease in other organs, even in the presence of pronounced clinical symptoms.
Decoding the results
Examination of the lungs using fluorography only allows one to assess the condition of the organ at a specific point in time. The data obtained as a result is not an indisputable reason to give the patient a particular diagnosis. In order to do this, several additional types of examinations must be performed.
Fluorography of the chest organs makes it possible to determine the proportion of the lungs in which pathological changes have occurred, the segmentation of the lesion, the estimated rate of development of the disease and some other aspects. In order to do this, the image obtained as a result of the procedure must be assessed and described by a radiologist.
How often can you do it
The frequency of fluorography is determined by the patient’s condition. When figuring out how many times fluorography can be done and how often the examination needs to be done, one should take into account the clinical picture and the form of the inflammatory process.
The acceptable rate is 1-2 times a year. In this case, the radiation exposure will be minimal and harmless.
More frequent sessions are necessary for the following groups of people:
- Employees of hazardous enterprises or people who are constantly in contact with patients with tuberculosis. These include TB doctors, correctional colony employees, etc.
- Patients with a number of chronic diseases that negatively affect the body's protective functions. These are diabetes mellitus, AIDS, hepatitis and other lesions.
- People serving time in prison.
If complications develop, a re-examination must be performed, but such diagnostics are often prohibited.
Indications for fluorography
This diagnostic method is used both for preventive purposes (once a year) and for certain ailments:
- determining the cause of cough, chest pain, shortness of breath;
- suspicion of pneumonia (pneumonia);
- the presence of pathology of the heart and blood vessels (atherosclerosis, aortic aneurysm, pathology of the heart valves);
- contact with a patient with tuberculosis;
- suspected HIV infection;
- search for foreign bodies in the respiratory tract and upper gastrointestinal tract.
Pulmonary tuberculosis on x-ray or fluorography: examination features
The incubation period of tuberculosis can last several years. Microbacteria of the disease can affect any tissue of the body, with the exception of nails and hair.
The most common place for their localization is the lungs. To diagnose the disease, various types of tomography, fluorography, as well as radiography in lateral and direct projections are used.
Most often, doctors detect pulmonary tuberculosis using x-rays or fluorography.
Suspicion of tuberculosis becomes a direct indication for a chest x-ray. Radiography is included in the mandatory diagnostic standards. The photo is prescribed to:
- refute or confirm the presence of the disease;
- distinguish tuberculosis from lung diseases with similar symptoms (pneumonia, abscess, silicosis);
- identify the degree of lung damage, the prevalence and localization of the process.
X-ray is necessary if the patient complains of cough, weakness, increased sweating, weight loss, shortness of breath and chest pain. Doctors are also required to refer the patient for examination if the Mantoux test (tuberculin test) is positive and it increases by more than 6 mm in relation to the previous study.
Unlike x-rays, fluorography is a preventive study. There are no direct indications for its passage. The procedure is carried out during medical examination, even if the person has been vaccinated with BCG. The main advantage of this method over x-rays is its low cost. Therefore, fluorography is widely used for routine examinations of the population.
For a specialist, the difference between x-rays and fluorography is significant. In the images obtained during a routine examination, the image is reduced, and therefore has less information for the doctor than an x-ray. Despite this feature, fluorography for tuberculosis can show all the main foci of lung damage.
Both methods are recommended to be used no more than once a year. At such doses, radiation is safe for the patient. Radiation exposure during radiography is lower than during fluorography.
Examination methods
In addition to collecting a history of the disease, the following diagnostic methods help the doctor.
Physical examination of the patient
The main method is auscultation or listening to the respiratory organs.
The development of pneumonia is indicated by:
- crepitus - characteristic creaks heard at the end of inspiration;
- difficulty breathing, moist, fine wheezing.
With tuberculosis, breathing is almost always normal - this is the so-called vesicular breathing. Moist rales may also be present, but they are subtle and not always audible.
In both cases there is a cough with sputum. But the cough with tuberculosis infection is constant, dry, and hysterical. With pneumonia, there is a change in the nature of the cough from dry to wet as the disease progresses. With pneumonia, changes occur more often in both lungs. Mycobacteria infect one lung.
During the interview, the patient may note the presence of relatives with tuberculosis, since the chance of contracting tuberculosis in close contact is higher. With pneumonia there is no such pattern.
Laboratory diagnostic methods
If any disease is suspected, laboratory tests of blood and urine are performed first. They will show:
- An increase in the rate at which red blood cells are deposited – in the case of both diseases.
- The increase in the number of leukocytes is significant in pneumonia, moderate in tuberculosis.
- An increase in lymphocytes and monocytes to a significant extent - only with tuberculosis infection.
- A decrease in hemoglobin is more common with long-term developing tuberculosis.
A tuberculin test will also be performed - Mantoux or Diaskintest. The main method for detecting tuberculosis is the Mantoux test, which allows you to determine whether there has been contact with mycobacteria. And Diaskintest will more accurately reveal their number and activity. If Diaskintest gives a positive result, then the patient is almost 100% infected with the tuberculosis bacillus.
If there is doubt about the nature of inflammation in the lungs, a sputum analysis is done. It helps to identify the pathogen. Sputum in tuberculosis will show the presence of active mycobacteria, and in pneumonia - pathogenic bacteria. To eliminate all doubts and finally confirm or refute the diagnosis, 2-3 cultures are done at short intervals.
X-ray signs of tuberculosis and pneumonia
The main method for detecting tuberculosis is fluorography. But in some cases, an x-ray of the lungs is also performed. For pneumonia, doctors prefer fluoroscopy. The image can clearly determine to what extent the lungs are affected by tuberculosis and pneumonia, and where the foci are localized. This instrumental diagnostic method is suitable not only for an adult patient, but also for children for whom fluorography is not recommended under 15 years of age.
X-ray signs:
- When pneumonia occurs, the lower part of both lungs is most often affected. Shadows indicating the presence of a focus for tuberculosis are located, as a rule, in one lung in the upper or middle segment.
- Outlines of lesions. Pneumonia is characterized by blurry shadows, the affected lungs seem to be filled with smoke in certain areas. In tuberculosis, the boundaries of the lesions are delineated; they have a clear outline on x-ray photographs.
Based on the results of all the studies, the doctor determines what the patient is sick with, what stage the disease is at, what form it is necessary to deal with, and only then selects the appropriate medications and treatment procedures.