Synonyms: ANA, antinuclear antibodies, antinuclear factor, ANF, antinuclear antibodies, antinuclear antibodies, ANAs, Fluorescent Antinuclear Antibody, Antinuclear factor, ANF
Scientific editor: M. Merkusheva, PSPbSMU named after. acad. Pavlova, medical practice.
Autoimmune diseases, when the immune system attacks the body's own tissues, are considered one of the most dangerous. Most autoimmune pathologies are chronic and can cause serious disruptions in the functioning of internal organs and systems.
One of the most common tests used in the diagnosis of autoimmune conditions is the antinuclear antibody (ANA) test, which is performed in three ways:
- by enzyme immunoassay ELISA (total ANA level is determined),
- method of indirect immunofluorescence reaction RNIF (up to 15 varieties of ANA are detected)
- immunoblotting method.
What are antinuclear antibodies
Glow of antibodies in a microscope
Antinuclear antibodies are pathological components of the immune system that lead to the occurrence of autoimmune connective tissue diseases, such as systemic lupus erythematosus, Sjögren's syndrome and disease, and systemic scleroderma.
Antinuclear antibodies are immunoglobulin proteins produced by the protective cells of the human body (lymphocytes). Due to a malfunction of the immune system, the nuclei of one's own cells are recognized by it as foreign and harmful, which leads to the erroneous production of antibodies to various components of the cell nuclei.
In total, more than 190 nuclear components have been identified to which a pathological immune response can be developed, but about 20 of them have diagnostic value. The most important include antibodies to single- and double-stranded DNA, histones, nucleosomes and ribosomal P-protein.
The nucleus is found in almost every cell of the human body, with the exception of some blood cells. It is located inside the cell and is protected by its own membrane, cytosol and outer cell membrane. Antibodies are located in the extracellular environment and most often cannot directly contact the nucleus, damaging it. However, with any violation of the integrity of cell membranes, antinuclear antibodies, if present in the body, are able to bind to the components of the nucleus, forming insoluble complexes. They are the cause of various autoimmune connective tissue diseases.
The essence of the blood test for antinuclear factor
Before delving into the specifics of conducting research at the ANF, it is worth noting that the technique was invented and began to be used quite a long time ago - in the 60s of the last century. But it became widespread in diagnostic practice only in the early 80s of the 20th century after improvements. Back in 1961, scientist Beck used laboratory animal cells as a substrate, and only in 1982 Tan used the continuous human cell line HEp-2 to search for ANF.
Although the main purpose of using this test is to establish a diagnosis of lupus erythematosus, it is still considered a universal technique for other collagen diseases (CCD). The latter include:
Blood on RFMK - what is it?
- scleroderma;
- dermatomyositis;
- periarteritis nodosa;
- chronic active hepatitis, etc.
One of the most convenient, and therefore most often used, methods for determining antinuclear factor in the blood of patients is indirect immunofluorescence. The study is carried out by applying blood serum to cells of the continuous epithelioid line of human laryngeal adenocarcinoma HEp-2 (containing a certain number of nuclear antigens) using a labeled conjugate (compound) with antibodies.
This choice was not made by chance - HEp-2 cells are a very convenient substrate for studying biomaterials. They have rather large nuclei, and when planted on laboratory glass they grow in a single layer. Other human cell lines can be used as a substrate, but successful morphology and cultivation clearly make HEp-2 an irreplaceable material.
During diagnosis, when the patient's serum is incubated with a cell substrate, in the presence of ANA, they combine with the corresponding nuclear antigens. The binding sites of ANF with HEp-2 are determined using a conjugate labeled with fluorescein (dye). To evaluate the results of the reactions that have occurred, a fluorescent microscope is used, which makes it possible to differentiate the nature and extent of the resulting ligaments.
Fluorescence microscope for laboratory research ANF
Reference! Human HEp-2, in contrast to animal tissue cryosections, have a higher rate of cell division, which makes it possible to detect antibodies to antigens that are expressed only during division. Also, the human substrate lacks a cellular matrix, which reduces the quality of visualization of the studied luminescence.
Education mechanism
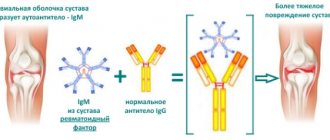
Antinuclear antibodies and receptors
Normally, the body’s own cells, even in a destroyed state, do not cause an immune response. However, malfunctions in the functioning of the immune system are constantly observed even in healthy individuals, and under unfavorable circumstances, immunity can form on any of the components of the cell. The body has a kind of “rejection” system for pathological antibodies; in most cases it works, the antibodies are destroyed without causing disease.
However, in some cases, antinuclear antibodies arise in large quantities and are not recognized by the body in time as pathological. This most often occurs with extensive sunburn, when millions of skin cells are damaged by ultraviolet radiation. The nuclei of dead cells end up directly in the internal intercellular environment of the body, where they are met by immune cells - lymphocytes and macrophages.
DNA from the nuclei, histone proteins and other protein and nucleic components can be so damaged by ultraviolet radiation that in some cases they are changed beyond recognition. This is what provokes immune cells to produce antibodies against them, as against foreign substances.
Normal ANA values
Absence of antibodies is normal
The normal value is the complete absence of antinuclear antibodies. In a screening ELISA test, a negative answer is most often recorded indicating the titer (dilution), for example: “Negative, < 1:160.” In a detailed immunoblot study for antibodies to different components of the cell nucleus, the response is often recorded for each type of antibody separately. For example: “AT to double-stranded DNA - negative; AT to PCNA - negative; AT to Scl-70 – negative.”
Sometimes AHA is detected in small quantities in healthy individuals (weakly positive), which may indicate a genetic predisposition to autoimmune diseases. The test result “Doubtful” may be caused by the presence of antibodies in a very low concentration, which is near the sensitivity thresholds of the medical test system for the analysis. Most often, after receiving a “Doubtful” result, it is recommended to repeat the analysis after 4-5 weeks.
Study of the results obtained
After all the necessary procedures have been carried out - taking the biomaterial and preparing it in the laboratory for research - the results are assessed and interpreted. This includes determining the titer (concentration) of antibodies and the type of glow. A significant parameter for diagnosis is a concentration value greater than 1:160. For example, during an exacerbation of rheumatism, it can exceed 1:640, while in the remission period there is a decrease to 1:160–1:320.
The type of luminescence shows the ANA targets, which is a particularly important clinical point that guides the doctor’s subsequent actions in prescribing diagnostic measures. Based on the nature of the luminescence of nuclei when using HEp-2, over 20 variants of nuclear staining will be determined, depending on the types of antibodies present in the biomaterial. The main ones include the following types of glow.
- Peripheral. The glow indicates the presence of anti-DNA antibodies, which confirms SLE. The main types of antigens for the peripheral type are histone proteins and DNA.
- Diffuse (homogeneous). This glow is observed in SLE, accompanied by damage to the kidney structure and similar CTDs, nephritis, scleroderma, as well as drug-induced SLE. Antigens in this type are represented by dsDNA, histonates and nucleosomes.
- Nucleolar (nuclear). This type is characteristic of the systemic form of scleroderma, and is determined by the presence of antibodies in patients - RNA polymerase 1, PM/Scl, NOR, U3RNP.
- Cytoplasmic. This type of highlighting indicates the presence of ANA to tRNA synthetases, namely Jo-1, and is observed in polymyositis.
- Granular. It is determined in Sjögren's syndrome, infectious mononucleosis, mixed CTD (Sharp syndrome, MCTD) and drug-induced lupus syndrome. The predominant antigens present for this type are SS-A, SS-B, Sm, U1-RNP, and PCNA.
- Coarse granular. It is typical for mixed CTDs and, according to many scientists, is associated with the presence of the RNP antigen.
- Fine granular. The presence of antibodies formed against ribonucleic proteins - ASSP (ACCP), SS-A, SS-B and others is determined. Such antibodies are characteristic of SLE, as well as its specific skin forms, rheumatoid arthritis, scleroderma, polymyositis, Sjögren's syndrome.
- Centromeric. This type is mainly observed in scleroderma. Although in one blood sample, especially in patients with diffuse CTDs, antibodies to various nuclear components can be detected in the separated plasma.
- Point inclusions in the core. This type is predominantly detected in liver diseases of an autoimmune nature. It can combine several fluorescent types, for example, nucleolar and fine granular, which is caused by antibodies to Scl-70.
Reference! It was noted that with increasing dilution of plasma biomaterial, the luminescence parameters can change, since many antibodies are characterized by a change in activity at different degrees of concentration.
Reasons for increased ANA
Increased antibodies in systemic scleroderma
A positive test result may indicate the presence of one or more of the following diseases:
- systemic lupus erythematosus,
- drug-induced lupus,
- Sjögren's syndrome or disease,
- systemic scleroderma,
- Sharp's syndrome.
Hepatitis can cause a weakly positive result
A weakly positive result can be caused by both the presence of the above diseases and diseases not related to the immune system. We list the main diseases that can cause it:
- rheumatoid arthritis, including juvenile (children's),
- primary pulmonary hypertension,
- idiopathic pulmonary fibrosis,
- Raynaud's syndrome (digital vasculitis),
- Crohn's disease,
- periarteritis nodosa,
- hepatitis of various natures,
- malignant neoplasms (tumors),
- some infectious diseases (tuberculosis, schistosomiasis, malaria).
A weakly positive test result is sometimes detected in healthy individuals, more often in women over 60 years of age.
Factors that can distort the results
The reliability of the data obtained during the study can be affected by only a few factors that can show both a false positive and a false negative result. Thus, implausible responses with an upward shift are observed in elderly patients over the age of 60 years (according to statistics in 10–37% of cases) and when taking medications that cause drug-induced lupus (some antibiotics, contraceptives, sulfonamides, thiazide diuretics).
It has been noted that 5–55% of females who have breast implants have increased ANA concentrations. The use of glucocorticoid drugs - Prednisolone, Metipred or Dexamethasone - can lead to an erroneous diagnosis with a downward shift.
Indications for the study
Indications for analysis may include joint pain
The study is indicated for symptoms that do not exclude autoimmune connective tissue pathology:
- long-lasting elevated body temperature;
- causeless weight loss;
- reduction of regional lymph nodes;
- pain and stiffness in the joints when no other cause of the pathology has been established;
- muscle pain;
- skin rash, especially on the face in the form of a “red butterfly” (nose and cheeks near the wings of the nose);
- pericarditis and pleurisy of unknown cause;
- changes in general and biochemical blood tests when other types of pathology are excluded.
The test is also prescribed for existing autoimmune diseases to monitor the effectiveness of drug therapy.
Types of research and their description
Currently, it is possible to detect antibodies in biomaterial in several ways:
- Using indirect immunofluorescence microscopy. If specific substances are present in the blood, they will begin to bind to specific nuclear antigens. Laboratories use elements that can glow in a separate spectrum. The biomaterial is then carefully examined under a microscope. The disease can be suspected by the type of glow. This method is recognized as the most informative in determining the value of antinuclear antibodies. One type of technique is research using HEp cells. Analysis of ANF in this case involves taking biomaterial from the larynx. The process is not associated with painful or other uncomfortable sensations. It is important to know that the ANF HEr-2 blood test is currently the most accurate test. Epithelial cells from the larynx are incubated with serum, after which they are also combined with fluorescent substances.
- Using enzyme immunoassay. Its essence lies in the fact that when the interaction of antibodies and antigens occurs, the color of the solution changes. The presence of one shade or another allows one to suspect the presence of a certain pathology.
The ANF analysis should be deciphered by the attending physician. If there are positive test results, additional tests are prescribed. The final diagnosis is not made based on the conclusion of one analysis.
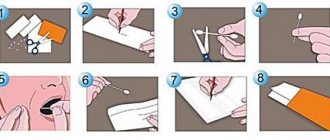
Preparation for analysis and research methodology
Antibody determination can be performed in several ways
The test is taken in the morning on an empty stomach or at another time, but not earlier than 5-6 hours after the last meal. It is also advisable not to take any medications before taking blood for testing.
There are several assay options that differ in their accuracy and ability to quantify antibody concentrations.
A screening ELISA test (enzyme-linked immunosorbent assay) allows you to detect the presence of total antinuclear antibodies and their titer. The advantages of the method include its relative cheapness and the ability to find out whether extensive research is necessary. If the analysis result is negative, further studies are often not indicated.
Indirect fluorescence microscopy is a method based on staining antibodies with special substances that produce a green glow under ultraviolet light. The type and nature of the glow allows the laboratory diagnostics doctor to determine which components of the cell the antibodies have bound to, as well as approximately their quantity.
Immunoblot study allows you to determine the presence of each type of antinuclear antibodies separately. Most often, this test is prescribed after a positive result of another study to clarify the diagnosis.
Antinuclear factor on the HEp-2 cell line (ANF)
Antinuclear factor on the HEp-2 cell line (ANF)
is a test for the detection of antinuclear antibodies using indirect immunofluorescence. In systemic lupus erythematosus (SLE) and other systemic rheumatic diseases, the immune response is directed against nucleoprotein antigens, i.e. complexes of nucleic acids and proteins. These endogenous nucleoprotein complexes are formed during the process of apoptosis of epithelial cells and resemble foreign viral particles. Acceleration of apoptosis processes under the influence of ultraviolet irradiation, viral infections and drugs triggers autoimmune responses in SLE. During apoptosis, major antibody antigens condense into apoptotic bodies, which become targets for autoantibodies. Currently, about 200 types of antibodies to nucleoproteins and ribonucleic acids, which are called antinuclear antibodies, have been described. In autoimmune diseases, autoantibodies to nuclear antigens do not have a direct cytotoxic effect on human cells, however, immune complexes are capable of triggering immunological inflammation, especially in places where the vessels are especially thin, including the kidneys, skin, central nervous system, synovium of joints, and pleura.
Antinuclear factor (ANF) testing is the main method for detecting antinuclear antibodies, allowing the detection of autoantibodies to nucleic acids (dsDNA, ssDNA, RNA), ribonucleoproteins, as well as most conformational and insoluble antigens.
Antinuclear antibodies are detected by their binding to intracellular antigens of a continuous human epithelial cell line (HEp-2). The nucleus and cytoplasm of HEp-2 cells contain all antigens characteristic of the human body, which makes it possible to detect all major antinuclear antibodies in one test. The method of indirect immunofluorescence on the HEp2 cell line is recommended as the gold standard for detecting antinuclear antibodies by leading European (EASIgroup2010) and American experts (ACRANATaskforce2008). Due to the diversity of antinuclear antibody antigens, not all of them can be purified or synthesized for use in enzyme immunoassays for the detection of antinuclear antibodies.
Positivity for ANF on the HEp-2 cell line is observed in systemic lupus erythematosus (SLE), systemic rheumatic diseases and many autoimmune diseases, which makes it a universal test in the examination of patients with autoimmune pathology. A positive result of ANF is observed in more than 90% of patients with diffuse connective tissue diseases, such as systemic lupus erythematosus and cutaneous forms of this disease, scleroderma and its varieties, mixed connective tissue disease, Sjogren's syndrome. Detection of ANF is of great importance in the diagnosis of juvenile rheumatoid arthritis and autoimmune liver diseases. Representatives of this family of autoantibodies can be found in many other autoimmune (thyroiditis, diabetes), infectious (viral hepatitis), inflammatory and oncological diseases. The incidence of ANF reaches 1–3% in clinically healthy people and increases slightly in people over 65 years of age. Individuals with high ANF titers are at increased risk of developing autoimmune diseases.
Indications:
- Systemic lupus erythematosus.
- Subacute cutaneous lupus and other types of cutaneous lupus.
- Mixed connective tissue disease.
- Sjögren's syndrome and associated diseases.
- Diffuse and localized scleroderma, CREST syndrome.
- Inflammatory myopathies (polymyositis and dermatomyositis).
- Juvenile chronic arthritis.
- Autoimmune hepatitis.
- Primary biliary cirrhosis and sclerosing cholangitis.
- Polyneuropathy and myelitis.
Preparation
It is recommended to donate blood in the morning, between 8 am and 12 pm. Blood is taken on an empty stomach or 4–6 hours after the last meal. It is allowed to drink water without gas and sugar. On the eve of the examination, food overload should be avoided.
Interpretation of results
Units of measurement: titer.
Reference values: <1:160 (negative).
The result of determining ANF is the titer, which is the value of the final dilution of the serum at which significant fluorescence of the nucleus remains. The higher the denominator of the fraction, the greater the dilution of the serum, the more antibodies in the patient’s serum. High serum dilution titers reflect high affinity and concentration of autoantibodies.
Detection of high levels (1/640 and above) indicates a high probability of systemic rheumatic disease or autoimmune liver disease and requires careful clinical, laboratory and instrumental examination. The absence of elevated antinuclear factor titers significantly reduces the likelihood of systemic autoimmune diseases.
In low titers (up to 1/160), antinuclear factor can be observed in 1–2% of healthy individuals and relatives of patients with systemic diseases. The frequency of positive titers in the population increases slightly with age. Low titers of antinuclear antibodies can occur in many autoimmune, infectious and oncological diseases. The absence of high titers of antinuclear antibodies significantly reduces the likelihood of a systemic rheumatic process and can be used to exclude rather than confirm the diagnosis.
Factors influencing the result
Medicines can distort the results
A false positive test result can be caused by taking certain groups of medications:
- antidepressants;
- antiarrhythmics (bisoprolol, biosotal);
- anticonvulsants (carbamazepine, phenytoin);
- drugs for the treatment of atherosclerosis (lovastatin, atorvastatin);
- drugs to lower blood pressure.
It is advisable to limit the intake of medications 1-2 days before the test in strict accordance with the recommendations of the attending physician.
Preparation
The collection of biomaterial is carried out in the morning. It is necessary to donate blood on an empty stomach. The last meal should be taken at least 4 hours before. At the same time, drinking water is acceptable at any time and in any quantity. Alcohol consumption is prohibited.
Rest is indicated 1 day before the study. Physical and psycho-emotional stress often lead to false results. Smoking is prohibited half an hour before donating blood.
It is necessary to inform the doctor about the medications you are taking when prescribing an ANF test. This is due to the fact that the active components of some drugs provoke the production of antibodies and can also cause drug-induced lupus. False-negative results are often a consequence of taking glucocorticosteroids.
If the patient has been prescribed physical procedures or instrumental examinations, they should be carried out only after blood donation.