Bilirubin is a bile pigment, one of the main components of bile. It is formed mainly from hemoglobin, which is found inside erythrocytes (red blood cells). The lifespan of red blood cells is about 120 days, and they are constantly renewed. As a result of the breakdown of old red blood cells, heme molecules from the released hemoglobin are converted into bilirubin. This form of bilirubin is called indirect (free, unbound, unconjugated) bilirubin.
Indirect bilirubin is transported by albumin in the blood to the liver, where it combines with glucuronic acid and becomes direct (bound, conjugated) bilirubin.
Decipher "General blood test" Decipher "General urine test"
Direct bilirubin then mixes with bile and enters the small intestine through the bile ducts, where it is destroyed by bacteria and ultimately excreted from the body in the stool. The breakdown products of bilirubin give the stool its characteristic brown color.
Direct bilirubin, unlike indirect bilirubin, is water soluble and can be excreted from the body. Indirect bilirubin is quite toxic; it can only be removed through transformation into direct bilirubin.
Using a blood test, you can determine the amount of direct and indirect bilirubin in the body, as well as its total amount - total bilirubin.
Preparing for the test
In order for the test results to be reliable, a number of simple rules must be followed and some preparation must be done. As with a regular biochemical blood test, when checking bilirubin, you must come to the treatment room early in the morning, on an empty stomach.
- 1 - 2 days before the planned blood draw, you should avoid eating fried and fatty foods so that the liver is not overloaded.
- 2–3 days before the test, you should refrain from playing sports, since intense exercise and stress affect the functioning of the liver. The use of medications should also be limited (about 1 to 2 weeks in advance), since the components they contain can also change indicators, complicating diagnosis.
In some cases, the doctor may prescribe a repeat test with mandatory adherence to a diet for several days, while the nutritional value of the foods consumed should not exceed 500 kcal.
Blood is drawn from a vein. The patient's arm above the elbow is clamped with a tourniquet, after which a vein is pierced with a syringe and the required amount of blood is drawn.
Bilirubin test: why is it prescribed and what can it tell you?
The concept of “jaundice” is probably familiar to everyone. But not everyone knows that bilirubin is responsible for all the signs of jaundice - from changes in skin color and whites of the eyes to darkening of urine and changes in stool color. Normal bilirubin metabolism indicates the health of the liver and all detoxification systems of the body. But how can you find out the level of bilirubin in the body?
What is bilirubin
Bilirubin is called bile pigment, a substance that is formed during the breakdown of certain substances, including waste hemoglobin.
The body reuses iron from hemoglobin, but the protein part of the molecule, after complex biochemical processes, is converted into bilirubin. Figures and facts Every day, about 1% of all red blood cells that carry hemoglobin are destroyed in our body.
That is, completely red blood cells are renewed in about 3 months. This primary bilirubin is also called indirect, unbound or free. It is poorly soluble in water, so it is transported by special proteins - albumin. With their help, bilirubin enters the liver, where a whole chain of transformations occurs again.
In the liver, the albumin + bilirubin group breaks down, bilirubin joins glucuronic acid, and bilirubin glucuronide is formed - a soluble form of this pigment, called bound or direct. It is excreted from the liver along with bile and enters the intestines. And there, bilirubin glucuronide, with the help of intestinal flora, is converted into urobilinogen (glucuronic acid is split off), which is partially reabsorbed into the blood, and stercobilinogen, the main part of which is excreted in the stool. It is this that gives stool its specific dark brown color.
Hepatitis, Rh conflict, cirrhosis, cholecystitis - all these diseases lead to increased bilirubin levels.
What are bilirubin tests?
Bilirubin is usually determined in the blood and less commonly in the urine. In a biochemical blood test for bilirubin, the total level of this pigment and its direct bound form are determined. And unbound bilirubin is simply calculated from these two indicators. These are three different analyses, so it’s worth looking at what exactly is indicated in the direction in advance.
The amount of this bile pigment is measured in milligrams or micromoles per liter of plasma, but most often you can see the result in µmol/l on the form. The result can usually be obtained the next business day or one day after the blood is drawn. If an answer is needed urgently, some laboratories are ready to conduct a cito analysis, that is, urgent, and issue a ready analysis within two to four hours.
Modern equipment makes it possible to determine the concentration of bilirubin in blood plasma with an accuracy of tenths of a micromole. The result obtained allows us to identify problems in the liver, even when there are no other symptoms yet. And if signs of jaundice have already appeared, then this analysis helps the doctor determine its possible cause and begin a targeted search.
Bilirubin in urine is determined during a standard general urine test. The result of such a study can be obtained in one to two days. If necessary, it can also be done urgently.
In many modern laboratories, urine analysis for bilirubin is done on automatic analyzers, which completely eliminates the “human factor” and significantly reduces the likelihood of error. This study alone will not make a diagnosis, but will help the doctor navigate the problem, assess the severity of the condition and the prognosis of the disease.
When is the test scheduled?
A biochemical blood test for bilirubin is performed when:
- liver diseases;
- destruction of red blood cells;
- violation of the outflow of bile and diseases of the biliary tract;
- the appearance of yellowness of the eyes and skin;
- preventive examination.
In order to detect bilirubin, a general urine test is usually prescribed for the same diseases as a blood test. But this is more of an auxiliary and screening analysis.
Rules for preparing for research
Blood for biochemical analysis is taken from a vein on an empty stomach. It is advisable to take the test in the morning, before meals. As a last resort - about four hours after a light breakfast. In short, the requirements do not differ from the standard ones.
For a general urine test, you need to prepare a small, clean, resealable container in advance. A special disposable container can be purchased at any pharmacy or supermarket with a health products section. It will cost about 15–20 rubles and will be much more convenient than any “homemade” jar.
For analysis, the first stream of urine should be released into the toilet, and then the biomaterial should be collected in a container. Before doing this, be sure to take a light shower so that cells and bacteria from the surface of the mucous membranes and skin do not get into the jar.
Norms in the results of bilirubin analysis
A normal indicator in a blood test is considered to be a total bilirubin concentration of 3.4–17.1 µmol/l. Of these, direct bilirubin is up to 3.4 µmol/l, and indirect bilirubin is up to 13.7 µmol/l. However, it is better to focus on the standards indicated on the test results form, since they may differ slightly in each laboratory.
In a newborn, the amount of bile pigment will always be much higher, approximately 24 to 250 µmol/l. This is a normal physiological reaction.
A urine test is much easier to interpret. Normally there should be no bilirubin in it.
What does elevated bilirubin level mean?
When interpreting test results, it is important to determine which type of bilirubin is elevated.
An increase in the level of indirect bilirubin indicates increased destruction of hemoglobin. This happens with Rh conflict, poisoning, and with some blood diseases. The concentration of direct bilirubin increases when some obstacle occurs in the path of bile outflow - spasm, swelling or stone.
In diseases that affect liver tissue, such as cirrhosis or hepatitis, all indicators increase at once.
When the level of total bilirubin is above 30 µmol/l, skin color begins to change and jaundice appears. Around the same time, this pigment begins to be detected in the urine.
Where can I donate blood and urine to test bilirubin levels?
You can get tested for bilirubin at a clinic under the compulsory medical insurance policy. To do this, you need to visit your local therapist. Usually he asks about complaints and conducts a general examination. If the doctor decides that such an examination is really necessary, he will write out a referral with which you will need to go to the treatment room.
Without a referral, tests can be taken for a fee in the same clinic, at any private medical center or in a laboratory. Here you may also be asked about complaints, but this is more of a general question: no one will insist on the presence of “serious” evidence.
The good thing about a local clinic is that you don’t have to pay for the analysis. Plus, the doctor can note in the direction not only bilirubin, but also other blood parameters. The disadvantages include a significant amount of time, which is usually spent in queues and long waits for results. In addition, the results of the study will again be sent to your doctor. And these are again coupons, queues and waiting. So you need to be prepared to set aside time for three visits to the clinic.
This is interesting According to social studies, residents of the Leningrad, Kurgan, Novgorod, Vladimir, Irkutsk, Amur, Ivanovo, Sakhalin regions and the Republic of Dagestan spend the longest time in line to see a doctor. In the Bryansk region, you will have to wait almost 1.5 hours to see a therapist. And the average waiting time in line across all regions is about 31 minutes.
The equipment in different public hospitals and clinics varies significantly. Medical institutions that fell under the modernization program or managed to find themselves in the market for paid services can boast of good modern equipment. In other institutions, tests are still carried out manually, which can lead to a wide range of results. So this point is also worth finding out in advance.
It will be easier to get tested for bilirubin in a private medical center. But it’s worth asking in advance how you can collect the result. In some cases, the research results again go to the doctor, and the patient will be able to receive them only after consultation with a therapist or gastroenterologist.
Of course, consultation with a specialist is necessary if you actually have abnormal test results. But paying extra for an appointment to find out that the tests are normal may not be very pleasant.
Most medical centers do not have their own laboratory and transport biomaterials for research to other institutions. That is, the cost and time of research increases, but its quality remains the same.
Private laboratories only conduct research, so you can’t count on a doctor’s consultation. But the research itself will be carried out quickly, accurately and without extra charges.
Determining direct and total bilirubin will cost approximately 150–260 rubles for each indicator, plus 100–170 rubles for drawing blood from a vein. In some laboratories, when ordering these two tests at the same time, the level of indirect bilirubin is calculated free of charge and also included in the study form. A general urine test will cost about 200–250 rubles.
When choosing a clinic or laboratory for testing, clarify in advance how long the test will take and how the result can be obtained. Some clinics and laboratories offer to send results by email or publish them in a private section of the website, while others will have to go again to pick up a paper form. If you need the result urgently, choose a laboratory that can perform a cito analysis.
Determination of the level of bilirubin in the blood and urine is included in the standard list of studies. This analysis is prescribed both when a number of diseases are suspected and for preventive examination. The main thing is to choose a clinic or laboratory where it will be convenient to submit biomaterial for analysis and you can quickly obtain reliable research results. And in case of any deviations, consult a qualified doctor.
Types of bilirubin
When determining the amount of yellow pigment, the concentration of total bilirubin is initially determined, after which the direct component is determined, and the difference between these indicators is considered the level of the indirect component.
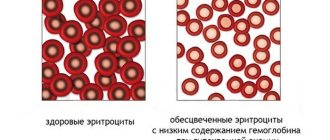
Total bilirubin is usually understood as the entire available volume of this substance in the blood plasma. The indirect type of bilirubin consists of unconjugated and water-insoluble elements. The direct type is a substance that is conjugated and soluble in water.
Each type of bilirubin (direct and indirect) has its own special significance, since it is through the determination of this substance that doctors are able to identify many pathologies in the functioning of not only the liver, but also other systems and organs.
The indirect form of bilirubin is a toxic element, and the liver’s task is to neutralize it, convert it into a direct form, that is, into substances soluble in ordinary water, with which bilirubin is excreted from the body. If the level of this substance in the patient’s blood is elevated, he develops characteristic “icteric” signs: yellowing of the skin, dryness and itching, toxicosis.
What is bilirubin, its functions and types
Bilirubin is classified as a hemoglobin pigment, since almost 85% of it is formed during the breakdown of red blood cells. This process is continuous.
Initially, indirect bilirubin is formed in the blood and tissues, which is sent through the bloodstream to the liver. Here its biochemical transformation occurs in the process of reaction with glucuronic acid.
As a result of this reaction, direct bilirubin appears and, together with bile, it is excreted into the duodenum. This substance dissolves in water and leaves the body along with feces. It is this indicator that gives the brown color to stool.
During the day, 1% of red blood cells in the human body are destroyed, resulting in the formation of 300 mg of bilirubin.
Bilirubin in a blood test is indicated in 3 values:
- Indirect - formed immediately after the breakdown of red blood cells and has not yet been processed in the liver;
- Direct – appears after processing in the liver;
- Total is all the pigment found in the bloodstream.
The norm of total bilirubin in the blood of women by age
The average normal pigment value is considered to be from 3.5 to 20.5 µmol/l. Of course, reference data is of decisive importance, so doctors mainly focus on them.
If the values of bilirubin in the blood are higher than the specified norm, then in some cases they are not considered a violation. The content of this indicator may be higher if a woman has any disturbances in the functioning of the gastrointestinal tract.
Various conditions, for example, the menstrual cycle, pregnancy, can distort the accuracy of the results of blood tests for bilirubin obtained in women.
As a rule, in the initial phase of the menstrual cycle, many women experience a slight increase in this component, but after the end of planned bleeding, everything quickly returns to normal. Indications also change with age. Increased bilirubin can be detected in the presence of hepatitis C in a chronic form, exacerbation of gastrointestinal diseases.
In newborns, levels of yellow pigment in the blood are always quite high, but only in the first days after birth. After the first week of their life, the bilirubin level is established and returns to normal.
An increase in the indicator: a variant of the norm or a sign of pathology?
The maximum values are typical for newborn babies. According to statistics, every second full-term baby experiences physiological jaundice. For premature babies, the incidence rate exceeds 80%.
Jaundice is not a pathology and normally goes away within 2 weeks. In the case of a protracted process, the newborn may be shown phototherapy (lighting with blue spectrum rays) or blood transfusion (with a critical increase in bilirubin levels and signs of damage to the central nervous system).
In adult men, exceeding the permissible values, without exception, is a sign of the disease. For a more accurate differential diagnosis, it is necessary to determine a set of additional laboratory tests (levels of aspartate aminotransferase, alanine aminotransferase, etc.) and instrumental examination methods.
The main reasons for increased bilirubin in men:
- hemolytic anemia, accompanied by excessive destruction of red blood cells;
- non-hemolytic familial jaundice (Gilbert's syndrome) is a benign pathology characterized by a moderate increase in the level of bile pigment in the blood;
- Crigler-Nayyar syndrome is a severe congenital pathology in which a toxic indirect fraction affects the human nervous system;
- blockage of the bile ducts with stones;
- hepatitis of viral or alcoholic etiology;
- cirrhosis of the liver;
- oncopathology of the liver or pancreas;
- congenital absence or underdevelopment of the biliary tract;
- infection with helminths from the Echinococcus family;
- use of hepatotoxic drugs;
- systemic infectious pathologies;
- purulent inflammation of liver cells and loss of their functional activity.
Features of deviations from the norms
With age, most women tend to decrease the level of this blood element, which is largely due to the gradual appearance of various ailments that affect the level of pigment formed.
As a rule, women who have given birth by this age have a weakening of the liver, which is caused by the increased load on the organ during the period of gestation. This also cannot but affect bilirubin levels and is not an abnormal deviation. Let us consider in more detail the features of deviations from the norm of total bilirubin in the blood in women after 40, 50, 50 years.
Features of decreased bilirubin levels in adult women:
- In women over 40 years of age, the norm is considered to be from 3.9 to 17.6 µmol/l, which is associated with various liver diseases, as well as disturbances in the digestive system as a whole. Also, deviations considered normal occur during ovulation, during menstruation. The amount of pigment can also be influenced by external factors, for example, climate change, excessively high temperature outside or, conversely, hypothermia.
- The normal level of bilirubin in the blood of women over 50 years of age ranges from 3.7 to 17.4 µmol/l, but sometimes the result may be somewhat underestimated. At this age, women already enter menopause, which causes not only hormonal instability, but also the appearance of many diseases on this basis. All this cannot but affect the level of bilirubin, but, as a rule, deviations are not negative.
- After 60 years, the level of bilirubin in the blood of women, as well as men, may decrease somewhat, since most people of this age develop diseases of the cardiac system. As a result of the lower content of red blood cells in the blood and the decrease in hemoglobin due to these diseases, the level of bilirubin, formed from the destruction of dead red blood cells, also drops.
How to correctly take a biochemical blood test for total bilirubin
To obtain a reliable result of a biochemical blood test for total bilirubin, you should:
- donate blood in the morning (from 7 to 11 o’clock) on an empty stomach - after a break in meals from 8 to 12 hours;
- 3-5 days in advance, agree with your doctor on the possibility of using medications and dietary supplements;
- 2 days in advance, alcohol, overeating and fasting are prohibited, you cannot start strict diets, or eat fatty and spicy foods;
- physical and psycho-emotional stress should be eliminated per day;
- stop smoking 1.5 hours before donating blood;
- In 30 minutes, it is important to limit physical activity and maintain psychological peace.
Blood sampling for biochemical testing
Set for determining the indicator: how it affects the result
A pigment determination kit can affect bilirubin levels; different laboratories use different reagents and methods . Therefore, if repeated blood tests are necessary, it is important to have the tests taken at the same institution.
Increased or decreased bilirubin
Reasons for the high rate
Bilirubin levels may increase due to:
- The presence of severe gallstone disease, especially in chronic or acute form.
- The presence of serious diseases of the gallbladder or liver, for example, cirrhosis or hepatitis.
- The presence of bad habits, such as smoking or alcoholism, especially with frequent abuse.
- The appearance of various forms of acute respiratory infections and acute respiratory viral infections, as well as influenza and other infectious diseases.
- Abuse of many drugs, especially analgesics, aspirin, various groups of antibiotics, hormonal drugs.
- Hereditary factor.
- The presence of prolonged and very frequent bleeding.
- The presence of malignant neoplasms in the body.
- Diseases of the pancreas that are inflammatory in nature.
Increased bilirubin in the blood for a long time poses many dangers to the female body, for example, this condition threatens serious toxic damage to the muscles, which can spread to the brain. This will require urgent qualified medical care.
Causes of low bilirubin levels
Low bilirubin levels may occur due to the following factors:
- Abuse of drinks containing a lot of caffeine, such as energy drinks, black coffee, tea.
- Diseases of the heart and blood vessels, especially in chronic form, for example, cardiosclerosis, heart failure of various types, coronary heart disease.
- The presence of bad habits, alcoholism or smoking, and their abuse.
- Excessive use of certain medications.
Concomitant symptoms with increased indirect bilirubin
Although self-diagnosis is a dead-end path, knowledge of the symptoms accompanying a particular disease is necessary. This makes it easier to figure out which specialist to contact.
- Anemia. Anemia is characterized by: weakness, vertigo (dizziness), pale skin, headache.
- Hepatitis is accompanied by: pain in the liver (aching, dull pain), a feeling of fullness in the right hypochondrium, bitterness in the mouth (due to the reflux of bile into the bloodstream and digestive tract), sour taste, belching.
- Cirrhosis of the liver. Constant companions of cirrhosis, in addition to the already mentioned “liver” symptoms, are: yellowing of the skin, development of spider veins on the skin, change in the color of stool (faint beige or white stools).
- Problems with the gallbladder are accompanied by nausea, vomiting, diarrhea or constipation, intense dagger pain in the right hypochondrium.
- Genetic and other syndromes. They are characterized by the development of severe jaundice.
- Parasitic lesions. When they occur: nausea, vomiting, sudden weight loss.
- Vitamin deficiencies are rarely accompanied by noticeable symptoms. We can talk about bleeding gums (as well as if direct bilirubin is increased), muscle weakness, skin problems, etc.
The most common symptoms of increased indirect bilirubin were and remain:
- decreased appetite;
- nausea;
- yellowing of the skin and sclera;
- belching with a sour taste;
- weakness, weakness;
- headache and dizziness;
- vomit;
- pain in the right side;
- flatulence;
- discoloration of stool;
- skin itching.
Based on the characteristic symptoms, the patient can assume this or that problem and go to a specialized specialist for help.
What to do if bilirubin levels are elevated?
If the pigment concentration does not increase too much, the therapy does not involve much difficulty. Treatment is prescribed only by specialists after identifying the provoking factors.
Treatment options:
- Glucose and medication are injected intravenously to remove toxins.
- Phototherapy, in which training occurs with lamps, while molecules of harmful pigment bind to other microelements.
- Medicines that improve the flow of bile.
- Diet.
- Maintaining a proper diet is considered mandatory for therapy.
Patients should not eat:
- alcohol;
- coffee;
- tea;
- fried food;
- spices;
- canned foods;
- The amount of egg yolk consumed is limited.
When preparing a diet, a specialist may prescribe activated carbon or some of its analogues. In this way, the body can quickly cleanse itself of toxic substances.
Therapy using traditional medicine, decoction, and tinctures is allowed. Extracts of the following plants have proven themselves to be effective:
- Rose hip.
- A combination of mint and St. John's wort.
- Corn silk.
- Motherwort.
Before regulating the amount of bilirubin in the blood using traditional medicine, you should consult your doctor. It is advisable to avoid possible complications from such treatment.
After receiving the results of the examination, you can solve the problem of regulating the amount of bilirubin in the blood. First you need to accurately determine the reason for the increase. Therefore, a detailed examination is carried out using laboratory equipment. Based on the results and analysis, the specialist determines the exact diagnosis. The choice of therapeutic technique is determined by the developing disease. Hepatoprotectors are often used; the medicine includes a list of complex methods of influence. The drug helps strengthen and normalize the functioning of hepatocytes.
If the bile ducts become clogged, medication is used to thin the secretions. When diagnosing a hereditary pathology, it is preferable to choose a treatment method that allows achieving stable remission. The main therapeutic measures aimed at reducing unpleasant symptoms. To combat viral hepatitis, antiviral drugs are used together with immunostimulants. In critical situations with chronic cirrhosis, surgery and liver transplantation are performed. High-quality sorbents and antioxidants help get rid of toxins.
Repeated analysis should be carried out after completion of the course of therapy. To ensure that the error in the data obtained when using instruments is minimal, the examination must be carried out in the same laboratory. If the level of bilirubin in a woman’s blood is restored, then the therapy was successful and the body is recovering. When a positive trend is not observed, the therapeutic technique needs to be adjusted.
What are the types of jaundice?
In newborns, physiological or transient jaundice usually occurs, which appears as a result of the body’s adaptation to new conditions. Transient jaundice occurs in 60-70% of cases and often does not require medical intervention. Pathological jaundice is much more dangerous and can lead to serious disturbances in the functioning of the central nervous system and brain. An increase in bilirubin to a critical level can lead to the death of the baby.
Physiological jaundice of newborns
Bilirubin standards for a newborn are up to 34 units per liter of blood. On the second day, the levels increase and can reach 150 µmol/liter. On the third day, the maximum value is 250 µmol/liter. After the third day of life, the child's bilirubin begins to gradually decrease. By the month it should be 9-20.5 µmol/liter. All indicators are checked only using a blood test.
In addition to bilirubin, doctors also look at other blood indicators that may indicate problems with the body. In some cases, the first signs of jaundice may appear only on days 4-7, which is due to the large birth weight and good appetite.
If the child has no changes in the color of feces and urine, he is calm, and his indicators are within normal limits, then they try not to prescribe medications and additional procedures to newborns.
One of the important factors for the successful removal of bound bilirubin is regular bowel movements and urination. Factors that cause transient jaundice include:
- Premature or difficult labor;
- The mother has chronic diseases, including diabetes, diseases of the hematopoietic system;
- Rhesus conflict;
- Stimulation of labor;
- Emergency delivery by caesarean section;
- Lack of breastfeeding;
- Anomalies in the development of organs and systems;
- Sudden weight loss after birth;
- Oxygen starvation of a child.
For children who were born before 34 weeks of pregnancy, critical bilirubin levels are half the normal level than for full-term children. An increase in bilirubin can be initially detected using a special device that photometrically determines the concentration of the substance in the blood. If suspicions arise, doctors conduct more detailed studies and take blood for analysis.
Total bilirubin is elevated - what does this mean in an adult and how to treat it?
If direct bilirubin is slightly increased (no more than 5 µmol/l), a repeat test is prescribed after 3-5 days in order to exclude internal and external factors that influence the result. For example, daily fluctuations in all laboratory blood parameters or the subject’s neglect of the rules for preparing for the collection of biomaterial.
Thus, bilirubin in the blood - 3 is considered a slight deviation to the lower side, which can be caused by recent consumption of alcohol, large amounts of coffee or medications.
Treatment of any pathology is the task of the doctor. Self-diagnosis and independent choice of treatment methods can lead to a worsening of the disease, even death.
The reasons why total bilirubin is elevated are different and are always pathological in nature. Of particular importance in differential diagnosis is which fraction exceeds the norm.
Read further: How to quickly and effectively reduce bilirubin in the blood at home?
What does it mean if direct bilirubin is elevated in an adult?
The reasons for the increase in the value of total bilirubin in the blood, mainly due to the direct fraction, include:
- Cholidocholithiasis is a pathological condition that occurs with cholelithiasis. It manifests itself in the form of the formation of stones that block the lumen of the bile ducts. The importance of early detection is due to frequent complications. Lack of adequate treatment contributes to the development of cirrhosis, pancreatitis or pancreatic necrosis. The preferred method of treatment is endoscopic or liparoscopic stone removal. Relapse in 25% of cases within 5 years. Repeated surgery is accompanied by removal of the gallbladder;
- Hepatitis C is an infectious disease that causes inflammation of the liver. According to statistics, 150 million people are infected with the hepatitis C virus. It is called the “gentle killer” because the patient may not know about the infection for a long time. The patient can live up to 40 years without showing serious pathological signs. The prognosis depends on the presence of concomitant diseases. Thus, HIV-positive status significantly increases the risk of developing cirrhosis or liver cancer;
- Primary sclerosing cholangitis is a rather rare pathology in which the tissue of the bile ducts becomes inflamed and grows. The outcome is biliary cirrhosis, accompanied by impaired immune regulation. At the same time, the immune system begins to destroy its own normal cells of the bile ducts, perceiving them as genetically foreign material (antigens);
- malignant neoplasms in the pancreas;
- Dubin-Johnson syndrome is a disruption of the process of releasing the bound fraction from liver cells, resulting in its abnormal movement in the opposite direction. In other words, bilirubin is not released from the liver, but, on the contrary, enters it from the bile ducts. The pathology is genetic in nature and manifests itself in the form of chronic jaundice. The prognosis of the disease is extremely favorable, since it does not affect life expectancy in any way;
- Rotor syndrome - similar to the previous disease, however, has a less pronounced degree of severity;
- alcoholic liver damage is a disruption of the normal functioning of liver cells due to long-term (more than 10 years) intoxication with alcohol and its breakdown products. Possible consequences: alcoholic hepatitis, cirrhosis, cancer and fatty liver.
Read further: Decoding, norm of biochemical blood test indicators in the table
Increase in total bilirubin due to the indirect fraction
List of diseases accompanied by high levels of indirect bilirubin in the blood:
- autoimmune hemolytic anemia - occurs as a result of the production of autoimmune heat antibodies (react at temperatures above 37 ° C). May be due to medications or leukemia;
- hemolytic anemia is characterized by increased destruction of red blood cells with excessive release of the indirect fraction into the blood;
- megaloblastic anemia - a lack of vitamin B 12 leads to the deposition of immature red blood cells. At the same time, the content of hemoglobin, and, as a consequence, its breakdown products increases significantly;
- hereditary microspherocytosis - changes in the protein of the erythrocyte membrane, leading to a violation of its integrity and increased degradation processes;
- Cooley's anemia is a mutation of the polypeptide chains of hemoglobin. Defective genes that increase bilirubin are HBA1, HBA2 and HBB. Characterized by severe changes in the structure of the skull, nose and teeth. Chronic jaundice, enlarged spleen and liver. Early manifestation of the disease leads to mental and physical underdevelopment;
- Gilbert's syndrome (non-hemolytic familial jaundice) is a pigmented benign liver disease in which the intracellular transport of the unbound fraction to the site of attachment of sugar-containing substances is disrupted. Despite the chronic course throughout life, it does not affect its duration;
- congenital Crigler-Nayjar syndrome is a malignant disease accompanied by chronic jaundice and pathologies of the nervous system. Jaundice occurs as a result of a failure in the transformation of indirect bilirubin into direct bilirubin due to the absence/lack of necessary enzymes;
- Malaria is an infectious disease, in the life cycle of which the pathogen includes a reproduction phase in erythrocytosis. After maturation, the parasitic plasmodium is released from red blood cells, starting the active process of their destruction. One of the complications is the occurrence of chronic renal or liver failure.
What does it mean if the fractions are increased in equal shares?
The reasons for the increase in total bilirubin in the blood, while the direct and indirect fractions are increased in equal proportions, are considered to be:
- hepatitis of a viral or toxic nature (alcohol or drugs);
- cirrhosis of the liver;
- infection with herpes virus type 4, which is characterized by increased body temperature, damage to the liver and spleen, as well as changes in the cellular composition of the blood;
- liver damage by tapeworm (echinococcosis). Once in the liver, the larvae begin to form echinococcal cysts in the form of blisters, reaching sizes up to 20 cm. The slow growth of cysts makes it difficult to detect infection earlier, and if they rupture, the larvae spread throughout the body;
- liver abscess - the formation of a cavity with pus in the organ, which is a consequence of appendicitis, cholelithiasis or sepsis. In 90% of cases, with a competent approach to treatment, it is possible to achieve complete recovery.
Alternative
As mentioned above, any treatment must occur with the approval of the attending physician. For this reason, traditional medicine can only be used as an addition to the prescription. The most commonly used herbal medicine is to help reduce the level of bilirubin in the blood.
Various herbal mixtures and decoctions help restore the functioning of the circulatory and vascular systems.
There are several recipes that allow you to reduce bilirubin in both adult patients and children. Here are some recipes:
- Beetroot juice. You should take 1/3 cup of fresh beet juice twice a day.
- Motherwort decoction. Taken on an empty stomach every day for two weeks.
- A mixture of chamomile, motherwort and St. John's wort. The decoction is infused and drunk half a glass twice a day.
- Birch leaves are poured with boiling water and infused. Then the decoction is taken before bed. The duration of treatment is one week.
Increased total bilirubin: treatment
- Blood transfusion - the results of studies and clinical trials conducted in China show that this method for reducing high bilirubin levels with fewer side effects is one of the effective methods.
- Medicines - to remove bilirubin from the body and reduce it, you can use drugs such as salicylates, furosemide, ampicillin and ceftriaxone (some of the drugs are quite dangerous, you need to consult a doctor).
- Phototherapy (phototherapy, phototherapy) - Hyperbilirubinemia caused by jaundice can be easily treated without or with minimal consequences using phototherapy (treatment with sunlight or artificial light, rays). The effectiveness of phototherapy depends on many factors (the information below will be helpful when talking with your doctor): The surface area of the body exposed;
- Spectrum of the light source: usually for effective therapy special blue tubes marked F20T12/BB are used, and not F20T12/B, while the irradiation or energy output can be increased in the phototherapy unit, reducing the distance to the person within 15-20 cm.
- Continuous phototherapy will be better than intermittent phototherapy.
Conventional phototherapy:
Conventional or fiberoptic phototherapy units can be used, provided the jaundice is not hemolytic or progresses slowly.
Intensive phototherapy:
In conditions of hemolytic jaundice, a rapid increase in bilirubin, or the ineffectiveness of a conventional block, it would be appropriate to use intensive phototherapy.
Bilirubin and pregnancy
The amount of pigment should be carefully monitored during pregnancy. When a woman is pregnant, the body may experience an exacerbation of chronic diseases acquired before pregnancy (cholecystitis, anemia). Normally, the concentration of bilirubin should not increase.
In the table you can see the rate of bilirubin in women during pregnancy (but without depending on age)
Some past infections can also increase bilirubin levels. Toxicosis in the 1st trimester signals that the norm of pigment in the body of a pregnant woman is exceeded. If the amount of pigment in the mother’s body reaches a critical value, early delivery is performed.
A growing embryo is able to put pressure on the liver and gallbladder, thereby disrupting the circulation of bile and causing a rise in pigment levels.