Von Willebrand disease (VWD) is a congenital disease of hemostasis, which is manifested by a quantitative as well as a qualitative deficiency of plasma von Willebrand factor (VWF) and this provokes increased bleeding.
Von Willebrand disease is associated with sudden formation of:
- Petechiae under the skin
- Nosebleeds that tend to recur
- Gastrointestinal bleeding,
- Uterine bleeding,
- Hemarthrosis,
- Large blood loss due to injuries, as well as during surgery.
What is von Willebrand disease?
Von Willebrand disease is a hematological disorder that is inherited and manifests itself with sudden bleeding wounds.
Hemostasis in the body is ensured by adequate functionality of the blood plasma coagulation system, and hemostasis is a protective function of the body. If a blood artery is damaged, then bleeding occurs and hemostasis is activated.
By activating the plasma blood factor, the entire blood coagulation system operates; platelet aggregation forms a clot from the blood plasma, which seals the defect in the vessel and the bleeding stops.
If at least one link of this chain of the hemostatic system is damaged, then deviations in its correct operation occur.
Willebrand's disease
What is von Willebrand factor?
This is a protein that has its own specificity in the hemostasis system. A deficiency of this protein, or its complete absence, leads to deviations in the functioning of coagulation processes. This protein is a multimeric type glycoprotein, a carrier of factor VIII.
The job of FB is to provide adhesion for platelets and attach the platelets to the arterial wall at the site of injury. Von Willebrand disease is transmitted genetically and most often occurs through the female line.
The name of this disease is angiohemophilia.
This name contains the essence of the processes occurring during an attack of this pathology . This name is very rarely used in modern medicine.
Diagnostics: necessary tests
Von Willebrand disease is diagnosed using laboratory tests including the following:
- von Willebrand factor antigen test. Necessary to determine the amount of factor in the blood;
- platelet aggregation with ristocetin in plasma. This study evaluates the effectiveness of the factor, namely, it determines the indicators of platelet adhesion, which will be reduced in the presence of pathology;
- activated partial thromboplastin time (aPTT). A technique that allows you to estimate the required amount of time for the formation of a blood clot. If pathology is present, this time will be increased;
- determination of coagulant (clotting) activity of factor VIII. In case of illness, it is normal or slightly reduced;
- artificial induction of bleeding to determine the time of its duration. In pathology - enlarged;
- coagulogram No. 3. A comprehensive analysis of the hematopoietic system, identifying any pathological changes in this area;
A coagulogram is a set of blood parameters indicating the coagulation process - general blood test - to assess your overall health.
A more extensive diagnosis is carried out in the presence of symptoms characteristic of type III disease, since in this case there is a high probability of an incorrect diagnosis due to the difficulties of differentiation with hemophilia.
Differential diagnosis with hemophilia: characteristic differences
Difficulties in diagnosing the disease lie in the sometimes arising problems of differentiation with hemophilia. The reasons for this are the following:
- the pathology does not manifest itself as clearly as hemophilia;
- the symptoms of both pathologies differ significantly, although at first glance they may seem similar;
- the disease is poorly understood compared to hemophilia.
The pathology differs clinically from hemophilia in that women can also get sick, and the hemorrhagic syndrome is not hematoma, but petechial-spotted or mixed. In addition, mild forms of the disease are diagnosed only in adolescence or during invasive surgery, unlike hemophilia, which is detected immediately after birth. Another difference is that bleeding occurs immediately after injury and does not recur after stopping.
Classification of BV
Von Willebrand disease is divided into types. There are 3 of them:
Type No. 1 lack of von Willebrand factor in the blood plasma. This deficiency leads to decreased activity of factor VIII, and a disruption in the aggregation of platelet molecules occurs.
This form of pathology is classic and most common.
Pathology blocks the synthesis of this factor in arterial endothelial cells. Coagulability does not change, patients do not feel painful symptoms.
The manifestation of the disease occurs in the form of bruises on the body from minor blows, and bleeding also occurs after dental surgical procedures and surgical intervention in the body.
Type No. 2 von Willebrand factor in blood plasma within the normal volume, only its structure is modified. The manifestations of the disease are influenced by various provoking factors.
The pathology manifests itself in the form of sudden bleeding in varying degrees of intensity and with different localization.
Type 3 is a severe stage of the disease, which is characterized by the complete absence of VWF in the blood plasma.
This is a rather rare manifestation of the disease, in which blood accumulates in the cavities of the joints.
A separate type of disease is a platelet type of pathology. This comes from matting the gene that is responsible for the functioning of the platelet receptor for VWF. Platelet VWF is released from active platelet molecules and ensures the aggregation of these platelets.
The division of the second type of pathology according to the characteristics of impairments in functionality made it possible to identify subtypes of the disease:
- Subspecies type No. 2 2A,
- Subspecies of the second type 2B,
- Subtype 2M,
- Also 2
Scientists have proven that these subspecies of the second type depend on:
- A type of von Willebrand disease that has a hereditary genetic lineage,
- Index of reduction in the composition of blood plasma von Willebrand factor,
- Stage of mutation of hereditary genes,
- The degree of expression of the hemorrhagic syndrome.
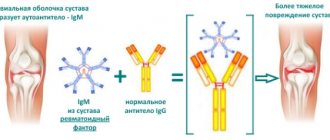
There is also a fairly uncommon form of the disease, which is an acquired pathology. It appears in the body with the appearance of autoantibodies in the blood plasma.
The consequences of an antibody invasion are that the body perceives its cells as foreign and produces antibodies (antigen) against them.
This pathology can be provoked by infectious diseases, invasion of the body by viruses, as well as traumatic situations and stress.
This pathology is found in the following diseases:
- Autoimmune diseases,
- Malignant neoplasms:
- Reduced functionality of the thyroid gland,
- Disorders in the endocrine system,
- Pathology in the functioning of the adrenal glands,
- Mesenchymal dysplasia.
Causes and development factors
The factors that cause von Willebrand disease are divided into 2 groups - internal and external.
What kind of disease is whooping cough: symptoms of the disease, treatment and prevention are described in the article https://krasnayakrov.ru/organizm-cheloveka/rebenok/lechenie-koklyusha.html
The pathology can be either congenital or acquired. The first form of the disease is caused by a mutation in the von Willebrand factor gene (the child is born with this disorder). Acquired - for the same reason, but it develops under external influence.
Under the influence of these reasons, the level of von Willebrand factor in the blood plasma drops below normal, after which, depending on the degree of deviation from the ideal indicator, certain symptoms appear.
The normal level of von Willebrand factor in the blood of a healthy person is 10 mg/l. Exceeding this value can be diagnosed after physical activity, stress, or previous infections.
Factors for the occurrence of von Willebrand disease - table
| Group of factors | Name |
| Domestic | Mutations in the von Willebrand factor gene |
| External (environmental factors) |
|
Etiology of von Willebrand disease
The main reason for the development of this pathology is a deficiency in the quantitative volume and quality of von Willebrand factor VIII.
The disease differs from hemophilia in that in hemophilia, where genetic transmission is only through the female line within one family branch, von Willebrand disease can be genetically transmitted by both the father and the mother according to the dominant type of genes.
This is a different stage and degree of manifestation of hemorrhagic syndrome in family members.
The membranes of the arteries are involved in the disruption of the synthesis of von Willebrand factor components. They contain the only place in the body where this protein is formed.
The causes of the disease may be:
- Factors associated with blood plasma, fluctuations in the quantitative ratio of the constituent elements of a given type of protein in the blood,
- Vascular factor of deviation in the functioning of the endothelial membrane, and a violation in its synthesis of this protein.
The main task of von Willebrand factor is the ability to attach platelets to fibrogen, and together they attach to the vessel wall.
von Willebrand disease
Von Willebrand disease is a congenital pathology manifested by a deficiency of von Willebrand factor and characterized by increased bleeding. The interaction of platelets with the walls of blood vessels is disrupted, which increases capillary fragility. The incidence is similar to that for hemophilia and is 10 cases per 100 thousand people.
Reference. Von Willebrand factor is a blood plasma glycoprotein that plays an important role in hemostasis (maintaining the fluid state of the blood).
The disease is named after its discoverer, Erik Adolf von Willebrand (1870–1949), a Finnish doctor with Russian noble roots. The first names of the considered pathology of the hematopoietic system were given by Willebrand himself - “pseudogemophilia”, “constitutional thrombopathy”. Later, American doctors discovered that the disease was based on protein, not platelets.
Eric von Willebrand - discoverer of the disease of the same name
The essence of von Willebrand disease is a blood clotting disorder. It is more common in women and is transmitted from mother to child. And it manifests itself in every generation. Those at risk are those whose blood relatives have this pathology. If at least one of the parents is a carrier of the defective gene, the probability of the disease developing in the child is 50% or higher.
The essence of von Willebrand disease is a blood clotting disorder.
According to medical statistics, in the majority of patients with von Willebrand disease the pathology occurs in a mild form (about 70%), while in the remaining patients it occurs in a moderate and severe form (30%). Of these, no more than 7% of patients experience an extremely severe stage of the disease.
Von Willebrand's disease - video
Manifestations of BV
The signs of von Willebrand disease differ from other pathologies; they occur unexpectedly, are not constant, and their manifestations are not uniform. This disease is commonly called chameleon.
Von Willebrand disease can manifest itself:
- In a newborn child after birth,
- Do not appear for quite a long time,
- Manifest itself suddenly with copious bleeding after a minor injury,
- Manifest after an infectious or viral disease.
In some relatives of the family line who are genetic carriers of von Willebrand disease, this pathology may not manifest itself during their entire life.
And for some, the first heavy bleeding can cost their lives.
Symptoms of a mild stage of the disease
This pathology can occur in a mild course, which does not pose a mortal danger, as well as in a severe (life-threatening) degree of the disease.
Symptoms of mild von Willebrand disease:
- Nosebleeds that occur systematically over a short period of time,
- Heavy bleeding during menstruation in women,
- Prolonged bleeding from a minor cut or minor injury,
- Petechiae on the skin,
- Post-traumatic hemorrhages.
Clinical manifestations of severe BV
The severe stage of von Willebrand disease manifests itself in life-threatening symptoms:
- Dysuria appears as pain in the lumbar spine and blood in the urine,
- Large localized hematoma after a minor bruise compresses large-diameter arteries, which causes pain,
- Excessive bleeding after injury, as well as internal post-traumatic leakage of blood,
- Severe bleeding during surgical intervention in the body,
- Bleeding after tooth extraction surgery,
- Recurrent bleeding from the sinuses and bleeding from the gums,
- Prolonged bleeding after cuts to the skin, which can cause fainting, dizziness,
- Uterine heavy bleeding monthly provokes a deficiency of iron in the blood, which manifests itself in anemia,
- Hemarthrosis disease is swelling of the affected joint, painful conditions in the joints, as well as extensive subcutaneous hematoma,
- Abundant leakage of blood from the nasopharynx, as well as the pharynx, leads to the pathology of bronchial obstruction,
- Cerebral hemorrhage affects the centers of the entire nervous system and is fatal.
In the severe stage of von Willebrand disease, the symptoms of hemophilia pathology are very similar.
Hemorrhages in the brain, as well as in internal organs, are characteristic only of type No. 3 of this pathology.
In the second type, it can occur only in the case of an anomaly in the structure of platelets, as well as in the formation of hemarthrosis.
If von Willebrand factor is lower (its deficiency), then an anomaly in the structure of the platelet molecule occurs, then the pathology has the following characteristic signs:
- Severe nasopharyngeal bleeding
- Bleeding inside muscle tissue and its manifestation in the form of a hematoma,
- Bleeding of internal organs: stomach, intestines (in case of injury),
- Damage to joint pathology.
The most dangerous to human life are gastric bleeding and intestinal bleeding inside the abdominal cavity. Arteriovenous anastomosis prevents stopping internal bleeding.
Clinical manifestations in children with BV
Von Willebrand disease in childhood is diagnosed and manifests itself before 12 months.
Vivid symptoms in infancy are:
- Blood leaking from the nose,
- Bleeding from gums during teething
- Bleeding inside the stomach, as well as blood in the intestines appears in the feces,
- Blood in urine.
As a girl gets older, she may experience increased uterine bleeding (menorrhagia).
Vivid symptoms and signs of iron deficiency anemia are expressed: pale skin, dizziness, fainting, signs of nausea.
Von Willebrand disease manifests itself as the child grows up through loss of blood through the socket of an extracted tooth, through a wound due to a cut or abrasion.
This pathology is also expressed in rashes on the skin in the form of ecchymosis, which are filled with blood, bruises on the skin and hematomas of intra-articular hemorrhage.
Bleeding begins immediately after the injury, and after it has been stopped, relapses do not recur; this is the main difference between von Willebrand disease and hemophilia.
Symptoms
A sure sign of von Willebrand disease is prolonged bleeding. Their intensity and extent largely determine the clinical picture of the pathology. Bleeding in patients with the disease occurs due to injuries, surgery, and dental operations. In addition, the main symptom is accompanied by weakness of the body, dizziness, pale skin, low blood pressure and often even fainting.
Von Willebrand syndrome is not constant, which means that the symptoms of the disease vary in a sick patient. They can either disappear for a long period of time or appear again for no apparent reason. Taking into account the types of pathology, each carrier of this disease feels differently. Some quietly enjoy a satisfying life. Other patients experience daily fear of deadly bleeding. The latter can be eliminated only in stationary conditions.
A mild form of von Willebrand pathology manifests itself individually in each patient. It is characterized by several symptoms:
- bleeding in patients with the disease occurs even with minor damage to the skin;
- often bleeding gums, nose;
- heavy menstrual bleeding in sick women;
- petechiae;
- hemorrhages after injuries.
A severe form of pathology is expressed in more dangerous symptoms. They are almost identical to hemophilia:
- Extensive hematomas that occur even after a slight bruise.
- Prolonged bleeding from the gums after routine teeth brushing.
- Blood in urine.
- Malaise in the lower back when a patient with an illness goes to the toilet.
- Bleeding in the area of the pharynx and nasopharynx. Can lead to bronchial obstruction.
- Hemorrhage into the lining of the brain. Involves damage to the central nervous system or even death.
Von Willebrand pathology has certain similarities with another disease. Doctors note a number of signs of BV, which are also inherent in hemorrhagic syndrome:
- Bleeding in the patient's digestive tract. They are provoked by drugs from the NSAID group and antiplatelet agents. Patients experience melena (black, tarry, loose stools, vomiting dark blood).
- Hemarthrosis. Painful bleeding into the joint cavity, accompanied by swelling, increased sensitivity to palpation and redness of the skin. At the same time, a patient with pathology has limited joint functions. The volume of the latter is increased, its shape takes on a smoothed spherical appearance.
- Signs of mesenchymal dysplasia. They appear in particularly severe cases of the disease. Local vascular and stromal dysplasias provoke systematic bleeding (mainly of a certain localization).
Von Willebrand factor in children
Hemorrhagic diathesis in young patients is sharply complicated after acute respiratory infections and other acute infections. During the period of intoxication, vascular permeability increases, which leads to spontaneous bleeding in von Willebrand disease. In other cases, this pathology manifests itself in children and adolescents in the same wave-like manner: periods of exacerbation of the disease are replaced by a complete absence of hemorrhages, and vice versa.
The mild form of the disease manifests itself in the same way as in adults. It is characterized by several signs:
- heavy bleeding after injury or local surgery;
- periodic nosebleeds;
- bleeding gums (in children with pathology this occurs without any damage).
Complications of the pathology give rise to a number of new symptoms. The more severe the form of the disease, the more intensely they manifest themselves in patients:
- presence of blood in the child/teenager’s urine and stool;
- formation of subcutaneous hematomas with mild bruises;
- internal damage to the joints with accompanying bleeding in their cavity.
Relationship between BV and pathologies in connective tissue
Research conducted by modern scientists has established the relationship between von Willebrand disease, as well as defects and anomalies in the development of connective tissue cells.
This relationship is manifested in the following violations:
- Mitral valve prolapse and pathologies of other heart valves,
- Dislocations in the joints due to disturbances in the ligaments of the muscular organs,
- Hyperelastosis of the skin,
- Degenerative myelopathy,
- Marfan syndrome manifests itself in cardiac pathologies, disorders of the eye organ, as well as elongation of skeletal bones in the body.
How close this relationship is between these two pathologies and its etiology needs to be clarified through research by scientists.
Dependence of the development of the disease on the type of genetic inheritance
Using research, geneticists concluded that the pathogenesis of von Willebrand disease depends on the nature of genetic inheritance.
If the patient received deformed genes from one of his biological parents (intrauterine formation of a heterozygous fetus), then mild symptoms appear, or they are completely absent.
With homozygous genetic inheritance (from two biological parents), then von Willebrand disease occurs in a severe clinical form, with all types and characteristics of bleeding, and quite often with the complete absence of the f VIII antigen in the blood plasma.
Less severe symptoms also appear than in the pathology of hemophilia, in lesions of the articular part of the body and in the muscular organs.
Classification
The advantages of testing include its high specificity, while the disadvantages include the difficulty of deciphering the results. Since many factors influence the final result of the examination, blood should be donated again after 1-3 months.
There are 3 types of BV. The classification is as follows:
- Type I - there is not enough vWF in the body, which leads to a reduction in the activity of factor 8 and abnormalities in platelet aggregation. This “classic” is diagnosed more often than others. The synthesis of vWF in the endothelium is partially or completely blocked. In this case, the functioning of the thrombosis system does not change significantly. The patient's condition is close to normal. Hemorrhaging manifestations form after surgery and a visit to the dentist. In such people, hematomas quickly form even from a slight touch.
- Type II - vWF is found in the blood in adequate quantities, its structure changes. Under the influence of a provoking factor, sudden bleeding develops.
- Type III - provides for the absolute absence of vWF in the bloodstream. This is the rarest form of BV, which is manifested by microcirculatory hemorrhages and accumulation of blood in the joint area.
In medicine, a thrombotype is isolated that carries a genetic mutation responsible for the vWF gene receptor. Platelet vWF exits the forward platelet-producing substances and creates their adhesion and aggregation. A non-congenital form of BV, it is rarely diagnosed.
The mechanism of its development is explained by the formation of autoantibodies in the body. Your own cells are now perceived by the body as foreign, and antibodies are formed to them. Acute infections, trauma, and stressful situations can trigger the development of the disease in people at risk. This type of disease is detected in people with autoimmune pathologies, oncology, and decreased thyroid function.
Von Willebrand disease and pregnancy
The course of pregnancy in von Willebrand disease types No. 1 and No. 2 partially compensates for the von Willebrand factor at the time of the birth process. Although its volume is higher than normal, it is still not enough for blood clotting at the time of childbirth and in the postpartum period. Gynecologists are always wary of sudden and heavy labor bleeding.
With von Willebrand disease, a third of pregnant women are at risk of artificial termination of pregnancy by the body due to severe toxicosis. Toxicosis also appears in the third trimester.
The most severe complication of von Willebrand disease during the period of intrauterine formation of a child is premature detachment of the placenta when it is correctly positioned intrauterinely. With normal therapy and monitoring of this pregnant woman within the walls of the hospital, the birth process takes place in a timely manner.
Von Willebrand factor is increased during pregnancy; it increases until the beginning of the 3rd trimester (this factor is compensated by the developing body of the child).
Sometimes pregnancy improves the course of this pathology. And quite often, after the birth of a child, remission of von Willebrand disease does not occur for a very long time.
Dangers during pregnancy, at the time of childbirth and the postpartum period:
- Miscarriage in the early stages of pregnancy (1st trimester),
- Placental abruption (3rd trimester),
- At the time of birth, heavy bleeding that is very difficult to stop,
- 6 calendar day and up to 10 days after the hearth process there is a danger of bleeding,
- Up to 13 calendar days, the danger after a cesarean section is an increased amount of bleeding.
During the postpartum period, the woman in labor remains in the hospital until the danger of von Willebrand disease has passed.
Reduced level
Venous blood is required for the study.
Reduced values are observed in different types of autoimmune diseases:
- Systemic lupus erythematosus;
- Hashimoto's disease (autoimmune thyroiditis with hypothyroidism);
- Systemic connective tissue diseases.
The lowest values are typical for von Willebrand disease, a hereditary deficiency of the blood coagulation system. There are several types of this disease, each of which has its own levels of deficiency:
- Type 1 is the most common type of pathology. Von Willebrand factor is produced, but in insufficient quantities for normal blood clotting.
- Type 2 - a defective factor is produced that is unable to fully perform its functions. The values determined in the blood may be normal.
- Type 3 - von Willebrand factor is not synthesized by the body at all. This is the most severe and least common variant of the disease; the prognosis for the course of the disease is often unfavorable; the disease begins to manifest itself in early childhood.
Diagnostics
Von Willebrand disease is quite difficult to diagnose. It is often diagnosed in children only in their teens. Diagnosis begins with a family history.
The hereditary genetic factor is always considered first and quite often it is the main factor in von Willebrand disease.
Hemorrhagic syndrome is the main symptom of this pathology. It establishes a preliminary stage of diagnosis.
For a more accurate diagnosis, it is necessary to undergo a number of diagnostic measures:
- Genetic intervention to install a modified gene. This event is performed for both biological parents before conceiving a child,
- Determination by biochemical analysis of the activity and ability of the von Willebrand factor, its quantitative concentration in the blood plasma, as well as the performance of the factor’s functional duties,
- Biochemical analysis - coagulogram for von Willebrand disease,
- A general analysis of blood plasma reveals the presence of post-hemorrhagic anemia in the body,
- X-ray of joints,
- MRI (magnetic resonance imaging) joint arthroscopy,
- Ultrasound of the peritoneum to detect bleeding of internal organs,
- Laparoscopy for intestinal diagnostics,
- Endoscopy for intestinal diagnostics,
- Analysis of urine for the presence of blood in it,
- Laboratory testing of stool,
- Pinch test.
You can get a number of tests done in the Invitro laboratory at reasonable prices.
Causes
The main source of the disease is polymorphism of the gene responsible for the synthesis of von Willebrand factor . The latter is either insufficient in the blood of sick patients or completely absent. This pathology occurs regardless of gender. True, it manifests itself more often in the fair sex. This is due to the physiology of the female body, and specifically the structural features of their reproductive system.
The acquired form of von Willebrand disease, associated with the formation of autoantibodies, develops only as a complication in the patient's body. It is preceded by numerous blood transfunctions or certain types of diseases:
- systemic (SLE, rheumatoid arthritis);
- cardiac (aortic valve stenosis);
- oncological (nephroblastoma, Wilms tumor, macrobulemia).
Article on the topic: Ointment for fungus on the skin of the body
Standard indicators for von Willebrand factor
Standard indicators for patients with blood group I will differ from those of people with the second, third, and fourth blood groups.
To make a diagnosis, it is recommended to undergo three types of tests:
- VWF: antigen level (VWF:Ag test),
- VWF: for factor activity in blood plasma (VWF:Act test),
- VWF VIII in the ratio: FVIII to VWF:Ag.
| VWA Ag - standard VWF Act - standard FV III - standard | von Willebrand disease and hemophilia pathology - not present |
| EF is very reduced | disease type No. 3 |
| VWF Act - 1 VWF Ag - 1 FV III -1 | disease type No. 1 |
| VWF Act, VWF Ag less than 0.70 | pathology type No. 2 - 2A, 2B, 2M |
| FV III, VWF Ag, less than 0.70 | disease type No. 2 - 2 N, as well as the pathology hemophilia |
| (FVIII:C), (VWF:Ag) and (VWF:AC) increases. | during pregnancy with type No. 1 |
| VWF Act, VWF Ag, FV III = 0 | for type number 2 - 2A, 2B, 2M |
Treatment of abnormalities
A blood test to determine the amount and activity of von Willebrand factor is a highly specific test that assesses the ability of platelets to aggregate and adhesive during clot formation. The results are used in hematology for diagnosis, including differential diagnosis, of von Willebrand disease. For proper interpretation of the results and prescription of treatment, you should contact a hematologist. Physiological deviations from the norm do not require special correction, but to obtain informative data, it is necessary to follow the recommendations for preparing for the analysis: exclude physical activity and stress, smoking, taking medications, donate blood from the 5th to the 7th day of the menstrual cycle.
Treatment
Therapy for Von Willebrand disease is prescribed by hematologists. This pathology cannot be completely cured because it is hereditary and genetic in nature. Treatment consists only of relieving symptoms in order to alleviate the patient’s condition.
The basis of therapeutic treatment is a transfusion drug course.
This course of medications is aimed at correcting all components of hemostasis and bringing them to standard values:
- Administration of hemotherapy,
- Antihemophilic blood plasma is administered by injection,
- Introduction of the drug cryoprecipitate into the body.
Therapy helps to increase the biosynthesis of the deficient factor in the body:
- Hemostatic wipe with thrombin,
- The drug Desmopressin,
- Antifibrinolytic drugs,
- Hormonal contraceptives for bleeding from the uterus,
- Wound gel with fibrin component,
- Hemarthrosis is treated with a plaster cast followed by heating with a UHF method,
- The drug Tranexam therapy for mild forms of pathology,
- Dicinon is used for severe cases,
- Medicine Etamzilat.
Cost of treatment
| 1896.00 rub. | consultation with a gynecologist |
| RUB 2016.00 | Abdominal ultrasound |
| RUB 933.00 | dentist consultation |
| 1859.00 rub. | consultation with an otolaryngologist |
| 1976.00 rub. | consultation with a gastroenterologist |
| RUB 391.00 | analysis of stool for hidden blood |
| 1164.00 rub. | coagulogram |
| RUB 569.00 | general blood analysis |
| RUB 552.00 | blood group test |
Causes
Von Willebrand disease is a hemorrhagic diathesis in which the blood clotting process is completely or partially disrupted. Hemostasis is a rather complex process and consists of several stages that successively replace each other. Under the influence of certain coagulation factors, the process of thrombus formation begins, as a result of which a blood clot is formed, clogging the site of damage to the vessel. With BV, the content of a special protein in the blood, von Willebrand factor, decreases, which ensures platelet aggregation and their adhesion to the damaged endothelium.
The main cause of the disease is polymorphism of the gene encoding the synthesis of von Willebrand factor . As a result, it is synthesized in insufficient quantities or is completely absent in the blood. BV occurs in both men and women. Due to the physiological characteristics of the structure of the female body, due to reproductive function, hemorrhagic syndrome occurs most often in women.
BV is often mild and may not be diagnosed at all. VWF deficiency usually results in bleeding from organs with a developed capillary network - the skin, gastrointestinal tract and uterus. A severe form of the disease, manifested clinically, occurs in people with blood group I (O). Banal bleeding from the nose or from a hole after tooth extraction can result in the death of the patient.
Prevention
This pathology is hereditary and there is no way to prevent it.
Preventive measures can only prevent severe and frequent bleeding:
- Before conceiving a child, consultation of biological parents with a hematologist,
- Observation of children (dispensary),
- Visit your doctor regularly,
- It is forbidden to take aspirin,
- Avoid traumatic situations
- Healthy lifestyle,
- Food culture.
Completing these measures will help avoid bleeding inside the joints and inside the muscle tissue. Will not allow von Willebrand disease to develop into a complicated form.
When to get tested
A doctor prescribes a test to detect vWF BV if a person has frequent and prolonged nosebleeds, especially if they occur in a child. A prerequisite for testing may be deviations from normal values in the results of a standard coagulogram:
- APTT.
- INR.
- Thrombosis indicator.
- Thrombin period.
The basis is also a decrease in the amount of factor 8. During screening, the disease is detected if the disease was diagnosed in a blood relative. BV can be congenital. In such a situation, the manifestations are usually mild; approximately 10% of cases need to be treated. The non-congenital form of BV is formed in the following pathologies:
- Heide.
- Vasculitis.
- Sclerotic lesions.
- Pulmonary necrosis.
- Heart diseases.
- Hypothyroidism.
- Acute leukemia.
- Lymphoma.
- Multiple myeloma.
- Autoimmune pathologies.
- Wilms tumor.
The disease can develop due to the consumption of medications. Because the factor is a protein of the acute phase of the inflammatory process, analysis to detect its level in the blood is not carried out during exacerbation of inflammation or oncology. In such situations, the analysis will not be reliable; the factor will be greater than normal.
Increased vWF is formed with extensive vascular damage, for example, with diabetic disease. If a person has obvious problems with blood clotting, the need for a blood test is discussed with the doctor personally.
Attention! If psychomotor agitation is observed, blood is not drawn.