Let's consider what is the current norm of cholesterol in men by age, what is it associated with, why cholesterol levels (CH) need to be regularly monitored, how to properly prepare and pass the necessary tests, how you can normalize hypercholesterolemia, how to prevent it.
The concentration of cholesterol in the blood is a marker of lipid metabolism and at the same time the main indicator of the risk of cardiovascular pathology, which often develops without any symptoms. That is why the age standards presented in the table should become a reference book for every person.
The role of cholesterol for men
The global significance of cholesterol (cholesterol) is that it is used to build the cell membranes of all organs and tissues. That is, without it there would be no basic structure of the human body - the cell.
For men, normal cholesterol levels are especially important, since it is one of the participants in the synthesis of sex and steroid hormones: testosterone, cortisol, which are responsible for sexual function and muscle growth.
Cholesterol is part of bile, concentrated in hepatocytes, erythrocytes, neurons and has a direct effect on the balance of vitamin D, supporting immunity, stimulating the synthesis of sphingomyelin - the basis of nerve fibers.
There are two types of cholesterol: high and low density. HDL (HDL) – high-density lipoproteins: good or useful because it utilizes excess lipids, transporting them to the liver. LDL (LDL) – low-density lipoproteins: bad or harmful, as it is the main carrier of endogenous sterol to cells, contributing to the development of atherosclerosis.
"Bad" and "good" cholesterol
Cholesterol moves through blood vessels only in tandem with protein, forming with it a special substance - lipoprotein, which moves through the bloodstream. The type of lipoprotein depends on the ratio of protein and fat: low and very low density lipoproteins (harmful to the body) and high density lipoprotein (beneficial), total cholesterol.
Peculiarities:
- HDL (high density) contains protein, phospholipids and triglycerides. Participates in cleansing the circulatory system of harmful cholesterol and prevents the formation of cholesterol deposits.
- LDL (low density) can cause atherosclerosis if the permissible values are exceeded. Blockage of the vascular system is the cause of ischemia, heart attacks and strokes, and dementia.
- VLDL (very low density), a variant of “bad” cholesterol. Exceeding the permitted values in the blood threatens the formation of plaques and the development of atherosclerosis.
Total cholesterol reflects a person's health status. A blood test determines not only the total cholesterol value, but also examines the indicators of all types of lipoproteins.
Using a special formula, the average coefficient is calculated, which indicates the ratio of “harmful” and “good” cholesterol in the body.
The body needs all types of lipoproteins, but quantitative indicators should not exceed reference values. All lipoproteins are involved in vital processes in the body: a small or increased number of lipoproteins indicates disorders occurring in the body.
Cholesterol levels in men: table according to age
The value of the lipid marker is determined using biochemistry. Cholesterol, the norm of which in men changes with age, is most conveniently compared with the results of the analysis in the table.
| Total cholesterol (TC) | LDL (mmol/l) | HDL (mmol/l) |
| Age 20-30 | ||
| 3,44-6,32 | 1,81-4,27 | 0,80-1,63 |
| Age 30-40 | ||
| 3,78-6,99 | 2.10-4,90 | 0,75-1,60 |
| Age 40-50 | ||
| 4,09-7,15 | 2,51-5,23 | 0,78-1,66 |
| Age 50-60 | ||
| 4.04-7,15 | 2,28-5,26 | 0,72-1,84 |
| Age 60-70 | ||
| 4,09-7,10 | 2,54-5.44 | 0,78-1,94 |
| Age >70 | ||
| 3,73-6,86 | 2,49-5,34 | 0,80-1,94 |
The male body constantly undergoes hormonal changes; this is the basis for the need for regular cholesterol tests after 30 years. From this age, the risk of cardiovascular pathology increases. It is better to carry out such control annually, but before 50 - this can be done once/10 years, after 50 - once/five years at least.
Let us consider in more detail the age-related characteristics of fat metabolism indicators and the reasons for their changes.
Age 30-40 years
After 30 years, men show a tendency to hypercholesterolemia (the level is higher than normal), the regenerative capabilities of the body decrease, which forces patients to regularly monitor blood sugar levels, blood pressure, and take tests that test the lipid profile.
Harmful cholesterol injures the vascular wall, so when taking tests, be sure to check TC and LDL, which destroys blood vessels, disrupting blood flow. The process is aggravated by physical inactivity and bad habits.
The norm of blood cholesterol in men after 30 and up to 40 years of age is as follows: TC in the reference (average) value - from 3.57 to 6.58 units, LDL cholesterol - from 2.02 to 4.79 units, HDL - from 0.72 up to 1.60. Determining bad cholesterol allows you to assess the risk of cardiovascular pathology and atherosclerosis.
Age 40-50 years
A period of hormonal changes in the body, testosterone synthesis decreases, the layer of subcutaneous fat thickens, and when a number of negative lifestyle aspects are combined, diabetes mellitus or obesity can occur, which plays a key role in vascular damage.
The norm of blood cholesterol in men after 40 years to 50 in reference values: TC - from 3.91 to 7.15, LDL - from 2.25 to 5.23, HDL - from 0.70 to 1.73.
Age 50-60 years
The risk of developing pathology of the heart and blood vessels doubles; it is necessary to give up bad habits, lead an active lifestyle, and monitor your diet.
The reference norm of cholesterol in the blood in men from 50 to 60 years of age: TC - from 4.09 to 7.17 units, LDL - from 2.28 to 5.26, HDL - from 0.72 to 1.84.
The effect of sport on cholesterol levels
Elevated cholesterol, together with a passive lifestyle and the presence of bad habits, threatens the development of complex life-threatening diseases. Sports activities are recommended for people suffering from atherosclerosis. Any physical activity aimed at improving the health of the body has a positive effect on cholesterol levels.
Morning exercise can be the first step towards health. An important rule is a sense of proportion: you should not abuse increased loads ; vessels weakened by the disease may not be able to cope at a high pace. Physical activity should increase evenly, without jumps, so that the body can adapt to a new way of life.
Physical activity should not cause a deterioration in general condition. Dizziness, shortness of breath, and irregular heart rhythm indicate that the load is chosen incorrectly and requires adjustment.
Regular exercise will lead to a reduction in adipose tissue, strengthen the heart muscle, and free blood vessels from cholesterol deposits. Age-related blood cholesterol levels in men and women will be stable if they adhere to the principles of proper nutrition and an active lifestyle, and if there is a genetic predisposition, a lipid profile should be taken regularly.
Author of the article: Shamina Anastasia
Article design: Oleg Lozinsky
Why is high cholesterol dangerous?
Bad cholesterol, LDL, has a frankly negative effect on blood vessels. The molecules of this fat stick together and damage the vascular endothelium. A defect in the vascular wall becomes the site of formation of an atherosclerotic plaque with subsequent stenosis of the lumen of the capillaries. As a result, there is a risk of serious complications:
- IHD – coronary heart disease, angina pectoris, arrhythmia, pre-infarction condition, infarction, myopathy, cardiosclerosis, heart failure of varying severity, thromboembolism, hypertension;
- atherosclerosis with damage to cerebral vessels, encephalopathies, strokes of various origins, migraines, memory loss, dementia;
- obliterating endarteritis, varicose veins of the lower extremities, convulsions, trophic ulcers, gangrene;
- endocrine pathologies;
- fatty liver;
- renal failure;
- violation of sexual and reproductive function.
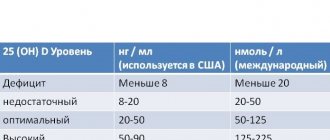
No less dangerous are changes in cholesterol that occur latently. Deviations from the norm lead to loss of elasticity of blood vessels, wear and tear of all organs, tissues, and systems of the body. The basis is the loss of the ability to synthesize the hormone of happiness - serotonin, with a simultaneous drop in the concentration of vitamin D, which is responsible for calcium metabolism. Clinically, this is manifested by depression, emotional lability, apathy, lack of appetite, muscle weakness, lymphadenitis, and dyspepsia.
Degenerative changes can become irreversible, especially affecting the spine and blood vessels of the lower extremities. Short-term normalization of indicators only worsens the prognosis.
How many should women have?
The normal cholesterol content in women corresponds to that in men – 3.5-6.5 mmol/l and does not depend on age.
At 50
After 50 years, most women experience menopause, which is characterized by a decrease in the content of all sex hormones. This causes cholesterol levels to rise and go beyond normal limits. Therefore, during this period it is important to monitor the values of this substance and correct its level with the help of medications - statins.
At 60 years old
Once a woman passes age 60, her comorbidities often place her at moderate or high risk. These categories of women need constant examination of lipid metabolism, where total cholesterol of 4 mmol/l is acceptable. Diet recommendations for women.
Causes and signs of cholesterolemia
The balance between harmful and beneficial cholesterol depends on the men themselves, that is, the level of normal cholesterol is the work of a person and his habits. The reasons for the imbalance are:
- heredity;
- age with the decline of metabolic processes and endocrine background;
- nicotine, alcohol, coffee addiction, drugs that directly affect lipid metabolism;
- overeating, obesity, unbalanced diet;
- stress;
- physical inactivity;
- concomitant somatic pathologies: diabetes mellitus, hypothyroidism, cardiovascular diseases, liver and kidney dysfunctions;
- inflammation (including tuberculosis, sexually transmitted infections, helminthic infestation), tumors;
- taking medications: beta blockers, diuretics, hormones, anticoagulants.
Hypercholesterolemia does not announce itself in any way, therefore, until fat deposits close the lumen of the vessel almost completely, it is difficult for an ordinary person to suspect deviations from the norm. However, there are a number of external signs that suggest high cholesterol:
- discomfort in the legs: heaviness, burning sensation, change in skin color;
- dyspnea;
- tachycardia, chest discomfort;
- hot temper;
- weakness combined with sweating, fatigue;
- blood pressure surges;
- headache;
- insomnia;
- xanthomas - fatty compactions at the folds or xanthelasmas - in the periorbital area.
Another specific sign may be gray hair, since it is the result of impaired blood flow in the capillaries. In addition to visually obvious signs of deviation of cholesterol levels from the norm, there are also those that can only be diagnosed by a doctor:
- lipoid arch - deposits of cholesterol on the eyelids, invisible to the naked eye;
- rupture of blood vessels;
- tumor;
- heart or kidney failure;
- obesity, diabetes, thyroid disease.
To confirm the identified pathologies, laboratory tests are necessary. They will also help prevent the development of diseases at an early stage or adjust their treatment. They can be submitted to the laboratory of any medical organization. If the analysis is carried out under a compulsory medical insurance policy, a referral from the attending physician is required.
Reasons for changes in cholesterol levels
Among the most common causes of high cholesterol in men:
- Burdened heredity. If the family has relatives diagnosed with coronary artery disease, atherosclerosis, who have suffered a stroke or heart attack, the risk of hypercholesterolemia increases;
- Physical inactivity. Physical activity burns “bad” cholesterol and improves metabolism;
- Systematic overeating, obesity, unbalanced diet;
- Constant stress, bad habits. A passive smoker is also automatically at risk;
- Diseases of the endocrine system;
- Hypertension;
- Kidney and liver failure;
- Oncology;
- Taking certain medications (diuretics, hormonal steroids);
- Age - the norm of cholesterol in the blood of men after 40 years is lower, and after 50 the cholesterol content stabilizes.
Very low cholesterol levels also do not promise anything good. At any age, the causes of very low cholesterol can be:
- A strict diet with insufficient amounts of animal proteins;
- Anemia;
- Consequences of infectious diseases;
- Tuberculosis;
- Hyperthyroidism of the thyroid gland;
- Liver pathologies;
- Blood diseases.
These are just some of the factors that influence changes in blood cholesterol levels; a biochemical analysis will help men identify the cause of deviations from the norm. If violations are detected, you must undergo an annual examination and follow the recommendations of specialists.
Preparing for analysis, common mistakes
To avoid mistakes when taking an analysis, which will reliably distinguish normal from pathology, patients should adhere to the preparation rules:
- The collection of biomaterial is carried out on an empty stomach, in the morning: the last meal should be 12 hours before the start of the study;
- a few days before the analysis, remove all fatty and fried foods from the diet, give up cigarettes and alcohol;
- a couple of days before biochemical testing, they stop taking all dietary supplements, and inform the laboratory assistant about the medications prescribed by the doctor (this is necessary to correct the results with the doses of the medications.) They distort the cholesterol level: antibiotics, statins, diuretics, hormones, vitamins.
Before the biochemical analysis, the patient donates blood for general testing, and only if the cholesterol level is above 5.2, a lipid profile is prescribed. Blood is taken from a vein, the procedure takes a few minutes, the results are ready after a few hours, and can be collected the next day. It is a big mistake to get tested for a cold, acute respiratory infection, acute respiratory viral infection, or exacerbation of somatic pathologies, since all this distorts the results obtained.
Usually examined:
- TC – total cholesterol;
- HDL – high density cholesterol;
- LDL – low density lipids;
- triglycerides.
This complex is called a lipid profile. In order to detect pathology in time, it is recommended to undergo tests annually (dispensary examination), and after 50 - twice a year. During the course of therapy - every three months.
At the same time, the following additional methods for studying cholesterol are used:
- titrometry - measure volumetric indicators;
- gravimetry – measure the mass of cholesterol;
- nephelometry – record the luminous flux in an opaque medium;
- chromatography – visualize the movement of particles in media.
It is impossible not to mention the express method for determining blood cholesterol. It is performed similarly to testing blood for sugar using test strips. You need to prepare for it according to the same rules.
Cholesterol level analysis: how it is done and what the results say
Testing blood cholesterol levels is a common procedure performed in any medical laboratory. The procedure is a regular blood donation from a vein, but you should prepare for it. The recommendations given by your doctor should be followed carefully.
Recommendations:
- Blood is donated on an empty stomach (12–16 hours must pass since the last meal).
- 3 days before the day of blood donation, exclude fatty and fried foods, alcohol, and nicotine from the diet.
- Consult with your doctor about discontinuing medications 3 days before the test (if they are used as prescribed by a doctor).
- If discontinuation of medications is not possible, then it is necessary to inform the medical professional of the names of the medications.
- The day before blood sampling, you should avoid stress and strong psychological stress.
Methods for determining cholesterol:
- rapid test at home;
- analysis for total cholesterol;
Cholesterol. The norm for men is calculated by age. To determine the amount of cholesterol you need to do a special analysis. - LDL analysis;
- HDL analysis;
- triglycerides;
- lipidogram.
The easiest way is a rapid test. To carry it out, you will need to follow the specified recommendations for preparing for blood donation. Blood is drawn from a finger. The results of the analysis are known instantly.
When conducting tests in the laboratory, blood is drawn from a vein located in the elbow. Results are prepared from several hours to days. The most complete picture of the ratio of lipoproteins is provided by a lipid profile.
If the cholesterol level is exceeded, the doctor, deciphering the lipid profile, determines which risk group the patient falls into, depending on quantitative indicators and age. Experienced doctors using this type of analysis are able to determine the risk of an early heart attack or stroke.
Features of treatment
To bring cholesterol back to normal, you need complex therapy, which includes giving up bad habits, changing your diet, and in some cases taking medications.
Diet
Considered a major hitter, as the most common cause of lipid changes in men is overeating. The diet is safe and effective for all ages, but is especially necessary after 50 years. The basic principles of reducing cholesterol to normal levels were developed by M. I. Pevzner and are the basis of table No. 10:
- exclusion from the daily diet of foods with unhealthy fats (LDL): meat, offal, lard, eggs, milk, margarine, mayonnaise, fast food, spreads, all fried foods;
- the calorie intake of an adult male is reduced to 2,500 kcal/day (or less) with a correlation to energy costs;
- the emphasis is on proper, long-digesting carbohydrates (legumes, cereals, whole grain bread) and fiber (fruits, vegetables, bran);
- OMEGA-3 unsaturated acids are required: seafood, vegetable oils, olives, nuts, avocados.
The volume of polyunsaturated acids should be at least 25% of the total daily diet. If necessary, add dietary supplements: Omacor, Vitrum, Norvesol.
Flavor enhancers, preservatives, thickeners are taboo: chips, soda, crackers, sauces, mayonnaise, yoghurts from packs. Food intake is fractional, in small portions. Instead of any liquid - water, fruit juice, dried fruit compote.
Any deviation of cholesterol from the norm requires a reasonable drinking regime: at least 2.5 liters of water daily. You should not drink during meals, but it is best to drink 20 minutes before meals.
Folk remedies
Ginger and green tea, milk thistle, and artichokes improve lipid metabolism.
- Ginger tea - fresh root (100 g) cut into thin strips, pour cold water (1 tbsp.) and boil for 15-20 minutes. Strain and cool. The drink is drunk warm, adding lemon juice and honey to taste. Ginger tea is drunk 2 times a day: morning and afternoon. This is a tonic drink, so it is not recommended to take it at night.
- Green tea – instead of regular black tea, it is very useful to drink regular green tea, sweeten it with honey.
- Garlic – to reduce cholesterol, it is recommended to eat 2-3 cloves of garlic every day for one month.
- Milk thistle herb – for high cholesterol 1 tbsp. l. dry ingredients are brewed with a glass of boiling water. Drink half a glass before breakfast and lunch.
- Artichokes – for the purpose of prevention, artichokes can be introduced into the daily diet as an independent dish or added to salads and side dishes. To reduce cholesterol, prepare a decoction from the leaves of the plant. To do this, pour 25 g of chopped artichokes into 500 ml of boiling water, place in a water bath and steam for another 15 minutes. Cool, filter and drink (but not more than 5 times a day) a quarter glass half an hour before meals.
Often cholesterol levels above normal are diagnosed in easily excitable patients, so they are recommended soothing teas based on:
- chamomile;
- motherwort;
- valerian;
- mint;
- lemon balm.
If diet and sedative herbs do not normalize the situation, medications are prescribed. More details: list of sedatives.
Medications
There are several groups of lipid-lowering drugs:
- statins normalize cholesterol by blocking the enzymes responsible for the synthesis of LDL: Liprimar, Crestor, Atorvastatin, Simgal, Lipostat, Rosuvastatin, Torvacard (they have many contraindications and are prescribed only by a doctor);
- fibrates – stabilizes the level of fats and uric acid, used only if the TC indicator is more than 7.4 units: Fenofibrate, Clofibrate, Ciprofibrate;
- ion exchange resins – bind bad cholesterol and remove it from the body. They are taken with food, in fact they are sorbents: Levatit, Amberlight, Purolite;
- acetylsalicylic acid preparations reduce blood viscosity, preventing thrombosis, the formation of cholesterol plaques, strokes, heart attacks: Aspirin, Cardiomagnyl, ASA;
- Dietary supplements - prescribed when other medications are contraindicated, correcting lipid metabolism: Chitosan, Taurine, Lecithin.
List of permitted and prohibited food products
If the norm of cholesterol in men is exceeded, it is necessary to review the diet, removing from it:
- fatty meat, lard;
- fast food;
- offal;
- high fat dairy products;
- processed meat products (sausages, smoked meats, stews);
- confectionery, baked goods;
- alcohol, store-bought lemonade, strong tea and coffee.
Recommended Products:
- vegetables, herbs, fruits;
- cereals, legumes;
- sea fish;
- vegetable oil;
- mushrooms;
- low-fat milk and yoghurts.
The importance of cholesterol for the body
Cholesterol refers to organic compounds that are found in cell membranes and dissolve in fats. Almost 75% of cholesterol is produced by the body itself (liver, kidneys, adrenal glands), the rest comes from food.
There are two types of cholesterol - good and bad. When free cholesterol enters the body through food, it must change and transform into a bound form in order to enter the bloodstream. There are signaling proteins on the surface of the cholesterol capsule. The liver cells recognize this protein and change the properties of cholesterol. This is the so-called good cholesterol, it is called high-density lipoprotein. Capsules without such proteins contain “bad” cholesterol that enters the blood vessels in free form. It is called low-density lipoprotein.
For normal life, a person needs both types of lipoproteins. The good ones are involved in the structure of cells and maintenance of functionality. Bad ones are necessary for the bone marrow, kidneys, and nervous system to function normally.
Until recently, it was believed that LDL was the main culprit in atherosclerosis, as it was deposited on the walls of blood vessels, forming plaques. Today this view is being questioned. The only danger is those plaques that have hardened under the influence of calcium. This occurs due to a lack of proteins necessary for vascular regeneration. This explains the presence of plaques in the blood vessels of people who do not eat protein foods. People with normal cholesterol levels are also susceptible to heart disease.
Article on the topic:
Normal values of ESR in a blood test in men
Thus, the main functions of lipoproteins in the body are distinguished:
- Normalization of metabolism.
- Helps in the synthesis of testosterone, cortisol, estrogen.
- Ensuring the functioning of the kidneys, spleen, bone marrow.
- Participation in the production of vitamin D.