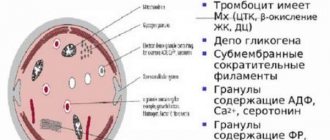
Platelets are the smallest blood cells that do not contain nuclei in the form of blood platelets, which are responsible for the process of blood clotting, i.e., for stopping bleeding that occurs. These plates essentially provide the liquid state of the blood and participate in the formation of clots called thrombi.
Platelets are produced by special cells in the red bone marrow (megakaryocytes). Platelets are short-lived cells: they live only up to 10 days, and then are destroyed in the spleen and liver. Instead of the “old” destroyed blood platelets (also called platelets), new ones are formed. This process is continuous. Why platelet counts in a child’s blood may be elevated and what to do in this case, we will discuss in this article.
Normal platelet counts in children
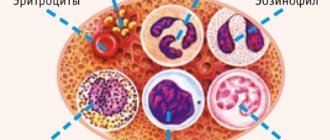
Platelets are blood cells that are responsible for blood clotting.
The number of platelets is determined in a general clinical blood test in terms of 1 cubic millimeter. The number of blood platelets is an important indicator of health, since it characterizes the child’s body’s ability to cope with bleeding and assess blood clotting.
Depending on the age of the child, the number of platelets varies:
- for a newborn, their normal content is from 100 thousand to 420 thousand;
- at the age of 10 days to a year, the norm is already 150–350 thousand;
- in children after a year, platelets are normally 180–320 thousand;
- in adolescence, in girls in the first days of menstrual bleeding, the number of platelets is 75–220 thousand.
An increased number of platelets in the peripheral blood is called thrombocytosis or thrombocythemia , and a decrease in their number is thrombocytopenia. In the first case, a deviation from the norm may indicate the possibility of increased thrombus formation, and in the second - bleeding. In both cases, the relationship between the formation of new platelets and their destruction is disrupted.
The platelet count is determined by testing blood from a finger or a vein. In newborns, blood is usually taken from a toe or heel. This study does not require special preparation. Blood should be donated on an empty stomach (you can give the child something to drink). In young children, the sample is taken before the next feeding or 2 hours after the previous feeding.
Before taking the test, physical and emotional stress is undesirable for the child. Even hypothermia can show distorted analysis results. The use of certain medications (corticosteroids, antibiotics) can also change the number of blood platelets. To ensure the authenticity of the detected increase in platelet count, it is recommended to take a blood test three times with intervals of 3-5 days.
The result of the blood test is ready on the same day (in some cases, the analysis is performed urgently in a shorter period of time). Platelet counting in a blood test is done quite often for children, especially for those who often have nosebleeds, often have hematomas (bruises) on the body, and bleeding gums. Parents may be alerted to the child’s complaints of weakness and dizziness, and frequent numbness in the limbs.
Indications for platelet counting are the following diseases:
- systemic lupus erythematosus and other autoimmune diseases;
- Iron-deficiency anemia;
- enlarged spleen;
- malignant blood diseases;
- viral infections.
What does thrombocytosis mean in children?
High platelets can increase transiently, without posing a danger to the child and due to a pathological reaction. Normally, the content increases to compensate for the changes that have occurred when the integrity of blood vessels is violated and vasopathies of various etiologies.
Reasons for the increase in quantity
The reasons why platelets are elevated in children are divided into two groups:
- primary;
- secondary.
Primary thrombocytosis is caused by a disturbance in the synthesis of platelets from immature cells.
A defect in the structure of precursors leads to the formation of atypical, or tumor, cells. A secondary increase in platelets in the blood of a child is caused by changes not related to the structure and function of hematopoietic (blood-forming) cells. These are benign disorders associated with an overestimation of the total number of blood platelets.
Causes of secondary thrombocytosis:
- acute and chronic infections;
- taking certain medications;
- splenectomy (removal of the spleen);
- bleeding, hemolysis, trauma;
- physical activity and stress.
The relative increase in the number of platelets is due to redistribution between blood and tissues. It is also called “false” because in reality the number of blood platelets does not increase.
In children, one of the most common reasons for increased platelets is iron deficiency anemia. At the same time, in the general analysis, a decrease in hemoglobin level is observed (a hidden course is possible, then the deficiency can be judged by the ferritin level). In this case, the child exhibits all the signs of anemia:
- pale skin;
- lethargy, drowsiness;
- decreased ability to learn and concentrate, memory impairment;
- brittle and dull hair, cracks in the corners of the mouth.
In addition to these symptoms, there are signs of high platelets: headaches, dizziness, petechiae and bleeding, swelling. This condition is extremely dangerous for the child’s body and requires urgent intervention.
During the examination, it is impossible to evaluate only one indicator in a general blood test in isolation. Their complex will tell much more about the reasons than a local decoding of platelet content.
Platelet functions
What does this mean for a newborn?
More than 10% of children in the first month of life may have a lot of platelets in the blood, but their number gradually decreases and is established by the age of one year. During this period, various genetic and metabolic diseases may begin to appear, so all indicators in a newborn require special attention so as not to miss anything. First of all, hemoconcentration and dehydration in the child should be excluded.
In a baby
In a child under one year old, an increased number of platelets may not manifest itself in any way. It happens that the symptoms of thrombocytosis are nonspecific and parents do not attach any importance to this. A small child cannot complain of malaise and headache. A decrease in the baby's usual activity may become noticeable. He may begin to suck milk less, gain weight poorly, and sleep more. But such behavior in a child can be characteristic of most diseases.
Regular screening is very important. A simple general blood test is sufficiently informative to rule out thrombocytosis. If the baby has problems with clotting, then a more in-depth blood test is required.
Why is it dangerous?
When platelets are elevated, this can lead to blood clotting disorders. The formation of blood clots is most common in the vessels of the lower extremities. Severance of the plate from the vascular wall can lead to thromboembolism.
The most dangerous are blockages of the pulmonary artery and cerebral vessels. But thromboembolism in another place can lead to necrosis and even gangrene.
Elevated platelets in a child’s blood can manifest as bleeding, petechiae, and edema. Children become more passive.
Bleeding with an increased platelet count is caused by the constant formation of microthrombi, which causes a deficiency of coagulation factors (chronic DIC).
How to lower the level?
The level of platelets in the blood is reduced by blood thinning. This can be done with a special diet and/or medication. If a child takes any medications, then you need to study the instructions and consult a doctor to exclude the influence of the drug on laboratory parameters.
The choice of drug therapy directly depends on the cause of thrombocytosis. Main directions in treatment:
- prevention of thrombosis;
- cytoreduction (based on reducing the formation of new platelets);
- treatment of complications.
When developing a diet, hematologists recommend including some blood thinning products in the children's diet:
- fish oil with a high content of polyunsaturated fatty acids;
- garlic;
- foods high in magnesium.
You need to limit your consumption of nuts, bananas, and pomegranates.
For children under one year of age, continued breastfeeding is extremely important. This has a positive effect on the fight against thrombocytosis.
A child should not be limited in water consumption. Liquid can also be administered with foods: soups, liquid porridges. Delicious teas, compotes, diluted juice - all this will help expand your drinking regime. The child should not consume less than 2 liters of fluid per day.
Otherwise, you need to rationalize your diet. A hematologist will help you create an individual diet for your child.
Fish oil is good for elevated platelets
Causes of thrombocytosis
Thrombocytosis can be caused by:
- increased production of blood platelets by megakaryocytes of the red bone marrow (with erythremia);
- slow platelet utilization (when the spleen is removed);
- disturbance of the distribution of platelets in the bloodstream (due to physical or mental stress).
When an elevated platelet count is detected, it is very important to determine the cause of this condition. Only a pediatrician or hematologist (a specialist in blood diseases) can identify this cause.
Thrombocytosis as a disease can develop in children at any age. But such a diagnosis is made with a significant increase in the number of platelets - more than 800 thousand/l. More often, a mild increase in the number of blood platelets occurs due to a number of reasons or in a number of diseases.
There are primary , clonal and secondary thrombocytosis.
With clonal thrombocythemia, there is a defect in the stem cells themselves in the bone marrow (they are damaged by the tumor process). They do not respond to stimulation of the process by the endocrine system, and the process of platelet formation becomes uncontrollable.
A similar mechanism is observed in primary thrombocythemia . It is associated with the proliferation of several areas of the red bone marrow and, as a consequence, with an increase in the number of newly formed blood platelets. The causes of this condition can be hereditary (congenital) diseases or acquired (myeloid leukemia, erythremia).
In primary thrombocytosis, the number of blood platelets can vary: from a slight increase to several million in 1 μl, but high levels are more typical. In addition, their morphology also changes: platelets of enormous size and altered shape are found in the blood smear.
The mechanism of development of secondary thrombocytosis can be different:
- when the spleen is removed, old or obsolete platelets do not have time to destroy, and new ones continue to form; in addition, the spleen produces antiplatelet antibodies and a humoral factor that inhibits platelet production;
- During the inflammatory process, the body intensively produces a hormone (thrombopoietin), which promotes the maturation of blood platelets, which help cope with inflammation; biologically active substances (for example, interleukin-6) are anti-inflammatory cytokines that stimulate platelet synthesis;
- in malignant diseases, the tumor produces biologically active substances that have a stimulating effect on bone marrow megakaryocytes and the production of blood platelets; this is more often observed in lung sarcoma, kidney hypernephroma, lymphogranulomatosis;
- thrombocytosis also develops as a response of the body to repeated blood loss (with ulcerative lesions of the intestine, with cirrhosis of the liver),
Secondary thrombocythemia (symptomatic or reactive) can develop in a number of diseases:
- tuberculosis;
- iron deficiency or hemolytic anemia;
- rheumatism in the active stage;
- ulcerative colitis;
- osteomyelitis;
- chronic and acute infections (viral, bacterial, fungal, parasitic);
- extensive surgical interventions;
- removal of the spleen (for injuries or hemophilia);
- acute blood loss;
- fractures of tubular bones;
- cirrhosis of the liver;
- amyloidosis;
- malignant diseases.
Secondary thrombocytosis is characterized by a less pronounced increase in the number of platelets: in very rare cases, their number exceeds a million in 1 μl. The morphology and function of blood platelets are not impaired.
In any case, detected thrombocytosis requires a full examination and clarification of the cause of its occurrence.
In addition to diseases, it can also be caused by side effects of medications (Vincristine, epinephrine, adrenaline, corticosteroids, etc.). There are no specific symptoms of thrombocytosis.
When an increased platelet count is initially detected, the following studies must be performed:
- determination of serum iron and serum ferritin;
- determination of C-reactive protein and seromucoids;
- blood coagulation analysis;
- Ultrasound of the abdominal and pelvic organs;
- if necessary, consult a hematologist;
- bone marrow examination (only as prescribed by a hematologist).
When to see a doctor
As soon as the analysis reveals that the child’s platelet count is elevated, you should immediately consult a doctor.
A hematologist deals with the problem, but you can also show the child to your local pediatrician . The doctor will prescribe all the necessary tests and, based on their results, make a diagnosis.
To make a diagnosis, the doctor will prescribe the following tests:
- blood test for platelets every 4 days (3 times);
- general blood analysis;
- ultrasound examination of the abdominal cavity and pelvic organs;
- bone marrow biopsy;
- analysis to detect iron and ferritin levels;
- coagulogram (a set of blood indicators indicating the coagulation process);
- C-reactive protein test (for signs of an infectious disease).
Additionally, the doctor may prescribe a consultation with a gynecologist and urologist. As soon as the results of these studies become known, the doctor will draw conclusions and prescribe effective treatment.
We will tell you all the details about the symptoms and treatment of cystitis in children, what to do in the acute form of the disease, on our website!
What is prescribed to children for urinary tract infections? You will find advice from experienced pediatricians in this review.
Do you know how to identify gastritis in a child? Find out about the first signs of the disease in the following material:.
Symptoms of thrombocytosis
An increase in the level of platelets in the blood leads to the formation of blood clots in vessels of any location.
With primary thrombocytosis, the size of the spleen is enlarged, blood clots of different locations can form, but bleeding in the digestive organs can also occur. Blood clots can also form in large vessels (veins and arteries). These changes contribute to the development of prolonged hypoxia or ischemia, which is manifested by severe itching and pain in the fingertips, and gangrene of the fingers may even develop. Hypoxia of tissues and organs leads to disruption of their function: disorders of the central nervous system and kidneys may be observed.
Clinical manifestations are caused by the underlying disease, the symptom of which is thrombocytosis.
Children, as noted above, may experience frequent nose and gum bleeding, bruises on the body with the slightest injury or even for no apparent reason. Vegetative-vascular dystonia (fluctuations in blood pressure, headaches, cold extremities, increased heart rate), and iron deficiency anemia may develop.
Reactive thrombocytosis is clinically mild and may be asymptomatic.
General information
Platelets are blood elements that are formed in the red bone marrow from megakaryocytes .
From one megakarikaryocyte, 5-10 thousand mature platelets are formed, the lifespan of which is 5-9 days. Then they are destroyed in the spleen and liver. About 70% of platelets are in the blood and they are located near the walls of blood vessels, and 30% are in the spleen. In the body, platelets take part in hemostasis (a complex blood clotting system) and stopping bleeding. In contact with the wound surface of the vessel, they are activated, changing shape, and stick together, forming a blood clot along with fibrinogen. In a healthy person, the normal platelet count is 180-400 × 10 in 9/l. That is, the upper limit of the norm is in the range of 350-400 × 10 in 9/l.
Thrombocytosis is an increase in the number of platelets in the blood above 450 × 10 in 9/L, which is not normal. If with a platelet count of up to 1000×109/l there is no risk of thrombosis and hemorrhage, then hyperthrombocytosis (blood cell level more than 1000×10 in 9/l) is accompanied by a high risk of thrombohemorrhagic complications. Thrombocytosis is observed in various conditions and diseases.
Reactive or secondary thrombocytosis is a response to various changes in the body of infectious, inflammatory and other origins. It accounts for 80-90% of cases of thrombocytosis and is the result of activation of megakaryocytopoiesis. Elimination of the cause (for example, treatment of an infectious disease or anemia) is accompanied by normalization of platelet levels. However, there is also true primary thrombocytosis (synonym essential thrombocythemia ) - this is a blood pathology related to myeloproliferative diseases (clonal proliferation of megakaryocytes). ICD-10 thrombocytosis code D75.2 (essential thrombocytosis). This pathology occurs at the age of 50-60 years, as well as in women under 30 years of age. It is very rarely diagnosed in children (hereditary thrombocytosis is more common in them). From the group of myeloproliferative diseases that occur with thrombocytosis, we can also name polycythemia vera and primary myelofibrosis.
Treatment
To treat primary thrombocytosis, the cytostatics Myelobromol, Myelosan and others are used for a long time until results are obtained.
In severe cases, in addition to cytostatics, thrombocytopheresis is used (removal of platelets from the bloodstream using special equipment).
Drugs that improve microcirculation and prevent the adhesion of blood platelets (Trental, aspirin, etc.) are also used. Aspirin can be used only if erosive changes in the digestive tract are excluded.
For clonal thrombocytosis, antiplatelet agents (Ticlopidine or Clobidogrel) are used in individual dosages.
In case of thrombosis or ischemic manifestations, anticoagulants (Heparin, Argotoban, Livarudin, Bivalirudin) are used under daily laboratory monitoring of platelet counts.
For secondary thrombocytosis, treatment includes therapy of the underlying disease and prevention of thrombosis associated with an increased platelet count. As a rule, reactive thrombocytosis does not lead to thrombohemorrhagic complications and therefore does not require special therapy. The prognosis is usually favorable.
In addition to drug treatment for thrombocytosis, it is important to provide the child with a balanced, rational diet rich in vitamins (especially group B). Breastfeeding is the most beneficial for infants.
Older children are recommended to consume the following foods:
- rich in iodine (seafood, nuts);
- rich in calcium (dairy products);
- iron-rich (offal and red meat);
- freshly squeezed juices (pomegranate, lemon, lingonberry, orange), diluted with water 1:1.
The following have a thinning effect on the blood: berries (cranberries, sea buckthorn, viburnum), lemons, ginger, beets, fish oil, flaxseed and olive oil, tomato juice and a number of other products.
It is very important to drink enough fluid (at the rate of 30 ml/kg). In addition to water, you should drink green tea, compotes and vegetable decoctions.
Bananas, mangoes, rose hips, and walnuts contribute to blood thickening.
Herbal medicine should not be used without the consent of a hematologist - after all, herbs are quite serious drugs and, if chosen incorrectly, can significantly aggravate the child’s condition.
Thrombocrit is increased in a child: what does this mean and what does it mean?
Sometimes it occurs that the thrombocrit is increased in a child.
An unfamiliar blood level causes panic in young mothers; we are always afraid of uncertainty and powerlessness to change circumstances. That is why every parent should understand what basic blood parameters and the normative value corresponding to the baby’s age mean. The birth of a baby is an unforgettable event that teaches us responsibility and a sense of duty for his future destiny. That is why blood counts are taken from all newborns to diagnose congenital diseases and prescribe timely treatment.
What does an increased rate indicate?
Thrombocrit reflects the level of platelets in the blood and is a percentage.
Platelets perform a number of important functions:
- accelerate plasma blood clotting;
- take part in tissue regenerative processes;
- stop blood loss from damaged blood vessels by forming a platelet plug.
To determine the thrombocrit level, a general blood test is taken, which is taken from the baby’s finger or from the newborn’s heel. A few hours before the test, the child should not be fed.
The rate of the indicator varies from 0.1 to 0.4 percent. When the indicator changes, the number of platelets in the blood also changes. When thrombocrit increases, thrombocytosis is diagnosed, and when it decreases, thrombocytopenia is diagnosed.
The characteristic signs of thrombocytosis are:
- internal bleeding;
- the presence of blood clots in blood vessels;
- functional disorders of the kidneys and nervous system;
- enlarged spleen;
- ischemia and tissue necrosis.
Thrombocrit does not depend on the gender and age of the patient.
Fluctuations in the indicator can occur for natural reasons that are not associated with pathological processes:
- Change occurs with the change of season and time of day.
- A decrease is observed during pregnancy and the menstrual cycle.
- An increased level is typical for professional athletes.
The platelet level is determined by the formula: the average level of platelet mass is multiplied by the number of platelet cells.
You should consult a doctor if your child experiences frequent nosebleeds, accompanied by headache, weakness, swelling of the legs and arms, bluish skin, itching, and blurred vision.
High platelet levels occur after surgery or severe stress. Every year the number of deaths that occur due to vascular thrombosis increases.
Doctors record an increase in thrombocrit in primary thrombocytosis caused by pathological processes in the bone marrow.
Primary thrombocytosis also provokes platelet growth.
The secondary form of thrombocytosis develops in the presence of the following diseases:
- for tuberculosis;
- with the development of ulcerative manifestations of the intestine;
- with acute inflammation of the joints;
- with cirrhosis of the liver;
- with high blood sugar levels (diabetes mellitus);
- with atherosclerosis;
- with a lack of iron in the blood (anemia);
- increased thyroid function;
- in case of protein metabolism disorders;
- in the presence of cancerous tumors.
Thrombocrit higher than normal in an infant does not indicate a final diagnosis. It is necessary to donate blood again to exclude an erroneous result.
The following also leads to an increase in this indicator:
- Fractures.
- Prolonged bleeding.
- Resection of the spleen.
- Taking corticosteroids.
How to achieve the norm
Reference values for a newborn baby are in the range of 100–400 thousand units per cubic meter. mm. After two weeks, the infant’s normative values are 150–350 thousand units per cubic mm.
In a one-year-old child, platelet counts are equal to the standard values of an adult – 180–320 thousand units per cubic meter. mm.
Thrombocrit is higher than normal in infants due to the adaptation of the newborn’s body to new environmental conditions.
Treatment of thrombocytosis of the primary form is carried out with medications that thin the blood: Myelosan, Myelobronol, Aspirin.
A prerequisite for treatment is adherence to a special diet:
- it is necessary to add buckwheat, beef, liver, seafood and nuts, foods high in vitamin B to the diet;
- It is forbidden to eat fatty, salty, pickled foods;
- ensure sufficient intake of water and non-concentrated juices;
- blood-thinning foods (beets, olive oil, ginger);
- exclude alcohol;
- reduce intense physical activity;
- try not to smoke.
It is worth excluding foods that thicken the blood (walnuts, bananas, rose hips).
Diagnosing pathologies of blood parameters does not mean that this is a verdict of inferiority of a small citizen. Prevention of this disease will help stop the development of the disease, even if the change in blood values is influenced by heredity.
Source: https://BolezniKrovi.com/analizy/obshhij/trombokrit-povyshen-u-rebenka.html
Which doctor should I contact?
If a child has an increased level of platelets in the blood, it is necessary to contact a pediatrician, and after the initial examination, a hematologist. If thrombocytosis is secondary, it is necessary to treat the disease that caused this syndrome with the help of an appropriate specialized specialist - oncologist, infectious disease specialist, gastroenterologist, traumatologist, nephrologist. It will also be useful to consult a nutritionist to select the right diet for thrombocytosis.
Rating: (votes - 2 , average: 5.00 out of 5)
Rules and technologies for passing analysis
Elevated platelets in a child can be determined using a clinical blood test. There is no separate study to determine their level, since not only the number of platelets is of diagnostic importance, but the counting and comparison of their level with all the formed elements of the blood.
Blood is collected by pricking the ring finger of the left hand. In newborns, blood is taken from the big toe, since the fingers on the hand are very small. Some laboratories take blood from a vein to test platelets.
This is usually done if venous blood is needed for other laboratory tests, such as blood chemistry tests. The examination is performed using an automatic analyzer or using microscopy.
Almost all modern laboratories are equipped with automatic analyzers. Blood testing by microscopy of a drop of blood is carried out when there is a suspicion of a defect in the result of the analysis performed by an automatic method. To determine platelets by microscopy, a drop of blood is smeared on a glass slide and the number of platelets is counted in relation to 1000 red blood cells.
Norm of thrombocrit in adults, children
Thrombocrit is elevated in the blood if its value is more than 0.39% (for both men and women under the age of 75). The lower limit of the normal interval is 0.14%. Since the relative number of platelets should be constant at any age, this value is the same for children.
For people over 75 years of age, the normal range is 0.18-0.31%.
Reasons for the increase
An increase in thrombocrit occurs in the following pathologies and conditions:
- Myeloproliferative diseases, in which tumors develop from hematopoietic stem cells of the bone marrow. These include: true polycythemia (the number of red blood cells, platelets and white blood cells increases in the blood), idiopathic myelofibrosis (overgrowth of connective tissue in the bone marrow), essential polycythemia (chromosomal disorder of hematopoietic stem cells). These pathologies can be either genetically determined or acquired.
- Connective tissue diseases.
- Iron-deficiency anemia.
- Large tumors of various locations.
- Diabetes.
- Atherosclerosis, in which the lumen of blood vessels narrows due to fatty deposits.
- Infectious and inflammatory diseases (pneumonia, meningitis, pyelonephritis, ulcerative colitis, Crohn's disease and others). With treatment and reduction of inflammation symptoms, PCT returns to normal.
- Hereditary disorders of the proper development of the spleen. Thrombocrit also increases in patients who have undergone surgery to remove this organ (up to 80% of cases). Normalization of the indicator usually occurs within 1-3 weeks, but in some cases the high level persists for years.
- Injuries and operations accompanied by large blood loss.
In young children, thrombocrit most often increases with viral infections or anemia.
Thrombocrit is elevated in the blood not only in serious pathologies, but also in some physiological conditions listed later in the article. In most patients (about 80%) this is a temporary phenomenon. Therefore, the doctor may order the test again.
Nutrition of a child with thrombocytosis
Drug treatment of the pathology in question is important, but doctors say that in order to obtain the expected result, it is necessary to monitor the patient’s diet. For infants, naturally, breastfeeding is the best option, but for older children it is extremely important to include the following products in the menu:
- seafood and nuts;
- milk and dairy products;
- red meat and offal (liver, heart);
- fresh juices (pomegranate, lemon, orange, lingonberry), diluted with clean water in a 1:1 ratio.
Ginger, olive oil, beets, tomato juice, fish oil, cranberries, lemons, viburnum and sea buckthorn have an excellent blood thinning effect. It is important that the child consumes the required amount of liquid per day - at least 30 ml per kilogram of weight; it is imperative to give the child tea, compotes and vegetable decoctions.
During the treatment of thrombocytosis, it is strictly forbidden to consume walnuts, rose hips, bananas and mangoes - these products actively thicken the blood, which can lead to the development of complications.
We recommend reading: Blood thinning - indications and rules for the use of drugs and folk remedies for blood thinning
An increased number of platelets in the blood of a child is a pathology that needs to be investigated. Only a doctor can carry out competent examinations, identify the true cause of the pathology and prescribe effective treatment - independent decisions lead to a deterioration in the child’s condition.
Tsygankova Yana Aleksandrovna, medical observer, therapist of the highest qualification category
20, total, today
( 55 votes, average: 4.18 out of 5)
Lymphedema, or elephantiasis: symptoms and treatment
Low leukocytes in the blood: causes of deviations
Related Posts
What is thrombocrit (PCT), the norm in a blood test
Thrombocrit is a blood indicator, which in the analysis form is designated as PCT (from the English plateletcrit), measured as a percentage. When the thrombocrit in the PCT blood test is higher than normal, this means that the risk of thrombosis is increased, and this change increases the risk of stroke or heart attack.
A low test result indicates a bleeding disorder, increasing the risk of internal bleeding.
Thrombocrit - what is it?
Thrombocrit is a blood test indicator that indicates what proportion of whole blood consists of platelets. The value of this general analysis parameter is determined only by the hematology analyzer and is calculated using the formula:
platelet count * mean platelet volume (MPV) * 10-4.
The value of the PCT indicator is directly affected by the average platelet volume MPV, as well as factors such as smoking, lack of vitamins B12, B9, B6, and depressive disorders.
Knowledge of the study results allows us to assess the effectiveness of the blood coagulation system. The test indicator reflects the human body’s tendency to bleed or form blood clots.
A thrombocrit test is prescribed as part of a comprehensive examination:
- heart and blood vessels;
- kidney;
- reproductive organs;
- endocrine system;
- respiratory organs;
- immune system.
Based on the test results, the risk of possible complications during organ transplantation is assessed and the course of diseases during treatment with immunosuppressive drugs is predicted.
Knowing the PCT value allows one to assess the risk of thrombosis when prescribing medications that affect the parameters of the coagulation system. Such an assessment is necessary for drawing up a treatment regimen and predicting the outcome of the disease in bedridden patients, with artificial ventilation, and before surgery.
Thrombocrit norm
Normal values for children and adults are the same. The PCT norm in adults and children averages 0.22 – 0.24%.
The normal range is the following values:
- lower limit – 0.11% – 0.15%;
- upper limit of normal – 0.28% – 0.4%.
The permissible limit experiences seasonal as well as daily fluctuations. In spring and at night, thrombocrit is 10% lower. In athletes, regardless of age and gender, the PCT value in the blood can double after physical activity. During menstruation and pregnancy, the test result may decrease by up to 50%.
Signs of deviation from the norm
A characteristic sign of deviation of the test results from the norm is the appearance of bruises on the body in the absence of injuries. Manifestations of the violation also include:
- cyanosis of the skin of the extremities;
- headache;
- decreased vision;
- skin itching;
- the appearance of traces of blood in the patient’s urine and feces.
Reasons for the increase
The PCT thrombocrit indicator in the analysis is increased in thrombocytosis - this condition is characterized by a high platelet count, which is manifested by thickening of the blood, which threatens thrombosis.
A deviation of thrombocrit from the norm is caused by pathologies that are accompanied by increased platelet production.
Thrombocrit levels are higher than normal in diseases:
- bone marrow – chronic leukemia, polycythemia, thrombocytopenic purpura;
- iron deficiency anemia;
- infections – viral, fungal, bacterial;
- diabetes mellitus;
- osteomyelitis;
- atherosclerosis;
- hyperthyroidism;
- ulcerative colitis;
- tissue necrosis.
If thrombocrit values in adults are elevated and their values are more than 0.4%, this indicates the possibility of a heart attack or stroke caused by thrombosis of a blood vessel. The cause of a condition where thrombocrit is elevated may be deep vein thrombosis of the lower extremities, which increases the risk of pulmonary embolism.
A higher than normal thrombocrit in the analysis in women can be caused by contraceptives, and this means that the medication should be discontinued, as changes occur in the blood that increase the risk of thrombosis.
The child's thrombocrit levels are elevated due to iron deficiency anemia, and this indicates that parents need to consult a nutritionist on what to feed the baby correctly for normal growth and development.
Treatment with hormonal drugs and antibiotics can cause an increase in PCT in children. Thrombocrit is increased in a child after an acute respiratory viral infection or influenza; in addition, this sometimes indicates a lack of daily water intake, which affects the condition in children more negatively than in adults.
A decrease in PCT occurs when the production of platelets or platelet precursors, which are megakaryocytes, is blocked. With a decreased PCT, there is a tendency to bleed.
This indicator is reduced during pregnancy. The drop in thrombocrit in women can be 2 times lower than normal, but during pregnancy this reduces the risk of thrombosis, and means that blood circulation and fetal nutrition will not be affected.
PCT decreases in conditions caused by:
- anemia - folate deficiency, aplastic, megaloblastic;
- autoimmune diseases – systemic lupus erythematosus, collagenosis;
- chronic diseases of the liver, kidneys;
- poisoning by poisons, drugs - diuretics, cytostatics, antibiotics, corticosteroids;
- chemotherapy;
- oncological diseases - hemoblastosis, leukemia.
When the thrombocrit is lowered and is less than 0.11%, then in adults this indicates a disorder of hematopoiesis in the bone marrow or an acceleration of the breakdown of platelets in the spleen.
A low PCT thrombocrit in a child’s blood test may be explained by:
- in infants - prematurity, low birth weight, hypoxia;
- in a child of an older age group – parasitic infection.
Thrombocrit analysis
The technique for calculating thrombocrit appeared with the introduction of automatic laboratory analyzers into clinical practice. This indicator is not determined “manually” or microscopically.
A study to assess thrombocrit levels is usually prescribed to the following categories of patients:
- pregnant women (in order to prevent possible complications);
- patients with varicose veins;
- patients with pathologies of the cardiovascular system, liver and other diseases listed above.
This indicator is usually assessed as part of a clinical (general) blood test or in a comprehensive study of the blood coagulation system.
How to prepare for research
Before donating blood for analysis, the following factors must be excluded:
- 8-14 hours before visiting the laboratory - consume food and drinks (you can drink clean still water);
- alcohol – 2 days in advance;
- fatty foods – per day;
- emotional and physical stress (including sports training) – 1 day;
- smoking - 2 hours before.
Blood is usually donated in the morning, but in some cases it is permissible to do this during the day, 4 hours after eating a light meal. Failure to comply with the above rules may lead to distortion of the research result.
How the biomaterial is collected
Biomaterial is collected from a finger (peripheral blood). In newborns and babies in the first months of life, it is difficult to take blood from a finger, so this can be done from the heel. In some cases, venous blood is used instead of peripheral blood.
The technique for carrying out this procedure is as follows:
- The subject is seated on a chair in front of the table. For people with increased nervous excitability, blood sampling can be done on a couch, in a supine position.
- A laboratory technician (or nurse) treats rubber gloves with 70° medical alcohol before each patient.
- The puncture site on the 4th finger of the left hand is also disinfected. After this, wait a while for the skin to dry, otherwise the drop of blood will spread.
- A puncture is made with a disposable sterile scarifier needle, which is removed from the sterile packaging in front of the patient. It is done on the side surface of the finger, since there are more blood capillaries in this area. In order for the blood to flow more abundantly, the puncture must be across the fingerprint lines (fingerprint lines).
- The first drop of blood is removed with a tissue. It contains a large amount of fluid that circulates in the tissues.
- Next, blood is drawn into a test tube.
- At the end of the procedure, a new sterile napkin (or cotton swab) soaked in alcohol is applied to the finger to prevent infection of the open wound. It must be pressed tightly for 5-10 minutes until the bleeding stops completely.
Thrombocrit is assessed in an automatic analyzer (in a closed chamber) along with other blood parameters.
How long to wait for research results
Analysis results can be ready within 1 business day. If the laboratory is heavily loaded, the data will be received within a few days.
Decoding analysis responses
The results of the study are deciphered according to the table indicated above, as well as in accordance with the characteristics of laboratory equipment and reagents. The form must indicate the actual values obtained and the reference values accepted in the laboratory.
In older people, the rate of platelet production decreases. In adults, the maturation period for these blood elements is about 10 days. This indicator may also differ from the norm in women during pregnancy and menstrual bleeding (0.07-0.21%).