Indications for the study
There are certain signs that indicate liver damage. As a rule, characteristic symptoms appear already in advanced stages, which complicates the treatment of the pathology. Blood biochemistry to check the liver is prescribed in the following cases:
- Yellowness of the skin. A typical sign of increased bilirubin levels. Yellowness of the skin/eye sclera indicates long-term inflammation.
- Increase in organ size. Deviations can be detected at the initial stage using an ultrasound examination. With a strong enlargement of the organ, the patient experiences a growth of the abdomen against the background of no changes in overall weight.
- Losing weight. For liver pathologies, nausea and refusal to eat are typical, which leads to weight loss.
- Bitter taste in the mouth. Liver disease is characterized by a bitter taste in the mouth, a coated tongue, a thick yellow-brown or white coating, and cracks on the surface of the tongue.
Symptoms
Symptoms of diseases are not always easy to recognize even for an experienced doctor. And of course, not everyone knows how to recognize liver disease. Liver diseases have a number of characteristic signs:
- Decreased appetite.
- Increased fatigue.
- Nausea and vomiting.
- Pain in the right hypochondrium.
- Abdominal enlargement.
- Increased bleeding.
- Digestive disorders.
- Poor general health.
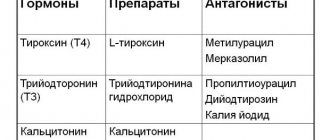
- Problems with hormonal levels.
Pain and bruising
The gland itself does not have pain receptors, so pain occurs due to tension in its capsule when the organ increases in size or inflammation spreads to its fibrous membrane. The pain is localized in the right hypochondrium, but in some cases it can be diffuse.
The character can be varied - from a feeling of discomfort to sudden attacks of pain. The increase can be determined by palpation of the abdomen. Due to its increased size, its lower edge will extend beyond the right costal arch, which will be noticeable upon palpation.
Most often this occurs with cirrhosis or acute infectious diseases, when other symptoms prevail over the pain syndrome.
Bruising occurs due to inhibition of the functions of hepatocytes, as a result of which the hemostasis process is disrupted and the walls of blood vessels are weakened. Bruises and hematomas occur even with the slightest injury, slight pressure and during sleep. It becomes difficult to stop bleeding even with a small cut. Wounds and scratches do not heal for a long time and periodically bleed.
Visual cues
One of the most characteristic signs of pathology of this organ is a change in skin color and turgor. Due to the fact that fat metabolism is disrupted, the skin becomes dry, flabby, various peelings appear, and there is a tendency to allergic rashes such as dermatitis and eczema.
In addition, spider veins and areas of hyperpigmentation are observed on the body. A man's appearance takes on feminine characteristics - fat is deposited on the hips, arms become thinner, mammary glands enlarge, and hair loss occurs.
Key indicators for liver diseases
The condition of the liver allows you to track certain enzymes. This:
- albumen;
- bilirubin;
- aminotransferases (AST and ALT)
- alkaline phosphatase (ALP)
- glutamate dehydrogenase (GlDH)
- sorbitol dehydrogenase (SDH)
- γ-glutamyltransferase (GGT)
- fructose monophosphate aldolase (FMPA).
Albumen
It is the main protein produced by liver tissue. A healthy organ produces 150–250 mg/kg albumin within 24 hours. The norm for an adult becomes 35–53 g/l. If the study showed a decrease, then the cause may be: liver failure, chronic hepatitis, cirrhosis.
A decrease in albumin levels is detected before the onset of typical symptoms
Bilirubin
This is a yellow pigment formed as a result of the breakdown of hemoglobin. The resulting indirect bilirubin enters the liver, is neutralized and excreted naturally. Normally, 250–300 mg (total bilirubin) is formed in the human body during the day. Indicators of direct bilirubin are of diagnostic interest. The norm is not higher than 5.1 µm/l.
Exceeding the permissible values in a blood test indicates the following pathologies:
The first symptoms of hepatitis
- inflammation of the gland of viral origin;
- cirrhosis;
- alcohol intoxication;
- cholangitis;
- stones in the bile ducts.
An increase in direct/indirect bilirubin fractions can be caused by:
- toxic/viral inflammation of the gland;
- suppuration, malignant neoplasms in liver tissue;
- cirrhotic organ damage;
- mononucleosis;
- echinococcosis.
Alanine aminotransferase (ALT, AlAT)
ALT norms depend on the gender of the patient: for men – 10–40 units/l, for women – 12–32 units/l. An increase in enzyme levels in the bloodstream can accompany acute hepatitis and obstructive jaundice. An increase in the ALT norm in relation to the permissible one is recorded in cirrhosis and during treatment with hepatotoxic drugs.
An increase in enzyme activity by 4-6 times or more indicates severe liver disease. The deviation is detected before the appearance of typical symptoms - jaundice, pain syndrome and others - in about 1-4 weeks. After the clinical picture develops, elevated ALT levels persist for no longer than 2 weeks, which is a sign of significant organ damage.
Aspartate aminotransferase (AST, AST)
The norm depends on gender: for men – 15–31 units/l, for women – 20–40 units/l. Increased AST activity is recorded in the event of hepatocyte death. Moreover, the more significant the damage to the organ, the higher the enzyme levels. An increase in quantitative indicators also occurs in acute infectious and toxic hepatitis.
Transaminases are an indicator of hepatocyte necrosis
Diagnosis of liver pathologies involves calculating the de Ritis coefficient - the ratio of AST/ALT numbers. Normally, it is equal to or exceeds the number 1.3. A change in numbers towards the lower side of the indicator indicates damage to the organ.
Alkaline phosphatase (ALP)
Enzyme activity depends on gender and age group. In a healthy adult – 30–90 units/l. An increase in alkaline phosphatase occurs in adolescents (up to 400 units/l) and expectant mothers (up to 250 units/l). A significant increase in the alkaline phosphatase level - 10 times or higher - occurs with the development of obstructive jaundice. If the excess is not so significant, one of the forms of hepatitis can be suspected.
Glutamate dehydrogenase (GlDH)
Normally, a biochemical blood test shows a low content of GLDG. The reason is that it is one of the liver enzymes located inside the cell. And an increase in its activity makes it possible to determine the severity of damage to the organ. Increased results indicate the onset of degenerative processes in liver tissue, caused by both external and internal factors.
It can be:
- neoplasms;
- liver metastases;
- toxic substances;
- infectious pathologies.
Calculating the Schmidt coefficient greatly helps in establishing the diagnosis: CS=(AST+ALT)/GlDH. With the development of obstructive jaundice it is in the range of 5–15, for acute hepatitis the figure reaches 30, and for metastases it is approximately 10.
Sorbitol dehydrogenase (SDH)
The norm is an indicator not exceeding 0.4 units/l. If the examination showed an increase in SDH by 10–30 times, then this is a clear sign of acute hepatitis.
γ-glutamyltransferase
In a healthy person, the permissible concentration of γ-glutamyltransferase is: for men – 250–1800 nmol/l*s, for women – 167–1100 nmol/l*s. An increase in enzyme levels is possible with the following problems:
- obstructive jaundice, cholestasis - an increase of 10 times or more is typical for them;
- malignant formations – enzyme activity increases 10–15 times;
- chronic hepatitis – 7 times.
In a blood test, the level of γ-glutamyltransferase is used to distinguish between alcohol and viral damage to liver cells
Fructose monophosphate aldolase (FMPA)
PMPA should be present in the blood only in trace amounts. Determination of this indicator is necessary for diagnosing acute hepatitis. In most cases, it is used to assess liver function in people whose professional activities require direct contact with substances toxic to the liver.
In acute hepatitis of infectious origin, the activity of PMPA increases several tens of times, and with regular exposure to toxic substances - no more than 3 times.
Instrumental diagnostics
In addition to laboratory tests, there are other ways to test a person's liver. Instrumental methods allow the doctor to expand the diagnostic search.
Many of them are absolutely safe and are performed even on children and pregnant women.
- Ultrasound. An ultrasound examination shows changes in liver tissue and can detect additional formations. You need to prepare for the procedure - do not eat foods that cause flatulence (baked goods, milk).
- Fibroscanning resembles ultrasound, but uses a highly sensitive sensor that is able to assess the degree of fibrosis of the liver parenchyma at an early stage of the disease. The results of the study can be compared in terms of reliability with a biopsy. Contraindicated for pregnant women.
- CT. Prescribed by the attending physician based on other diagnostic data. It is better to carry out with contrast in order to study in more detail the anatomical structure of tissues and the size of pathological formations. Thanks to CT, tumors, stones, and cysts are well visualized.
- MRI is used to evaluate soft tissues and blood vessels. Cannot be used if there are metal structures in the body. Most doctors consider MRI to be the most informative and safe research method.
- Biopsy. It is an invasive intervention and is performed under ultrasound guidance. A histological examination of the obtained biopsy specimen and a description of its morphological characteristics are performed. The method is gradually losing its leading position after the invention of laboratory test systems (“Steatoskin”, “Fibromax”).
- Laparoscopy. It is a surgical research method. On the anterior abdominal wall, gas, instruments, and an optical system are introduced through several accesses. The method allows you to assess the condition of organs and, if necessary, perform surgery.
Blood test for malignant neoplasms
Liver cancer and hepatitis are determined by identifying antigens to certain diseases. Hepatitis markers: A (HAV) – Anti-HAV-IgM, IgM class antibodies to virus A; B (HBV) – Anti-HBs antibodies to the HBs antigen of the B virus; C (HCV) – Anti-HCV-total antibodies to C virus antigens.
The tumor marker AFP becomes a marker for cancer. The disease is confirmed by a result of more than 10 IU. An increase in the indicator may indicate the presence of a malignant neoplasm in the organ itself, the presence of metastases, or embryonal cancer.
If there is a slight excess, you can suspect:
- cirrhosis;
- hepatitis;
- renal failure.
The presence of oncology is better indicated by a general clinical analysis in combination with biochemistry
What are liver tests?
Liver tests are a complex that includes a biochemical blood test without taking into account glucose levels and several other tests. Usually all necessary checks are carried out by a general practitioner. However, from time to time there is a need for the help of an infectious diseases specialist, hepatologist or surgeon. The diagnosis is positive if liver test readings are elevated.
If liver tests are normal, a negative diagnosis is made. If the level is low, additional examination may be required for diseases not related to the liver.
Preparing for the test
Blood biochemistry is prescribed if it is necessary to check liver function. Proper preparation for donating blood will help you get the most accurate results. Two to three days before visiting the laboratory, you need to exclude fatty, fried foods, fast food, sweets, smoked foods, cocoa, coffee, and marinades from the menu.
You should stop drinking alcohol a week before the test. Ethyl affects not only the condition of hepatocytes, but also the blood clotting rate. On the morning of blood donation, the patient should not smoke. But it is better to give up nicotine 10–12 hours before visiting the laboratory.
7 days before the test, you must stop taking any medications, including vitamin complexes. If this is not possible, then you need to stop taking the pills at least on the morning of blood donation. A woman must be sure that she is not pregnant. Due to gestation, it is possible that the permissible norms may be exceeded. And this cannot be considered as a symptom of a pathological condition.
On the morning of donating blood, you should avoid doing morning exercises, since increased physical activity can affect blood counts. The donation of biomaterial is carried out in the morning, on an empty stomach. The last meal should take place the night before. Dinner should be light.
Blood is drawn from the ulnar vein. The procedure is painless, but may be accompanied by slight dizziness. The interpretation of the resulting analysis should be carried out by the attending doctor, since only a qualified specialist is able to compare all the data received and determine the presence or absence of pathology.
The largest gland
Those who consider the liver to be an organ of the digestive system alone argue incorrectly. She has to carry out more than five hundred different “responsibilities” in the human body. The most important functions for life are entrusted to her shoulders. Let's list the most important ones:
- Cleans and filters the contents of blood vessels - blood.
- With its help, all kinds of toxins are removed.
- Participates in the formation of bile, part of urea and lymph.
- Provides regulation of fat and carbohydrate levels.
- Accumulates energy by releasing glucose from glycogen when a deficiency occurs.
Our most distant ancestors understood the value of this organ. In ancient Greek mythology, it was Prometheus's liver that was pecked out. And grooms in ancient times proposed to the bride “hands and livers,” and not hands and hearts, as they do today. Some African religions consider this organ to be the repository of the soul.
This glandular organ, provided that it belongs to an adult and healthy person, during its normal work requires oxygen tens of times more than a muscle of the same weight. And this fact speaks for itself. Whoever works, eats the same way.
Such an efficient organ requires careful attention. Considering that the disease is easier to prevent than to treat, it is important to know what is included in the list of preventive measures and what tests to take to check the liver.
Additionally
What additional things can a doctor include in the examination program, and what tests should be taken to check the liver? Here are some of them:
- Organ biopsy. Using special equipment, a microscopic sample of organ tissue is removed to study the structure and condition of tissues and cells. This is the most accurate diagnostic method.
- To clarify the diagnosis, the doctor prescribes studies that can characterize the cause of the disease. A blood test for AFP (protein) will show the presence of tumors or metastases in the liver. The presence of antibodies will help differentiate viral pathologies of the system. If toxic damage to an organ is suspected, the doctor may prescribe an analysis for the content of ethanol, drugs, and other breakdown products of toxic agents. And so on.
Scientific research in the field of diagnostic medicine is quite intense and fruitful, so the list of all tests for checking the liver and pancreas is updated with the advent of the latest advances in this field. In parallel with the biochemical examination, a hardware examination is carried out.