The norm of leukocytes in the blood of children: reasons for the increase and possible diseases. A decrease or increase in the level of leukocytes indicates the development of disorders in the human body.
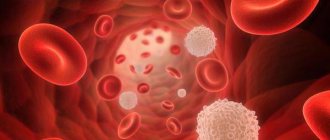
Leukocytes are otherwise called white blood cells, which are produced by the bone marrow. Their function is to restore damaged tissue and maintain immunity at the proper level. Leukocytes live for 20 years or more, although some types of cells live for only a few hours. Memory cells are distinguished by their long life, which, if necessary, are ready at any moment to remember the health offender and rush to destroy him. In the event of a quantitative violation, suspicion immediately arises of the penetration of an infection or virus.
In any case, the level of leukocytes changes frequently, this is influenced by stressful situations, physical activity, changes in the body’s condition, but the indicators fluctuate within the normal range. However, blood sampling for testing is carried out early in the morning on an empty stomach, then the indicators give an accurate result.
What are leukocytes and what are they for?
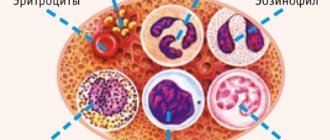
White blood cells are produced by the bone marrow and move throughout the body, penetrating even into its most secluded areas. If inflammation is detected in any organ or tissue, the number of cells begins to increase in this particular focus, and the bone marrow begins to produce them with renewed vigor. Leukocytes themselves are divided into several types. Cells with a granular component are usually called granulocytes, and those without grains are called agranulocytes.
The first category includes band and segmented, basophils and eosinophils. Agranulocytes are divided into lymphocytes and monocytes. They all have different structures and perform different functions in the process of hematopoiesis. The total number of white blood cells is called the body's leukocyte formula. White blood cells protect the child from various diseases that develop due to the penetration of viruses and infections into the body.
It is worth noting that they are the main assistant in the restoration of tissues after injury and inflammation, and also contribute to the manifestation of the body’s reactions to allergens, unusual stress, and fluctuations in ambient temperature.
What it is?
Leukocytes are white blood cells whose main task is to maintain immunity and protect the body from foreign agents. Unlike red blood cells (red cells), their content is approximately 1000 times less, so the blood itself is red. There are so many types of white blood cells that perform specific functions and are contained in different percentages.
When a foreign cell enters the body, leukocytes rush to it and completely block it. There are several subtypes of white blood cells:
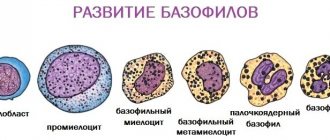
- Basophils contain heparin and histamine. This helps them be a catalyst for the process of lipolysis of fats in the blood. Histamine has an anti-inflammatory effect and stimulates phagocytosis. Basophils perform the function of preventing the formation of blood clots.
- Neutrophils are “suicide” cells. They absorb and break down the harmful cell. In this case, the neutrophil itself dies. The accumulation of dead neutrophils is called pus. Their main function is to fight bacteria and toxic substances. They can exist in tissues with poor oxygen supply. Active against virus attacks.
- Lymphocytes are the largest group of white blood cells. They make up approximately 40% of the total. Lymphocytes fight antigen proteins and bacteria. Some of them synthesize groups of immunoglobulins.
- Monocytes are macrophages that are the main catalysts of phagocytosis. These cells are designed to fight parasitic attacks. Actively block tumor tissues and stimulate normal levels of cell regeneration.
- Eosinophils perform an antibacterial function. They penetrate the membrane of the infectious cell and destroy it from the inside with the help of secreted enzymes. An active process of accumulation of eosinophils also occurs at the site of an allergic reaction.
In total, human blood contains 4000–9000 μl of leukocytes. Their number is constantly fluctuating. Red blood cells are more permanent. They have a fixed level.
The norm of leukocytes in the blood of a child
The norm of leukocytes in children at different ages is not the same and differs from the same indicator in adults. A child's white cell count is usually higher.
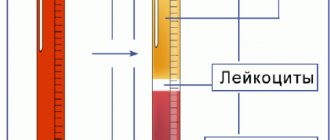
Their content is shown by the leukocyte formula, which changes in the child depending on age. When deciphering the analysis results, both the absolute number of different types of leukocytes and the relative number (in %) are assessed. A newborn normally has high lymphocytes (up to 60%), while neutrophils are reduced to 40%. By one year, there is a decrease in lymphocytes and an increase in neutrophils.
For children by age, the following norm of leukocytes in the blood is established:
- for newborns – 8-25Х10⁹/l;
- in the first week – 7-18Х10⁹/l;
- first month – 6.5-14Х10⁹/l;
- the first six months – 5.5-12Х10⁹/l;
- second six months – 6-12Х10⁹/l;
- second year – 6-17Х10⁹/l;
- from 2 to 12 years – 4-5.2Х10⁹/l;
- from 12 years - as in adults - 4-8.8X10⁹/l.
The relative content of different types of leukocytes in a child is as follows:
- segmented neutrophils – 59%;
- band neutrophils – 2%;
- basophils – 0-1%;
- eosinophils – 1-4%;
- lymphocytes – 46%;
- monocytes – 8%.
When deciphering the results, it is important to evaluate both the total number and the relative level. The absolute number may correspond to the norm, while certain types of leukocytes will deviate from the norm. Thus, a high level of neutrophils most often indicates the development of a bacterial infection, and elevated eosinophils most likely indicate infection with parasites. Each type of white blood cell performs its own specific function, so a change in the level of a particular variety may indicate a possible disease and its origin.
In the table, the norms are presented depending on age (the total number and relative level (in%) of different types of white cells).
Reasons for deviation from the norm
As mentioned above, the norm of leukocytes in children can deviate both upward and downward, and each such disorder has its own predisposing factors.
For example, when there are a lot of white blood cells, this is called leukocytosis, which can occur against the background of:
- a wide range of infectious and viral diseases;
- various allergic reactions;
- oncological processes;
- bone marrow lesions;
- purulent and fungal infections;
- inflammatory processes - leukocytes most often increase in appendicitis;
- diseases of the hematopoietic system;
- autoimmune and endocrine diseases;
- allergic reactions;
- parasitic and helminth infestation;
- extensive burns;
- surgical removal of the spleen.
Although the white blood cell count in newborns is elevated and this is considered a natural condition, this disorder can also be caused by:
- wide range of injuries;
- various infections;
- high blood viscosity;
- damage to the bone marrow, against which a large number of white blood cells are released.
Among the harmless sources it is worth highlighting:
- poor nutrition;
- physical activity;
- prolonged crying;
- powerful emotions;
- influence of stress;
- taking a hot bath.
When a child’s leukocytes are low, this is leukopenia, which in the vast majority of cases is a consequence of:
- immunodeficiency states;
- diabetes mellitus;
- allergic reactions;
- infectious and viral pathologies;
- long-term chemotherapy and radiotherapy;
- hypovitaminosis;
- hyperfunction of the spleen;
- renal failure;
- sepsis and leukemia;
- anemia;
- anaphylactic shock;
- drug overdose;
- previous surgical intervention;
- poor nutrition;
- penetration of chemicals and toxic substances into the body.
Degrees of leukopenia
In any case, it is very important to detect the root cause in time in order to prevent the development of dangerous complications.
How is the analysis performed?
When testing blood for a general or, as it is also called, clinical analysis, the child should, if possible, be hungry, i.e., the procedure is done on an empty stomach. Typically, blood collection rooms in clinics are open from 8.00. until 9.30. At this time, blood levels in the body are the most optimal.
Blood must be donated on an empty stomach, because after eating, the stomach begins to work actively and the number of leukocytes may increase, and this, in turn, may give the doctor incorrect information about the child’s health status. Also, before taking the test, you should not undergo any procedures, such as x-rays, FGDS and various physiotherapeutic procedures, this can also lead to an increase in leukocytes in the blood. [adsen]
Prevention and prognosis
To avoid the development of a problem such as leukocytosis, parents need to constantly monitor the implementation of several general, simple recommendations.
Prevention rules include:
- maintaining a moderately active lifestyle;
- healthy and balanced diet;
- strengthening the immune system;
- taking medications as prescribed by the clinician;
- avoiding the influence of stressful situations;
- regular visits to the pediatrician, and, if necessary, other pediatric specialists, as well as blood donation, which will indicate not only the main deviation, but also that the ESR values have changed, lymphocytes are decreased or increased, as well as monocytes, basophils or other components the main biological fluid of the body.
The prognosis of elevated leukocytes is directly dictated by the main etiological factor. In any case, parents should take into account that complete refusal of medical help and independent attempts to get rid of such a problem will lead to the formation of complications of the underlying disease, which can pose a danger to the child’s life.
Classification of causes
Elevated leukocytes in a child’s blood have the following forms:
- Physiological (natural) leukocytosis;
- Pathological – against the background of various changes;
- Monocytic – for bacterial infection and cancer;
- Eosinophilic – for allergic reactions;
- Pathological-symptomatic – occurs in infectious diseases;
- Neutrophilic surge - manifests itself against the background of acute infections, chronic inflammation;
- Short-term – suddenly appears and disappears;
- Basophilic – with nonspecific ulcerative colitis.
The process characterized by a change in the cellular composition of the blood, when leukocytes are elevated, is called leukocytosis. For a child, elevated leukocytes in the blood can serve as a sign of two groups of conditions: physiological and pathological. Therefore, in addition to the study, they carefully collect the analysis and take into account age.
Preparing for analysis
The cellular composition of blood is the most sensitive to all external factors, therefore, in order to obtain the most reliable results, it is necessary to properly prepare the child for the donation of biomaterial. Preparation rules:
- the biomaterial must be donated strictly on an empty stomach; at least 6 hours must pass between the last meal and the donation procedure;
- It is necessary to give the baby clean, non-carbonated water. This will reduce the risk of hemolysis in vitro, and will also greatly facilitate the collection of biomaterial;
- limit physical and emotional stress, which changes the functioning of the nervous and endocrine systems.
Parents often ask how they take blood for general analysis from children? For a general blood test and for calculating the leukocyte formula, venous blood (collected from the cubital vein in the bend of the elbow, in newborns - from the vein of the head) or capillary blood (taken from the ring finger) is suitable. The number of white blood cells is determined by flow cytometry. The execution time for private and public laboratories does not exceed 1 day.
Physiological causes of increased white blood cells
An increased level of leukocytes in the blood for a child may be a sign of physiological conditions that are caused by reasons such as:
- Taking a bath, both hot and cold, before performing medical procedures.
- Physical activity. Therefore, before the analysis, it is better to refrain from active games with the child, which can increase the amount of formed elements in the blood.
- Recent feeding. This is due to the fact that food entering the stomach increases the number of white blood cells. The highest rate is observed after eating. In addition, their number may fluctuate throughout the day. That is why there are certain preparation requirements before donating blood.
- Carrying out physiological procedures: x-rays, fibrogastroduodenoscopy.
- Fear. Before visiting the laboratory, it is necessary to distract the child from sad thoughts and not focus on the procedure. A large number of white blood cells can even be associated with the child’s crying before the test.
Appointment with a doctor after receiving the results
The pediatrician who referred for the study deciphers the microscopy results. A one-time low WBC reading usually does not cause concern to the doctor. If leukocytes are low, a repeat test is prescribed.
Persistent leukopenia is a clinical sign of disorders that cause the development of serious diseases. In this case, the child needs to be examined. Additional laboratory blood tests are performed on an outpatient or inpatient basis:
- serological tests to detect viral infections;
- biochemistry (liver enzymes and bilirubin are important);
- analysis of vitamin B12 concentration.
Additionally, microscopy of urine and feces and hardware diagnostic procedures are prescribed. If bone marrow pathology is suspected, a myelogram is performed. Leukopenia is not a disease, but its consequence. Symptomatic manifestations indicate developing diseases. The main symptoms of viral infections, for example, include:
- febrile (38-39℃) body temperature;
- weakness and lethargy (babies become capricious);
- sleep disturbance;
- skin rashes;
- lacrimation;
- rhinitis.
Normal levels of leukocytes in the blood
The condition may be accompanied by signs of intoxication (vomiting, nausea, diarrhea).
Why are leukocytes elevated: possible diseases
In some cases, indicators exceed acceptable values due to a pathological process. The reasons for this may be:
- Worm infestation. Any intestinal parasites (worms are more often detected in children, especially if they have cats/dogs and live in their own home) provoke elevated leukocytes in the blood and a high level of eosinophils.
- Infection. To any invasion (bacterial, viral or fungal), the body almost instantly reacts with an increase in protective cells - leukocytes. In the first days of the disease, a maximum jump in this indicator is observed, but even after recovery (in the absence of symptoms), slight leukocytosis may persist for some time. Leukocytosis is characteristic of both common childhood infections (acute respiratory infections, acute respiratory viral infections, chickenpox, rubella, cystitis) and more severe pathologies (tuberculosis, hepatitis, brucellosis).
- Allergy. The entry of an allergen into the body immediately responds with leukocytosis. If inflammation occurs at the site of an allergic reaction (itching, swelling, redness), this immediately provokes additional production of leukocytes.
- Diseases of the spleen. The spleen is an organ for recycling outdated leukocytes. When it is damaged or splenectomy (operation to remove the spleen), significant, long-term leukocytosis is observed.
- Autoimmune disorders. The most serious causes of leukocytosis lie in the autoimmune aggression of leukocytes against the body's own cells. The failure that led to this pathological condition is observed in lupus erythematosus and rheumatoid arthritis.
- Endocrine pathology. For example, with hypothyroidism (insufficient thyroid function), basophilia is observed - an increase in the level of basophils.
- Blood loss, hemolytic anemia. A decrease in the number of red blood cells in the blood due to blood loss or anemia causes the bone marrow to work harder. At the same time, new (immature) leukocyte cells are also synthesized, so these conditions are almost always accompanied by neutrophilic leukocytosis.
- Oncology. A very important sign: very often with oncology, a large number of monocytes are found in the blood. Fluctuations in leukocytes from 0.1 to 300 x 109/l (from leukopenia to large-scale leukocytosis) are observed in leukemia, a cancerous degeneration of leukocytes.
In newborns, especially in the first weeks of life, a high level of leukocytes is explained by the fact that the fetus at first does not need its own immune system, having become accustomed to developing at the expense of maternal immunity. Along with breastfeeding, the mother supplies antibodies and other substances to the baby, thereby replacing the infant's immunity. Therefore, an excess of leukocytes in the analysis of newborn babies is a standard phenomenon, indicating insufficient maturity of their immunity.
Leukocyte formula
Leukocytes are a group of cells, united by a common name, and belong to the immune system. Shaped cells not only have different structures, but also perform different functions. For example, lymphocytes act to protect the child’s body during a viral infection, and neutrophils act to fight bacteria.
Leukocyte formula - the ratio of all leukocytes, expressed as a percentage, consists of:
- Neutrophils;
- Eosinophils;
- Lymphocytes;
- Monocytes;
- Basophils.
A clinical blood test contains data on the number of white cells, and the leukocyte formula will tell you about their percentage.
A high level of white blood cells in the blood indicates the presence of an infection in the body, but thanks to the leukogram you can determine its type:
- Neutrophilia (there are many neutrophils in the blood) with general leukocytosis indicates a bacterial infection.
- In cases of viral etiology, lymphocytosis is observed in the blood.
- An increase in eosinophils and leukocytes is characteristic of helminthic infestations or allergic diseases.
- Monocytosis is observed in prolonged and indolent infections, such as tuberculosis. An increase in monocytes is a specific sign of infectious mononucleosis.
The main reasons for the increase in leukocytes in the blood of children, table:
| Diseases | Blood counts |
| Neutrophilia, increased ESR |
| Monocytosis, increased ESR |
| Eosinophilia, increased ESR |
| Lymphocytosis, increased ESR |
| Increased number of basophils |
What diseases do elevated rates indicate?
The level of ESR and eosinophils in children is higher than normal:
- helminthiasis;
- allergies to medications;
- bronchial asthma;
- dermatitis caused by allergies;
- oncological diseases.
The number of neutrophils and the ESR rate are higher than normal:
- meningitis;
- sepsis;
- pneumonia;
- angina;
- pyelonephritis;
- abscess;
- inflammation of the appendix.
An increased number of basophils in the blood is a rare phenomenon that indicates:
- lymphogranulomatosis;
- some types of leukemia;
- thyroid diseases;
- allergic reactions.
The number of monocytes and ESR rate are higher than normal:
- lupus erythematosus;
- pulmonary tuberculosis;
- syphilis;
- brucellosis;
- leukemia
Lymphocytes and ESR can be elevated when:
- measles;
- mononucleosis caused by infection;
- cytomegalovirus;
- flu;
- ARVI;
- whooping cough;
- rubella;
- hepatitis;
- tuberculosis.
Important: upward deviations of lymphocytes from the norm for children under 5 years of age may be physiological. To confirm the possible cause, additional testing is necessary.
Dangers of Increased White Blood Cells
Leukocytosis does not pose a health hazard, according to Dr. Komarovsky, if its occurrence is associated with physiological reasons. This sign in some cases indicates a certain disease that negatively affects the quality of life and leads to complications. The main place is given to tumor processes, which can be asymptomatic for a long time and are often discovered by chance during a routine examination.
What symptoms might bother a child?
Leukocytosis itself does not manifest itself with any symptoms, but the pathological conditions that cause it cause disruptions in the body and are manifested by the following symptoms:
- Stomach ache;
- General weakness;
- Increased sweating;
- Lack of appetite;
- Temperature increase;
- Increased fatigue;
- Dizziness;
- Bleeding.
If a child older than one month has at least one of the listed symptoms, you should definitely consult a doctor and conduct a laboratory blood test.
Manifestations of leukocytosis
An increase in the number of leukocytes does not refer to an independent disease, but the symptoms associated with its appearance reflect the pathology that has appeared in the child. These include:
- dizziness;
- headaches;
- weakness that remains after rest;
- increased body temperature;
- disturbance of appetite and sleep.
In some children, leukocytosis does not manifest itself in any way and for this reason you should visit the pediatrician on the days when a preventive examination is scheduled.
What to do and how to treat?
To reduce the level of white blood cells, you first need to find out the cause of their appearance and make a diagnosis. Leukocytosis itself is not a disease, but only a consequence of some cause that can only be determined by a competent specialist.
Treatment may vary depending on the cause:
- non-steroidal anti-inflammatory drugs are prescribed for inflammatory processes;
- antibiotics are used for viral and infectious diseases;
- a diet is prescribed if deviations are caused by malnutrition;
- antimicrobial ointments or spray are used to treat injuries and tissue damage;
- in case of oncology, treatment is selected individually;
- antihistamines relieve the effects of allergic changes;
- if a sharp increase in leukocytes was caused by the drug, reduce its dosage or cancel it.
Physiological leukocytosis does not require treatment. You need to take the test again if there were violations in preparation for it (for example, eating).
What to do in case of deviations
Any deviation of leukocytes from normal values (up or down) requires diagnostics to clarify the causes of this condition with further prescription of treatment.
How to reduce
In the presence of infectious diseases, anti-inflammatory drugs and antibacterial drugs are prescribed. If the increase is caused by allergic reactions, additional tests are taken to determine the irritating substance (allergen). Antihistamines are prescribed to relieve symptoms.
Important information: What do low platelets in the blood indicate during pregnancy (increasing foods)
If the increase in the concentration of cells occurs as a result of damage to the skin, the use of topical antimicrobial drugs is prescribed. The choice of one or another medication is made by the doctor individually in each clinical case.
If there are no obvious reasons leading to an increase in white blood cells, perhaps the diet is incorrectly selected, which is dominated by foods high in protein, which is why the liver and spleen are under excessive stress. In this case, it is necessary to exclude fried and fatty foods, salty foods, marinades, and spicy foods from the menu.
How to increase
If the number of leukocytes is insufficient, the child is examined to identify possible reasons for this. If no obvious pathologies are detected, the child will be periodically examined by a doctor and a blood test will be prescribed.
You can increase the number of leukocytes by adjusting your diet. The diet should include foods enriched with potassium, vitamins E and C, and zinc. Particular attention should be paid to products high in omega-3 acids; they are present in sufficient quantities in walnuts and red fish. Omega-3 acids protect cells from pathogenic microflora.
To compensate for the lack of vitamin E, you need to introduce cabbage and spinach, turkey and chicken meat into your diet. These products are enriched with essential substances that protect cells and restore their functioning. If the concentration of leukocytes is low, the menu should regularly include:
- eggs;
- Cod liver;
- lean white meat;
- seafood;
- red fish;
- fermented milk products.
If the diet helps normalize the level of white cells, in the future you will need to periodically donate blood for testing to monitor this indicator.
Prevention
In order to prevent an increase in the level of leukocytes in the blood of a child, it is necessary to adhere to the following preventive measures:
- Avoid hypothermia;
- Monitor the child’s health;
- Enrich your baby’s diet with vitamins and macroelements (as a last resort, consult a doctor about the possibility of taking multivitamin preparations);
It is also worth remembering that the pathology can be asymptomatic. That is why it is important to regularly visit the doctor and have the little patient’s blood tested.
Symptoms
When the rate of leukocytes in the blood of children is increased or decreased, this affects the child’s well-being. Parents need to be very careful, since any deviation has nonspecific and mild external manifestations. The specificity also lies in the fact that symptoms may go unnoticed due to the fact that signs of the underlying disease come to the fore.
However, leukocytosis can be suspected when the following conditions appear:
- constant fatigue and weakness;
- loss of appetite;
- increase in temperature indicators;
- dizziness and headaches;
- profuse sweating;
- sleep problems;
- muscle and joint pain;
- weight loss;
- frequent mood changes;
- increased moodiness and tearfulness in infants;
- problems with concentration;
- decreased physical activity.
Symptoms of leukopenia, in turn, are presented:
- increasing temperature;
- increased heart rate;
- severe chills;
- migraine;
- body aches;
- causeless anxiety;
- weakness and weakness;
- increased volume of lymph nodes and spleen;
- hoarseness of voice;
- aversion to food;
- exhaustion;
- bleeding gums.
It should be remembered that the above are only general symptoms, which will necessarily be supplemented by specific signs of a particular underlying ailment.
Decoding the formula
The number of leukocytes directly depends on the age of the child. For a one-year-old baby the following indicators are normal (in%):
- total white blood cells - 6−12;
- neutrophils - 0.5−4;
- basophils - 0−1;
- eosinophils - 0.5−7;
- monocytes - 2−12;
- lymphocytes - 38−72.
An increase in the number of neutrophils in the blood indicates the entry of pathogenic components into the body. This indicates that the body is actively fighting the infection. In addition, the level of neutrophils exceeds the permissible norm in the presence of cancer of the bone marrow, acute pancreatitis, and burns.
Lymphocytes are very sensitive to viruses entering the body. Their number increases with:
- chicken pox;
- cytomegalovirus;
- rubella.
The number of lymphocytes increases in the presence of cancer, when the immune system is trying with all its might to eliminate mutating cells. The number of monocytes in the blood increases when:
- acute infections;
- cancer of the lymph nodes, red bone marrow, stomach, ovaries;
- connective tissue pathologies;
- lung diseases.
The number of eosinophils increases when exposed to allergens, which can provoke allergic shock. Sometimes these components increase when infected with parasites. The number of basophils increases extremely rarely; this can happen due to allergies or cancer.
Necessary tests
The number of leukocytes can be determined by taking a general blood test. If the result obtained is not normal, the doctor prescribes:
- peripheral blood smear examination;
- complete blood test.
The listed tests are necessary to identify the number of eosinophils, monocytes, and basophils. If cancer is suspected, a biopsy of the lymph nodes, spleen, bone marrow, and liver structures is taken.
The baby's first blood test is done 2-3 days after he is born. Afterwards, blood is taken at 3 months and one year of age. Doctors recommend donating blood annually until the age of 6. This is necessary to prevent various diseases, even if the baby is healthy. This reveals:
- level of red blood cells, platelets;
- hemoglobin indicators;
- hematocrit number;
- blood clotting rate.
Blood is drawn from a vein or finger. In infants, biological material for analysis is taken from the heel.