Share
Parents should not be alarmed if their newborn has elevated leukocytes in the blood. This phenomenon most likely will not be a sign of something out of the ordinary. In many cases, it turns out that there is no reason to worry at all. But you still need to figure this out so as not to miss something more serious, which indicates the development of some disease.
Blood, like any tissue, consists of cells, some of which are called erythrocytes, the other part - leukocytes. Their number does not stand still; it is constantly changing, especially in newborns. Fluctuations in the number of blood cells are influenced by many factors - the child’s character, his lifestyle, immunity, etc. When white blood cells increase in size, it is called leukocytosis.
However, this does not mean at all that something terrible happened to the child, and leukocytosis is not a diagnosis at all. Some immune changes in the body have caused this reaction in the body, so the causes of leukocytosis may or may not be serious.
The norm of leukocytes in the blood of a newborn
Leukocytes in the blood of a newborn may be elevated in the first days of his life. The fact is that he plunges into a new world for him, where thousands of bacteria attack him. It is still difficult for the child’s body to adapt to working in this mode and he begins to protect himself in all possible ways.
In healthy adults, the level of white blood cells is not the same as in a newborn. In a small, newly born child, in one liter of blood the number of white cells can be about 24 billion leukocytes. A little later, after 6 months or more, the norm of leukocytes in the blood of a newborn drops to 5-9 billion. This is the norm in adulthood. If these values are exceeded, it is called leukocytosis.
Premature babies also often have elevated white blood cell levels. But usually after a while everything returns to normal.
Causes of elevated leukocytes in the blood of a child
There are many factors that provoke leukocytosis in a newborn baby. It is impossible to say with certainty that the cause was illness. Even in a healthy baby, white blood cells increase for a number of reasons. In this case, we are talking about physiological leukocytosis, which does not require therapeutic measures and goes away on its own after a short period of time. The following may influence its occurrence:
- Strong emotional outburst. Stressful conditions accompanied by frequent crying of the baby.
- Increased physical activity shortly before submitting the material for analysis.
- After a warm bath, the concentration of white blood cells increases. Prolonged exposure to the sun has the same effect.
These points are taken into account on the day before the test. An increased number of white blood cells is observed after eating, and the consumption of foods with high levels of protein has a particularly strong effect. The natural change in their concentration, provoked by these factors, is not dangerous to health and is the norm in children, as it quickly returns to the old value.
If leukocytosis is pathological, it is necessary to identify what disease caused this process. High leukocytes in an infant will result from:
- viral infections (hepatitis, ARVI, bronchitis and others);
- purulent infections (appendicitis, meningitis or otitis media);
- malignant neoplasms;
- chronic inflammatory processes, for example: arthritis or intestinal inflammation;
- allergic reactions;
- autoimmune diseases;
- fungal diseases;
- burns and injuries.
The reason why a newborn child has elevated white blood cells may be a previous operation, including the removal of the spleen. During the recovery period, this is a normal reaction of the body.
Leukocytes: description and functions
Functions of leukocytes in the body
Before moving on to why a newborn baby may have elevated white blood cells in the blood, it is necessary to learn in more detail what these cells are and why they are so important.
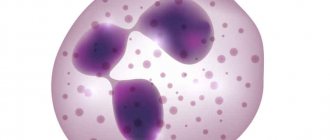
Leukocytes, or as they are commonly called, white blood cells (which are actually transparent), protect the human body from external influences. A leukocyte can reach a size from 6 to 20 microns, and all of them can be of different shapes, both regular round and uneven.
There are many white blood cells in the human body, each of which can perform different functions. For example, some protect the body from antigens, others from bacteria and microbes, others from dead cells, etc.
If there are no foci of inflammation in the body, then the leukocytes will be within normal limits.
But if bacteria or microbes enter the newborn’s body, or, for example, the child is injured during childbirth, then they will increase sharply, which can be seen from the results of a blood test taken from a finger.
Diagnosis and therapy of leukocytosis
Only a specialist can make an accurate diagnosis of the baby by performing blood tests and other tests. To carry out effective therapy, it is necessary to identify the cause that caused the increase in the level of leukocytes.
Examination of the baby
Leukocytosis can be detected in a newborn on the first day of his life, when blood is taken from the baby to determine his ability to adapt and the presence of diseases that developed in utero. A repeated examination, the so-called heel test, is performed on the 3rd–4th day of the baby’s life. Next, the diagnosis is carried out according to the blood sampling plan for prophylactic purposes. Such screening of the baby’s health allows us to identify various pathologies in the early stages, when, as is known, they are better treatable and entail fewer complications.
If the blood test shows a persistent excess of the leukocyte norm, additional examinations of the baby may be prescribed:
- echocardiography - allows you to identify congenital problems in the heart;
- MRI – is performed if there is a suspicion that a newborn has pathologies of the central nervous system, skeletal system, lungs, or abdominal cavity;
- Ultrasound of internal organs.
However, all these diagnostic methods are used only in extreme cases. Usually, to make a diagnosis, a visual examination of the baby, a general and detailed analysis of blood and urine, and monitoring changes in the baby’s health are sufficient.
Treatment of pathology
The physiological form of leukocytosis does not require any therapy - blood counts will return to normal after a while on their own. If any pathological form of the disease occurs, treatment cannot be avoided. Specific methods of control are selected taking into account the factor that caused leukocytosis. Therapy should mainly be aimed specifically at eliminating the underlying ailment in the newborn.
Depending on the type of leukocytosis and its cause, one of the following groups of drugs is prescribed:
- antibiotics - help suppress the infection that caused changes in blood counts;
- antiviral – allow you to stop viral infections;
- anti-inflammatory – fight inflammatory processes, help reduce the number of leukocytes.
- antihistamines - help prevent the risk of allergies, including to antibiotics;
- enterosorbents – cleanse the baby’s body of toxic substances and allow normalization of the digestive tract;
- chemotherapeutic - prescribed in difficult situations with the development of oncological processes.
When selecting and prescribing medications, the doctor must take into account the fact that the immune system of infants is not fully formed, and therefore is not able to fully protect the body from drug poisoning.
During treatment of the baby, parents are required to do the following:
- follow all doctor's recommendations;
- Do wet cleaning in the house every day and regularly ventilate;
- when breastfeeding, the mother needs to closely monitor her diet (it should be enriched with vitamins and minerals);
- change and monitor the cleanliness of the child’s bed linen and hygiene items in a timely manner;
- lead a healthy lifestyle with your baby, make every effort to strengthen the baby’s immunity;
- at high temperatures, ensure a full drinking regimen; drinking plenty of fluids will help avoid dehydration.
Prognosis and complications
Leukocytosis in children mostly responds well to treatment, the chances of a successful cure are 85–90%. The unfavorable outcome of the disease in most situations is due to the occurrence of an oncological process, which caused an increase in leukocytes in the blood.
In addition, without proper therapy, a baby may develop serious consequences:
- various blood diseases;
- heart disease;
- cardiovascular pathologies;
- hydrocephalus;
- extensive sepsis, which affects internal organs and tissues and disrupts their activity.
It is necessary to pay close attention to the baby’s health and monitor his well-being. With timely and correct treatment, dangerous consequences can be avoided.
If an increased number of leukocytes is detected in the baby’s blood, parents should not immediately panic and assume the worst. In children, quite often this condition is considered a variant of the physiological norm. However, you should not let the situation take its course; you should definitely consult with a specialist and, if necessary, undergo additional examinations.
Signs
Mild leukocytosis in newborns is asymptomatic. A pronounced increase in the level of leukocytes in the blood is accompanied by the appearance of the following symptoms:
- lethargy, lack of appetite and physical activity;
- slight increase in temperature;
- skin rash;
- periodic nosebleeds;
- fainting conditions;
- slower hair growth or hair loss;
- impaired coordination of movements;
- deterioration of the functions of the visual organs;
- rapid shallow breathing;
- muscle and joint pain, expressed by constant crying;
- weight loss with a normal diet.
Other symptoms of the pathological condition occur depending on the type of underlying disease:
- Intrauterine infection of the gastrointestinal tract. This disease is characterized by the presence of intestinal colic, increased gas formation and loose stools.
- Bacterial infection of soft tissues or internal organs. The pathology is accompanied by a pronounced increase in temperature, convulsions, and cyanosis of the skin.
- Viral infections. An increase in the level of leukocytes in the blood of an infant is accompanied by a feverish syndrome and the appearance of clear discharge from the nose and eyes. The condition poses a danger to a child under one year old, so timely elimination of the cause of leukocytosis is necessary.
Elevated leukocytes in children over one year of age
As the child grows, the reasons for the increased content of these blood cells in the blood become more diverse. The level of leukocytes in a child’s blood can vary from 6 to 17 percent from year to year. When he gets older, reaches three years, the spread decreases to 6.1-11.4%.
The physiological factors that cause the increase are the following:
high protein foods; nerves, stress; overheating or cooling.
If this is the reason, then the leukocyte level should recover within a maximum of three hours.
The child may also have pathological ones. Then the following factors are to blame:
- chronic and acute inflammatory diseases;
- purulent inflammation;
- tumors;
- leukemia (acute and chronic);
- exposure to toxic substances and heavy substances such as lead and mercury;
- tissue death;
- severe intoxication;
- acute infections (except for influenza, typhus, measles and paratyphoid);
- pathologies of the autoimmune type and a number of other problems.
In this case, prompt elimination of the pathology is necessary. Once it disappears, the increase in white blood cell levels will also disappear.
There are also several types of leukocytes - and their increase occurs for various reasons. An increase in the first type, neutrophils, which activate hematopoiesis, occurs when:
Another type of these blood cells are eosinophils. They occur when:
- blood diseases;
- allergic reactions;
- rheumatic diseases;
- ulcerative colitis;
- lung diseases.
When the problem is eliminated, the composition of the blood also normalizes, high leukocytes in the child’s blood will become normal.
If it is not clear what caused the sharp and stable increase in the level of leukocytes, it is necessary to conduct a comprehensive examination. There is a high probability that there is no dangerous situation, that the reason for this change is temporary and will soon come to an end.
There are coincidences that can affect blood test readings, such as taking antibiotics coupled with hunger or other physiological stress.
But even if the problem is more significant, in most cases it can be dealt with fairly quickly.
It is important to remember that in the first week of life and at 4-5 years, an increase in the level of leukocytes occurs constantly, this is the norm, and therefore at this age you should not take any measures to normalize them. In other cases, a good pediatrician will tell you what examination to undergo - and what diagnosis caused the deviation from the norm, why the leukocytes in the child’s blood are elevated in your particular case
In other cases, a good pediatrician will tell you what examination to undergo - and what diagnosis caused the deviation from the norm, why the leukocytes in the child’s blood are elevated in your particular case.
Leukocytes are also known as white blood cells, although in reality they are colorless. In the body, they perform a protective function, that is, they recognize harmful microbes and bacteria and literally “attack” them. The reaction of leukocytes is instantaneous, thanks to the blood vessels they easily spread throughout the body. These cells are produced:
- spleen;
- bone marrow;
- tonsils;
- lymph nodes.
On the first day of a newborn’s life, the level of leukocytes in his blood ranges from 8.5 to 24.5 units, this is due to the immaturity of the infant’s immune system. This indicator persists for several weeks, but gradually it decreases and by the age of six months it should be in the range of 5.5–12.5 units. Exceeding these values is called leukocytosis.
It is worth remembering that the content of leukocytes in the blood of an infant is not constant; their concentration can change not only daily, but also every hour. This indicator is influenced by many factors, even the baby’s nutrition and activity during the day.
However, a stable and significant excess of the normal level of white cells in the blood indicates the development of leukocytosis. This condition requires diagnosis, clarification of the causes of its occurrence and further therapy. Without appropriate therapy, a serious complication may occur.
Why can a baby's white blood cell count be significantly elevated in a blood test?
Children often have to have their blood tested. This is done during routine examinations or in case of illness. The value of one of the main indicators, leukocytes, can tell a lot about the child’s condition. To understand why they deviate from the norm, you need to know the basic functions of “white” blood cells.
Child
Leukocyte concept
Leukocytes are “white” blood cells that guard the immune system. Their main task is to detect harmful bacteria and viruses and neutralize them. They also react to foreign bodies and waste.
Despite the definition, white blood cells are pink-violet when examined closely under a microscope. They actively move throughout the body, detecting and identifying dangerous bodies. Leukocytes move freely through the walls of capillaries to reach pathogenic particles.
Note! “White” blood cells rush to places where dangerous viruses and bacteria accumulate, they destroy them along with infected cells. As a result, pus is formed, these are the leukocytes that have done their job.
Types and functions of leukocytes
Blood in the urine of a child - possible causes in infants
The following types of leukocytes are distinguished:
- Neutrophils. This is the largest group. Neutrophils are found in tissues and form a reserve, located in the bone marrow. As soon as the body needs them, they are activated. They are the first to arrive in places where germs and toxins accumulate. Moving quickly throughout the body, they strive to destroy infected cells and foreign particles. One neutrophil kills about 20-30 microbes; it acts on them with its own enzymes and bactericidal substances. If it dies, the proliferation of bacteria does not stop;
- Eosinophils. This is a small group of leukocytes. They also move freely throughout the body and penetrate to the place of danger. But, compared to neutrophils, there are not so many of them, so their role is not so significant. When allergic reactions occur in the body, mast cells are activated, and eosinophils are sent to destroy them. Therefore, their number increases with infection with worms and allergies. It also destroys basophils, another type of white blood cell. When fighting mast cells, histamine is released, which provokes allergy symptoms. If it enters the blood in large quantities, swelling of the mucous membranes occurs, for example, and rashes appear on the skin. It is eosinophils that are called upon to destroy dangerous histamine;
- Basophils. A type of white blood cell that produces histamine, which helps dilate capillaries, which is necessary for cell and tissue healing. Basophils also secrete heparin, which creates obstacles to blood clotting in the area of inflammation. Their number increases with allergies, stress and inflammation;
- Monocytes. This is the main active force against microbes. They work several times more efficiently than neutrophils in this direction. They are also able to survive and remain active in an acidic environment. This is another advantage over neutrophils, which die under such conditions. They not only fight microbes, but also cleanse the body of dead neutrophils;
- Lymphocytes. This type of leukocyte, after entering the tissue, is able to return back to the blood. They live for quite a long time, unlike other species, which often last for several days.
Leukocytes under a microscope
Leukocyte formula
Why can bleeding come from the ear of a child under one year old when cleaning?
The leukocyte formula characterizes the values of all types of leukocytes. In this case, not only their absolute values are determined. It is important what percentage each type occupies in the total volume of blood cells.
Normal values for a child
Normal values for a child depend on his age. So the indicators on the first day of life and a month later are very different.
Normal values of leukocytes in a child under one year old
IndicatorNewborn1 month6 months1 year
| Leukocytes, *〖10〗9/l | 8,5-24,5 | 6,5-13,5 | 5,5-12,5 | 6,0-12 |
| Band neutrophils, % | 1-17 | 0,5-4 | ||
| Segmented neutrophils, % | 45-80 | 15-45 | ||
| Eosinophils, % | 0,5-6 | 0,5-7 | ||
| Basophils, % | 0-1 | |||
| Lymphocytes, % | 12-36 | 40-76 | 42-74 | 38-72 |
| Monocytes, % | 2-12 |
Changing indicators allows you to evaluate the processes occurring in the body and determine the presence of a viral or bacterial infection.
There is such a thing as a shift in the leukocyte formula:
- It shifts to the left if the number of band neutrophils increases. This means that the body is under the influence of infection;
- The formula shifts to the right, respectively, with a decrease in band neutrophils and an increase in segmented neutrophils. This may indicate problems with the kidneys and liver.
In any case, test results alone do not provide a complete picture of the child’s condition. After an examination, in particular, examining the throat, palpating the lymph nodes and talking with the parents, the doctor will prescribe additional tests to make an accurate diagnosis and prescribe treatment.
Usually, the first step is to undergo a general urine test to rule out a urinary tract infection and monitor kidney function.
Doctor visit
Note! Only a specialist who understands what could increase and decrease the main indicators can decipher the test results. He will immediately determine whether we are talking about a dangerous disease or whether there is no need to worry.
Diagnosis of leukocytosis
Why does a child under one year bleed from the nose?
With leukocytosis, the number of “white” blood cells increases compared to their normal value. The increase may be slight or severe.
Thus, the level of leukocytes increases after eating or during exercise. These are physiological processes and do not pose any danger. After a short period of time, the indicators return to normal. If such growth is considered as a pathological reaction of the body, we are talking about an inflammatory process.
The famous pediatrician Komarovsky recognizes the need for a general blood test. It, first of all, allows you to determine the nature of the disease, bacterial or viral. This is the basis for subsequent treatment.
If the body is attacked by bacteria, then it will be difficult to cope without antibiotics, but they have no effect on viruses. Therefore, their use does not make sense, just like the use of antiviral drugs. Immunity to them is usually developed on days 6-7, and the body copes on its own.
If this does not happen and the disease develops, most likely a bacteria has joined.
Possible symptoms in a child
When a child's white blood cell count is elevated, it not only indicates that he or she is sick, but also that the immune system is active. The body's defenses began to fight pathogenic microorganisms.
The following symptoms may indicate leukocytosis in a child:
- Increased body temperature without identifying the cause;
- Weakness and dizziness;
- Indigestion, lack of appetite, weight loss;
- Nausea, vomiting;
- Headache and migraine;
- Aches in joints and muscles;
- Sleep disorder, most often insomnia. The child becomes anxious and shudders;
- Increased sweating;
- Moodiness and irritability.
An infant will not be able to talk about his health; parents only have to guess about existing problems.
What should alert you is that the baby’s behavior has changed, he is not the same as before. When this happens once, and then the baby becomes himself again, then there is no need to worry.
If the condition drags on, behavior and well-being worsen, then you need to consult a pediatrician.
Upset child
We must remember! In a baby, a temperature of up to 37.5° is considered normal. At the same time, he is calm and active, no unpleasant symptoms are observed. This is often due to uncomfortable indoor conditions and too warm clothing. If the temperature is higher and the baby begins to act up, you should consult a doctor.
How to donate blood correctly
You need to donate blood on an empty stomach: the baby should not eat for at least two hours before the procedure.
Otherwise, this will not only affect the results of the study, but may spoil the material itself - the baby’s blood may clot, then the sampling will have to be repeated another day.
In the morning, you can offer your child only water, in a small volume. It’s better to take a snack with you and make your baby happy immediately after the procedure.
Note! When it is not possible to donate blood on an empty stomach, then when you repeat the analysis, you need to do it at the same time and it is better not to change the laboratory. The main thing is to create the same conditions in order to track changes in indicators.
It is better to carry out the procedure the first time so that the baby does not experience unnecessary stress, which can also affect the test results. Strong emotions, like physical activity, lead to an increase in white blood cells.
If a child is undergoing drug therapy, the doctor must be notified about this. He will determine whether this will affect the result, or advise you to postpone taking the medication until after the test is taken.
The younger the child, the more difficult it is to explain the significance of the procedure to him, so he will have to be distracted. It is much more difficult to take blood from a crying baby; he pulls out and squeezes his hands, so you have to extract the material drop by drop. As a result, the process is delayed, and the baby may become hysterical out of fear.
If the baby is cold, you need to warm his hands to speed up the blood collection process.
Blood collection
It is necessary to explain to children from childhood where they are going and why. You cannot scare babies with doctors and white coats; they must understand that people work for their benefit, their task is to help and treat.
What does an increase in leukocytes indicate?
If a child’s blood has elevated leukocytes, it means that the body has detected a threat and has begun to fight it. Perhaps he can cope on his own, but often it is necessary to turn to drug therapy to get rid of inflammation and normalize the child’s condition. Based on the indicators, the doctor will determine what caused leukocytosis in the child’s blood:
- High white blood cells usually indicate the presence of a bacterial infection, if at the same time the ESR increases and hemoglobin decreases. The minimum acceptable value of the latter indicator is 110 g/l. Sometimes, to raise it, you have to take iron supplements. In this case, anemia is diagnosed, which is often accompanied by a decrease in platelets. The erythrocyte sedimentation rate should be below 10 mm/hour. If all three indicators: white blood cells, hemoglobin and ESR are not normal, then most likely the doctor will prescribe antibacterial therapy;
- By growing neutrophils, the body responds to the spread of a bacterial or fungal infection. If the indicators are very high, then they think about pancreatitis and bone marrow diseases. Also, such changes can accompany severe burns and purulent processes. After an illness, neutrophils may be reduced if they have not had time to recover as a result of the fight against harmful bodies. In this case, an increase in lymphocytes is usually observed;
- High values of monocytes signal the presence of a viral infection and often indicate the development of herpes-type diseases;
- An excess of eosinophils occurs with helminthic infestation and allergies. For example, in babies with bowel disorders, without other symptoms, cow's milk protein intolerance can be suspected;
- There is practically no growth of basophils in children. It accompanies anaphylactic shock, gastric ulcers;
- High lymphocyte counts confirm the spread of the virus. This happens with childhood infections such as measles, rubella, and chickenpox. Whooping cough and tuberculosis also cause their growth. Most often, an increase in the number of lymphocytes is associated with the development of an adenoviral infection, which can affect the respiratory tract, provoke conjunctivitis, and upset intestinal function.
Note! All indicators must be assessed together. The value of one of them cannot make a diagnosis.
When a child’s leukocytes are elevated, it is imperative to look at other indicators. You need to connect them so that an accurate picture appears before your eyes; only a doctor can do this.
Preventive measures
Preventive measures should be aimed at restoring and strengthening the child’s reduced immunity. These include:
- A nutritious and healthy diet;
- Walks in the fresh air and sufficient activity of the child during the day;
- Comfortable home conditions, maintaining optimal temperature and humidity;
- Drinking the age-appropriate amount of fluid;
- Hardening the body. This does not mean you need to pour ice water on your baby. You can, for example, bathe him in a cool bath, but do it gradually. Starting with a comfortable water temperature for the baby, lower it by one degree every day. For each age group, its minimum values are determined. So, children under one year old should not be bathed in water whose temperature is below 26-27 degrees. After 12 months, you can take cooler baths, but continue to make sure that the water is warmer than 23-24 degrees.
Bathing
To monitor the child’s condition, you need to come to the pediatrician for routine examinations in a timely manner and take the necessary tests. If elevated leukocytes are detected in a toddler and treatment is prescribed, then a re-examination can be carried out after 10-14 days. If it was not possible to reduce the indicators, then it is necessary to change the treatment tactics, based on new results.
White blood cells in a child’s blood increase when the immune system begins to work actively. It fights inflammation by destroying pathogenic organisms and particles. His actions are not always enough for the baby to recover. A general blood test will tell you how to help the immune system and not harm the child.
Source: https://kpoxa.info/zdorovie-pitanie/povysheny-lejkocity-u-rebenka.html
Reasons for low leukocyte levels
A decrease in the number of white cells in the blood is called leukopenia. This deviation is rare in newborns. A lack of leukocytes indicates that the process of their production by the bone marrow is slowing down. An examination of the child is required to identify the causes of leukopenia.
- HIV infection transmitted from mother to fetus. If during pregnancy a woman took medications to prevent infection of the fetus, the number of leukocytes in an infant may decrease relative to the norm. Infection of the fetus is possible with premature rupture of intrauterine fluid, with a prolonged stage of the disease, with early birth and breastfeeding.
- Toxoplasmosis is a parasitic disease transmitted from animals. Damage to the fetus occurs if the mother has been infected and there are no antibodies to the disease. During pregnancy, all women are required to take a blood test for toxoplasma, and doctors also advise avoiding contact with animals. Signs of the disease may be completely absent in a pregnant woman, but may cause severe visual and auditory disorders and nervous disorders in the child.
- Cytomegaly is a viral infectious disease transmitted from mother to fetus. The mother may not show signs of illness. Often, infection during pregnancy provokes premature birth, miscarriages, fetal death and developmental defects. The severity of complications depends on the stage of pregnancy at which the infection occurred, the timeliness and correctness of therapy.
- Listeriosis is an infectious disease caused by bacteria of the genus Listeria. The bacterium is transmitted to the fetus in utero through the umbilical vein and provokes an inflammation process. In this case, the mother may not know about the infection. The infection process occurs through milk and raw eggs.
In addition to the listed reasons for the decrease in the level of leukocytes, it can also be noted that a pregnant woman takes medications that help reduce white cells and slow down the process of their production. In this case, a deviation from the norm is not a pathology and the leukocyte level will gradually recover.
Leukocytes are important blood cells that perform a protective function in the body of both adults and children. If their level deviates from the norm in infants, a thorough examination is required, which will allow timely treatment to begin and avoid the development of complications. It should be noted that during pregnancy, the mother needs to take responsibility for her health. Following doctors' recommendations will help avoid undesirable consequences for the unborn child.
How to bring your white blood cell count back to normal
The choice of treatment method depends on the reason why the number of leukocytes in a newborn increases. The doctor should pay attention to the general condition of the child.
Increased values
With physiological leukocytosis in the blood of a newborn, the indicators return to normal after the cessation of the influence of the stimulus. In other cases, drug treatment is prescribed, the regimen of which includes the following drugs:
- Antibiotics (Ampicillin, Cefazolin). Antibacterial therapy is aimed at eliminating foci of infection that provoke increased production of leukocytes. Injections are given every 8 hours for a week.
- Interferons. Genferon and Viferon have antiproliferative and immunomodulatory effects. They normalize the immune system and eliminate viral infections. The drugs are used in the acute course of the disease, they can be combined with other drugs.
- Non-steroidal and hormonal anti-inflammatory drugs (Hydrocortisone, Nimesil). The drugs stop the development of the inflammatory process, normalizing the functioning of the bone marrow.
- Antihistamines (Fenistil, Zyrtec). Used for leukocytosis of allergic origin.
- Chemotherapy drugs (Methotrexate). Prescribed when there is a marked increase in the number of white blood cells, which poses a danger to the child’s life.
Important information: What do elevated white blood cells mean in a child’s blood test?
Additionally, plasmapheresis (purification of blood from toxic substances) and leukopheresis (removal of leukocytes) are performed.
Decreased performance
When the number of leukocytes decreases, the following therapeutic methods are used:
- temporary creation of sterile conditions for the child to live;
- eliminating foci of infections;
- cessation of radiation and administration of chemotherapeutic agents;
- timely treatment of viral infections;
- administration of antifungal agents;
- stimulation of white blood cell production;
- transfusion of donor leukocyte mass;
- administration of medications that normalize metabolic processes (Methyluracil, Pentoxyl);
- carrying out detoxification therapy (this means that toxic metabolic products and poisonous substances are removed from the child’s body and blood);
- administration of drugs that stimulate the functions of the hematopoietic system (Filgrastim).
Norm of leukocytes in a child
You should not compare a child’s blood counts with those of an adult. As the baby grows (from birth to 10 years), the number of leukocytes changes significantly. Normal age indicators of leukocytes (x109/l):
- 1 day - 8.5 - 24.5;
- 1 month - 6.5 - 13.8;
- 6 months – 5.5 – 12.5;
- up to 1 year – 6.0 – 12.0;
- 1-4 years - 6.1 - 12.0;
- 4-10 years – 5.2 – 11.4;
- from 10 years – 4.5 – 10.0.
Physiologically, the ratio of the leukocyte formula also changes (determined in%):
- stab: in newborns - 1 - 17; in 1 month – 1 year – 0.5 – 4.0; older – 0.5 – 5.0;
- segmented: in newborns - 45 - 80; up to 1 year – 15 – 45; up to 6 years – 25 – 60; up to 12 years – 35 – 65;
- eosinophils: in newborns - 0.5 - 6.0, then 1 - 4;
- basophils: in any age group 0 – 1;
- monocytes: at any age 4 – 8;
- lymphocytes: in newborns - 12 - 36; 1 month – 49 – 76; 6 months – 42 – 74; 1 year – 38 – 72; 1 – 6 years old – 26 – 60, older – 24 – 54.
Sometimes, to clarify the diagnosis and determine the factor that provoked leukocytosis, it is important to record the deviation of certain types of leukocytes. Therefore, along with determining the total number of leukocytes in children’s blood, the leukocyte formula is often calculated
Symptoms and diagnosis
The main symptoms of elevated white blood cells in infants:
- The first sign of the disease is an increase in temperature (37-39°C);
- Lethargy, lack of age-appropriate activity;
- Poor appetite, breast refusal;
- Weight loss;
- Excessive sweating, lack of physical activity;
- Disorders of urination (either frequent urges or very rare ones), changes in the color of urine (too dark or colorless), its quality (sediment appears);
- Chills;
- Attacks of nausea, vomiting.
Necessary tests and examinations for leukocytosis:
- Repeated blood test (which can be compared with the previous one to track changes);
- Ultrasound examination of the abdominal cavity for suspected pathologies of internal organs;
- Tomography scan (MRI);
- Echocardiography, for further examination when there is a possible risk of cardiac dysfunction.
Early signs of low white blood cell counts in infants include:
- Feverish state, increased temperature;
- Anxiety, tearfulness and moodiness;
- Sleep disorders (short, restless sleep);
- Refusal to feed;
- Attacks of nausea, vomiting;
- Enlarged lymph nodes, spleen.
Diagnostic measures:
- Blood tests (biochemistry, serological);
- Liver tests that detect the presence and types of hepatitis, bilirubin, transaminases;
- Blood tests for folic acid, B12;
- Bone marrow aspiration with cytological examination of the material. The most informative procedure to determine the nature and degree of development of leukocytopenia;
- Lymph node biopsy;
- Radiography;
- MRI;
- Ultrasound of the gastrointestinal tract.
Leukocytes in the urine of an infant
A clinical urine test quite informatively illustrates the general condition of the body and the presence of various pathologies. Determining the total number of leukocytes in the urine of an infant greatly facilitates diagnosis and subsequently helps in the treatment of identified diseases.
The normal level of leukocytes in the urine of an infant varies significantly depending on the sex of the child. For girls, a normal indicator is considered to be a leukocyte count of 8-10 cells per field of view, for boys 5-7. The difference is explained by differences in the anatomical structure of the genitourinary system in children of different sexes. In girls, such cells are formed more often as a result of the close proximity of the vagina and the entrance to the urethra, since in this case there is a high probability that the cells will enter the urine along with vaginal discharge, and not from the genitourinary system.
It is important to note that the inflammatory process is directly dependent on how many leukocytes are released during urination. The more of them are released, the more active the inflammation process is.
In addition, the transparency of the urine decreases, it becomes cloudy, and the sediment becomes more pronounced.
Leukocytes in a baby's urine appear as a result of infection entering his body. In this case, the action of protective systems is activated, which, among other things, includes inflammatory cells. Their action is capable of destroying, neutralizing and absorbing pathogenic bacteria, thus eliminating the causative agent of the disease. Thus, it becomes clear that the detection of leukocytes in the urine of an infant may indicate the following diseases:
- process of inflammation of the urinary tract. This could be cystitis or urethritis;
- inflammation of the external genitalia;
- stagnation phenomena caused by abnormalities in the structure of the urinary tract;
- violations of the rules of personal hygiene of the child, they may have forgotten to wash themselves or did it poorly before collecting material for analysis. This also includes the presence of diaper rash.
If an insufficient amount of material is collected for research, errors in the final results of the analysis may occur. A more reliable and accurate way to clarify the diagnosis is the Nechiporenko analysis, which shows the level of leukocytes per milliliter. This particular method can confirm or refute the presence of an infectious agent in the baby’s body. In order to identify it, culture is carried out on a nutrient medium.
Decoding the results
Deciphering the results of a general blood test helps to assess the condition of the body and identify indirect signs of pathologies.
Norm
If there are no infectious diseases or congenital defects, the baby's white blood cells will have a normal level. The average value for a healthy child is 9-30 billion/l. This is much higher than the norm for an adult patient.
Deviations
Deviations are considered to be both low and high leukocytes in a newborn.
The first category includes values below 9 billion/l, the second category includes values exceeding 30 billion/l.
A low level of leukocytes is rarely detected and does not have a significant effect on the child’s condition. Increasing the indicator should not go unnoticed.
Causes of high white blood cell count
The development of leukocytosis can be caused by various factors. Activation of the baby’s body’s defenses can be caused not only by pathological (diseases), but also by physiological (physiological stimuli).
Physiological leukocytosis
Leukocytosis provoked by physiological stimuli is not dangerous for the baby. The condition indicates the impact on the body of a completely healthy baby of a number of irritating factors that provoked an increase in the number of white cells. Physiologically caused leukocytosis does not require medical intervention; to eliminate it, you need to remove the irritating factor, which will lead to the restoration of normal leukocyte levels.
The main irritating factors are:
- Excessive physical activity before the blood collection procedure;
- Infants experiencing a strong emotional surge - stress in the infant, manifested by constant crying;
- The content of white blood cells is also increased during temperature fluctuations. A warm bath and exposure to the sun increase the concentration of leukocytes;
- Critical periods after birth: 2 days after birth, 2 weeks. During these periods, leukocytes increase for no apparent reason;
- After the mother eats food (especially high-protein food) and subsequent breastfeeding;
- The period of introduction of complementary feeding - the amount of breast milk consumed decreases, as a result of which the amount of antibodies entering the baby's body decreases.
Pathological leukocytosis
A pathological increase in white cells is a reaction of the hematopoietic organs to toxic, infectious, radiation, purulent-inflammatory lesions. This deviation can be provoked by increased blood viscosity, untreated illnesses of the mother during pregnancy (even a common cold just before childbirth).
Diseases
In cases where preparation for the test was carried out correctly and a physiological irritant was excluded, a high concentration of WBC indicates the development of the disease. Some pathologies can cause an increase in the level of leukocytes:
- Allergic diseases;
- Infectious attacks accompanied by suppuration: meningitis, otitis media, cholecystitis, pneumonia;
- Inflammatory process (damage to the intestines, kidneys);
- Severe poisoning (medicines, spoiled food, heavy metals);
- Infectious diseases of a viral nature (rubella, hepatitis, bronchitis, ARVI);
- Fungal, parasitic infections;
- Autoimmune diseases;
- Injuries and burns;
- Blood loss;
- Bone marrow pathologies;
- Oncological diseases;
- Postoperative period.
Drugs
The decrease in WBC in an infant is influenced by the mother's use of certain medications. During pregnancy and breastfeeding, the drug affects the composition of the baby's blood. Such medicines include:
- Methyluracil;
- Hormonal agents;
- Derinat;
- Dexamethasone;
- Codecor;
- Diction.
Physiological leukocytosis
Features of physiological leukocytosis
It’s not for nothing that doctors say that before taking any test you need to prepare. And all because there are a number of factors that can affect the content of leukocytes in the blood. And if the tests were collected incorrectly, or the person did not prepare in any way or did not follow the recommendations of specialists, they may be false.
Very often, newborns exhibit physiological leukocytosis, which appears due to exposure to physiological stimuli on the body.
It may be in the following cases:
- Two days after birth. For some reason, this particular day is considered critical.
- In the middle of pregnancy, namely in the fifth or sixth month.
- Two hours after eating. And since small children eat often, this factor largely has an influence.
- In the second week after birth.
- With strong excitement. In the case of small children, this may be crying
- With strong physical stress, the child quickly moves his arms and legs.
After the physiological factor is removed, leukocytes and their content are restored.
Leukocyte formula and its changes
In the diagnostic process, doctors pay attention to the excess of the norm of leukocytes in the blood of children, to the ratio of different types of leukocyte cells. To determine which infection caused the pathology, the specialist must evaluate the change in concentration in the leukocyte formula
Table of limits of leukocyte blood formula norms in children
Leukocytes are divided into several types: neutrophils, eosinophils, monocytes, lymphocytes and basophils. They are united by the presence of a nucleus and the absence of their own color. Each type of white blood cell plays a specific role in the human immune system:
- Neutrophils form the bulk of leukocytes. Their main function is to find and destroy infections and bacteria.
- Basophils participate in the formation of inflammatory reactions, which attracts immune cells to the lesion. Exchange information between them.
- Eosinophils are an important link in the development of the body's allergic response.
- Monocytes regulate the immune response and promote the restoration of skin and nerve fibers.
- Lymphocytes organize the fight against bacteria and viruses and tumor cells.
Types of leukocytes
By observing an increase in the concentration of one of them, conclusions can be drawn regarding the disease that served as the root cause of the pathology. For example: if a baby’s test results show an excess of leukocytes and eosinophils in the blood, then the likely reason for this is the presence of worms and allergic reactions in the body. This disease is called “eosinophilia”.
If, against the background of high leukocytes, a child has elevated monocytes, then the disease is called monocytosis, and the efforts of doctors are aimed at excluding the diagnosis of mononucleosis.
Reasons for the increase in different types of leukocytes
In newborns and up to 4-5 years of age, an increase in white blood cells occurs frequently. And this is not always a signal about the presence of health problems. Additional examination will be needed in a situation where an excess of leukocytes in the blood is accompanied by the following symptoms:
- increased body temperature;
- painful sensations in joints and muscles;
- constant feeling of fatigue;
- periodic dizziness;
- deterioration in sleep quality and loss of appetite;
- sometimes increased sweating.
Taking a blood test from an infant
How to take a blood test correctly
Blood is taken from a newborn in the first hours after birth. This helps determine the child’s ability to adapt and identify the dangerous consequences of intrauterine infection. Blood must be collected from the umbilical cord. In addition to the general analysis, the sample is examined for the presence of infections that can be transmitted to the child from an infected mother.
After 3-4 days in the maternity hospital, blood is taken from the heel. The heel test is indicated for all newborns. The test may be delayed if you are preterm or underweight. During the examination, the following rules are observed:
- the child is fed 2 hours before blood sampling (drinking water is not prohibited);
- stressful situations should be excluded;
- the child must be awake (sudden awakening can cause stress).
Important information: What do increased segmented or band neutrophils in the child’s blood indicate?
Leukocytes in infant stool
The level of leukocytes in the stool of an infant is one of the main indicators of a coprogram - a general analysis of stool. Research data provides the opportunity to determine the presence of inflammation in the gastrointestinal tract and disruptions in the enzymatic state of digestion.
A single white blood cell count in the stool of an infant is normal. Often their number in the sphere of visibility does not exceed ten. If there is an increased content of white blood cells, this is a signal of a violation of the internal intestinal microflora.
The most common reason for an increase in the level of leukocytes in the stool of an infant is prolonged diarrhea, which causes the loss of a large amount of fluid. The combination of leukocytes and mucus in the stool should cause particular concern.
A sharp increase in the level of leukocytes in the feces of an infant may indicate a number of diseases:
- the onset of follicular rhinitis is characterized by the presence of mucus in the form of lumps in the child’s stool;
- dysbacteriosis is indicated by the presence of cocci, E. coli with a high level of leukocytes in the feces;
- an increased content of eosinophils - leukocytes that destroy foreign proteins, indicates the onset of allergic colitis;
- the appearance of neutrophils - leukocytes that carry the function of protection against various infections, leads to the conclusion about the onset of ulcerative colitis;
- dysentery is characterized by an increased number of neutrophils and general intoxication of the whole body. In this case, urgent measures to correct the situation are necessary, since the trend is extremely dangerous;
- Spastic colitis is indicated by a changing number of leukocytes combined with undigested fiber.
In the case when the baby’s feeding process is not structured correctly, disturbances in the daily diet occur, and the appearance of white blood cells may also occur.
However, it is important to know that quite often there is an increase in the number of leukocytes in the feces even in a completely healthy baby. This suggests that with the disease, deterioration in the general condition of the child, the presence of intestinal colic, loss of body weight and an allergic rash are of greater importance.
When the baby feels well, his appetite is not impaired, he does not feel unwell, he does not have pain in the abdominal area - parents should not be afraid of the greenish tint of the stool.
When your health worsens significantly, you should immediately consult a doctor. You should not self-medicate - in the case of infants this is strictly contraindicated.
Urine analysis for newborns
Urinalysis is done in clinics and any medical institutions. The technique is quite simple and does not require specialized equipment. Often, the reliability of the results can be influenced by several factors that are not related to the equipment, but distort the final assessment:
- the presence of vitamin C or protein in large quantities;
- violation of the rules of hygiene of the external genital organs, which can lead to the entry of leukocytes from other parts of the body and skin;
- insufficient amount of urine to assess chemical indicators.
More on the topic: How is bladder cystostomy performed?
How to properly take urine from a newborn?
Some inexperienced mothers fall into a stupor when it is necessary to collect urine from a newborn, since the baby not only does not sit on the potty, but also does not indicate the urge to deurinate. As a rule, they begin to cry after urination, because discomfort arises. Before submitting the biomaterial to a paid clinic, specialists themselves collect urine, but government institutions require the liquid already collected.
To collect urine from a baby, parents must follow the following procedures:
| № | Helpful information |
| 1 | Wash the baby's groin and perineum with baby soap or clean water, wiping the skin and mucous membranes with sterile material. |
| 2 | Buy urine collection bags at the pharmacy |
| 3 | Choose a bag according to the gender of the children; there are differences in collection for boys and girls |
| 4 | The device is attached with strips included in the kit and all you have to do is monitor when the container is filled |
Treatment of leukopenia
There is no pathogenetic treatment for leukopenia. Therapy for leukopenia begins with the elimination of the etiological factor that caused it; treatment is aimed at combating infectious complications, preventing infection, and treating the underlying disease that led to leukopenia.
To avoid infection, the following measures are taken:
- The patient is placed in a separate room with aseptic conditions, where regular cleaning is carried out using disinfectants and quartz treatment.
- Contacts of the patient with others are excluded;
- Careful care of the oral cavity, sanitation of mucous membranes and skin is provided.
- Careful control of food processing.
Treatment of leukopenia is carried out by two main groups of pharmacological drugs:
- drugs to stimulate hematopoiesis and metabolism;
- hormonal drugs that activate the formation of neutrophils and monocytes in the bone marrow.
During the period of agranulocytosis and/or exacerbation of infectious processes, treatment is carried out with immunostimulating, antibacterial drugs, symptomatic and rehabilitation therapy (vitamin therapy, detoxification therapy, maintenance of cardiovascular activity). If there are antibodies and circulating immune complexes in the blood, plasmapheresis is indicated.
Source: vekzhivu.com
Indications for the use of corticosteroid hormones may include relapses of immune agranulocytosis. Radical treatment for special indications is bone marrow transplantation. Chronic leukopenia of splenic origin is eliminated after splenectomy.
Causes of leukopenia in children:
Infectious origin:
- sepsis;
- herpes virus types 6 and 7;
- typhus and paratyphoid.
Non-infectious origin:
- ionizing radiation;
- acute leukemia;
- systemic connective tissue diseases;
- anaphylactic shock;
- plasmacytoma;
- Addison-Brimer disease;
- hypersplenism (enlarged spleen);
- tumor metastases to the bone marrow;
- drug-induced leukopenia.