The medical diagnostics industry already has enough methods in its arsenal to determine the disease that has affected a particular organ. MRI (magnetic resonance imaging) is an examination that has firmly taken a leading position due to its features. What MRI is and why the technique has become in demand in the last few decades almost throughout the civilized world can be found out by becoming familiar with the operating principle of the equipment used to carry out the procedure.
MRI - how the word stands for
MRI (magnetic resonance imaging) is a modern high-tech non-radiation method used to diagnose various pathologies of tissues and internal organs.
Without resorting to internal intervention, MRI makes it possible to obtain highly informative images of any body structure, including in three-dimensional projections.
The advantage of the examination is its complete safety; ionizing radiation is completely excluded. Diagnosis is carried out even on pregnant women and young children.
Medicine has gained wide diagnostic capabilities thanks to the use of MRI. In order for the result to be of high quality, during the examination the patient must strictly follow the doctor’s instructions. The specialist knows how the MRI is interpreted; he takes into account data from other studies and anamnesis.
Preparing for the examination
The positive side of the magnetic resonance scanning method is the almost complete lack of preparation for diagnosis. But doctors advise a few days before the tomography session to stop drinking alcohol and not to eat a lot of food that is difficult for the gastrointestinal tract. Although this remains at the level of recommendations. If contrast is used, it is better to eat heavily. This will help avoid attacks of nausea.
Before the procedure, you need to remove all metal jewelry, cufflinks, watches, glasses, and removable dentures. There should be no metal parts left on clothing. Modern medical diagnostic centers provide sets of disposable clothing for examination. The best thing is to change into it. If an unnoticed metal part remains in your clothing, then when examining the brain or neck, you may subsequently experience a headache from the presence of a foreign iron object on the clothing.
The scanning device is a tunnel into which a table with a patient slides. It is important not to move during the examination, then the images will be clear and of high quality. To prevent accidental movement of the limbs, the patient’s arms and legs are secured to the table with soft straps.
MRI can be used to diagnose any organ without harm, the procedure is painless
Main indications for MRI
In the following conditions, an MRI examination is recommended:
- circulatory disorders;
- developmental defects;
- various tumor processes;
- monitoring the patient after surgery or during therapy;
- degenerative, demyelinating changes;
- arteriovenous malformations, aneurysms, thrombosis, vascular stenosis, various vascular pathologies;
- inflammatory processes;
- chronic, acute sinusitis;
- previous injuries;
- arthrosis, bursitis, arthritis;
- compression of the spinal cord, spinal nerve roots;
- heart defects, coronary disease, myocardial infarction;
- damage to tendons, ligaments, joints, menisci, nerve endings, muscles;
- pathologies of the pelvis and abdominal organs.
If a doctor detects any of the listed conditions in a patient, he will refer the patient for an MRI to conduct a reliable examination. After that
As the MRI is interpreted, an accurate diagnosis is established.
In what cases should tomography not be done?
There are serious limitations for magnetic resonance scanning:
- early pregnancy;
- claustrophobia;
- mental disorders, when a person cannot remain in a stationary position for a long time and control his condition;
- metal inclusions in the patient’s body – pins, clips on blood vessels, staples, prostheses, knitting needles;
- implanted electronic devices that operate constantly and cannot be removed during tomography, for example, pacemakers;
- epilepsy;
- tattoos made with paint containing metal particles;
- the patient’s severe physical condition, for example, being constantly on a ventilator.
There are no such contraindications for computed tomography. It is prescribed if it is impossible to do an MRI. Such an examination is suitable where a tomograph does not work.
Metal fragments in the body make images blurry and difficult to decipher. Electronic devices break under the influence of a strong magnet. When using a tomograph, restrictions must be observed to avoid such troubles.
Benefits of MRI
In medicine, MRI is preferred in diagnosing soft tissue pathologies. The examination is widely used in oncology, in the diagnosis of diseases of the brain, spine, as well as in angiology and some other areas of medicine. The key advantages of this method are:
- no radiation exposure compared to CT examination;
- the method is highly informative in diagnosing tumor development in the early stages;
- high-quality images are possible without the use of contrast;
- the examination clarifies not only the structure, but also functional parameters (speed of blood flow, cerebrospinal fluid, activation of the cerebral cortex). A trained specialist knows how MRI is interpreted based on these indicators.
MRI is practically not used in diagnosing pathologies of the lungs, intestines, stomach and bones.
Operating principle and advantages over other diagnostic methods
The operating principle of an MRI scanner is based on the characteristics of the magnetic field and the magnetic properties of body tissue. Thanks to the interaction of nuclear magnetic resonance and the nuclei of hydrogen atoms, during the examination a layer-by-layer image of the organs of the human body is displayed on the computer screen. In this way, it is possible not only to differentiate some organs and tissues from others, but also to record the presence of even minor disorders, tumor and inflammatory processes.
The operating principle of MRI allows you to accurately assess the condition of soft tissues, cartilage, brain, organs, spinal discs, ligaments - those structures that are largely composed of fluid. At the same time, MRI is used less in medicine if it is necessary to study bones or tissues of the lungs, intestines, stomach - structures in which the water content is minimal.
Closed-type tomography apparatus
Due to the way MRI works, there are a number of advantages of this type of research over others:
- As a result of the examination, it is possible to obtain a detailed image. Therefore, this technique is considered the most effective for the early detection of tumors and foci of inflammation, the study of disorders of the central nervous system, musculoskeletal system, abdominal and pelvic organs, brain, spine, joints, and blood vessels.
- Magnetic tomography allows diagnostics to be made in areas where CT is not effective due to the overlap of the examined area with bone tissue or due to the insensitivity of CT to changes in tissue density.
- There is no ionizing radiation to the patient during the procedure.
- It is possible to obtain not only an image of the structure of tissues, but also MRI indications of their functioning. For example, the speed of blood flow, cerebrospinal fluid flow and brain activity are recorded using functional magnetic resonance imaging.
- Possibility of conducting contrast MRI. The contrast agent increases the diagnostic potential of the procedure.
- Open MRIs allow patients with fear of closed spaces to undergo examinations.
Another advantage is that errors are virtually eliminated when making a diagnosis. If the patient is concerned with the question: “Can MRI be wrong?”, then the answer is a little ambiguous. On the one hand, this procedure is one of the most accurate diagnostic methods. On the other hand, errors can occur at the stage of deciphering the results and making a diagnosis by the doctor.
How is the examination carried out?
In most cases, special preparation is not required for MRI. An exception is abdominal MRI.
Before undergoing the procedure, the doctor asks the patient to remove all metal objects (buttons, jewelry, etc.), as they will negatively affect the quality of the examination.
The patient goes into the research room, where he is placed in a special tube. In some devices you can stand during the examination, but the image quality is lower.
During the procedure, it is possible to talk with the doctor through an intercom; he carefully monitors the patient using video equipment.
For the highest quality image, the main requirement is complete stillness. The process takes about half an hour.
Contrast agents may be used to help certain areas be seen more clearly.
During examination, some patients are bothered by noise; this is normal in the operation of the equipment. You can use headphones to eliminate discomfort.
Some people experience claustrophobia; such patients are recommended to undergo examination in an open-type apparatus.
If an examination is carried out on newborns or small children, the doctor uses short-term anesthesia, because it is difficult for babies to remain still.
Those who are nervous before the procedure or have had any negative experiences can take mild sedatives to calm them down.
Conducting research
So, a fully prepared patient is placed on a hardware table-couch and the medical staff fixes him to ensure complete immobility, taking into account which area needs to be examined. To secure the patient's body, specially designed belts and bolsters are used. At the same time, it is explained to him that the operation of the tomograph is accompanied by a rather loud noise - tapping, humming - that this is absolutely normal and should not cause concern.
Special mount for MRI of the head
For comfort during the procedure, the patient is offered headphones or earplugs, which will help get rid of unpleasant noise effects. Notify about the presence of two-way communication between the diagnostic room and the room in which the specialist managing the process is located. At any time, if the patient feels an increase in panic or a change in his condition towards deterioration, he can inform the doctor and he will interrupt the scan.
Of course, it will be good if the patient, before undergoing an MRI, reads reviews about it on any Internet portals left by people who have already undergone diagnostics. Then he can prepare himself mentally. If he knows that in such situations he may get scared, then he should invite a loved one with him to the procedure in advance. To do this, you need to first find out whether the accompanying person has any contraindications to being in the electromagnetic field, so as not to harm him or create interference with the procedure.
If all the conditions are met, then the tomograph couch on which the patient is located is moved into the apparatus tunnel and a magnetic resonance scan is started. The procedure itself can last from 20 minutes to an hour - it depends on the characteristics of the area being examined. If there are indications for MRI with contrast, for example, in case of suspected oncological processes, then the diagnostic time, as a rule, doubles.
MRI contraindications
Although an MRI examination is a fairly safe procedure, there are still a number of contraindications:
- the patient has a pacemaker;
- metal plates, any fragments, Ilizarov apparatus;
- some implants in the middle ear;
- Examination is not recommended for patients with unstable mental health;
- pregnant women in the first trimester - there is still no information about how magnetic fields affect the development of the fetus;
- coma or severe illness (stage of decompensation);
- the presence of tattoos if they contain any metal-based dyes.
- if a contrast agent is used, then contraindications include allergic reactions to the constituent components.
Do I need to prepare for the procedure?
Diagnostics using an electromagnetic field does not require a preparatory process. There is no need to adhere to a specific diet or diet. Only if it is necessary to examine the pelvic organs, you need to come to the procedure with a full bladder - since MRI diagnoses this area with the walls of the organ straightened.
There is one more point to consider when ordering a contrast-enhanced MRI. Even if non-allergic drugs based on gadolinium salts (Omniscan, Gadovist) are used for contrast contrast, a test must still be performed first. Individual intolerance of each individual patient cannot be ruled out.
Before going for the procedure, it is best to think over your clothes and choose one that does not contain metal objects - zippers, buttons, rhinestones and other decorations. Some private clinics offer to change into a medical gown specially designed for this type of event. You should not come to an MRI wearing underwear with lurex, as its thread is created with an admixture of iron.
Immediately before the diagnosis, you need to remove all jewelry, watches, glasses, removable dentures and ear aids.
An important point that should not be ignored is visiting the office with all previous, if any, examination results. This will allow the doctor to immediately compare new images and draw a conclusion about the effectiveness of treatment or the rate of progression of the disease or its remission. MRI machines create such a powerful magnetic field that there are no metal objects in the diagnostic room - couches, crutches, canes and other personal belongings of patients - all objects remain behind the door of the room. After which only the patient is allowed to undergo diagnostics.
What does MRI stand for in medicine?
The results of an MRI examination are released in the form of layer-by-layer images. They can be immediately seen on the monitor; they are recorded on a disk, which the patient receives along with the images.
The main diagnostic factor is deciphering the results. This is not an easy process that requires special knowledge. Only a professional knows how an MRI of the brain or other organ is interpreted.
Correct interpretation of the result, together with other indicators from the medical history, allows the doctor to establish an accurate diagnosis and prescribe the correct effective treatment.
In some cases, some patients receive remote consultation via the Internet to interpret MRI results.
If the case is complex or controversial, the doctor takes several images from different angles, so the picture becomes more complete and reliable. This makes the diagnosis more accurate.
As for the duration of decoding, it takes much longer than the examination itself. For example, an MRI of the brain takes about one and a half hours to decipher.
MRI for microstroke
Very often, a microstroke is easier to identify from the outside than on your own (because people sometimes ignore their symptoms), so what symptoms of a microstroke appear first:
- the person suddenly, for no reason, fell silent and began to speak incoherently (the photo shows the main symptoms of a mini-stroke);
- you are forced to ask him again several times;
- he does not respond to your questions, looks confused, in prostration;
- suddenly drops an object that was previously held tightly;
- It’s not on the first try that you manage to lift that object;
- suddenly begins to stutter;
- movements resemble a person who is intoxicated.
What to do when the first signs are identified When the first symptoms and signs of a microstroke are identified, it is necessary to provide the patient with complete rest. If possible, place him on high pillows (so that his head is in an elevated position).
How to minimize the consequences
Prognosis and consequences regarding further human conditions directly depend on the causes and symptoms of a mini-stroke. If the cause is more superficial (for example, stress, obesity), then most likely, eliminating negative factors will be the best prevention of further micro-strokes and possible stroke. However, if the cause of a micro-stroke is a consequence of a certain disease, then it is worth choosing additional comprehensive treatment. It has been proven that even one minor stroke is an indication of the possibility of a major stroke in one out of ten cases. And many people know about the consequences of a massive stroke - this is irreparable damage to health. Or death. Get examined by a doctor in a timely manner to prevent relapse or the development of complications! The first micro-stroke tells us that we need to be more attentive to the body.
Video: How not to miss a micro-stroke? A microstroke does not cause significant harm, but it does indicate difficulties within the body. What are the consequences of the attack in the future?
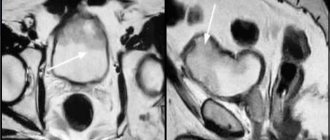
An MRI of the cervical spine and head may not show a stroke in the acute period if standard classical research protocols are used, although even with classical protocols, MRI in diagnosing a stroke reveals changes much faster compared to CT (computed tomography). This is a T2 MRI image of a patient who showed neurological symptoms two hours ago. Conclusion is the norm. The same patient who underwent diffusion-weighted and perfusion MRI scans. Lesion in the basin of the right middle cerebral artery. The patient was prescribed intensive therapy.
What does an MRI show after a stroke?
On MRI sequences such as PD/T2WI (proton-weighted imaging) and FLAIR (fluid attenuation inversion recovery) MRI sequences appear to be high intensity signal from a lesion. MRI sequences such as PD/T2WI (proton-weighted imaging) and FLAIR (fluid-attenuated inversion recovery) detect up to 80% of strokes with first-onset symptoms within 24 hours.
In up to 30% of cases, for the first time 2-4 hours after the onset of symptoms, these sequences may not detect a stroke, then DWI (Diffusion weighted imaging) comes to the rescue. The high signal on these classic MRI sequences is the result of irreversible brain damage—cell death. A high signal is very bad news, indicating the death of brain tissue.
Is it possible to decrypt it yourself?
MRI is the most accurate method in diagnosis. The patient receives black and white photographs, as well as recordings on digital media. In addition, the photographs are accompanied by a conclusion from specialists, which is written based on the results of the study.
Some people wonder how an MRI of the brain is deciphered independently. In fact, this requires a long learning curve. You can, of course, try to study reference literature, medical atlases, catalogs, but only a specialist can decipher the full picture; only his eye can see the smallest problems in the photographs.
It is only possible to see a major pathology on your own if it is pronounced. But never try to diagnose yourself. The human body is a complex structure and any self-medication can only harm your health.
Deciphering MRI is impossible without experience and special education. In addition, additional studies may be required to make a correct diagnosis.
What are MRI images and how to understand them?
To understand what MRI is, I read quite a lot of material on the Internet, and what I suggest you read is the work of many authors, which I combined in one article. I do not claim to be the author of this article, but unfortunately, I also cannot name the authors whose materials I used. For this I apologize. Magnetic resonance imaging (nuclear magnetic resonance imaging, MRI, nuclear magnetic resonance imaging, MRI, NMR) is a non-radiological method for studying internal organs and human tissues. This method does not use X-rays and is safe for most people.
How the research is carried out
MRI technology is quite complex: the effect of resonant absorption of electromagnetic waves by atoms is used. A person is placed in a magnetic field that is created by the device. Molecules in the body unfold according to the direction of the magnetic field. After this, scanning is carried out using a radio wave. The change in the state of the molecules is recorded on a special matrix and transmitted to a computer, where the received data is processed. Unlike computed tomography, MRI allows you to obtain an image of the pathological process in different planes. A magnetic resonance imaging scanner is similar in appearance to a computer scanner.
The study is carried out in the same way as a computed tomography scan.
The table gradually moves along the scanner. An MRI requires more time than a CT scan and usually takes at least 1 hour (diagnosis of one section of the spine takes 20-30 minutes). The technique was called magnetic resonance imaging , rather than nuclear magnetic resonance imaging (NMRI), due to negative associations with the word "nuclear" in the late 1970s.
MRI is based on the principles of nuclear magnetic resonance (NMR), a spectroscopy technique used by scientists to obtain data about the chemical and physical properties of molecules. MRI originated as a tomographic imaging technique that produces images of the NMR signal from thin sections passing through the human body. MRI has evolved from a tomographic imaging technique to a volumetric imaging technique. The method is especially effective for studying dynamic processes (for example, the state of blood flow and the results of its disturbance) in organs and tissues. Advantages of Magnetic Resonance Imaging MRI better visualizes some structures of the brain and spinal cord, as well as other neural structures. In this regard, it is more often used to diagnose damage, tumor formations of the nervous system, as well as in oncology, when it is necessary to determine the presence and extent of the tumor process. The list of diseases that can be detected using MRI is impressive: inflammatory, dystrophic and tumor lesions of blood vessels and the heart, thoracic and abdominal organs, damage to the lymph nodes, parasitic processes and other pathologies.
Is magnetic resonance imaging harmful?
Currently, nothing is known about the harm of a magnetic field. However, most scientists believe that in conditions where there is no data on its complete safety, pregnant women should not be subjected to such studies. For these reasons, as well as due to the high cost and low availability of equipment, computed tomography and nuclear magnetic resonance imaging are prescribed according to strict indications in cases of a controversial diagnosis or the failure of other research methods. MRI cannot also be performed on those people whose bodies contain various metal structures - artificial joints, heart pacemakers, defibrillators, orthopedic structures that support bones, etc. Like other research methods, computed tomography and magnetic resonance imaging are prescribed only by a doctor. Not all medical institutions carry out these studies, so if necessary, try to contact a diagnostic center.
Sectional anatomy of the spine
Color codes for the spinal column.
MRI of the spine
1. Nuchal ligament 2. Tooth of the second cervical vertebra 3. Prominent vertebra C 7 4. Thoracic vertebral body T1 5. Spinal canal 6. Thoracic spinal cord 7. Intervertebral disc 8. Supraspinous ligaments 9. Infraspinous ligaments 10. Lumbar vertebral body L1 11. Conus medullaris 12. Cauda equina 13. Spinous process 14. Thecal bursa 15. Sacrum (S1) 16. Sacral promontory 17. Coccyx
MRI of the cervical spine
1. Foramen magnum 2. Trapezius muscle (descending part) 3. Integumentary membrane 4. Occipital bone (internal occipital protuberance) 5. Anterior atlanto-occipital membrane 6. Semispinalis capitis muscle 7. Apical ligament of the odontoid process 8. Dorsal rectus minor muscle head 9. Longitudinal fasciculus 10. Posterior atlanto-occipital membrane 11. Second cervical vertebra (anterior arch) 12. Suboccipital fatty tissue 13. Middle atlanto-axial joint 14. Second cervical vertebra (posterior arch) 15. First cervical vertebra (odontoid process) ) 16. Deep veins of the neck 17. First cervical vertebra (body) 18. Transverse ligament of the first cervical vertebra 19. Longus capitis muscle 20. Posterior longitudinal ligament 21. Lower end plate of the C3 vertebra 22. Interspinous ligament 23. Upper end plate of the C4 vertebra 24 Cervical spinal cord 25. Anterior longitudinal ligament 26. Subarachnoid space 27. Intervertebral disc 28. Interspinous muscles 29. Esophagus 30. C7 spinous process 31. Basal vertebral veins 32. Ligamentum flavum 33. T1 thoracic vertebral body 34. Supraspinous ligament 35. Spinal canal
MRI – cervical spine
1. External auditory canal 2. Stylomastoid foramen 3. Vertebral vein 4. Internal jugular vein 5. Occipital condyle 6. Mastoid process 7. Parotid salivary gland 8. Lateral rectus capitis muscle 9. Atlanto-occipital joint 10. Integumentary membrane 11. Second cervical vertebra 12. Transverse ligament 13. Second cervical vertebra (transverse process) 14. Digastric muscle (posterior belly) 15. Second cervical vertebra (odontoid process) 16. Cuneiform ligaments 17. C2 spinal nerve 18. Vertebral artery 19. Lateral atlantoaxial joint 20. Inferior oblique capitis muscle 21. Intervertebral joint 22. Levator scapulae muscle 23. First cervical vertebra (body) 24. Spinal ganglion S3 25. Cervical plexus 26. Sternocleidomastoid muscle 27. Average scalene muscle 28. Intervertebral disc (C2/S3) 29. Transverse process of C7 30. Superior articular process of C4 31. Cervical vertebral body C7 32. Inferior articular process 33. Spinal nerve C8 34. Uncinate process of C7 35. Posterior scalene muscle 36. Subclavian artery 37. Esophagus 38. Longus colli muscle 39 .Lung
Thoracic spine
1. Esophagus 2. Seventh cervical vertebra 3. Thyroid gland 4. Interspinous muscle of the neck 5. Trachea 6. Supraspinous ligament 7. Sternohyoid muscle 8. Body of the T4 thoracic vertebra 9. Brachiocephalic trunk 10. Interspinous ligament 11. Sternum (handle) 12. Spinous process 13. Left brachiocephalic vein 14. Basal vertebral vein 15. Ascending aorta 16. Thoracic spinal cord 17. Anterior longitudinal ligament 18. Posterior intercostal artery 19. Pulmonary artery 20. Posterior longitudinal ligament 21. Inferior end plate of the T6 vertebra 22 Intervertebral disc T9/T10 23. Left atrium 24. Ligamentum flavum 25. Superior end plate of the T7 vertebra 26. Epidural fat 27. Azygos vein 28. Conus medullaris 29. Intervertebral disc T9/T10 30. Cauda equina 31. Liver 32. Filum terminale of the spinal cord 33. Descending aorta MRI of the thoracic spine
1. Trachea 2. Splenius neck muscle 3. Thyroid gland 4. Semispinalis capitis muscle 5. Sternohyoid muscle 6. Serratus posterior superior muscle 7. Esophagus 8. Rhomboid major muscle 9. Brachiocephalic trunk 10. Intervertebral joint T3/T4 11. Left brachiocephalic muscle vein 12. Inferior articular process T4 13. Sternum (manubrium) 14. Superior articular process T5 15. Left main bronchus 16. Trapezius muscle 17. Ascending aorta 18. Posterior intercostal artery 19. Pulmonary artery 20. Intervertebral vein 21. Hemizygos vein 22 . Erector trunk muscle 23. Intervertebral disc T7/T8 24. Intervertebral foramen 25. Left atrium 26. Spinal ganglion (dorsal root) 27. Superior end plate of the T vertebra 28. Spinal ganglion (ventral root) 29. Right atrium 30. Multifidus floor spinalis thoracis muscle 31. Inferior end plate of the vertebra 32. Posterior external vertebral venous plexus 33. Body of the thoracic vertebra 34. Latissimus dorsi muscle 35. Descending aorta 36. Leg of the vertebral arch 37. Liver 38. Ligamentum flavum MRI of the lumbar spine
1. Spinal cord 2. Conus medullaris 3. Abdominal aorta 4. Ligamentum flavum 5. Lumbar vertebral body L1 6. Spinous process L1 7. Intervertebral disc L1/L2 (nucleus pulposus) 8. Interspinous ligament 9. Anterior longitudinal ligament 10. Supraspinous ligament 11. Intervertebral disc L2/L3 12. Cauda equina 13. Basal vertebral vein 14. Epidural fatty tissue 15. Left common iliac vein 16. Posterior longitudinal ligament 17. Sacral canal 18. Thecal bursa (lumbar cistern) 19. Sacral promontory 20. Dura mater 21. Sacrum (S1) 22. Medial sacral crest MRI of the lumbar spine
1. Diaphragm (lumbar part) 2. Thoracic fascia 3. Anterior external vertebral venous plexus 4. Erector trunk muscle 5. Posterior intercostal artery 6. Nerve fibers 7. Thoracic vertebral body 8. Superior articular process 9. Lumbar vertebral body L1 10. Posterior vertebral arch (plate) 11. Intervertebral disc L1/L2 12. Ligamentum flavum 13. Inferior vena cava 14. Anterior internal vertebral venous plexus 15. Intervertebral disc L2/L3 16. Lumbar artery and nerve 17. Lumbar artery 18 Multifidus muscle 19. Common iliac artery 20. Sacrum (S1) 21. Spinal ganglion 22. Medial sacral crest 23. Promontory of the sacrum MRI of the spine is currently the main method of choice in the diagnosis of herniated intervertebral discs , which are the most common cause of pain in the spine (up to 80%), as well as other degenerative-dystrophic diseases of the spine, inflammatory and tumor changes in the vertebrae, soft tissues and structures of the spinal cord.
Today, MRI is the optimal method for screening and differential diagnosis of pathological changes in the spinal cord, as well as the only method for diagnosing its demyelinating diseases.
Magnetic resonance imaging of the spine allows us to identify traumatic injuries to the structures of the spinal canal , including those invisible on radiographs. The use of contrast in addition to standard examination allows for differential diagnosis of space-occupying lesions and other diseases in this area. MRI is an indispensable method for assessing indications for therapeutic or surgical treatment of most spinal diseases, as well as monitoring the effectiveness of the chosen treatment. The method makes it possible to assess static disorders (strengthening and straightening of natural curves, scoliosis), detect vertebral displacements (spondylolisthesis), and metabolic disorders (osteoporosis).
Extended tumor of the spinal cord. After the administration of a contrast agent, its pronounced accumulation in a space-occupying formation is determined. In modern MR centers, examination of the spine is performed using high-field (1.5T) MRI and ultra-high-field (3T), which has a higher resolution with a smaller slice thickness, MRI. Thanks to the ultra wide aperture (70 cm) and its short length, the 3T tomograph provides maximum comfort for the patient during the examination, including those with mild forms of claustrophobia. In addition, the device allows you to examine patients weighing more than 110 kg. If your weight exceeds 110 kg, it is optimal to conduct a 3 T MRI examination. During the study, if a number of pathological changes are detected, indications for intravenous administration of a contrast agent may arise. Contrast agents used for MRI do not contain iodine, are safe for the body and do not cause allergic reactions. If necessary, you will definitely be offered to conduct an extended study. The decision on the final scope of the study should always be left to the patient, but following the recommendations of specialists helps the patient receive the most informative conclusion, and subsequently save time and money by avoiding the need for a repeat diagnostic procedure. Modern centers are ready to offer a large list of MRI studies of the spine, covering the following areas and their various combinations:
Craniovertebral region and cervical spine. Indications for using the method:
• herniated intervertebral discs, as a manifestation of osteochondrosis, which are the most common cause of pain in the cervical spine with possible irradiation to the shoulder joints, upper limbs and head; • large disc herniations that put pressure on the spinal cord and nerve roots, as well as causing ischemic damage, which in turn leads to disturbances in the sensitivity and motor function of the upper extremities; • tumors of the cervical spine, including secondary (metastatic) ones; • demyelinating processes (multiple sclerosis, acute disseminated encephalomyelitis). In this case, MRI is the only method for instrumental diagnosis of demyelinating diseases; • traumatic damage to the structures of the spinal canal, including in the absence of changes on the radiograph. MRI is the method of choice in the diagnosis of traumatic injuries to spinal cord structures; • inflammatory diseases of the structures of the spinal canal, both specific and non-specific, non-infectious inflammatory diseases (ankylosing spondylitis, rheumatoid arthritis, Reiter's syndrome); • acute violation of spinal circulation, as well as vascular malformations; • granulomatous, fungal, parasitic infections of the spinal cord and other structures of the spinal canal; • developmental anomalies of the spine.
Indications for MRI of the thoracic spine:
• herniated intervertebral discs, especially causing pain in the thoracic spine with possible irradiation (reflection) into the chest and abdominal wall, organs of the chest and abdominal cavity, often simulating angina pectoris, intercostal neuralgia, cholecystitis, pancreatitis and other diseases of internal organs; • tumors of the thoracic spine, including secondary (metastatic) ones; • demyelinating processes (multiple sclerosis, acute disseminated encephalomyelitis). MRI is the only method for instrumental diagnosis of demyelinating diseases; • traumatic damage to the structures of the spinal canal, including in the absence of changes on the radiograph. MRI is the method of choice in the diagnosis of traumatic injuries to spinal cord structures; • inflammatory diseases of the structures of the spinal canal, both specific and non-specific, non-infectious inflammatory diseases (ankylosing spondylitis (ankylosing spondylitis (Bechterew's disease), rheumatoid arthritis, Reiter's syndrome); • acute violation of spinal circulation, as well as vascular malformations; • granulomatous, fungal, parasitic infections; • developmental anomalies of the spine.
Indications for MRI of the lumbosacral spine and/or coccyx:
• herniated intervertebral discs, causing pain in the lumbosacral spine with possible irradiation to the hip joints, lower extremities, pelvic organs, or leading to impaired sensitivity and motor dysfunction of the lower extremities and pelvic organs; • tumors of the lumbosacral spine, including secondary (metastatic) ones; • traumatic damage to the structures of the spinal canal, including in the absence of changes on the radiograph. MRI is the method of choice in the diagnosis of traumatic injuries to spinal cord structures; • inflammatory diseases of the structures of the spinal canal, both specific and non-specific, non-infectious inflammatory diseases (ankylosing spondylitis, ankylosing spondylitis, ankylosing spondylitis, psoriatic arthritis, Reiter's syndrome, etc.); • vascular malformations; • suspicion of the presence of granulomatous, fungal, parasitic infections of the structures of the spinal canal; • developmental anomalies of the spine.
Magnetic resonance imaging of the spine does not require special preliminary preparation. The patient must have with him all medical documentation related to the area of interest: postoperative statements, data from previous studies, such as MRI (images and reports, if available), ultrasound, SCT. A referral from your primary care physician is encouraged. The doctor needs this information before performing the diagnostic procedure in order to think through and optimally plan the course of the magnetic resonance examination.
Decoding MRI of the brain
MRI of the brain produces layer-by-layer images. If someone is thinking about how to decipher an MRI of the brain themselves, we repeat - you shouldn’t do it. This will be done by a diagnostician, he will carefully study the result and draw up a diagnostic conclusion. Only a qualified specialist will correctly and objectively decipher the image and correlate the description with the clinical picture.
The doctor will examine in detail and determine the size of the bones, blood vessels, the presence of lesions with fluid, and will see possible tumors and foreign bodies. The presented picture corresponds to the norms (they are different for different age groups).
Possible deviations that a diagnostician can detect in the images:
- expansion of the ventricles of the brain;
- damaged nerve fibers;
- aneurysms;
- violation of the integrity of bones or blood vessels
- bone deformation;
- tumors.
To identify such pathologies, you must have qualifications, so do not think about how to interpret an MRI of the brain yourself, but entrust the process to a doctor.
All examination results are recorded in a coding sheet, which is attached to the medical record.
To perform an MRI, contact only professionals; even a small oversight in decoding during diagnosis can play a huge role not in your favor. The MRI method detects various diseases at the earliest stages, and this is a guarantee of successful treatment.
When is contrast used?
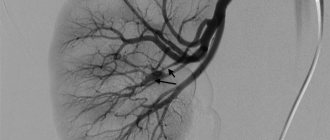
Sometimes a contrast agent is injected into the patient's vein before the examination. This is necessary to obtain a clearer image of some areas in the photographs. MRI works with it in more detail. This happens when diagnosing tumors. The contrast agent accumulates in the tumors and additionally highlights them in the images. When diagnosing a vascular aneurysm, a whole diagram of the circulatory system is drawn with contrast, which makes it easier for the doctor to identify disorders.
Gadolinium is used as a contrast agent for MRI. It works to illuminate blood vessels and is excreted from the body by the kidneys, is well tolerated by patients, and rarely causes an allergic reaction. There are certain contraindications to its use. Therefore, before administering the drug, tests are carried out to determine its tolerability.
The use of contrast media is contraindicated:
- persons with an allergic reaction to gadolinium;
- pregnant and lactating women;
- people with diabetes;
- patients with chronic kidney disease.
After the tomography procedure, gadolinium is excreted through the kidneys within a few hours. Excessive stress on them can provoke an exacerbation of chronic pathologies. This is why contrast is not used for sick kidneys.
Interpretation of MRI of the spine
How is MRI of the spine interpreted? After the images are received, using a special viewer program, the radiologist makes a visual assessment of the examination and forms an expert opinion. The results are printed on photographic paper, X-ray film, digital media, and given to the patient. The images and the specialist’s opinion are also included in the medical history.
The patient will learn about the results within 1-2 hours. In an individual interview, the radiologist can conduct a consultation, point out the pathologies found, special points, tell you what you need to pay attention to and which specialist to turn to for help. After the images are examined, the radiologist interprets the result, draws up a conclusion, and presents it to the attending physician.
If the patient requires additional research, the reason for it is explained directly by the attending physician.
Magnetic resonance imaging of the paranasal sinuses - how to do it
With the introduction of a contrast agent, the study takes much longer than without it. Also, the specialist must be qualified in the administration and diagnosis of its use. When the patient is stationary in the tomograph cylinder, the device takes pictures of the paranasal sinuses from different angles in several projections. The examination lasts 15-20 minutes; if a contrast agent was used, the examination time is 30-50 minutes. The device produces noise and hum while diagnosing a patient. Before the study, it is necessary to have a conversation and talk about the unpleasant sound. If necessary, you can offer the patient sedatives and secure the limbs with straps built into the device. During the MRI process, the patient is alone in the room. A medical worker monitors his condition and the quality of the images from an adjacent room.
The frontal and maxillary sinuses are located superficially, so for diseases of frontal sinusitis and sinusitis, an MRI appointment will be an unnecessary luxury. The best research option would be the least expensive x-ray of the paranasal sinuses. However, only MRI can reveal the cause and type. The sinuses of the ethmoid labyrinth and the canals of the sphenoid bone are located deeper and are more complex, because of this it is possible to identify changes using layer-by-layer research methods - CT and MRI. An experienced otolaryngologist prescribes a current sinus examination based on the nature of the disease. By contacting a good specialist, you will save not only money, but also your precious health. During a magnetic resonance imaging study, you can view the mucous membranes of the nose. It is also good to diagnose nasal polyps and the labyrinth of the sphenoid void. The test helps specialists distinguish which bacteria are causing the disease and rule out sinusitis caused by fungi. What does MRI of the paranasal sinuses show? Interpretation of the results The photographs clearly show the existing pathologies, inflammatory processes or neoplasms in the paranasal sinuses. In the process of magnetic resonance therapy it is possible to diagnose:
- Nasal bone disease
- Inflammatory process in the paranasal sinuses (sinusitis, frontal sinusitis, sphenoiditis, ethmoiditis)
- Formed cysts or polyps
- Chronic diseases
- Incorrect structure after injury
Upon completion of magnetic resonance imaging, the images are interpreted by a radiologist, who confirms or refutes the diagnosis of the attending physician. The patient is given a conclusion, photographs and a disk (which can be viewed on a home PC).
The description of the conclusion is about 20 minutes. MRI of the sinuses during pregnancy MRI in the 1st trimester is prohibited. During a magnetic resonance imaging study, a pregnant woman's body is exposed to a strong magnetic field. It is strictly not recommended to perform diagnostics in the first trimester. The fruit begins to form during this period. From the second trimester, doctors also do not recommend MRI, but in special cases it is still allowed and only as prescribed by the attending physician. Under the influence of noise and heat emitted from the device, the woman will experience anxiety, which will adversely affect the child. If possible, it is better to postpone the diagnosis before the birth of the child and before the mother feeds him with breast milk. Research during lactation is also prohibited.
Interpretation of MRI of the abdominal cavity
MRI of the abdominal cavity allows you to assess the condition of the internal organs, determine the distribution and nature of the disease process. At the same time, it is possible to accurately establish a diagnosis and begin treatment in a timely manner, preventing the development of any complications. MRI allows you to monitor the size of tumors in oncology. Identify metastases and new lesions in a timely manner, and draw up a plan for surgical intervention.
MRI interpretation is the most important factor on which the accuracy of the diagnosis depends. This process is quite complex, and how an MRI of the abdominal cavity is deciphered is known exactly to a specialist who has deep medical knowledge of human anatomy and the characteristics of the disease. The radiologist usually has experience in interpreting ultrasound and X-ray machines, and also undergoes special training courses.
If controversial, difficult cases arise during decoding, several interpretations of the images are used. Currently, other specialists can be involved remotely. Exists . Large medical portals on the Internet attract leading specialists from all over Russia, as well as from abroad. The importance of such a project is obvious, especially for small cities, where the shortage of specialists is very noticeable.
Is a stroke visible on an MRI?
Stroke is always visible on MRI, and according to the recommendations of the World Health Organization (WHO), the World Association of Neurologists (WAN) is the “Gold Standard” in identifying any type of stroke. The radiologist, after receiving the data on his personal computer, evaluates the anatomical changes of the brain. Since the data from the first study is saved to disk and printed on film, the attending neurologist after treatment can evaluate the prescribed therapy and raise the question of correcting drug treatment, which is very important for the patient’s future quality of life. In a patient even with sparse neurological symptoms, lesions are detected on classical MRI sequences.
Hemorrhagic stroke MRI
Hemorrhagic stroke occurs in 15% of all strokes. Hemorrhagic stroke is an acute cerebrovascular accident (CVA), and as a result, the release of blood from a cerebral vessel into the brain substance. This pathological condition is possible in the following cases: when a person has high blood pressure and the brain vessel cannot withstand it, its wall ruptures. “sweating” of the vascular wall with cellular elements of the blood is less common. Types of hemorrhagic stroke.
- parenchymal hemorrhage (blood in brain tissue).
- subarachnoid hemorrhage (blood in the pia mater).
- subdural hemorrhage (cause: trauma. Blood in the subdural space).
- epidural hemorrhage (cause: trauma. Blood in the epidural space).
Since the main substrate of pathology is blood that has left the normal course, then with MRI, depending on the “age” of the blood, we will see characteristic changes. Blood leaves its usual channel into the brain tissue. Hemorrhagic stroke: increased signal on T2 sequence in the left hemisphere.
Stroke on MRI
On MRI after a stroke in the acute period (1-7 days after the development of stroke symptoms), pathological foci are clearly identified and delimited from normal brain tissue. On the T1 sequence, the ischemic zone appears as a hypointense signal, and on T2, on the contrary, a hyperintense signal. Edema around this lesion and mass effect (displacement of the brain towards the normal brain) are also visualized. On MRI in the subacute period (7-21 days after the development of stroke symptoms). Resolution of edema (reduction in size), the infarction zone still appears as a hypointense signal, and on T2, on the contrary, a hyperintense signal. On MRI in the chronic period (more than 21 days after the development of stroke symptoms). Swelling is completely resolved. The infarction zone still appears as a hypointense signal, and on T2, on the contrary, a hyperintense signal. Expansion of the cortical grooves of the brain, expansion of the lateral ventricles.
MRI signs of stroke
Diffusion-weighted image: infarction in the left middle cerebral artery, stroke in the right middle cerebral artery. The hyperintense signal in this case indicates the most acute period of the stroke. Stroke in the left hemosphere of the pons. A clear delineation of normal brain tissue from the affected brain tissue is visualized along the midline. Ischemic stroke MRI - there are five main periods of completed ischemic stroke:
- Early recovery;
- Late recovery;
- Remote.
In ischemic stroke, MRI shows, respectively, the ischemic zone, that is, a deficiency of blood supply in a certain localization of the brain in the early period and in the late period - necrosis of part of the brain (zone of cerebral infarction). In addition to these pathological changes on MRI, it is possible to establish the cause of the hemorrhage, namely: if it is an atherothrombotic ischemic stroke, MRI images of the brain visualize a blood clot, a narrowing of the lumen of a brain vessel with cholesterol plaques. MRI and lacunar stroke Lacunar stroke is a type of ischemic stroke of the brain, characterized by limited small foci of the brain (up to 2.0 cm), which formed as a result of blockage of one of the small arteries of the brain and resolved over time into a cyst (lacuna).
Signs that are detected on MRI:
- Unilateral pontine infarction has a sharp midline demarcation.
- Increased intensity or density at the end of the acute or at the beginning of the subacute stage
- Small, discrete, low-density/diffusely limited lesions 3-20 mm in diameter, usually 10 mm in diameter
- The signal from the lesion is more intense compared to the signal from the cerebral fluid.
MRI for stroke - what will show, why
Stroke is a pathological condition characterized by acute cerebrovascular accident (ACVA), which is manifested by the appearance of focal or cerebral symptoms that persist in the patient for more than 24 hours or lead to the death of the patient. MRI for stroke “shows” the ischemic zone (in ischemic stroke), lacuna (cyst in lacunar infarction) or blood saturation of brain tissue (in hemorrhagic stroke). What the MRI shows is important for choosing the right treatment. The earlier adequate correct therapy for stroke is started, the higher the patient’s quality of life in the future. MRI of the brain, stroke When a stroke occurs, irreversible changes occur, which can always be diagnosed after performing an MRI. MRI is able to recognize any stroke, clarify the cause of its occurrence, its age, and is able to identify which parts of the brain are affected. All this further contributes to the appointment of correct treatment. MRI, as noted earlier, always shows a stroke. This statement is confirmed from the standpoint of evidence-based medicine. MRI examination is recommended by both the World Health Organization and the World Association of Neurologists. Since the development of medical physics does not stand still, such phenomena as diffusion and perfusion are also applicable to MRI. It is with the help of diffusion-weighted imaging (MRI scanning mode) that changes in the brain are detected minutes after the onset of stroke symptoms.
Differences between MRI and CT
How MRI and CT are interpreted and how these types of examination differ.
CT (computed tomography) - this examination is carried out using x-rays. Unlike a conventional X-ray examination, where a two-dimensional image is displayed on a plate or film, with computed tomography the image appears in three-dimensional form. The fact is that the device is designed in such a way that a person is inside the device in a ring-shaped circuit. Pictures of organs are taken from different angles, from different points, the images are processed and a three-dimensional picture is obtained.
The principle of obtaining images on MRI (magnetic resonance imaging) is the same. The difference is in the nature of the waves. MRI uses electromagnetic waves.
The main differences between X-ray examinations are also that each method in its own way is better at identifying a particular pathology.
A little history
The year 1973, in which Paul Lauterbur, a professor of chemistry, published his article on the creation of images based on magnetic resonance in the scientific journal Nature, is unanimously accepted by everyone as the founding of the method. A little later, Peter Mansfield, a British physicist, improved the mathematical components of image creation. Both scientists received the Nobel Prize in 2003 for their contributions to the development of magnetic resonance imaging.
A significant breakthrough in the development of the method occurred with the invention of the MRI scanner by the American scientist and physician Raymond Damadian, one of the first researchers of the capabilities of MRI. According to numerous sources, the scientist is the creator of the method itself, since back in 1971 he published the idea of detecting cancer using MRI. There is also information about submitting an application to the Committee of Inventions and Discoveries from the Soviet inventor V.A. Ivanov. on this topic, described in detail already in 2000.
Answers to common questions
We will answer questions that patients often ask before undergoing an MRI:
- Is it possible to eat something before an MRI? If the procedure is not carried out to study the condition of the gastrointestinal tract, then the patient does not need to limit himself in food. Otherwise, you should not eat for 6-8 hours before your MRI procedure.
- What foods can you eat before an MRI? If a patient is prescribed an MRI of the gastrointestinal tract, then for two days it is necessary to follow a diet and exclude from the diet foods that lead to increased gas formation (eggs, legumes, cabbage and other vegetables with a high fiber content).
- Can a patient drink alcohol before an MRI? No, the last drink of alcohol is permissible no later than 2-3 days before the test. Alcoholic drinks negatively affect the condition of blood vessels. If an MRI is performed soon after drinking alcohol, the diagnosis will give unreliable results.
- Can I drink water before an MRI? The patient should not limit himself to drinking if the study does not concern the gastrointestinal tract. Otherwise, you should abstain from water for 3-4 hours before the MRI.
- Do I need to undress for an MRI examination? Typically, the patient undresses and is given a hospital gown or gown. You can leave underwear (women's bras cannot be left if they have metal wires or hooks). If the patient's clothing is loose and without metal fittings, doctors may allow an MRI to be performed in it. But first you need to remove all items from your pockets.
- Is it possible to do an MRI if you have a runny nose or a cold? It all depends on the severity of the symptoms. Usually colds and runny nose are associated with inflammatory processes. They may distort the results of the study. Therefore, it is better to be healthy for diagnosis. But this only applies to MRI of the brain and temporomandibular joints. When scanning other human organs and tissues, a cold is not a contraindication.
- How long does an MRI take? Typically the study lasts 20-30 minutes. The procedure will be delayed if the patient is given a contrast agent or sedative. Then the MRI will last about 60 minutes. The maximum duration (with MRI of the whole body) is 2 hours.
- At what age do children have an MRI? Magnetic resonance imaging is safe even for the fetus in the womb. Therefore, tomography can be done on babies of any age, including newborns and premature babies. The only caveat is that children are put under anesthesia before the study so that they remain motionless. The procedure without anesthesia is performed for children over 7 years old.
MRI has great value in medicine. The results of such a study will be useful for phlebologists, cardiologists, oncologists, surgeons, traumatologists and other specialists. Thanks to them, it is possible not only to make a correct diagnosis, but also to accurately identify the localization of the pathological process. All this will help prescribe early and effective treatment, as well as shorten the rehabilitation period.
How to prepare for a tomography mentally and physically
Here's what you need to take with you when going for an MRI diagnostic:
- Referral from the attending physician (possible without it if the patient himself initiates the examination);
- Results of previously performed diagnostic procedures such as ultrasound, CT, MRI;
- Medical history (a copy is possible), outpatient card, extracts and expert opinions;
- Documents confirming the right to preferential research (if any);
- VHI policy (additional medical insurance), if the clinic’s services are paid for by the insurer.
Typically, no preparation is required for an MRI examination. The patient simply has to come to the diagnostic room at the appointed time. Before the procedure, it is enough to remove everything that contains metal and is sensitive to the magnetic field:
- Keys;
- Wallet;
- Mobile phone;
- Bank cards;
- Jewelry (earrings, rings, hairpins, chains, piercings);
- Clothes with metal fittings.
If you have metal structures that cannot be removed, be sure to notify your doctor. We are talking about metal and metal-ceramic crowns, implants, wires, pacemakers and other medical devices.
Preparation is only required when an MRI of the gastrointestinal tract is prescribed. It is important that the stomach and intestines are empty and their muscles are relaxed. That's why:
- You can eat before an MRI no later than 6-8 hours before the procedure (if the diagnosis is scheduled for the morning, then the last meal is in the evening).
- You can drink no later than 3-4 hours before the MRI examination.
- To prevent bloating, drink activated charcoal at the rate of 1 tablet for every 10 kg of body weight.
30-40 minutes before the MRI, it is advisable to take an antispasmodic drug to prevent smooth muscle spasms. Suitable drugs: No-shpa, Drotaverine, Spasmonet-Forte, Spasmol.
What pathologies does MRI reveal?
The range of diagnosed diseases in the case of MRI is wide. An abbreviated list of pathologies:
- diseases of an inflammatory nature (diseases of the genitourinary system);
- pathological phenomena in the brain and spinal cord (diseases of the pituitary gland, spine, damage to the nervous system);
- benign and malignant tumors (in the brain, liver, respiratory organs, mammary glands, etc.);
- cardiovascular pathologies (vascular pathological processes, heart defects);
- lesions of a traumatic nature;
- infections of joints and bone tissue (osteochondrosis, etc.).
When is an MRI indicated?
The MRI procedure is indicated under the following circumstances:
- if necessary, assess the condition of individual organs or parts of the human body (brain, jaw rows, maxillary sinuses, heart and blood vessels, pelvic organs, etc.);
- to monitor the development of malignant neoplasms, determine the presence of metastases in other anatomical units;
- in order to exclude/confirm recurrent pathology after surgical treatment of the tumor.
Scan Modes
The following types of MRI studies are distinguished:
- Diffusion-weighted tomography. This is an MRI technique that allows you to study the movement of water molecules in human cells and tissues. It is based on recording the speed of movement of protons of hydrogen atoms, which were tagged with radio pulses. Thanks to it, doctors judge the state of cell membranes and intercellular space. Diffusion-weighted MRI is used to diagnose ischemic strokes and cancer.
- Magnetic resonance perfusion. MRI in perfusion mode determines the amount of blood distilled through individual organs. The study reveals the speed and volume of blood flow, and also evaluates the degree of venous outflow and the permeability of the vascular walls. This MRI method helps distinguish between healthy and diseased tissue.
- MR spectroscopy. This is a type of research that determines the biochemical changes in tissue that occur as a result of diseases. Any pathology leads to metabolic disorders, and certain metabolites accumulate in the affected organs. Using MRI in spectroscopy mode, their concentration is detected, which increases even before the onset of clinical symptoms. The method is valued because it helps diagnose diseases in the early stages, when their treatment is most effective.
- Tomographic angiography. The method visualizes the lumen of blood vessels, which differentiate from other tissues thanks to the blood flow: its labeled protons move, unlike other, stationary cells. MRI angiography reveals anatomical and functional pathologies of the circulatory system.
- Functional MRI. This method examines the brain, identifying the individual structure for an individual patient. It is based on the flow of blood to the zone that is currently most active. The patient is asked to perform various tasks, and the computer records areas of increased activity.
- MRI of the spine with axial load. The method appeared recently, and in Russia there is only one clinic offering diagnostics in this mode. It consists of scanning the lumbosacral area of the spinal column, first in normal mode, and then dynamically (with load). To do this, the tomograph table and its magnets are moved to a vertical position together with the patient. When exposed to gravity, pathological structures of the spine are better identified.
- MR thermometry. It allows you to record the temperature of various tissues and organs inside a person by changing the frequency of radio waves depending on the degree of heating of parts of the body. This MRI method is necessary to assess the effectiveness of procedures involving local heating of tissues in cancer.
The result of an MRI study is high-quality images. But sometimes this is not enough to make a diagnosis. Then a contrast-enhanced tomography is prescribed: the patient is injected with a drug containing gadolinium, a metal that responds well to radiofrequency waves inside the tomograph. It spreads throughout the body within 1-2 minutes and makes it possible to obtain a clearer image of the area under study, revealing even minor pathologies in the structures of organs and tissues.