Designations of blood test indicators
Red blood cell indices (MCV, MCH, MCHC):
- MCV is the average volume of a red blood cell in cubic micrometers (µm) or femtoliters (fl).
- MCH is the average hemoglobin content in an individual red blood cell.
- MCHC is the average hemoglobin concentration in a red blood cell.
Platelet indices (MPV, PDW, PCT):
- MPV (mean platelet volume) - average platelet volume.
- PDW is the relative width of platelet distribution across the volume.
- PCT (platelet crit) - thrombocrit.
- LYM% (LY%) (lymphocyte) - relative (%) content of lymphocytes.
- LYM# (LY#) (lymphocyte) - absolute content of lymphocytes.
- MXD% is the relative (%) content of a mixture of monocytes, basophils and eosinophils.
- MXD# is the absolute content of a mixture of monocytes, basophils and eosinophils.
- NEUT% (NE%) (neutrophils) - relative (%) content of neutrophils.
- NEUT# (NE#) (neutrophils) - absolute content of neutrophils.
- MON% (MO%) (monocyte) - relative (%) content of monocytes.
- MON# (MO#) (monocyte) - absolute content of monocytes.
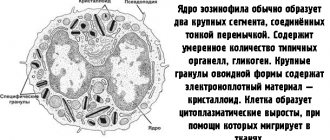
- EO% is the relative (%) content of eosinophils.
- EO# is the absolute content of eosinophils.
- BA% is the relative (%) content of basophils.
- BA# is the absolute content of basophils.
- IMM% is the relative (%) content of immature granulocytes.
- IMM# is the absolute content of immature granulocytes.
- ATL% —relative (%) content of atypical lymphocytes.
- ATL# is the absolute content of atypical lymphocytes.
- GR% - relative (%) content of granulocytes.
- GR# is the absolute content of granulocytes.
- RBC/HCT - average volume of red blood cells.
- HGB/RBC is the average hemoglobin content in a red blood cell.
- HGB/HCT is the average hemoglobin concentration in a red blood cell.
- RDW - Red cell Distribution Width - coefficient of variation of the average volume of red blood cells.
- RDW-SD - relative width of the distribution of erythrocytes by volume, standard deviation.
- RDW-CV - relative width of distribution of erythrocytes by volume, coefficient of variation.
- P-LCR —large platelet ratio.
- ESR is the erythrocyte sedimentation rate.
published 06/22/2011 20:40 updated 12/06/2015 — Clinical blood test
What are lymphocytes
Lymphocytes (lymph) are the “censorship” of our body.
Lymphocytes are responsible for the immune surveillance of our body. The body of the lymphocyte has special receptors that are activated upon contact with a foreign cellular protein.
A lymphocyte lives not a couple of days, like “typical” leukocytes, but from several months to more than 20 years.
Individual lymphocyte cells can be born and live until a person’s death!
Compared to red blood cells, they are very small 7-10 microns in diameter. The main difference between a lymphocyte and all leukocytes in the blood is that it gives them the ability to easily pass through body tissue and return back to the blood.
Normally, the percentage of lymphocytes in the blood is from 20 to 40%. There are higher numbers of lymphocytes in tissues than in blood, or vice versa. This is considered normal; some lymphocytes may differ from their “brothers” who live in different places in the body and belong to different species.
The specificity of the function of the lymphocyte included in the group of leukocytes is immune surveillance, an amazing ability to recognize in the body on the principle of “friend” and “foreign”.
It does not destroy bacteria, unlike other leukocytes, but its own diseased cells, cells modified by viruses, those that have undergone mutations, and cancer cells at an early stage.
Lymphocytes are divided into:
How are lymphocytes indicated in a blood test?
The designation of lymphocytes in a blood test varies depending on:
- quantitative content of blood elements;
- percentage compared to other bodies.
Knowing how lymphocytes are designated in blood test , it is easy to compare their quantitative and percentage indicators with reference values.
In the test results of some laboratories, the level of cells may be indicated slightly differently, which does not change the essence of the results obtained.
The quantitative indicator corresponds to the designation LY or LY “#”, and when designating the ratio, lymphocytes as a percentage of the norm look like LY% with the corresponding value.
What are the causes of mononucleosis in children?
Infectious mononucleosis develops in children at any age, but most often before 10 years of age. The child spends more time indoors, in kindergarten or at school, and there they are more likely to catch an infection or virus. Children are poorly able to produce antibody cells that can fight infections and viruses, so in childhood they are more likely to catch infectious mononucleosis. This disease develops in human saliva and is transmitted in the following ways:
- when kissing, since saliva is transmitted to a person, and with it the bacteria of mononucleosis,
- When sneezing and coughing, bacteria spread, especially in closed spaces where there are many people and children,
- when using shared utensils and hygiene products (towel, soap, toothbrush).
Experts have noticed that boys suffer from this infectious disease much more often in childhood than girls.
Mononucleosis affects the body in the autumn-winter period and spring, as weather conditions change and bacteria multiply more actively.
People affected by mononucleosis may not initially feel symptoms, but they carry the virus and pose a danger to others. The virus enters the body through saliva or the respiratory tract, the incubation period lasts 5-15 days, or maybe more, depending on the body and immune system.
Norm of lymphocytes
The norm of lymphocytes in children and adults is different.
The main difference is that in the latter the lymphocyte count does not fluctuate, but remains stable, unlike infants and young children.
In any teenager and adult, the number of these cells in a general blood test is 20-40%.
This corresponds to 1-3 thousand cells in 1 microliter of blood (if we evaluate the indicator not as a percentage, but as an absolute number).
However, accurate quantitative counts are rarely carried out, so the generally known norm of lymphocytes is the 20-40% indicated above. Deviations within 4-5% up or down are not considered pathology.
Number of individual lymphocyte subpopulations:
As you know, lymphocytes are divided into three main types:
T cells, B cells and NK cells. Their content in the blood is not the same.
There are the most T-lymphocytes, about 70-80% of all lymphocytes.
There are much fewer B cells, only 7-20%.
Finally, NK cells are usually the fewest in number, ranging from 5 to 20%.
Table of lymphocyte norms by age in adults and children.
Functions in the body
Lymphocytes protect the body from pathogenic microflora. They are responsible for humoral and cellular immunity. Lymphocyte elements create antibodies to destroy foreign cells. Immune system cells are produced by the bone marrow.
In the blood of an adult, lymphocytes make up 35% of all leukocytes, in children - 50%. Their number prevails over other blood cells and can reach 1500 per 1 μl.
There are three types of lymphocytes based on their functions:
- NK cells in the form of granules – destroy virus-infected and tumor cells;
- B cells – form special antibodies that kill dangerous cells;
- T cells consist of suppressor T cells, helper T cells, and killer T cells. T-killers are responsible for normalizing immunity, T-helpers help produce antibodies, and T-suppressors inhibit this process.
Lymphocytes can change their shape, different from the established norm, as a result of exposure to pathogenic microflora or a negative reaction associated with allergies to medications. The changed lymphocytes are called atypical.
Atypical lymphocytes
Atypical lymphocytes: what are they and why do they appear?
Atypical lymphocytes can occur in some diseases. Many people believe that their appearance indicates the presence of cancer, but this is not the case.
Such lymphocytes indicate the presence of an allergy or infection.
Lymphocytes are a type of white blood cell that are responsible for protecting organs from pathogenic microorganisms. They help destroy and remove bacteria from the body. Under the influence of some of them, lymphocytes change their properties and size. This condition is not normal and requires additional research to determine the cause of the problem and eliminate it.
Atypical lymphocytes that appear under the influence of antigens acquire the following characteristic features:
- Their size changes. In their normal state, the largest leukocytes, macrophages, reach a size of no more than twelve micrometers. Lymphocytes are very rarely large, but under the influence of viruses they can grow up to thirty micrometers. This is what atypical leukocytes are.
- In normal condition, the lymphocyte is round in shape. When the structure of cells changes, they can become polygonal with jagged edges.
- The nuclei of lymphocytes also undergo changes. In a blood test, you can find that in an atypical leukocyte the nucleus is elongated and covered with clefts, whereas in the normal state it has a round shape, elongated only slightly.
- The color of leukocytes also changes. Thus, the blood test procedure includes determining the color of blood cells. To do this, hematoxylin and eosin are added to the biomaterial taken from the patient. These are standard dyes. During this procedure, you can see that reactive or atypical white blood cells are brighter in color than normal ones. They take on a dark gray or blue color with a purple core.
Value of the study
The main indicators that the doctor pays attention to when deciphering a general blood test are hemoglobin and red blood cells, ESR, leukocytes and leukocyte formula. The rest are more likely to be auxiliary.
Most often, a general blood test is prescribed to understand whether there is inflammation and signs of infection in the body, and if so, of what origin - viral, bacterial or other.
Also, a general blood test can help determine anemia - anemia. And if there are signs of it in the blood, additional tests are prescribed to establish the causes.
A general blood test is also prescribed if there is a suspicion of an oncological process, when there are a number of warning symptoms and clues are needed. In this case, the blood can indirectly tell you in which direction to move next.
Other indications are usually even rarer.
Abbreviation
Nowadays, English is mostly used on test result forms. abbreviations. Let's go through the main indicators and figure out what they mean.
The leukocyte formula is a separate block
This is more detailed information about the same WBC from the previous block.
White blood cells are very different. All of them are generally responsible for immunity, but each individual species is responsible for different directions in the immune system: for the fight against bacteria, viruses, parasites, and nonspecific foreign particles. Therefore, the doctor always looks first at the total leukocyte count from the list above, and then at the leukocyte formula to understand which part of the immune system is impaired.
Please note that these indicators usually come in two dimensions: absolute (abs.) and relative (%).
Absolute ones show how many cells are in the field of view, and relative ones show how many of these cells make up the total number of leukocytes. This may turn out to be an important detail - for example, in absolute numbers, lymphocytes seem to be within normal limits, but against the background of a general decrease in all leukocytes, their relative number is much higher than normal. So, leukocyte formula.
What are the symptoms of mononucleosis?
If a child had to come into contact with a patient with mononucleosis, then parents need to pay attention to the symptoms and well-being of the baby.
If signs do not appear and do not bother you, this means that the child is not infected or the immune system has overcome the infectious disease.
Mononucleosis can be identified by the presence of the following symptoms:
- fever and increase in body temperature up to 38°C, which is due to the fact that lymphocytes increase and the blood circulation process occurs much faster,
- drowsiness, sweating and weakness, which bothers you during the incubation period and the development of the disease,
- headache, nausea and sore throat, which are intense when swallowing food or when the vocal cords are strained.
If symptoms are not treated in time, the disease will progress and the following signs will appear:
- severe sore throat and the development of sore throat, which can develop into a purulent form,
- enlargement of the liver and kidneys, since due to the increased level of lymphocytes there is a greater load on these organs,
- swollen lymph nodes and the appearance of a rash that spreads throughout the body.
Decoding
Now let's go through each of these indicators and figure out what they mean.
HGB - hemoglobin - Hemoglobin
Hemoglobin is a protein that carries oxygen throughout the body and delivers it to the necessary tissues. If there is not enough of it, the cells begin to starve and a whole chain of symptoms develops: weakness, fatigue, dizziness, hair loss and brittle nails, snags in the corners of the lips and others. These are symptoms of anemia.
The hemoglobin molecule contains iron, and vitamin B12 and folic acid also play an important role in its formation. If there are not enough of them, hemoglobin synthesis is disrupted in the body and anemia develops.
There are also hereditary forms of anemia, but they occur much less frequently and deserve separate analysis.
Normal hemoglobin is 120-160 g/l for women and 130-170 g/l for men. You need to understand that in each specific case the standards depend on the laboratory. Therefore, you need to look at the reference values of the laboratory in which you took the test.
Elevated hemoglobin numbers most often occur due to blood thickening, if a person sweats excessively during the heat, or takes diuretics. Climbers and people who often go to the mountains may have even higher hemoglobin - this is a compensatory reaction to a lack of oxygen. Hemoglobin can also increase due to diseases of the respiratory system - when the lungs work poorly and the body constantly lacks oxygen. Each specific case needs to be examined separately.
A decrease in hemoglobin is a sign of anemia. The next step is to figure out which one.
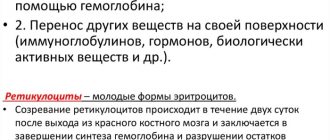
RBC - red blood cells - Erythrocytes
Erythrocytes are red blood cells that transport hemoglobin and are responsible for the metabolic processes of tissues and organs. It is hemoglobin, or rather its iron, that colors these cells red.
Standards for men are 4.2-5.6*10*9/liter. For women - 4-5*10*9/liter. Which again depends on the laboratory.
Red blood cells can increase due to fluid loss through sweat, vomiting, and diarrhea when the blood thickens. There is also a condition called erythremia, a rare bone marrow disorder where too many red blood cells are produced.
A decrease in levels is usually a sign of anemia, more often iron deficiency, less often another.
MCV - mean corpuscular volume - Average volume of red blood cells
The norm is 80-95 for men and 80-100 for women.
The volume of red blood cells decreases in iron deficiency anemia. And it increases with B12 deficiency, with hepatitis, and decreased thyroid function.
MCH - mean concentration hemoglobin - Average hemoglobin content in a red blood cell
This indicator rarely increases, but a decrease is a sign of anemia or decreased thyroid function.
Leukocyte formula
NEU - neutrophils
The largest pool of leukocytes, accounting for 50 to 75% of the entire leukocyte population. This is the main link of cellular immunity. Neutrophils themselves are divided into band-nuclear (young forms) and segmented (mature). An increase in the level of neutrophils due to young forms is called a shift in the leukocyte formula to the left and is characteristic of an acute bacterial infection. A decrease may be a sign of a viral infection, and a significant decrease may be a sign of blood disease.
LYM - lymphocytes
The second pool of leukocytes after neutrophils. It is generally accepted that during an acute bacterial infection the number of lymphocytes decreases, and during a viral infection and after it it increases.
A significant decrease in lymphocytes can be observed with HIV infection, leukemia, and immunodeficiency. But this happens extremely rarely and is usually accompanied by severe symptoms.
EOS - eosinophils
Rare representatives of leukocytes. An increase in their number occurs during allergic reactions, including drug allergies, and is also a characteristic sign of helminthic infestation.
BAS - basophils
WITH
the smallest population of leukocytes. Their increase may indicate allergies, parasitic diseases, chronic infections, inflammatory and oncological diseases. Sometimes a temporary increase in basophils cannot be explained.
MON - monocytes
The largest representatives of leukocytes. These are macrophages that eat bacteria. An increase in values most often indicates the presence of an infection - bacterial, viral, fungal, protozoal. And also about the recovery period after them and about specific infections - syphilis, tuberculosis. In addition, it may be a sign of systemic diseases - rheumatoid arthritis and others.
gra blood test transcript
Decoding should be carried out by a doctor and only a doctor. Since the number of granulocytes can be affected by many factors, from a simple cold to taking certain medications. They can calculate not according to the norm table, but according to a certain formula. Only a doctor can determine the normal granulocyte count.
Blood test, gra increased
If the analysis showed an increased number of granulocytes, this is rather an alarm bell, notifying that an inflammatory process has begun in the body or a disease has appeared. But there is no need to be particularly afraid, since the immune system has already begun to fight the viruses. Granulocytes can often increase after a recent vaccination or an allergic reaction. Other reasons could be:
- Infection
- Heart attack or stroke
- Oncological diseases
- Parasites in the body
- Inflammatory processes
- Ulcer
- Course of hormones
- Recent surgery, particularly to remove organs
If the doctor cannot determine the exact cause of the increase in granulocytes, a biochemical blood test is performed, which will show which form of granulocytes is larger, and only then, having narrowed the search, the attending physician will be able to determine the exact cause of their increase and begin the appropriate course of treatment.
ESR – erythrocyte sedimentation rate
If you draw blood into a test tube and leave it for some time, the blood cells will begin to precipitate. If after an hour we take a ruler and measure how many millimeters of red blood cells have precipitated, we will get the erythrocyte sedimentation rate.
Normally, it ranges from 0 to 15 mm per hour in men, and from 0 to 20 mm in women.
It can increase if red blood cells are burdened with something - for example, proteins that are actively involved in the immune response: in the case of inflammation, an allergic reaction, autoimmune diseases - rheumatoid arthritis, systemic lupus erythematosus and others. May increase in cases of cancer. There is also a physiological increase explained by pregnancy, menstruation or old age.
In any case, a high ESR always requires additional examination. Although it is a non-specific indicator and can speak about many things at the same time, it speaks little about anything specific.
In any case, it is almost impossible to make an accurate diagnosis using a general blood test, so this analysis is only the first step in diagnosis and some beacon to understand where to go next. Do not try to look for signs of cancer or HIV in your test - most likely they are not there. But if you notice any changes in your blood test, do not delay visiting your doctor. He will evaluate your symptoms, collect your medical history, and tell you what to do next with this test.
We noticed that in the comments there are a lot of questions about deciphering the analyzes that we do not have time to answer. In addition to making good recommendations, it is important to ask follow-up questions to find out your symptoms. We have very good therapists in our service who can help with deciphering the tests and answer any of your questions. For consultation follow the link.
LiveInternetLiveInternet
Quote from message lj_prosto_kat
Read in full In your quotation book or community!
Changes in the leukocyte formula in pathology Features of the blood system - quick response and INDIVIDUALITY!
- if you have abnormalities in your blood test, do not rush to make a will, because what you take to be a manifestation of an incurable disease may turn out to be a variant of the norm! - if the deviations are insignificant - for example, the upper limit of the norm for segmented neutrophils is 72%, and you have 77% of them - with a probability of 99% this is not a problem :) Just so you know, laboratory assistants who calculate the formula (and even more so, automatic analyzers!) are often mistaken in the count of a couple of cells, or even more. As a rule, crappy analyzers give a higher percentage of errors in formula calculations than an aunt in a white coat with a dead microscope. By the way, if a smear is suspicious, particularly suspicious (or particularly cautious) laboratory assistants usually let the doctor review it. - look carefully at the form - in our laboratory, for example, it is customary to emphasize the pronounced pathology with a red pencil 1. Neutrophils. Normally 47-72%, in children under 5-6 years old - up to 50-60% (this is not neutropenia, this is a physiological phenomenon!) a) An increase in the amount - redistributive - after heavy food, physical activity, convulsions, strong emotions, physical procedures , baths, vomiting - symptomatic - acute bacterial infections, intoxication, bleeding, hemolysis, treatment with glucocorticoids - pregnancy - leukemia - chronic myeloid leukemia, erythremia, subleukemic myelosis b) reduction in quantity - redistribution - when circulating cells leave the marginal group (starvation, hypothermia, stress, parasympathicotonia, hypertensive crisis, collapse). - true - 1) hereditary - in 2-12% of people the so-called innocent neutropenia, that is, the number of neutrophils is below normal, but the person lives, is healthy and feels great! 2) acquired - associated with a violation of the formation of neutrophils in the bone marrow when exposed to chemicals and drugs, viruses, toxins, bacteria, deficiency of vitamin B12, folic acid, iron, copper, replacement of the bone marrow with tumor cells, with agranulocytosis - associated with increased destruction of neutrophils in autoimmune diseases, consumption neutropenia in extensive inflammatory processes c) shift to the left - in a healthy person, mainly segmented neutrophils and up to 6% of band neutrophils enter the peripheral blood (in newborns, up to 10-12% of band neutrophils are allowed). The appearance of immature forms of neutrophils (rods, myelocytes, promyelocytes) is called a shift of the formula to the left (infections, acidosis, heavy physical activity, etc.) NB: if myelocytes, metamyelocytes, promyelocytes appear in the formula (TTT) against the background of complete health - immediately doctor! d) shift to the right - the appearance of neutrophils with hypersegmented nuclei, rarely - hereditary, more often with impaired DNA synthesis (megaloblastic anemia, use of cytostatics, tumors) e) degenerative changes in neutrophils - toxogenic granularity of neutrophils - in severe infections or intoxications. May occur in pregnant women! - Dele's bodies - in very severe intoxications. May occur in pregnant women! - pelgerization of nuclei - an early sign of agranulocytosis, can be hereditary (Pelger's anomaly, inherited as a dominant type, its carriers are practically healthy people, since leukocytes are functionally complete) - vacuolization of nuclei and cytoplasm - in chronic infections, intoxications - pyknosis nuclei - irradiation, leukemia 2. Eosinophils - their number depends on the concentration of glucocorticoids, therefore there are daily fluctuations - at night, when the concentration of glucocorticoids decreases, eosinophils are higher. Normally 1-5% (in children under one year old it can be up to 7%) a) increased level of eosinophils - may be hereditary - allergic reactions - helminthic infestations - malignant tumors, leukemia (especially with metastasis). Eosinophilia may be the only early manifestation of tumor growth, so its presence, after excluding other causes, requires a thorough oncological examination! - during the period of recovery from acute infections (“pink dawn of recovery” - IMHO, Schilling was a romantic:) - low-dose irradiation - collagenosis - thyrotoxicosis - hypocortisolism - skin diseases - splenectomy - gonorrhea (!) - fasting - red hair color (of course, natural, and not obtained with the help of products - during menstruation - idiopathic hypereosinophilic syndrome (a variant of chronic myeloid leukemia) With long-term eosinophilia, organs and tissues are always damaged due to the cytotoxic effect of eosinophilic granules b) decrease in the level of eosinophils - acute period of infections and intoxications - acute period of an allergic reaction - increased levels of glucocorticoids or treatment with glucocorticoids - stress, severe physical activity - ovulation 3. Basophils. Normally 0-1% (in newborns up to 4%) a) increased level of basophils - allergic reactions - malignant tumors - stress - hypothyroidism - before menstruation - during treatment with estrogens - in chronic myeloid leukemia, erythremia - acute hepatitis - splenectomy - pregnancy - after vaccinations! b) decrease in the level of basophils (rare) - see decrease in the level of eosinophils 4. Monocytes. Normally 3-11% (in newborns up to 35%) a) increase in the level of monocytes - recovery period for acute infections - chronic infections (tuberculosis, syphilis, malaria, brucellosis, chronic pyelonephritis, septic endocarditis) - paraproteinemia (myeloma, Waldenström's disease ) - malignant tumors - lymphogranulomatosis - hepatitis - collagenosis - recovery from agranulocytosis - chronic myeloid leukemia - chronic monocytic leukemia - viral infections in children, especially infants b) decrease in the level of monocytes (rarely) - acute period of infections, intoxications - high-dose irradiation - treatment with glucocorticoids 5. Lymphocytes. Normally 19-37%, in children under 5-6 years old - up to 50-70% (so do not faint when you see a child’s analysis on an adult form:) a) an increase in the level of lymphocytes - the recovery period for acute infections - chronic infections ( tuberculosis, syphilis, brucellosis) - viral infections (influenza, measles, rubella, chickenpox, viral hepatitis, etc.) - allergic reactions - chronic lymphocytic leukemia - hyperthyroidism - after vaccination! b) decrease in the level of lymphocytes - all immunodeficiencies (congenital and acquired) - lymphogranulomatosis - tuberculosis of the lymph nodes - radiation sickness - treatment with immunosuppressants - acute infections c) the appearance of wide-cytoplasmic lymphocytes (atypical mononuclear cells) - up to 5% normal, 5-15% - viral infections, >15% - infectious mononucleosis d) plasma cells - normally single, 5-10% - viral infections, long-term chronic infections, tumors, myeloma, collagenosis, after vaccination!
- if the deviations are insignificant - for example, the upper limit of the norm for segmented neutrophils is 72%, and you have 77% of them - with a probability of 99% this is not a problem :) Just so you know, laboratory assistants who calculate the formula (and even more so, automatic analyzers!) are often mistaken in the count of a couple of cells, or even more. As a rule, crappy analyzers give a higher percentage of errors in formula calculations than an aunt in a white coat with a dead microscope. By the way, if a smear is suspicious, particularly suspicious (or particularly cautious) laboratory assistants usually let the doctor review it. - look carefully at the form - in our laboratory, for example, it is customary to emphasize the pronounced pathology with a red pencil 1. Neutrophils. Normally 47-72%, in children under 5-6 years old - up to 50-60% (this is not neutropenia, this is a physiological phenomenon!) a) An increase in the amount - redistributive - after heavy food, physical activity, convulsions, strong emotions, physical procedures , baths, vomiting - symptomatic - acute bacterial infections, intoxication, bleeding, hemolysis, treatment with glucocorticoids - pregnancy - leukemia - chronic myeloid leukemia, erythremia, subleukemic myelosis b) reduction in quantity - redistribution - when circulating cells leave the marginal group (starvation, hypothermia, stress, parasympathicotonia, hypertensive crisis, collapse). - true - 1) hereditary - in 2-12% of people the so-called innocent neutropenia, that is, the number of neutrophils is below normal, but the person lives, is healthy and feels great! 2) acquired - associated with a violation of the formation of neutrophils in the bone marrow when exposed to chemicals and drugs, viruses, toxins, bacteria, deficiency of vitamin B12, folic acid, iron, copper, replacement of the bone marrow with tumor cells, with agranulocytosis - associated with increased destruction of neutrophils in autoimmune diseases, consumption neutropenia in extensive inflammatory processes c) shift to the left - in a healthy person, mainly segmented neutrophils and up to 6% of band neutrophils enter the peripheral blood (in newborns, up to 10-12% of band neutrophils are allowed). The appearance of immature forms of neutrophils (rods, myelocytes, promyelocytes) is called a shift of the formula to the left (infections, acidosis, heavy physical activity, etc.) NB: if myelocytes, metamyelocytes, promyelocytes appear in the formula (TTT) against the background of complete health - immediately doctor! d) shift to the right - the appearance of neutrophils with hypersegmented nuclei, rarely - hereditary, more often with impaired DNA synthesis (megaloblastic anemia, use of cytostatics, tumors) e) degenerative changes in neutrophils - toxogenic granularity of neutrophils - in severe infections or intoxications. May occur in pregnant women! - Dele's bodies - in very severe intoxications. May occur in pregnant women! - pelgerization of nuclei - an early sign of agranulocytosis, can be hereditary (Pelger's anomaly, inherited as a dominant type, its carriers are practically healthy people, since leukocytes are functionally complete) - vacuolization of nuclei and cytoplasm - in chronic infections, intoxications - pyknosis nuclei - irradiation, leukemia 2. Eosinophils - their number depends on the concentration of glucocorticoids, therefore there are daily fluctuations - at night, when the concentration of glucocorticoids decreases, eosinophils are higher. Normally 1-5% (in children under one year old it can be up to 7%) a) increased level of eosinophils - may be hereditary - allergic reactions - helminthic infestations - malignant tumors, leukemia (especially with metastasis). Eosinophilia may be the only early manifestation of tumor growth, so its presence, after excluding other causes, requires a thorough oncological examination! - during the period of recovery from acute infections (“pink dawn of recovery” - IMHO, Schilling was a romantic:) - low-dose irradiation - collagenosis - thyrotoxicosis - hypocortisolism - skin diseases - splenectomy - gonorrhea (!) - fasting - red hair color (of course, natural, and not obtained with the help of products - during menstruation - idiopathic hypereosinophilic syndrome (a variant of chronic myeloid leukemia) With long-term eosinophilia, organs and tissues are always damaged due to the cytotoxic effect of eosinophilic granules b) decrease in the level of eosinophils - acute period of infections and intoxications - acute period of an allergic reaction - increased levels of glucocorticoids or treatment with glucocorticoids - stress, severe physical activity - ovulation 3. Basophils. Normally 0-1% (in newborns up to 4%) a) increased level of basophils - allergic reactions - malignant tumors - stress - hypothyroidism - before menstruation - during treatment with estrogens - in chronic myeloid leukemia, erythremia - acute hepatitis - splenectomy - pregnancy - after vaccinations! b) decrease in the level of basophils (rare) - see decrease in the level of eosinophils 4. Monocytes. Normally 3-11% (in newborns up to 35%) a) increase in the level of monocytes - recovery period for acute infections - chronic infections (tuberculosis, syphilis, malaria, brucellosis, chronic pyelonephritis, septic endocarditis) - paraproteinemia (myeloma, Waldenström's disease ) - malignant tumors - lymphogranulomatosis - hepatitis - collagenosis - recovery from agranulocytosis - chronic myeloid leukemia - chronic monocytic leukemia - viral infections in children, especially infants b) decrease in the level of monocytes (rarely) - acute period of infections, intoxications - high-dose irradiation - treatment with glucocorticoids 5. Lymphocytes. Normally 19-37%, in children under 5-6 years old - up to 50-70% (so do not faint when you see a child’s analysis on an adult form:) a) an increase in the level of lymphocytes - the recovery period for acute infections - chronic infections ( tuberculosis, syphilis, brucellosis) - viral infections (influenza, measles, rubella, chickenpox, viral hepatitis, etc.) - allergic reactions - chronic lymphocytic leukemia - hyperthyroidism - after vaccination! b) decrease in the level of lymphocytes - all immunodeficiencies (congenital and acquired) - lymphogranulomatosis - tuberculosis of the lymph nodes - radiation sickness - treatment with immunosuppressants - acute infections c) the appearance of wide-cytoplasmic lymphocytes (atypical mononuclear cells) - up to 5% normal, 5-15% - viral infections, >15% - infectious mononucleosis d) plasma cells - normally single, 5-10% - viral infections, long-term chronic infections, tumors, myeloma, collagenosis, after vaccination!
https://prosto-kat.livejournal.com/232904.html
What are lymphocytes?
Lymphocytes in the blood are a type of leukocyte and, together with monocytes, form a group of agranulocytes, i.e. cells that do not have granules. Lymphocytes are the leading component of the immune system. Knowing what lymphocytes are in a blood test, doctors determine the patient’s immune status and receive information about the presence of infection and other diseases in the body.
Blood cells are produced in lymphoid organs. Here they differentiate and function. Production takes place in:
- bone marrow and fetal liver;
- central organs (for example, thymus);
- peripheral organs (spleen, lymph nodes, tonsils, blood, appendix).
Lymphoid cells
All lymphoid cells have in common: basophilia of the cytoplasm of varying degrees, the cloud-like nature of the chromatin, the granularity has the appearance of granules.
Lymphocyte precursors are formed in the bone marrow, then, during differentiation and maturation, they populate the central organs of the immune system, where the maturation of B-lymphocytes (humoral immunity) and T-lymphocytes (cellular immunity) occurs. After that, B-lymphocytes and T-lymphocytes populate the spleen and lymph nodes, where they are located in well-differentiated B-dependent and T-dependent zones.
A prolymphocyte is a round-shaped cell with rather difficult differentiation and morphological characteristics. Contains a nucleus with a delicate structure with remnants of nucleoli. The cytoplasm is basophilic, without granules.
Narrow cytoplasmic lymphocyte
Lymphocyte has a variety of morphological characteristics, since the populations of lymphocytes found in the peripheral blood are quite diverse. It has a number of clear characteristics: the cytoplasm of the cell is light basophilic, the nucleus is round or oval, eccentrically located, the chromatin is cloud-like, the color of the nucleus is intense. When stained according to Romanovsky, nucleoli in lymphocytes are not detected, but 1-3 nucleoli are distinguishable with special staining with methylene blue.
What are lymphocytes responsible for in the human body?
To understand what lymphocytes in the blood are responsible for, it is necessary to consider the functions of these blood cells. Blood cells signal the state of the immune system and are primarily responsible for fighting foreign elements that have entered the body. You can also read what eosinophils and segmented neutrophils are on the website.
At the same time, protective cells fight equally well against viruses and bacteria, fungi and other organisms. Foreign cells include malignant and aged cells that do not fulfill their purpose in the body. The work of blood cells in the body has clearly defined stages, for which various types of lymphocytes are responsible:
- providing cellular immunity;
- regulation of hematopoiesis;
- release of cytokines;
- regulation of humoral immunity.
How to take the test correctly?
There is no special blood test for lymphocytes; this indicator is traditionally determined in each analysis - general or extended. It is not difficult to take a general blood test for lymphocytes, so no special preparation is required for it. The only thing doctors warn about before the analysis is:
- The test must be taken in the morning, in the first hours after waking up;
- Before donation, you cannot eat food; children and adults are only allowed water in small quantities;
- Do not smoke, give your body increased physical activity, or experience stress.
If all recommendations are followed, the doctor receives reliable results and compares the numbers in the blood test with the norm of lymphocytes in a person according to age. The level of lymphocytes in the blood allows us to judge the presence of diseases in the patient.
Designation of lymphocytes in blood tests
The designation of lymphocytes in a blood test varies depending on:
- quantitative content of blood elements;
- percentage compared to other bodies.
In the test results, protective bodies are designated by the Latin letters LYM with a “%” sign next to them. Knowing how lymphocytes are designated in a blood test, it is easy to compare their quantitative and percentage indicators with reference values.
In the test results of some laboratories, the level of cells may be indicated slightly differently, which does not change the essence of the results obtained. The quantitative indicator corresponds to the designation LY or LY “#”, and when designating the ratio, lymphocytes as a percentage of the norm look like LY% with the corresponding value.
What does an increase in lymphocytes in the blood indicate?
The penetration of foreign cells into the human body leads to changes in test results, as shown by lymphocytes in a blood test. An increase in the norm of lymphocytes in the blood indicates:
- infectious pathologies, for example, syphilis, rubella, measles, hepatitis, cytomegalovirus, chickenpox or whooping cough;
- oncological diseases of the bone marrow - non-Hodgkin's lymphoma, chronic lymphocytic leukemia.
Normal and elevated lymphocytes in the blood
High rates in women
Increased levels of corpuscles in women occur in the above conditions.
Above normal in children
If lymphocytes do not correspond to the norm in children and the numbers are significantly increased, then this may indicate:
- infectious diseases, in particular chickenpox, rubella, mononucleosis, mumps, etc.;
- oncological pathologies (for example, Ewing's sarcoma, neuroblastoma, acute lymphocytic leukemia, Hodgkin's disease and other oncological diseases occur in childhood).
Table of normal values by age
The norm of lymphocytes in a person’s blood varies depending on age. When deciphering test results, it is taken into account what norm of lymphocytes in the blood corresponds to a particular age. The norm of lymphocytes in the blood of an adult will be significantly lower than that of a child.
Norms for women
The table of lymphocyte norms by age in women contains absolute and relative indicators of blood cells. The number of lymphocytes in the blood of women and the norm by age are expressed in the following table:
Varieties
The structure of the cell changes under the influence of microorganisms. As a result, its functions and parameters completely change.
Degenerative
A period of prolonged intoxication leads to the formation of degenerative cells that are unable to divide and function due to accumulated toxins. Their size decreases or increases. The culprits of the changes are liver dystrophy, sepsis, and abscess.
Downey cells
The size of atypical mononuclear cells is larger than that of healthy lymphocytes. They are characterized by the presence of a monocytic nucleus. Lymphomonocytes are an indicator of the presence of a viral infection. Most often it is herpes or mononucleosis. Recovery leads to normalization of blood composition. In the blood of children, atypical mononuclear cells are present in an amount of no more than 1%. Indicators may be elevated due to recent illnesses or vaccinations. They are also found in adults. The appearance of such cells is associated with an increased likelihood of infection with herpes or allergies.
Downey cells in the blood
Botkin-Klein-Gumprecht shadow cells
This concept includes destroyed lymphoid cells obtained during the preparation of the test material for analysis. This means that blood cells are subject to rapid destruction. Because they are difficult to detect, they are called shadows. Characteristic of chronic lymphocytic leukemia.
Reader cells
The detection of kidney-shaped cells with nuclei that have a jagged outline signals serious diseases. Most often, a person is sick with leukemia, pernicious anemia, and severe infections.
Latin (English) letters in blood tests. How to decrypt?
Currently, most indicators are performed on automatic hematology analyzers, which are able to simultaneously determine from 5 to 24 parameters. The main ones are: the number of erythrocytes, the average volume of an erythrocyte, the number of leukocytes, hemoglobin concentration, hematocrit, the average concentration of hemoglobin in an erythrocyte, the average hemoglobin content in an erythrocyte, the half-width of the size distribution of erythrocytes, the number of platelets, the average volume of a platelet.