Transabdominal ultrasound of the internal organs of the pelvis is a diagnostic procedure that determines what is happening to the body and what abnormalities are present. Examinations are prescribed for men and women when indications are identified. Diagnostics is easy to perform, has a minimal number of contraindications, and is safe for the body.
Why do you need a transabdominal ultrasound?
Women are recommended to attend preventive examinations by a gynecologist at least twice a year. Barely noticeable pain or pulling sensations in the lower abdomen may indicate the development of diseases affecting the reproductive system. If the pathology is not detected in time and does not get rid of it, the risk of infertility increases.
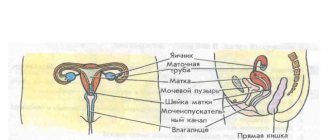
Transabdominal ultrasound of the pelvic organs allows you to assess the condition of:
- uterus;
- fallopian tubes;
- ovaries.
These organs are responsible not only for the ability to conceive and bear a child normally. They affect the general condition of the body because they produce hormones necessary for the normal physical and psychological health of a woman.
Androgens, estrogens and progesterones that the ovaries produce affect not only hormonal levels. The level of development of adipose tissue, bone strength, the appearance of the skin and the condition of the mammary gland depend on the hormonal balance.
In parallel with the ultrasound, the specialist can palpate the problem organ
It is recommended that women of reproductive age undergo a preventive ultrasound of the pelvic organs at least once every 1-1.5 years. Only a few adhere to such a schedule. Most women consult a doctor only after the appearance of alarming symptoms.
For medical reasons, transabdominal ultrasound examination is prescribed for the following pathologies:
- suspected ectopic pregnancy;
- disruption of the menstrual cycle;
- pathological periods (scanty or too heavy);
- suspected neoplasms;
- pain syndrome;
- suspected infertility;
- inflammatory diseases of the reproductive organs;
- inflammatory processes in the organs of the urinary system.
Ultrasound is also required after surgery in the pelvic organs, after installation of an intrauterine device, and during pregnancy.
Decoding the results
During the study, the doctor will evaluate the size of the internal organs, the degree of enlargement, the presence of cysts, polyps and adhesions. The interpretation of results for women differs from that for men. When studying the body of the stronger sex, special attention is paid to the organs of the prostate and seminal vesicles.
Normal ultrasound results in men:
- prostate: size - 2.5x2.3x1.5 - 4.5x4.0x2.5 cm, volume - 30 cm3. The heterogeneous structure of tissues may be due to the presence of neoplasms, cysts and the inflammatory process. An enlarged prostate gland indicates prostatitis;
- seminal vesicles: size - 1 cm, shape - elongated. An increased size may indicate the presence of inflammatory diseases;
- bladder: volume - from 350 to 750 ml, shape - round or oval. The walls are up to 3 mm thick, clear and even. Sediment, blood clots and stones indicate pathology; thickening of the walls may indicate chronic cystitis.
Women have smaller normal bladder sizes than men. The normal volume is from 250 to 550 ml. With cystitis, thickening of the walls is also observed.
Ultrasound diagnostics will show:
- uterus: size - from 50x50x45 mm (for women who have not given birth) to 70x60x50 mm (for women who have given birth). An increased size may indicate the development of fibroids or endometriosis; a decreased size may indicate underdevelopment of the organ;
- endometrium: thickness is determined depending on the day of the menstrual cycle. Hyperechogenicity indicates the presence of neoplasms;
- cervix: size – 40x30 mm, long canal – up to 3 mm. Changes and deformation of the structure and contours, as well as expansion of the canal indicate pathology;
- ovaries: volume - 10 cm³, size - 37x30x22 mm. Before menstruation they are enlarged and the contours are uneven. The left and right ovaries may differ in size;
- fallopian tubes: when visualized, they may be a sign of an ectopic pregnancy or an inflammatory process. Should not be visible on transabdominal ultrasound.
Any deviation should be investigated further. The doctor will prescribe laboratory tests and a repeat ultrasound if there is a suspicion of the disease. Following simple preparation rules will help make the study as informative as possible.
How is a transabdominal examination performed?
The procedure is absolutely painless, but if you are sensitive, it may cause slight discomfort. In the specialist’s office, the patient undresses from the waist down, exposes her stomach and lies on her back.
During external ultrasound, the skin in the pelvic area is lubricated with a special gel, which ensures contact of the sensor with the body. With light pressure, the device moves over the skin. Using sensors, a dynamic, accurate image of the tissues and structure of the organs being examined is obtained. The picture can be enlarged many times.
Rear access
8.5. Surgical approaches to the sacrum and sacral canal.
Tumors found in the sacral region vary in variety. The following types of tumors are distinguished (Hulen CA et al. 2006, Klimo P et al. 2003):
— Tumors located in the sacral canal (ependymomas, neuromas);
— Tumors limited to the bone structures of the sacrum;
— Tumors spreading from bone structures ventrally into the pelvic cavity.
Taking into account the types of tumors, the following approaches to the sacrum are used (Alla AH et al. 2005).
— Rear access
— Transperineal access
— Anterior approaches (transabdominal, retroperitoneal).
— Combined accesses
From this approach it is most easy to identify neural structures located in the sacral canal and separate the tumor from them. Access is performed both with the patient lying on his side and on his stomach. When planning sacral fixation, a prone position is necessary. A longitudinal incision is made over the sacrum. Skeletonization of the sacrum is performed. The vessels emerging from the intervertebral foramina are coagulated. If the tumor is localized only in the sacral canal, skeletonization is limited to the intervertebral foramina, but if necessary (with a tumor of the bone structures), it is possible to expose the sacroiliac joints and dissect the dorsal sacroiliac ligaments. A laminectomy of the sacrum is performed. Subsequently, the main stage is performed, the tumor is removed. After the main stage, the wound is sutured in stages (
Klimo P et al. 2003, Pogoda P et al. 2005). The approach allows one to reach the caudal presacral space. This approach can be used independently, but in most cases it is combined with others, most often with the posterior median approach. Its combination with a posterior approach allows for low sacral resection (below S3). However, this approach is not recommended for high resections of the sacrum, since it is difficult to separate soft tissue from the sacrum, and the risk of damage to the great vessels and rectum increases.
Access technology.
A midline incision is made from S1 to the end of the coccyx. The dorsal surface of the sacrum is skeletonized. Laterally from the sacrum the gluteus maximus muscles, ligaments sacrotuberous and sacrospinous, are separated. At the point of attachment to the sacrum, the coccygeal and piriformis muscles intersect. Access to the presacral space is obtained after dissection of the anococcygeal ligaments and anosacral muscles. The coccyx can be removed to increase access to the presacral space. In the presacral space, the tumor is manually separated from the surrounding tissue. During resection of the sacrum, the sciatic nerves, n. pudentus, as well as the gluteal arteries. A laminectomy of the sacrum is performed dorsally, all sacral nerves are isolated and protected (Zhang HY et al. 2003).
With this approach, basically only low resection of the sacrum is performed; the sacroiliac joint is not damaged, so the pelvic ring is not destabilized. Taking this into account, such access and operation do not require subsequent fixation. After resection of the tumor and the sacrum, a large cavity is formed below S3, which requires careful hemostasis and the establishment of active drainage. The wound is sutured in layers (Nader R et al. 2003).
They are often combined with posterior approaches, since it is impossible to completely remove the tumor from one anterior approach and preserve the sacral nerves (Mauroy B et al. 2003).
It is most convenient for exposing the anterior surface of the sacrum at the S1-S3 level (Fourney DR et al. 2005). The patient is positioned on his back, and a lower median laparotomy is performed. The intestines are displaced, the anterior surface of the sacrum is examined. The internal iliac artery and vein are highlighted around. The internal iliac artery and vein are then ligated with two thick ligatures. The rectum is shifted to the side, and the peritoneum is crossed behind the rectum. This allows the rectum and sigmoid colon to be moved away from the sacrum. After ligation of the internal iliac vessels, the sacrum is partially devascularized, but, nevertheless, bleeding from the presacral veins is often significant, requiring careful hemostasis (Papalambros E et al. 2005). For high resections of the sacrum, it is necessary to isolate and move the common iliac vessels to the sides and ligate the sacral arteries (Glatt BS et al. 2006). The ventral intervertebral foramina on the sacrum serve as the best guide to level and medial-lateral position. The ventral surface of the sacrum is then skeletonized, and the nerves emerging from the intervertebral foramina are isolated and preserved. Subsequently, osteotomy is performed with a drill or osteotome (Bohinski RJ et al. 2005). The lateral border of the osteotomy is usually the sacroiliac joint. Care is taken not to damage the dura mater and nerves passing through the sacral canal. Typically, to perform radical removal of the sacrum, this approach must be combined with the dorsal one (Osaka S, Kodoh O, Sugita H et al. 2006).
After completion of the main stage, active drainage is installed and the wound is sutured (Dickey ID et al. 2005).
similar to the transabdominal approach. An anterior paramedian incision is made, and oblique incisions are also possible. After dissection of the abdominal walls, the peritoneum is bluntly peeled off from the inner surface of the pelvis along with the sigmoid and rectum. The peritoneum is displaced from the iliac vessels and ureters. Subsequently, the access is similar to the transabdominal one. In contrast to the latter approach, the retroperitoneal approach provides less visibility and the ability to visualize the side of the sacrum opposite to the approach (Rousseau MA et al. 2005, Osaka S, Kondoh O, Yoshida Y et al. 2006).
Combined
approaches use a single-stage or staged combination of transperitoneal and posterior median access. Simultaneous combined access requires the patient to be positioned on his side. In this position, it is difficult to fix the pelvis, lumbar spine, and remnants of the sacrum. In cases where fixation is planned, a staged approach is performed - first transabdominal, then posterior median. Often, a transabdominal approach is required again to complete the operation (Samartzis D and Savot. 2006).
What the research results show
During the examination, the specialist can assess the position and size of the uterus and ovaries, the degree of passage of the fallopian tubes, the features and thickness of the inner layer of the uterus. Pathological phenomena are also detected - the presence or absence of fluid in the pelvis, neoplasms or adhesions.
In most cases, one ultrasound examination is enough to assess the condition of the reproductive system and make a diagnosis
Additionally, auxiliary tests or other types of ultrasound may be prescribed.
After deciphering the results, the following problems are identified:
- neoplasms in the ovaries or uterus;
- congenital pathologies;
- polycystic disease;
- malignant tumors;
- functional disorders;
- inflammatory diseases;
- endometriosis.
If one of the pathologies is identified, further prescriptions and treatment are prescribed by the attending physician.
How to prepare?
To obtain normal external access to the pelvic organs, simple preparation of the body is necessary. Access to the internal genital organs from the abdominal wall is “blocked” by the bladder. For effective diagnosis, it must be filled: the liquid transmits ultrasound well, allowing one to assess the condition of “hidden” organs.
To ensure that the bladder is full, you need to drink about 1.5 liters of non-carbonated liquid 40-50 minutes before the scheduled ultrasound time
You cannot go to the toilet until the ultrasound examination is completed. If you are prone to flatulence, a simple diet is prescribed a day before the procedure. You will have to exclude vegetables, sweets, flour and fruits. If there is gas in the intestines, the view of some organs will be difficult.
When can an ultrasound be performed?
Due to the characteristics of the reproductive organs of women, the schedule of the menstrual cycle is taken into account when setting a date for the study. The optimal period is 5-7 days after the end of menstruation. This is justified by the fact that during the cycle the functional state of the pelvic organs changes, which may affect the results of the study.
In the last phase of the cycle, the overgrown epithelium may resemble pathology, so the time for the examination should be prescribed by a doctor
If you need to directly assess the functional state of organs, ultrasound will have to be performed several times a month. This will allow you to trace natural processes, from the onset of ovulation to the dynamics of follicle development.
During menstruation, transabdominal ultrasound is permitted. This is especially true for women whose periods last about a week: the period suitable for examination occurs before their end.
In case of exacerbation of the pathological condition or acute pain, ultrasound can be performed on any day of the cycle in a special order. Also, examinations are carried out at any time during pregnancy.
Preparing for an ultrasound
There is no need to carry out any special preparatory procedures. For the accuracy of the study and a clearer picture, it is recommended to avoid gas-forming products on the eve of the ultrasound. Flatulence can make accurate diagnosis difficult.
It is recommended to drink plenty of water 1 hour before the test. During transabdominal ultrasound, the bladder must be full so that it displaces the intestines from the screen.
In emergency cases, when an ultrasound is performed urgently, filling the bladder can be done using a catheter. Men can come for an appointment at any time; for women it is important to choose the right day of the cycle. Usually this is the period after menstruation (7-10 days).
Benefits of the study
Transabdominal ultrasound examination is painless and does not cause much discomfort. During the examination, a specialist can assess not only the condition of a specific “problem” organ, but also evaluate the appearance of neighboring ones, obtaining a general panorama. This increases the likelihood of making an accurate diagnosis.
The condition of the pelvic organs in virgins can only be assessed in this way. An equally accurate transvaginal ultrasound, during which a probe is inserted into the vagina, is not available in this case.
Ultrasound during pregnancy
This diagnostic method is very widely used during pregnancy. After all, it is safe and does not cause any discomfort to the expectant mother. In this case, ultrasound helps to obtain a large amount of information.
Transabdominal ultrasound during pregnancy allows you to assess the condition of:
- child;
- amniotic sac;
- placenta;
- ovaries.
Also, during an ultrasound, serious anatomical abnormalities or congenital changes in the fetus can be detected. Most prenatal ultrasound procedures are performed through the abdominal wall, especially in the later stages. Research shows that ultrasound is not harmful to both mother and baby. There are no side effects to this procedure. Moreover, this scan is considered the safest, because it does not use radiation, as, for example, in x-ray examinations.
Disadvantages of transabdominal ultrasound
If you do not carefully prepare, the results of the examination may be erroneous, and some organs may not be examined. Certain problems with visibility also arise in overweight people: adipose tissue becomes some kind of barrier to the rays.
Difficulties in performing ultrasound may also arise with a thickened abdominal wall.
Some of the ultrasonic waves are absorbed by the tissues of the abdominal cavity, and the more of them, the less clear the resulting image. The organs will not be detailed enough, which affects the diagnosis. The specialist may simply miss some problems.
The frequency of the transabdominal transducer also affects the clarity of the resulting image. The information content of this type of ultrasound is somewhat inferior to the transvaginal method. Therefore, to clarify the diagnosis, two types of research may be needed.