Bladder functions: do not treat and you will pee
The main job of the bladder is to collect and remove urine (urine) from the body.
The organ is equipped with nerve endings, so when the bladder fills, signals about filling are sent to the brain. An adult can control the urge by tensing the muscles to drain urine. When they relax, urine flows out through the urethra. Various pathologies disrupt the normal functioning of the organ, which significantly reduces the patient’s quality of life. The result is pain when urinating, incontinence or stagnation of urine. Sometimes the organ is completely removed, bringing the urine collector out.
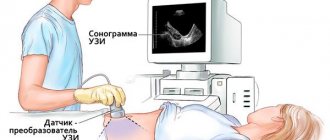
You can check the condition of the organ by undergoing an ultrasound examination of the bladder, which is usually performed together with a kidney examination or separately. The examination shows changes invisible to the eye that have occurred in the internal organs. The big advantage is the speed and painlessness of the method.
The study of the kidneys and bladder is a complex undertaking, so before starting the diagnosis you should do blood and urine tests and take them with you.
Hyperechoic formation in the heart
Increased brightness of a certain area of the heart muscle on ultrasound is a hyperechoic formation. In the heart, it is very often diagnosed in an unborn child at 32-34 weeks of pregnancy. The focus of increased density is not a developmental defect, but simply reflects the nature of the ultrasound. This phenomenon may indicate the deposition of calcium salts in one of the muscles of the organ, which does not affect its functioning in any way.
Echo-positive compactions require observation, since ultrasonography may disappear over time. In some cases, inclusion indicates chromosomal diseases, for example, Down syndrome. But this marker is a minor marker of this syndrome, so its presence very rarely confirms the disease and does not require additional research.
Structure of the bladder
The disease is not the main one, it is considered a clinical manifestation, so doctors have to identify real pathologies in order to prescribe the correct treatment course.
Research is carried out using ultrasound. Before this, the patient needs to drink a lot of fluid so that the water fills the entire volume of the organ.
During the examination, the doctor will determine all formations, their locations, and the degree of risk. In addition, the size of the bladder will be revealed and its ability to retain urine volumes will be determined. In order to diagnose thickening of its walls, you need to have an idea of the normal thickness. Normal thickness is 3-5 mm. The normal rate of urine flow is 14 cm per second.
An ultrasound examination visualizes not only the structure of tissues, but also the location of the organ in the pelvis. The ultra-sensitive sensor detects the slightest structural changes caused by disease or infection. At the same time, the location and structure of the bladder is different in men and women, which is due to the anatomical and physiological characteristics of the sexes.
- In men, the bladder is located between the two seminal ducts, with the prostate (prostate gland) located below.
- In women, the uterus and vagina are located in front of the bladder.
Why is this important to know? Diseases of nearby organs affect the functioning of the bladder. Thus, the proliferation of glandular tissues of the prostate (prostate adenoma) causes pressure on the walls of the bladder, which leads to a frequent urge to urinate in men. The bladder in women suffers especially during pregnancy, when the growing fetus puts pressure on neighboring organs.
Differences in the structure of the urinary organs are also noticeable in the size of the urinary tract. In men it is 16-20 cm, and in women it is short, only 2-5 cm. Thanks to the length of the canal, men are better protected from pathogens and infections entering the body, but women pick up pathogenic microflora immediately.
The ultrasound machine “sees” right through the bladder. The organ is a round-shaped muscular sac consisting of several layers:
- The inner mucous layer is folded, but as it fills, the folds smooth out, except for the fold near the ureter (to prevent urine from flowing back out). The mucous membrane is very sensitive to infections that enter the body through the urethra.
- The submucosal layer is located between the mucous membrane and the muscular layer. It is replete with nerve endings and blood vessels, so any foreign body (infection, stones, sand) causes a burning sensation, frequent urge to go to the toilet, and nagging pain.
- The muscle layer consists of smooth muscles lying in three layers, connected into one large compressor muscle, responsible for pushing urine out. Around the ureter, the muscles form circular sphincters - peculiar valves responsible for the release of urine into the ureter.
- The serous layer covers the entire surface of the bladder.
The urethra is examined with both superficial linear and cavity covex sensors with a frequency of 7.5-15 MHz. In ultrasound diagnostics, there are three ways to examine the urethral canal:
- Victory echourethrography. The method is used in cases where the patient suffers from spontaneous urination. The essence of the method is this: using a catheter, the canal from below is filled with a special liquid. Then the doctor examines the width of the urethra, the condition of the tissues, as well as the dynamics of the mobility of the neck of the canal.
- Retrograde urethrography. Well visualizes the anterior part of the urethral canal. The doctor uses an ultrasound machine to monitor the speed of urine flow and identify diverticula (protrusions), structural damage, adhesions and inflammation.
- Combined counter urethrography combines ascending and descending methods. The drug Urografin is injected into the urinary canal, which also has an antibacterial effect.
These methods are used on men. They have a longer urethral canal than women, but are no less susceptible to various diseases. Using ultrasound urethrography, various congenital defects are detected: epispadias (partial or complete splitting of the wall), hypospadias (displacement of the urethra), congenital urethral valves, hypertrophy of the spermatic tubercle (proliferation of the tissue of this rudiment), accessory urethra (causing urinary incontinence).
Also, ultrasound diagnostics of the urethral canal visualizes rare pathologies: urethrocele (cyst inside the canal), stricture (narrowing of the lumen), obliteration (tissue proliferation, as a result of which the lumen of the canal is blocked), agenesis (absence of the urethra).
If you find an error, please highlight a piece of text and press Ctrl Enter
What is hyperechogenicity and acoustic shadowing?
“Echogenicity” is the ability of solid and liquid physical bodies to reflect sound waves. All internal organs are echogenic, otherwise an ultrasound would be simply impossible. “Hyper” means beyond anything, in our case, beyond the normal echogenicity of kidney tissue. A hyperecho signal means that something has appeared inside the kidney that can powerfully reflect ultrasound waves.
The doctor identifies the inclusion on the screen by a light, almost white spot, and immediately pays attention to whether the detected inclusion casts an acoustic shadow, that is, a bunch of ultrasonic waves that did not pass through it. An ultrasonic wave is slightly denser than air, so only a very dense object can prevent it from passing through.
Hyperechoic inclusions are not an independent disease, but a signal about the development of pathology inside the kidney.
How is pathology treated?
The normal bladder has the following characteristics: a flat, round shape when the bladder is empty and a pear-shaped shape when the bladder is full.
On the screen of an ultrasound machine, a transverse image visualizes the round shape of the organ, and a longitudinal image visualizes the ovoid shape. Any deformation indicates pathology:
- inflammation or cancer on neighboring organs raises the bottom of the bladder and compresses the back wall;
- prostate adenoma raises the fundus, deforming its contours;
- cystitis also deforms the contours, as do uterine fibroids, pregnancy after the 4th month and stones.
Based on the type of formation of thickenings, diffuse and local disease are distinguished.
Such thickening of the walls can cause inflammatory processes or a sudden increase in stress on the muscles.
The ureter is a hollow organ consisting of muscles. It is designed to accumulate and retain urine. The process of urine excretion is designed in such a way that when the bladder is filled, its nerve cells begin to experience irritation.
The signal sent to the brain returns as a command to begin draining urine, after which the muscle tissue begins to contract.
If urine output is blocked, then the muscles will begin to make great efforts, trying to push urine out even through the obstacle that appears. Prolonged and numerous contractions cause an increase in muscle mass, which causes the walls to thicken.
Having identified such changes, the doctor must perform all studies in order to promptly identify the probable pathology and prescribe the correct treatment.
Thickening of the walls may appear due to cystitis. Having penetrated the urinary tract, the infection will affect the mucous membrane, causing changes that will cause the appearance of thickenings.
It is not distributed over the entire surface of the walls, but only in small areas. One of the reasons may be heredity associated with certain structural features of the genital organs.
It happens that local pathology is acquired during life. Corrections can be made by injuries to the bladder, which provoke the appearance of hematomas that precede thickenings.
Formations of a malignant and benign nature, papillomas, polyps, identified by ultrasound of the bladder, manifest themselves as hyperechoic formations. An ordinary stone can also look like this.
The walls of the bladder can also become thicker due to tuberculosis. True, in this case there are no external signs, and to identify the pathology, the doctor will need to conduct a diagnostic examination.
https://www.youtube.com/watch?v=fcwzf7h0WnQ
The bladder has nerve endings that trigger when it is full and send signals to the brain. The result of deciphering them is very simple - there is a need to empty the bladder.
Ultimately, the muscles contract and urine is directed outward through the ureteral canal. If the bladder does not work correctly, then it is not able to “push out” the accumulated volume of fluid, which causes a gradual thickening of the muscle layers.
One of the reasons for such a change could be a large stone blocking the ureter.
There are some other reasons why the walls of the bladder thicken:
- New formations in a narrow place of the cervix, which can also block the channel for drainage of urine.
- The narrowing of the opening connecting the bladder with the outlet canal causes diffuse pathological manifestations. This is a stenosis that can be congenital or acquired as a result of previous diseases.
- Urethritis is a chronic inflammatory process in the urinary canal.
- Diverticulum. This is a sac-like depression in the walls of the urethra, located near the cervix and interfering with the normal output of urine.
Quite often, doctors prescribe Allochol to treat thickening of the bladder walls. The treatment course lasts up to fifteen days. It is aimed at disinfecting and eliminating inflammatory processes, giving the walls normal dimensions.
In cases of exacerbations, drugs against microbes and parasites are prescribed - Nikodim, Cholenzym, Amizil and others. If a tumor is detected, chemotherapy or surgery is performed.
As folk remedies, you can use mint tea, infusion of dandelions, and celandine. Vodka tinctures made from the juices of beets, carrots, black radishes, aloe, and honey are excellent.
Hyperechoic formation in the liver
Very often, on ultrasound examination, the tumor appears as a hyperechoic formation. In the liver, it may indicate cancerous lesions or metastasis from other organs. After such an ultrasound conclusion, the patient is sent for histological verification.
Hyperechogenicity in the liver most often indicates hemangioma. The size of this neoplasm depends on its type. Capillary lesions are about 3 cm, and cavernous lesions can exceed 20 cm. According to medical statistics, women are more likely to encounter this problem. At the same time, its exact causes are unknown, but scientists associate the appearance of compactions with hormonal levels. There are also a number of cases where tumors were detected in pediatric patients. This may indicate a genetic predisposition.
Signs of liver formation may not appear. If it grows quickly, the symptoms become pronounced. The patient complains of attacks of nausea and vomiting, pain in the side. Treatment depends on the size of the tumor. If it is less than 5 cm, then only medical supervision is indicated. But if the compaction interferes with the normal functioning of neighboring organs or its size is more than 5 cm, then surgery is performed.
Bladder stones on ultrasound
Stones can migrate into the bladder from overlying areas. Urine stagnation due to bladder outlet obstruction due to prostatic hyperplasia, neurogenic bladder, urethral strictures, urethral or bladder diverticula, or cystocele predisposes to the formation of bladder stones.
Drawing. On ultrasound, a stone in the bladder is a hyperechoic inclusion with an acoustic shadow; with color doppler, a flickering artifact is observed. On the cross section in the supine position (1, 2), doubt arises - these are two round stones or one elongated stone. When turned on its side (3), a single rounded stone of a smaller size was identified, which was regarded as a specular artifact.
Note to women
Hypo- and hyperechoic inclusions in the uterus can be diagnosed using ultrasound. Gynecologists recommend undergoing a thorough medical examination every six months - this will help prevent the development of many pathologies. As medical practice shows, most diseases do not cause discomfort at the initial stage of development, so it is important to regularly visit a gynecologist. If inclusions are identified, this is not always a sign of serious pathology. But it is still better to get additional advice from your doctor. Based on the diagnostic results obtained, the doctor will prescribe, if necessary, complex therapy. It is forbidden to self-medicate and use folk recipes in order to improve your well-being - this will only aggravate the course of the disease and harm your overall health.
Echogenicity of the bladder
Echogenicity depends on the acoustic resistance of tissues: the denser the formation, the higher the echogenicity. A healthy organ has an anechoic structure, which is reflected on the monitor in dark color. The organ is hollow inside.
Cysts have slight echogenicity against the background of anechoic healthy bladder tissue. Stones that also move when the position of the patient’s body changes have the highest echogenicity.
- Hyperechogenicity indicates a foreign body (stones).
- Increased echogenicity without an acoustic shadow indicates chronic cystitis; an acoustic shadow with hyperechogenicity indicates the formation of stones in the bladder.
- Increased echogenicity and uneven contours indicate possible cancer.
Acute cystitis is characterized by increased echogenicity and wall thickening. An echo-positive sediment of red and white blood cells, as well as salt crystals, forms at the bottom of the bubble. The sediment is mobile, it moves as soon as the patient turns on the other side.
Uneven echogenicity, a combination of hyper- and hypoechogenicity indicate a purulent-inflammatory process in the bladder. Endometriosis (growth of the endometrial layer inside the uterus) in advanced cases leads to the drift of endometrial cells into the bladder. This is reflected on ultrasound by thickening of the organ wall and echogenic inclusions.
The signs of endometriosis are similar to those of bladder cancer, so if pathology is suspected, additional research is required. But stones have high acoustic density. They are easily visible against the background of the anechoic base. Stones come from the kidneys, carried in the flow of urine. Sand and very small stones are often found in the folds of the mucous membrane, so cytoscopy (bladder endoscopy) will be more effective in identifying them.
Important features. Cancer is difficult to identify using ultrasound diagnostics. However, any tumors are clearly visible on the screen, but their nature should be clarified by other methods (X-ray, MRI).
Treatment of the disease
Depending on the diagnosis, each patient is prescribed treatment on a purely individual basis.
If a patient is diagnosed with an anomaly in the structure of the kidney, then in most situations a decision is made to monitor the patient’s condition and monitor all changes. If we are talking about disturbances in the functioning of the kidney, then the only way out of this situation is surgical intervention.
Very often, patients experience hemorrhages or hematomas as a result of injuries; surgical intervention, of course, is not prescribed for the treatment of such formations, the only exception being situations where there is a real threat to the normal functioning of the kidney.
Medicines are prescribed individually by a doctor
Diagnosed purulent processes are treated mainly with medications and, in extreme cases, removed surgically. In this case, the decision is made exclusively by the attending physician separately in each case.
As for formations such as cysts, each case is also considered separately. If there is no threat of its rupture, degeneration or suppuration, then observational tactics are chosen, otherwise an operation is performed to remove it.
Tumors are rightfully considered one of the most dangerous formations. Treatment decisions are made only after the type, size and location have been determined. If a patient is diagnosed with a malignant tumor, then it can only be gotten rid of surgically and then only with timely access to a medical facility. In an advanced stage, malignant tumors in almost all cases lead to death. In the process of getting rid of malignant tumors, either part of the organ or the entire kidney can be removed. Metastases and lymph nodes are also removed together.
If a patient is diagnosed with a malignant tumor, the only way to get rid of it is through surgery.
Regardless of what kind of formation develops in the kidney, all of them can be gotten rid of without harm to health, only if you contact a medical facility in a timely manner and strictly follow all the recommendations of your doctor.
Bladder diverticulum on ultrasound
Visualization of a diverticulum is possible only if its size is at least 1 cm. An anechoic diverticulum protrudes beyond the bladder, sometimes the neck of the diverticulum is visualized, the diverticulum can collapse or enlarge. A bladder diverticulum is a protrusion of the bladder mucosa due to local detrusor weakness.
Ultrasound clearly shows the diverticulum and neck. When a bladder diverticulum has a narrow neck, it may be difficult to show the connection to the bladder lumen. Transrectal ultrasound may be superior to transabdominal ultrasound in showing the diverticular neck.
CDUS can be helpful in differentiation by showing the movement of urine through the opening in the diverticular neck. This urine flow is best demonstrated using the Valsalva maneuver. Diagnosis of bladder diverticulum can also be facilitated by ultrasound scanning at varying degrees of bladder filling.
Congenital bladder diverticula are rare and usually solitary, and most are located paraureterally along the posterior edge of the bladder.
Acquired diverticula are often multiple and result from chronically elevated intravesical pressure combined with anatomical or neuropathic bladder outflow obstruction. Small differences between hypertrophied muscle bundles are called cells or sacs. Although the distinction is somewhat arbitrary and subjective, in this order it is convenient to consider cells, sacs, and diverticula as increasingly serious manifestations of chronically elevated intravesical pressure.
Tumors may arise in the diverticulum, which appears as a solid mass in a cystic ultrasound lesion. CDUS may be useful in differentiating a tumor from a blood clot in a diverticulum. A diverticular tumor that appears on ultrasound cannot be demonstrated by cystoscopy if the diverticular neck is narrow. Diverticular cancer tends to invade the perivisual tissue earlier due to the lack of a muscular layer.
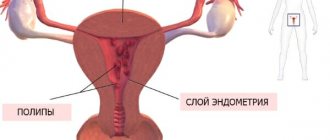
Hyperechoic formation of the cervix
An area with increased density, that is, a hyperechoic formation of the cervix, may be a polyp or a blood clot that has not been released after menstruation. To differentiate these conditions, an ultrasound examination is performed on days 5-10 of the cycle. If echo-positive structures are detected in the muscle tissue of an organ, this may be a sign of fibroids, lipomas or tumors. In this case, the uterus increases in size and changes its contours.
Foci of increased acoustic density in the thickness of the myometrium are observed in women with diabetes mellitus during menopause or after endometrial curettage. In the latter case, light areas on ultrasound indicate scarring of the walls of the organ or remnants of the fertilized egg.
Bladder fullness
https://www.youtube.com/watch?v=5lbjXka1ijI
The volume of urea is 350-750 ml in men, 250-550 ml in women.
The volume decreases if scars form on the walls, which in turn arise due to inflammation. Developmental pathologies of neighboring organs (uterine fibroids, prostate adenoma) also reduce the volume of the bladder.
After operations on the abdominal organs (removal of the appendix, intestinal surgery) it leads to adhesions that reduce the ability of the bladder walls to stretch.
In pregnant women, the organ narrows and elongates. Its volume decreases, so expectant mothers feel the need to go to the toilet more often.
An increase in the volume of the bladder occurs when it overflows with urine, and this occurs when the urethra is blocked by a stone or tumor, as well as the growth of the prostate gland.
Filling rate is about 50 ml per hour. Normally, a persistent urge to urinate occurs when at least 250 ml of urine enters the bladder. That. a person goes to the toilet 5-7 times per day. If this happens more often, then we can talk about infection or inflammation (cystitis).
After urination, no more than 50 ml should normally remain. To do this, the bladder is checked twice by ultrasound: first in a full state, then in an empty state. If urine remains more than 50 ml, this indicates problems with the urinary canal or ureter (polyps, deformation).
Hyperechoic formation in the uterus
If during an ultrasound examination a woman has a hyperechoic formation in the uterus, this may indicate the following conditions:
- In the middle of the menstrual cycle, the central part of the endometrial tissue becomes hyperechoic with a dark rim. During menstruation, the “rim” brightens and increases in thickness.
- A lump may indicate a formation in an organ cavity, for example, polyps or fibroids, but not pregnancy.
- After an abortion, fetal skeletons may remain in the uterus, which become calcified and are defined as hyperechogenicity. Very often, such women are diagnosed with secondary infertility, and menstruation is very heavy.
- In case of chronic endometritis or after surgical curettage, acoustic-type seals and air bubbles are visible on ultrasound.
- Advanced uterine fibroids are another possible cause of high-density tissue for ultrasound waves. Myoma may contain calcifications with a distal shadow. If the neoplasm is multiple, then the normal contour is disrupted and the organ cavity is displaced.
- Calcified areas indicate myomatous nodes in the uterine cavity. This is possible after intrauterine surgery or recent labor.
To identify each of the above conditions, the patient is prescribed a set of additional studies. After which treatment or observation by a doctor may be prescribed.
Cystitis on ultrasound
Cystitis is an inflammatory lesion of the bladder caused by bacteria (much less commonly, viruses and fungi). The disease can be provoked by the following factors and pathologies:
- hypothermia;
- urolithiasis disease;
- sexual infections;
- pyelonephritis;
- adenoma and prostate cancer with difficulty in urine outflow;
- abuse of alcohol, spicy and fatty foods;
- weakened immunity.
There are chronic and acute types of cystitis. The main symptoms of the disease are:
- pain in the groin area;
- pain, burning when urinating;
- increased urination;
- unpleasant odor of urine;
- unusual color of urine, blood, pus or mucus.
- This symptomatology manifests itself most clearly during the acute course of the disease or exacerbation of the chronic form.
The most informative methods of examination for cystitis include ultrasound of the bladder with detection of residual urine and ultrasound of the prostate. Before the study, certain preparation is required, the purpose of which is to fill the bladder. To do this, an hour and a half before the procedure, you need to drink about 1 liter of liquid (non-carbonated).
An ultrasound sign of acute cystitis is the presence of small hyperechoic particles in the bladder cavity. This is the so-called “sediment”, which consists of accumulations of epithelial cells, red blood cells, white blood cells and necrotic tissue. It is possible that the walls of the organ may thicken by more than 3 mm, but in general their contours are smooth and without deformation.
If the disease becomes chronic, the walls may become deformed, the shape of the bladder often changes, and it becomes asymmetrical. The cavity also contains sediment in the form of hyperechoic (light in the picture) clots. The size of the organ decreases slightly, which indicates fibrous changes in the walls due to prolonged inflammation.
Sometimes round hyperechoic formations are found in the cavity of the bladder, which indicates urolithiasis. In men, it is possible to identify signs of prostate adenoma - an increase in its size, heterogeneity of structure, etc.
With cystitis, ultrasound reveals diffuse or focal thickening of the bladder wall. Cystic cystitis, eosinophilic cystitis and condyloma can closely mimic a bladder tumor.
Hemorrhagic cystitis often occurs after irradiation of the pelvis, where ultrasound shows hypervascularization in the thickened wall and clot in the lumen.
Emphysematous cystitis is an uncommon complication of urinary tract infection, and ultrasound shows intramuscular echogenic foci accompanying gas-induced reverberation artifact.
Tuberculous cystitis develops in approximately one third of patients with upper urinary tract tuberculosis. In the early destructive phase of the disease, ultrasound shows thickening of the mucosa with an irregular margin due to coalescing mucous tubercles and ulcerations. In the late stage of the disease, the ultrasound bladder is reduced in size with a thickened wall due to transmural fibrosis.
With schistosomiasis, the walls of the bladder and ureters are thickened, uneven and poorly stretchable; their echogenicity can be increased due to calcification, which usually affects the intramural spaces and does not interfere with the normal contraction of the bladder. Poor emptying of the bladder means the presence of an acute inflammatory process, as well as a long-term or recurrent infection. Hydronephrosis and hydroureter, a thick sediment in the renal pelvis as a result of the addition of inflammation of the urinary tract, can also be detected.
Hyperechoic formations in the thalamus
The thalamus is a large paired collection of gray matter in the lateral walls of the diencephalon. Hyperechoic formations in the thalamus are detected in 4% of people with organic lesions of the nervous system. In most cases, they indicate tumor lesions. This pathology ranks fifth among oncology of other localizations, inferior to neoplasms in the uterus, lungs, and gastrointestinal tract.
Seals in the thalami occur in patients of any age, but most often in puberty and at the age of 45-50 years. The exact cause of pathological inclusions is not known. Scientists suggest that they are associated with the late active development of cells that were previously dormant. Also, do not forget about exogenous and endogenous factors: infections, hormonal disorders, injuries.
The symptoms of pathological compactions are based on the histostructure of the tumor. Patients experience increased intracranial pressure, which provokes headaches and dizziness, bouts of vomiting, changes in the bones of the skull, damage to the cranial nerves and psyche. Treatment of these conditions depends on the patient’s age, the characteristics of his body and the volume of the hyperechoic compaction.
Source: ilive.com.ua
Wall thickness, calcification and structure
During an ultrasound examination, a diagnostician can detect echo-dense structures that appear on the screen as light, almost white spots. The equipment also makes it possible to differentiate these objects based on the presence of an acoustic shadow. It occurs in cases where the area is so dense that it does not allow a sound wave to pass through it.
Hyperechoic inclusions, based on how they are visualized on the monitor and the presence/absence of an acoustic shadow, are divided into three groups:
- Significantly sized formations with the presence of an acoustic shadow. This picture is typical for stones and macrocalcifications. Sometimes this is what areas of sclerosis (connective tissue that has replaced functional tissue as a result of a necrotic process) or hematoma (bleeding in the kidney tissue) look like, in which a large amount of calcifications have been deposited over time.
- Large, moderately dense inclusions with no acoustic shadow. This is what benign neoplasms can look like on ultrasound - fibromas, oncocytomas, hemangiomas, as well as fluid-filled cavities - cysts (dense). Sclerotic tissue areas, accumulations of very small kidney stones (sand), or abscess areas may also have medium density.
- Small inclusions of white color that look like luminous dots on the monitor. These can be either very dense, but small calcifications, or psammoma bodies - round-shaped formations up to 3 mm in size, having a layered structure. The latter are based on protein-lipid complexes. Such inclusions are denser than any tissue of the human body; their presence in the kidneys can be a symptom of a malignant neoplasm.
In real conditions, changes in the ultrasound picture are rarely homogeneous; more often, inclusions contain a combination of hyperechoic structures; for example, an area of sclerosis may also contain calcifications.
The wall thickness is 2-4 mm, the contours are smooth. Any thickening of the walls indicates pathological changes. It is caused by various reasons.
- A diverticulum (protrusion) of the wall leads to the fact that urine first comes out of the body of the bladder, and only then from the diverticulum. If urine remains in the pouch, the pouch becomes inflamed, leading to local thickening of the wall.
- The bladder is susceptible to a parasitic disease such as schistosomiasis. It is caused by fluke parasites that lay eggs in the walls of the organ. The larvae die, but fibrosis occurs at their location - the proliferation of connective tissue, leading to thickening of the walls.
- If there are problems with the prostate gland, stagnation of secretion occurs, and against this background, foci of calcification form on the walls of the bladder. An advanced infection leads to the fact that the body begins to fight it itself, enclosing it in a calcium shell.
- With age, the structure of the muscular membrane of the organ changes, it becomes deformed and stretched.
Features depending on the organ
Hyperechoic formations appear in various organs of the human body. They are found in soft tissues or inside cavities. Formations are distinguished according to the following characteristics:
- form;
- size;
- contours;
- intensity of brightening in the image.
Based on these criteria, the specialist suggests a particular disease.
The hyperechoic neoplasm here is a tumor; more often it is malignant. Represented by a light spot of irregular shape.
Completely clear liver tissue combined with a decrease in size is a sign of cirrhosis. This is a disease in which normal liver tissue is replaced by scar tissue.
Liver cysts can be detected due to the reverberation effect. Once in the cavity, ultrasound is reflected several times from its walls and attenuates. The image shows the light walls of the cyst with a darkening in the center.
Read a detailed article about formations in the liver.
In the video you will see the hyperechoic walls of the liver portal system:
Gallbladder
Hyperechoic formations of the gallbladder are located inside it or on the wall.
- Sludge is a thick hyperechoic suspension of bile at the bottom of the bladder. Represented by a white stripe along the bottom contour.
- Polyp. Formed by cholesterol deposits, it grows from the wall of the organ. It has a wide base and elongated shape. Size up to 4 mm.
- The stone is compressed bile salts. It looks like a bright white spot at the bottom of the bubble. There is always an acoustic shadow. The shape of the stones is often round.
It is easy to distinguish sludge or stone from a polyp. The stones move when the body position changes, but the polyp remains in place.
A hyperechoic focus in the uterine muscle is a fibroid or malignant tumor. With fibroids, an increase in the organ itself and its deformation are simultaneously observed.
A hyperechoic formation may be a uterine polyp or a menstrual blood clot. To confirm this, an ultrasound should be done 3-4 days after menstruation.
If a hyperechoic formation is detected, shaped like the letter T, this is an intrauterine contraceptive. It has clear contours and is located in the middle of the organ.
Breast
Dense neoplasms in the mammary gland occur against the background of hormonal imbalances or inflammation:
- fibrous mastopathy - rounded light formations with an acoustic shadow;
- mastitis - linear areas of clearing or nodes;
- malignant tumor is a formation with unclear contours.
To distinguish between neoplasms, mammography and puncture are performed.
Bladder
Most often, stones are found here - small light inclusions with an acoustic shadow. They have different shapes and sizes. At the initial stage of urolithiasis, sand is detected - a hyperechoic suspension.
The bladder is affected by the infectious disease schistosomiasis. Many pinpoint hyperechoic inclusions are found in its wall.
Hyperechoic formations are often stones. Small white inclusions located in the cups provide an acoustic shadow. They have a round or coral shape.
A kidney tumor is usually located on its surface. It is represented by a light, rounded growth. A benign tumor has an even lighter rim - the capsule.
Thyroid
The hyperechoic area is a tumor of the thyroid gland. A light, round formation with clear contours. Inside there may be even denser areas - calcifications.
A dense formation in the ovary with unclear contours and a dark border around it is cancer. A tumor with a capsule around it and a heterogeneous structure is a teratoma. This is a congenital ovarian cyst containing fat, hair, and teeth.
Ultrasound of the fetus
When examining pregnant women, the fetus sometimes reveals a GEF - a hyperechoic focus - in the left ventricle of the heart. Most often, it does not matter for the further development of the fetus. The GEF in the heart is an accumulation of calcium salts or an additional chord - an outgrowth of the ventricular wall.
But sometimes it is a sign of chromosomal abnormalities. If a woman has risk factors, she undergoes additional examination. A needle is inserted into the amniotic sac and a small amount of water is taken for analysis.
The same examination can be done in the placenta. The analysis identifies any genetic abnormalities.
Watch a video about fetal GEF:
Bladder tumors on ultrasound
Although ultrasound is not the primary imaging modality for staging bladder tumors, it can provide general information about the depth of tumor invasion into underlying muscle or living fat tissue, and colorectal dosage can reveal tumor vascularity. Ultrasound is also useful in showing non-neoplastic bladder lesions such as stone, cystitis, diverticulum and ureterocele.
Most bladder tumors are multiple, but are usually localized in one area. Such tumors are characterized by the appearance of polypous growths (exophytic form). In this case, you should try to establish whether there is germination of the wall of the bladder or not. Some tumors cause local thickening of the bladder wall due to infiltrating growth (endophytic form).
With schistosomiasis, as well as with a tumor, hyperechoic areas can be detected due to encrustation. A blood clot and a tumor look identical on ultrasound and are combined with hematuria. 2. Benign tumors of the bladder (polyps) are very rare, mobile and have a thin stalk (cystoscopy, biopsy).
Thickening of the tumor stalk indicates the presence of inflammation, but more often it is a sign of bladder cancer. 3. Granulomas (for example, tuberculosis) cause multiple local thickenings of the wall, and with long-term disease, a “microcystis” is often formed - a small bladder, painful when stretched, which leads to frequent urine discharge.
Any chronic infection reduces the capacity of the bladder. With schistosomiasis, multiple flat plaques or polypous structures often form. Tumor lesions of the bladder, as a rule, are not accompanied by pain when stretched. 4. Trauma. If, after an injury, local thickening of the wall of the bladder is determined, a pelvic examination is performed to exclude the presence of fluid (blood or urine) outside the bladder.
Most bladder tumors are transitional cell carcinomas, accounting for about 90% of all primary malignant lesions. Men are more often affected than women, and about a third of bladder transitional cell carcinomas are multifocal at the time of diagnosis (Figure 3).
They most often occur at the base of the trigone or bladder or on the lateral walls. They show different growth patterns, including papillary, infiltrative, and mixed papillary and infiltrative. On ultrasound they appear as polypoid or plaque-like lesions. Bladder inflammation, swelling, or postoperative changes may mimic a bad infiltrative tumor.
Figure 3. Multiple cell carcinomas of the bladder in a 74-year-old man. Ultrasound of the bladder in the transverse plane shows multiple papillary tumors (arrowheads) in the bladder.
Transit cell carcinomas often have calcification that is caused by dystrophic calcification, usually on the necrotic surface of the tumor. A displaced bladder tumor shows posterior sound shadows and flickering artifacts that occur when crystalloid material or the rough surface of the lesion is sampled with Doppler ultrasound (Fig. 4).
Sometimes bladder tumors are detected by transrectal ultrasound performed to evaluate the prostate. Small bladder tumors in the trigone or neck area are particularly well demonstrated by transrectal ultrasound (Fig. 5). Color Doppler ultrasound (CDUS) shows tumor vascularity and often shows linear vessels in the tumor pedicle.
The depth of wall penetration and involvement of adjacent organs are the most important elements in the staging of bladder cancer. Ultrasound is not an imaging modality for staging bladder tumors, but the depth of tumor invasion into the overlying muscle and primary adipose tissue can be suggested [11,12].
A papillary tumor without bladder contour deformation indicates the absence of significant invasion of the underlying muscle (Fig. 6). A tumor with invasion into the overlying muscle shows rigidity and deformation of the bladder contour beneath the tumor (Fig. 7). Involvement of perivesic fatty tissue may be suggested when the tumor extends beyond the expected bladder contour (Fig. 8).
Transrectal ultrasound may show extension of the bladder tumor toward the prostate gland, showing a poorly defined hypoechoic lesion in the prostate gland continuous with the bladder tumor. CDUS may show prominent vessels at the interface between the tumor and the prostate gland, indicating tumor invasion of the prostate. Figure 4.
Calcified transitional cell carcinoma of the bladder in a 54-year-old man. (A) Longitudinal ultrasound examination of the bladder shows a mass with an echogenic surface (arrow) and posterior sound shadowing, suggestive of a calcified mass. (B) Doppler ultrasound shows flickering artifact occurring on the surface of the lesion, indicating calcification.
UB = urinary bladder. Figure. Small transitional cell carcinoma near the bladder neck in a 47-year-old man. (A) Transrectal ultrasound in the transverse plane shows a small polypoid mass (arrow) near the bladder neck. (B) Color Doppler ultrasound shows a vessel within the pedicle of the mass (arrow). P = prostate.
Squamous cell carcinomas represent 5% of bladder cancers and are the most common nontransitional cell tumor of the bladder. They are usually associated with chronic irritation from urinary stones, long-term catheters, chronic or recurrent infection, and schistosomiasis. Although squamous cell carcinomas cannot be differentiated radiologically from transitional cell carcinomas, they usually appear as sessile masses with or without extractive extension.
Papillary tumors or predominantly intravesical growth patterns are not characteristic of squamous cell arcinomas. The prognosis of this tumor is poor, since leiomyomas are the most common, with a tendency to infiltrate early. Adeno-epithelial benign tumors of the bladder.
They are characterized by the presence of less than 2% of the bladder with slow and non-invasive growth, without cancer. They usually occur in the dome and destroy the overlying mucosa (Fig. 9). trigone of the bladder [7,13]. Adenocarcinomas may be other benign non-pithelial tumors of the bladder associated with chronic irritation.
Cystitis glan- include neurofibromas, ganglioneuromas and extradularis, bladder exstrophy and remnants of the adrenal pheochromocytomas (paragangliomas) are also associated with adenocarcinoma [7,14,15]. These tumors are non-epithelial mesenteric bladder tumors [13]. Calcification is more common in chymal tumors, and ultrasound usually shows adenocarcinomas than in other tumors.
Another rare demarcated, lobulated, hypoechoic mass in bladder carcinomas is the bladder wall small cell carcinoma, convex both internally and externally and carcinosarcoma [7]. bladder (Fig. 10). Hemangioma is a benign congenital tumor usually found in children and young adults.
The most common histologic type is cavernous hemangioma, with other types being capillary and venous hemangiomas. Most of them involve the submucosal and detrusor muscles. Bladder hemangiomas usually appear hyperechoic on ultrasound. They are often calcified and ultrasound shows posterior sound shadowing (Fig. 11).
Rare sarcomas of the adult bladder include leiomyosarcoma, fibrosarcoma, and osteosarcoma. The radiological findings of these sarcomas are nonspecific, and differentiation between them or from large invasive transitional cell carcinoma is difficult [7]. Rhabdomyosarcomas are the most common pelvic malignancy in the pediatric group, which can arise from the bladder wall itself or from adjacent structures and secondarily involve the bladder.
Lymphoma of the primary bladder is extremely rare, and secondary involvement of systemic lymphoma is more common. Irregularity, thickening, and nodularity of the bladder wall are nonspecific radiographic findings and are radiographically indistinguishable from transitional cell carcinoma [7].
Hyperechoic formation in the prostate
The main cause of hyperechoic formation in the prostate is inflammatory lesions of the gland. If high-density inclusions were detected during an ultrasound examination, then this is a reason to undergo additional tests. First of all, this is a bacteriological culture of prostate secretions, a smear from the urethra for infection.
Bright light inclusions of the prostate on the monitor of an ultrasound machine may indicate neoplasms of phosphorus and calcium. Their size ranges from 2-20 mm. Prostate calcifications are characterized by a special form. Stones may indicate benign hyperplasia or chronic prostatitis. In most cases, high-density tissue is detected in men over 50 years of age.
Calcifications in the prostate gland are associated with many factors, let's consider them:
- Lack of meaningful sexual relations for a long period of time.
- Sedentary work and sedentary lifestyle.
- Physical inactivity.
- Frequent constipation.
- Chronic infectious lesions of the body.
- Poor diet with a predominance of fatty foods.
- Regular hypothermia of the body.
Hyperechogenicity of this nature does not require treatment and is not accompanied by painful symptoms. The main contraindication for the deposition of calcium salts in the prostate is massage of this organ. This is associated with a high risk of injury and stagnation of prostatic secretions. If calcifications occur against the background of chronic prostitis, surgery is performed.
What could it be?
Gallbladder stone
If a doctor sees an acoustic shadow behind a dense formation in the gallbladder, he first of all thinks about a gallbladder stone.
Agree, a stone is a very dense formation, so dense that ultrasonic waves are not able to penetrate through it. That is why a dark path, or “acoustic shadow,” is formed behind it.
1 - stone
2 - gallbladder
3 - acoustic shadow
4 - liver
But, unfortunately, not everything is so simple.
Gallbladder polyps
Some gallbladder polyps have the same high density. These are polyps “impregnated” with cholesterol, the so-called cholesterol polyps.
A polyp by its nature is a soft tissue formation, and therefore it usually reflects only part of the ultrasonic waves. The rest of the waves pass through it.
In such cases, it is displayed on the screen of the ultrasound machine as a formation of medium echogenicity, that is, as a gray formation. Such polyps never give an acoustic shadow behind them.
And only when the polyp tissue is replaced by cholesterol does the polyp become as dense as a gallstone. In this case, it is quite difficult to distinguish a polyp from a stone.