Formed elements of blood
The formed elements of blood provide its versatility
Formed elements provide the versatility of blood functions. They create the body’s defense against pathogenic microbes, transport oxygen and nutrients, cleanse the circulatory system and remove waste products, restore damaged tissues and prevent blood loss, stopping bleeding.
All elements originate in the bone marrow from a single stem cell. As cells develop, they differentiate and transform into one of the types of formed elements: red blood cells, platelets and leukocytes. In total, they make up 40 - 48% of blood volume, the remaining 52 - 60% are plasma. The ratio of the total number of formed elements is called hematocrit. Sometimes hematocrit is calculated based on the number of red blood cells only, since they are the main cellular elements of blood.
Where are leukocytes formed in humans?
Human blood consists of formed elements and plasma. Leukocytes are one of these formed elements along with red blood cells and platelets. They are colorless, have a nucleus and can move independently. They can be seen under a microscope only after preliminary staining. From the organs included in the human immune system, where leukocytes are formed, they enter the bloodstream and body tissues. They can also freely pass from vessels to adjacent tissues.
Leukocytes move in the following way. Having secured itself on the wall of the vessel, the leukocyte forms a pseudopodia (pseudopod), which it pushes through this wall and clings to the tissue from the outside. Then it squeezes through the resulting gap and actively moves among other cells of the body that lead a “sedentary” lifestyle. Their movement resembles the movement of an amoeba (a microscopic single-celled organism from the category of protozoa).
Red blood cells: structure and functions
Red blood cells - erythrocytes
Red blood cells (RBCs) are anucleate, biconcave, round cells. The diameter of a developed cell is about 7 - 8 µm, thickness - 2.2 µm at the edges and 1 µm in the central part. The shape and structure of the cell determine the optimal performance of its functions by red blood cells. The concave shape increases the surface of the red blood cell by 1.7 times compared to a spherical cell, and also allows it to move through the thinnest capillaries - penetrating into narrow vessels, red blood cells are able to stretch and twist. The nucleus is lost as the cell matures, making room for hemoglobin molecules.
Red blood cells move smoothly along the bloodstream, lining up in the form of columns, the ends of which are connected to each other, forming rings, which facilitates the movement of blood. Each cell contains about 300 million hemoglobin molecules, which reversibly bind to oxygen and then distribute it to the tissues of various organs. Hemoglobin is a complex protein containing 574 amino acids and consisting of 4 subunits. Each of them includes heme, an iron complex that provides the red color of the cell, and the collection of red blood cells gives the red color to the blood.
The main function of red blood cells is to transport oxygen and remove carbon dioxide from tissues. A decrease in the number of blood cells, changes in their shape and flexibility due to various diseases lead to a lack of hemoglobin and oxygen starvation of all organs. Red blood cells take part in immune reactions and maintaining acid-base balance, and transport nutrients. Also, these cells carry about 400 antigens on their surface; antigens of blood group systems are of primary importance, that is, antigens of blood groups II, III, IX and the Rh factor.
Destruction of the red blood cell.
Blood cells are constantly being destroyed in the body. Red blood cells undergo especially rapid turnover. It is calculated that about 200 billion red blood cells are destroyed per day. Their destruction occurs in many organs, but in especially large quantities - in the liver and spleen. Red blood cells are destroyed by dividing into smaller and smaller sections - fragmentation, hemolysis and by erythrophagocytosis, the essence of which is the capture and digestion of red blood cells by special cells - erythrophagocytes. When red blood cells are destroyed, the bile pigment bilirubin is formed, which, after some transformations, is removed from the body in urine and feces. Iron, released during the breakdown of red blood cells (about 22 mg per day), is used to build new hemoglobin molecules.
Leukocytes: structure and functions
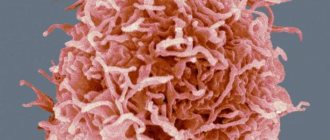
White blood cells - leukocytes
White blood cells (WBC) are a group of cells, each of which has a specialized protective function. Leukocytes contain nuclei; the cells contain hydrolytic enzymes, a protein synthesis system, biologically active compounds and other organelles. Leukocytes have the ability to migrate through the vascular wall, rushing towards foreign particles to capture and destroy them. The destruction of harmful cells is carried out by leukocytes using the process of phagocytosis - absorption and digestion. Leukocytes include 5 groups of protective cells.
1. Basophils (BAS). They make up only 1% of all leukocytes. These cells are round in shape, their diameter is approximately 12 - 15 microns. Basophils contain irregularly shaped granules that contain histamine, heparin, serotonin, prostaglandin and other substances. If necessary, basophilic leukocytes release the contents of their granules, participating in allergic reactions, blocking poisons, protecting blood vessels from the formation of blood clots, and attracting other helper cells to the site of inflammation.
2. Eosinophils (EOS). Their number in leukocytes is also small - from 1 to 4%. The cells have a round shape, the nucleus forms 2 segments connected by a bridge. The diameter is about 12 - 17 microns. Eosinophil granules contain collagenase, elastase, peroxidase, acid phosphatase, prostaglandins, alkaline protein, etc. Eosinophils are able to attach to parasites and introduce enzymes from their granules into the cytoplasm of harmful organisms, dissolving their membrane.
Agranulocytic leukocytes - lymphocytes
3. Lymphocytes (LYM). They make up about 30% of leukocytes and are the main immune cells. Lymphocytes are spherical formed elements, most of them are small cells with a dark nucleus, 5 - 7 microns in diameter. Large lymphocytes have a bean-shaped nucleus, their diameter exceeds 10 microns. These cells are functionally divided into types:
- B lymphocytes. They form antibodies against harmful agents.
- Killer T cells destroy pathogenic cells (parasitic, viral, tumor).
- T-helpers help in the processes of proliferation and differentiation of lymphocytes and promote the production of antibodies.
- Suppressor T cells stop helper T cells from working when needed.
- T-memories “record” information about microbes that have entered the body, so that when a new attack by harmful microorganisms occurs, the appropriate antibodies are directed against them.
- NK lymphocytes destroy abnormal cells.
Band neutrophil
4. Neutrophils (NEU). The most numerous group of leukocytes, makes up up to 75% of the number of protective cells. The diameter is approximately 12 - 15 microns; they circulate in the blood in the form of two subtypes:
- Rods. They are immature elements, their nuclei are similar to rods, which will then divide into segments, forming the next subspecies.
- Segmented. Their nuclei are segmented and usually contain 3 lobes connected by chromatin threads.
Neutrophils actively absorb bacteria, fungi and some viruses. They are the first to rush to the source of infection, capture pathogenic particles with their pseudopods and place them inside the cytoplasm, releasing the contents of their granules. Their granules contain collagenase, aminopeptidase, cationic proteins, acid hydrolases, and lactoferrin. Having digested harmful microorganisms, neutrophils usually die, at this moment releasing a number of substances that help suppress the remaining bacteria and fungi, and also enhance the process of inflammation, which becomes a signal for other immune cells. The mass of dead neutrophils, mixed with cellular detritus, represents pus.
5. Monocytes (MON). These leukocytes do not have granules; their nuclei can be presented in the form of an oval, horseshoe, bean, and the diameter is 12 - 20 microns. They make up about 4 - 10% of the number of immune cells. They are active phagocytes, capable of absorbing large microorganisms, and usually do not die after the digestion process. They remain at the site of inflammation and clean it, separating healthy tissue from damaged tissue. Monocytes destroy both pathogenic microbes and dead leukocytes, promoting the subsequent regeneration of damaged tissues.
Why does the content of red blood cells in urine increase?
An increase in the concentration of red blood components in the secretions is called a special term - hematuria. If during the examination a small amount of red blood cells is detected in the urine, this condition indicates microhematuria. In this situation, there are no visible changes in the secreted liquid - it remains straw-yellow, as it should be.
But if the urine acquires a burgundy or reddish tint, then this phenomenon is called gross hematuria (indicates serious kidney damage). When studying such biomaterial under a microscope, red blood cells are found in the urine, which completely cover the entire field of view of the magnifying device. Their shape often changes under the influence of various substances present in the discharge - which is also a sign of pathology.
What causes increased red blood cells in urine? The cause of this condition is often the following violations:
- Cystitis - with this disease, the presence of red blood components in urine is sometimes noted. If the bladder lesion has an infectious etiology, then during the examination proteins and bacteria in the urine are determined. The disease is more common in the female half of the population.
- Pathologies of the genitourinary organs - inflammatory processes always affect the permeability of the vascular walls. An increase in red blood cells in the urine is observed with urolithiasis, pyelonephritis, functional renal failure, and especially glomerulonephritis.
- Hemophilia is a disease that occurs with severe disorders affecting the circulatory system. In such a situation, the blood clotting function suffers, and hematuria also appears.
- Hydronephrosis is an increase in the volume of the pelvis and calyces of the filtering organs, which occurs due to improper outflow and retention of urine. Prolonged residence of fluid in the upper parts of the urethral canal leads to the fact that the discharge stagnates. Pathogenic microorganisms begin to actively multiply in them, so the level of red blood cells and bacteria in the urine increases significantly.
- Erosion of the uterine cervix occurs with damage to the vascular walls. With this disease, bloody impurities are almost always found in the urine.
- Traumatization of the urinary canal - severe mechanical damage to these organs is characterized by severe hematuria.
- Infectious diseases - a small amount of red blood cells often ends up in the secretions of malaria, febrile conditions, and chickenpox.
- Bleeding from the reproductive organs - red blood components are carried into the urine from the vagina, uterus or genitals during urination (for example, with uterine bleeding).
- Other pathologies - an increase in red blood cells in the secreted fluid often occurs with various disorders of the blood coagulation system, mononucleosis, heart failure, and tumor processes.
But the very presence of these components in urine does not always indicate a possible infection or pathological changes occurring in the patient’s body. The permeability of the walls of blood vessels is also affected by the use of certain medications - Ascorbic acid, Hexamine, drugs of the sulfonamide group and anticoagulants.
Important! A couple of days before the urine test, it is recommended to somewhat limit the consumption of very salty or spicy foods. Drinking sour juices and fruit drinks on the eve of the test, or heavy physical labor can slightly increase the level of red blood cells in the secretions.
Platelets: structure and functions
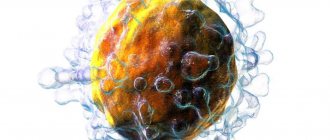
Red blood platelets - erythrocytes
Platelets (PLT) are platelets with a diameter of 2 - 11 microns. These cells do not contain nuclei and are round or oval in shape. But their shape changes when bleeding occurs. As soon as a vessel is damaged, the platelet takes on a spherical shape and releases pseudopods, with the help of which it connects with other platelets and aggregates to the site of damage.
The granules contain the elements necessary for coagulation: coagulation factors, fibrinogen, calcium ions, and growth factor. Some anticoagulants and coagulation factors may be on the surface of the plates.
The main function is to ensure the integrity of the circulatory system through the process of coagulation. When the vessel wall is damaged, collagen is released, to the fibers of which nearby platelets adhere. By releasing the contents of the granules, platelets trigger a chain of reactions that form a blood clot that prevents blood loss.
In addition to participating in the hemostasis system, platelets promote tissue regeneration by releasing growth factors from their granules, which stimulate cell proliferation. Another function is to nourish the endothelium of the blood vessels of the circulatory system.
Protection against infections
Blood is made up of several components, including red blood cells, white blood cells, platelets, and plasma. A healthy adult has between 4,500 and 11,000 white blood cells per cubic millimeter of blood. White blood cells, also called leukocytes or white corpuscles, are a cellular component of blood that protects the body from infection and disease by ingesting foreign materials and destroying infectious agents, including cancer cells, and by producing antibodies.
An abnormal increase in the number of white cells is known as leukocytosis, while an abnormal decrease in the number is called leukopenia. The number of white blood cells can increase in response to intense physical activity, convulsions, acute emotional reactions, pain, pregnancy, childbirth and some other painful conditions, such as infections and intoxications.
Norms of blood cells
Standard indicators expressed in absolute values.
| Shaped elements | Norm |
| red blood cells | 4.0 - 5.5*1012/l |
| leukocytes | 4.0 - 9.0*109/l |
| band neutrophils | 0.04 - 0.3*109/l |
| segmented neutrophils | 2.0 - 5.5*109/l |
| eosinophils | 0.02 - 0.3*109/l |
| basophils | 0.02 - 0.06*109/l |
| lymphocytes | 1.2 - 3.0*109/l |
| monocytes | 0.09 - 0.6*109/l |
| platelets | 180 - 320*109/l |
Subgroups of leukocytes in the analysis results can be presented as a ratio to the total number of leukocytes.
| Leukocytes | Ratio(%) |
| band neutrophils | 1 — 6 |
| segmented neutrophils | 40 — 70 |
| eosinophils | 1 — 4 |
| basophils | 0,2 — 1 |
| lymphocytes | 20 — 37 |
| monocytes | 4 — 10 |
Increased levels of leukocytes in urine - reasons
Any inflammatory reaction that affects the urinary tract occurs with an increased content of white blood cells in the urine. In adult females and males, the norm of leukocytes in the secretions is no more than 3 units. For pregnant patients and children, this value is considered normal when the content of white components is from 0 to 4-6 in the field of view.
An increase in the concentration of leukocytes in the urine of more than 8-10 units, visible in the lens of the device, indicates an infectious or inflammatory lesion of the genitourinary area. If the level of these cells increases, the patient is urgently referred to the appropriate doctor - urologist, nephrologist. Often, with leukocyturia, a large number of bacteria are found in the urine during the study.
The following pathologies can cause an increased content of white blood components in urine:
- Pyelonephritis - this disease is a purulent inflammation of the pyelocaliceal apparatus of the kidney. It occurs due to infection, so the disease is characterized not only by leukocyturia, but also by the presence of bacteria in the urine.
- Malignant neoplasms of the kidneys - oncological processes also occur with an increase in the level of leukocytes and erythrocytes in the secretions. At the beginning of the development of a tumor, its appearance is often indicated only by some changes in the urine test, which is why it is so important to monitor this indicator. Timely detected pathology is cured in 8 out of 10 cases.
- Urolithiasis - the formation of stones in the urethral canal is also accompanied by leukocyturia. When a stone with sharp edges moves through the lumen of the ureters, it can scratch the mucous membrane and cause minor blood loss. In this case, a person experiences an increase in leukocytes and red blood cells in the urine.
- Tuberculosis of the urinary tract - manifests itself as a result of human infection with the tuberculosis bacillus. In the absence of timely treatment, urethral damage develops 2.5-3 years after the mycobacterium enters the body. Harmful microflora is carried by blood throughout the body and causes a corresponding immune response. Leukocyte cells try to fight infection in the urinary tract, which is why they are found in the secreted fluid.
- Cystitis - if the pathological process occurs due to bacterial or viral infection, then an increase in leukocytes is necessarily detected in the urine.
- Other factors in such a situation include chronic, sluggish inflammation of the genital area and sexually transmitted diseases, hypothermia, allergies, helminthiasis, decreased efficiency of the immune system, physical inactivity, use of medications (Ampicillin, Kanamycin, Aspirin) and the use of iron salts.
An important component of the blood system
White blood cells are an important component of the blood system, which also consists of red blood cells, platelets and plasma. Although they make up only about 1% of all blood, their impact is significant: they are essential for good health and protection against disease. We can say that these are immune cells.
When a specific area is attacked, white blood cells rush to destroy the harmful substance and prevent disease. White blood cells are produced within the bone marrow and stored in the blood and lymph tissues. Since the lifespan of human leukocytes is short, some types have a completely short lifespan - from one to three days. Therefore, the bone marrow is engaged in their constant reproduction.
Leukocyte disorders
The main disorders of leukocytes include the following pathological conditions:
- Neutropenia (abnormally low neutrophil count).
- Neutrophil leukocytosis (abnormally high number of neutrophils).
- Lymphocytopenia (abnormally low number of lymphocytes).
- Lymphocytic leukocytosis (abnormally high number of lymphocytes).
The most common are disorders of neutrophils and lymphocytes. Abnormalities associated with monocytes and eosinophils are less common, and problems associated with basophils are less common.