Preparing for the study
48 hours before the x-ray, you must follow a diet according to which you should exclude foods that stimulate gas formation (legumes, cabbage, brown bread) from your diet.
At least 12 hours must pass between the last meal and the x-ray examination. The day before, the patient takes enterosorbent medications and is given a cleansing enema, which can be repeated several hours before the test if necessary.
Activated carbon
With high-quality preparation for the study, the image turns out to be the clearest and most diagnostically valuable.
X-ray examination of the pelvic bones
To most accurately determine pathologies of the pelvic bones, radiography is most often used. This is a simple technique, the result of which is highly informative and accurate. The main advantages of x-rays are:
- accessibility – there is an X-ray machine in almost every clinic;
- painlessness;
- relative safety;
- efficiency - together with decoding, this diagnostic procedure lasts approximately 10 minutes;
- simple preparation for a pelvic x-ray (how to do it will be described below).
How is it done?
Typically, radiography is performed in a direct (antero-posterior) projection. The examination is carried out in a strictly horizontal position of the patient (any deviation or rotation of the patient can lead to distortion of the image). Description of installation:
The patient lies down, legs extended, internally rotated approximately 15° (however, internal rotation should not be performed if there is a suspicion of a fracture or dislocation in the hip joint), and a radiolucent pad is usually placed under the knees. Elbows on the sides of the body, hands on the chest (arms can be extended along the body).
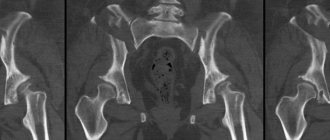
The x-ray should produce a symmetrical image of the pelvis, both halves, a clear image of the sacrum, intervertebral foramina of the sacrum, as well as the branches of the pubic and ischial bones. The bone substance should be well visualized, the contours of both acetabulums and the neck of the femur should be clearly visible.
Scheme of plain radiography of the pelvis: direct projection (A), internal oblique projection (B)
If any changes are detected or data that requires clarification is obtained, the images are taken:
- In the posterior axial projection of the pelvic inlet (Lilienfeld modification).
- In the posterior axial projection of the pelvic outlet (according to Taylor).
- To visualize the acetabulum in the posterior oblique projection of the pelvis.
- In the axiolateral inferior superior projection of the hip joint and proximal femur, as well as its modification according to Clements-Nakayama.
- Aimed for visualization of the sacroiliac joints in the posterior axial projection and posterior oblique projections.
When examining after injuries, if the patient is stable, an X-ray of the pelvis is taken in the emergency room; if the patient’s condition is serious, X-rays can be performed directly in the intensive care unit using mobile X-ray machines (included in the standards for examining patients with polytrauma).
Do I need to prepare for a hip x-ray?
Preparing for an x-ray of the hip joint is no different from many identical procedures and is particularly difficult. There is no need to adhere to a specific diet and nutrition regimen. However, given the proximity of the intestinal loops, you should give a cleansing enema the night before or in the morning before the examination. This is done so that feces and gas in the colon cannot affect the quality of the x-ray image, leaving dark spots on it or, conversely, light spots that can mislead the diagnostician.
X-ray of the leg + photo
The enema can be replaced with any laxatives, but you need to drink them in the evening so that the intestines are cleansed by the morning of the procedure. In cases where contrast-enhanced radiography of the pelvic bones is prescribed, the patient must be tested for a radiocontrast agent that will be used during the examination. This is done to determine whether the subject has allergic reactions to the components of the drug.
Immediately before starting the procedure, the patient must get rid of clothing that restricts movement and items containing metal. You can use medical clothing specially designed for such purposes. To reduce the negative impact when taking X-rays, nearby organs that do not need to be examined are covered with lead protection - capes, aprons or pillows. Warn the patient about the need to remain still and proceed to positioning him.
This study in childhood
In a child, this type of study is often used to diagnose such a common disease as congenital hip dislocation. Joint damage is often unilateral. After examining the child by a doctor and if there is a suspicion that the child has a pathology of the hip joints, the doctor prescribes a diagnosis:
- If the child is under 4 months old. ─ ultrasound examination of the hip joints.
- If the child is older than 4 months. ─ X-ray examination may be used.
When interpreting a radiograph in a child, it is important to remember that at an early age the acetabulum and femoral heads consist of cartilaginous tissue and do not create contrasting shadows.
X-ray signs of hip instability include:
- Smoothness of the articular cavity.
- Late-appearing ossification nuclei in the femurs of a child.
In case of subluxation, along with the listed signs of instability, there is non-closure of the head of the child’s femur with the acetabulum.
For hip dislocation:
- Smoothness of the articular cavity.
- The femoral head is smaller than on the healthy side, flattened and located outside the socket.
Congenital hip dislocation
What will a CT scan of the sacroiliac joints show?
Various ailments of the sacroiliac joints are characterized by pain in the lumbar region, limited freedom of movement, and they often have serious consequences for the patient’s quality of life.
CT sacroiliac joint
Experts distinguish the following groups of diseases of the sacroilial joints:
- inflammatory processes - can be infectious and non-infectious (tuberculosis, brucellosis, Reiter's syndrome, ankylosing spondylitis);
- degenerative processes (osteoarthritis);
- SIJ dysfunction during pregnancy;
- injuries of the sacroiliac joint (bone fractures, rupture of articular structures).
Sacroiliitis or arthritis is an inflammatory disease of the sacroiliac joint. At an early stage, the pathology on computed tomography is manifested by widening of the joint space, marginal proliferation of bone tissue (subchondral sclerosis), and a decrease in the density of the sacrum and ilium of the pelvis.
Osteoarthritis or arthrosis is a chronic degenerative pathology of the sacroiliac joints against the background of a long-term inflammatory process, causing deformation and cessation of joint mobility. As the disease develops, computed tomography shows pronounced bone growths (osteophytes) and a reduction in the lumen of the joint space. In late-stage disease, CT scans can show hardening of the articular surfaces and the absence of joint space as a result of fusion of the joint surfaces (ankylosis).
Alternative techniques
Other research methods: ultrasound, CT, MRI can complement the picture of an x-ray examination and even completely replace it. The integrated use of several diagnostic techniques is indispensable, especially in case of multiple injuries (as a result of injuries):
- Ultrasound in this location is used mainly to determine the presence of bleeding in the abdominal cavity in patients with polytrauma.
- Computed tomography (CT) allows not only to more accurately diagnose the presence and location of fractures of the pelvic bones and proximal femurs, but also to determine the presence of injuries to the pelvic organs and concomitant injuries to the abdominal cavity, chest, and brain. If a violation of the integrity of large vessels is suspected, multispiral computed angiography (MSCT) is performed.
CT reconstruction of the pelvis in volume
- Magnetic resonance imaging (MRI), compared to CT, has the advantage of no ionizing radiation. This type of examination better visualizes changes in soft tissues.
But among its disadvantages: a long examination time, difficult access to the patient, as a result of which in acute pathology it is used less often than CT.
A doctor’s quick and competent choice of research method ensures a speedy diagnosis and initiation of treatment.
Features of the technique and its essence
Classic radiography works equally for all parts of the human body, so the pelvic circle is no exception. Unlike magnetic resonance imaging or computed tomography, x-rays are more focused on obtaining information about the condition of the bone structure. By changing the percentage of stiffness, other tissues appear on the image, but this is usually not enough to make an accurate diagnosis. Patients are sent for a CT or MRI scan.
Content:
- Features of the technique and its essence
- Preparatory stage
- Scheme of implementation
- When do children need x-rays?
But as for bone visualization, it is excellent for making a diagnosis regarding the pathology of this tissue of the body. Against the backdrop of modern methods of studying internal organs and body parts, this diagnostic is in consistently high demand due to its relative cheapness and ease of implementation. Therefore, if the patient suspects the most common pathologies of the pelvic bones, then it is much more beneficial for the wallet to use radiography.
This method will be a particularly successful diagnostic option if the examination is carried out on a digital device. It irradiates a person with a smaller dosage of radioactive rays, which has a positive effect on overall well-being. Searching for a digital camera has a number of other positive aspects, among which the most notable is the ability to instantly display the resulting image on the computer screen.
The information received, along with the radiologist’s report, can be recorded on digital media. But if the information is required in hand, then the x-ray technician can print the image on film and, together with the description made by the radiologist, provide it to the attending physician.
Most often, surgeons, orthopedists or traumatologists send you for examination. Moreover, it is not at all necessary that the reason for referral was a suspicion of a closed or open fracture. There are many other abnormalities affecting both the pelvic bones themselves and the hip joints. The condition of the latter is checked using radiography in identical positions and projections as the bones. This allows you to get a detailed picture of the clinical situation in one image, which helps to establish the extent of the lesion.
In addition, the image can provide information about the specific location of the lesion, perhaps even the degree of the disease, and the spread of the pathological process to neighboring areas. Such an integrated approach is especially important if the patient is suspected of having a neoplasm. Using a black and white image, you can find out whether there are metastases in neighboring tissues, or whether the process is only at the initial stage of development.
But other histochemical analyzes of the material taken during a biopsy, or the entire removed tumor during surgery, will help to accurately and reliably determine whether the tumor found is benign or malignant.
Since one image can provide an assessment of several structures and tissues of the area under study, these capabilities are used to not only identify the problem point. Based on the results obtained, the attending physician will decide which treatment format is ideal for this particular patient. We are talking about surgical intervention, or its alternative version - conservative treatment using medications and other means.
In the first case, the resulting image will become a kind of map of the state of the pelvic region inside, which will allow you to calculate the risks and percentage of successful outcome of the operation. Once completed, the patient may need to undergo this type of re-examination periodically. This is necessary to monitor the dynamics of recovery. If no positive changes are found within the specified time, then this is a reason to revise the previously approved therapy program. Even after osteosynthesis, regular checks are necessary to assess the ongoing successful fusion of the assembled fragments.
Other indications for radiography include the following:
- damage to the iliosacral and pubic joints;
- fractures of the neck, head, proximal femur;
- joint pathologies such as arthritis and arthrosis;
- dislocations;
- subluxations, including congenital ones;
- osteochondropathy of the femoral head;
- osteoporosis;
- tumors of any etiology.
Sometimes research is indispensable when it is necessary to confirm rare hereditary or acquired diseases.
The place of radiography in the diagnosis of hip joint diseases
The advantages of x-ray remain:
- Speed.
- Easy to do.
- Availability.
As an alternative to radiography, the following are possible:
- Ultrasound examination. It is actively used in young children, as well as for diagnosing soft tissue pathology, when high resolution of the method is not required.
- Magnetic resonance imaging (MRI) provides good image quality and high accuracy of detection, especially of lesions of non-osseous structures, including the condition of the ligamentous apparatus, and the presence of effusion in the joint cavity.
Magnetic resonance imaging
- Computed tomography (CT) creates a three-dimensional model of the area being examined, which greatly facilitates diagnosis. The image obtained using CT is of high quality. The main disadvantage is that due to the many images, the radiation exposure to the body is greater than with a regular x-ray. However, in some cases, computed tomography cannot be done without.
- Hip arthroscopy is performed for both diagnostic and treatment purposes. Allows you to examine the joint cavity using an arthroscope and immediately carry out the necessary manipulations. Like any invasive procedure there can be many complications.
Despite the emergence of ever new, more modern and high-tech research methods, it is radiography that plays a key role in most cases when quick and low-cost diagnosis and differential diagnosis of diseases of a given localization are required.
Tags: grip, bone, radiography, joint, hip
About the author: admin4ik
« Previous entry
Indications for computed tomography of the sacroiliac joints
This type of radiation diagnostics of the sacroiliac joints is prescribed for:
- lower back pain of unknown origin;
- injuries in the area of the sacrum and sacroilial joints;
- inflammatory processes in joints;
- rheumatic diseases;
- neoplasms;
- preparation for surgery.
CT picture of sacroiliitis. Arrows indicate areas of inflammation and ankylosis
How and where is it carried out?
Installation for radiography of hip joints
Before the examination, areas of the body that are not of interest to the doctor are covered with a special apron that screens out X-rays.
X-rays are taken in two projections: frontal and lateral.
- To obtain an image in a direct projection, the patient lies on his back with his legs extended, turned slightly medially (internal rotation is not carried out if there is the slightest suspicion of a fracture or dislocation in the hip joint).
- The lateral projection is obtained when the patient lies on his back, bending one limb at the hip joint. If movements in the joint being examined are very painful, you can bend the healthy leg.
If necessary, the doctor can prescribe diagnostics at the angle he needs.
An X-ray can be done in a public clinic at your place of residence, by taking a referral from a therapist, traumatologist, orthopedist or other specialist, as well as in any private medical center that has an X-ray machine. In an emergency, an x-ray is taken in the emergency room, in the emergency department.
Contraindications for examination
In the modern tomograph installed in our center, radiation exposure is reduced to minimal values, which makes it possible to safely perform computed tomography of the sacroiliac joint. However, even under such gentle conditions, there are a number of contraindications for CT of the sacroiliac joints:
- patient weight more than 150 kg;
- any stage of pregnancy;
- children under 5 years old;
- children from 5 to 18 years old without a referral from a doctor.
Features of pelvic x-ray in newborns
In newborn children, hip dysplasia is very often diagnosed. It is characterized by certain symptoms and to confirm or refute the diagnosis, the patient is sent for an x-ray. Without making an accurate diagnosis, it is impossible to build a further correct course of treatment, which means that the risk of the child becoming disabled subsequently may increase.
In such a situation, parents wonder whether it is possible to do x-rays of the joints and pelvic bones of a newborn child. There is no clear answer to this question. On the one hand, any radiation exposure to a child’s body entails the risk of developing various pathologies. From another point of view, if you correctly dose the radiation dose, then you can identify the pathology without harm and in a timely manner.
For reference! There is no guarantee that exposure to even a small dose will not affect the child in the future. For this reason, it is not advisable for infants, especially those under 3 months, to have an X-ray; it is better to get by with an MRI or ultrasound.
X-ray is an excellent and painless way to diagnose pathologies of the organs and bones of the pelvic joints, with a minimum of contraindications. The procedure is widespread and is performed in almost all medical institutions. In commercial clinics, this study is relatively cheap, and in government institutions, the image is taken free of charge upon the direction of the attending physician.
We will be very grateful if you rate it and share it on social networks