When receiving the results of a blood test, the MID is increased - what does this mean for the patient? First of all, this means that there are pathological processes in the body that affect the fluctuation of the normal level of this indicator. MID, which is also called MXD, is an analysis for a specific complex of leukocytes, i.e. cells responsible for maintaining immunity and resistance to external factors. That is why an increase in its level means that the body is struggling with certain pathological phenomena.
Position of MID in blood OCA
Formed elements are cells of biological fluid (blood). Each group of elements performs certain functions that ensure the full functioning of the body. With the development of pathological processes, the qualitative and quantitative composition of the blood changes, which is reflected in the analysis and allows one to make (assume) a diagnosis.
| Blood cells | Red blood cells | Platelets | Leukocytes |
| Functional responsibilities | Transfer of oxygen from the lungs, and transport of dioxide in the opposite direction | Ensuring coagulation (blood clotting process) | Protecting the body from invasion of foreign antigens (bacteria, viruses, parasites, allergens, etc.) |
Since leukocytes (white cells) play the role of guards of the body, their number increases when danger arises. The threat is posed by foreign agents that provoke inflammatory and allergic processes. The overall rate of leukocytes increases due to the mobilization of individual species that are responsible for the elimination of certain agents. In medicine, the process of capturing and eradicating (destructing) pathogens is called phagocytosis, which is why all leukocytes are phagocytes.
As part of the leukogram, the MID (total number of monocytes, eosinophils, basophils) can be determined or each element can be deciphered separately. The types of colorless cells and their responsibilities are discussed below. Agranulocytes (non-granular formed elements):
- lymphocytes – responsible for humoral immunity (immune response to invasion of viruses, allergens, bacterial microorganisms and activation of cancer cells)
- monocytes - provide phagocytosis of foreign substances in the peripheral blood.
Granulocytes (granular cells):
- neutrophils – capture and eliminate bacterial pathogenic microorganisms;
- eosinophils - fight parasitic infestations;
- basophils - are in correlation with immunoglobulin E, release histamine to eliminate allergic manifestations.
All colorless formed elements of blood are in a correlation relationship.
Eosinophils
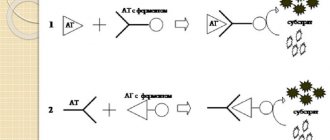
Eosinophils are cells produced by the bone marrow. When an infection enters the body, the immune system produces antibodies. Complex complexes are formed from antigens of microorganisms and cells that fight foreign proteins. Eosinophils neutralize these accumulations and cleanse the blood.
The normal percentage of eosinophils in the leukocyte formula is from 1 to 5%. If these indicators are exceeded, then doctors talk about eosinophilia. This may indicate the following diseases:
- helminthic infestation;
- allergy;
- malaria;
- bronchial asthma;
- skin diseases of non-allergic origin (pemphigus, epidermolysis bullosa);
- rheumatic pathologies;
- myocardial infarction;
- blood diseases;
- malignant tumors;
- pneumonia;
- lack of immunoglobulins;
- cirrhosis of the liver.
In addition, eosinophilia can be triggered by taking medications: antibiotics, sulfonamides, hormones, nootropics. The reasons for such a deviation in the blood test for leukocyte formula can be varied. Additional examinations are required to clarify the diagnosis.
If eosinophils are reduced, doctors call this condition eosinopenia. This suggests that cell production is suppressed due to the depletion of the body's defenses. The following reasons for the decrease in eosinophils are possible:
- severe infections;
- sepsis;
- appendicitis complicated by peritonitis;
- infectious-toxic shock;
- emotional stress;
- injuries;
- burns;
- operations;
- lack of sleep.
Test results may be affected by recent childbirth, surgery, or medications.
Components of MID
MID in the leukocyte formula combines the smallest types of white blood cells: monocytes, eosinophils, basophils.
Monocytes (MON)
Agranulocytic leukocytes of this type are large in size and have a red-violet nucleus. The cells are formed in the bone marrow and then move into the systemic circulation, where they live on average for about three days. Monocytes then transform into macrophages and move to the tissues of the liver, spleen and lymph nodes.
Macrophages are active phagocytes of the immune system that cleanse the body of cellular debris (dead cells) and bacterial microorganisms. The hallmark of MON is its survival. Neutrophilic granulocytes (neutrophils) are initially programmed to die after meeting foreign agents and performing their function, while monocytes are not destroyed, but continue their security activities.
In addition to phagocytosis, the responsibilities of monocytes include the production of the protective protein interferon, which inhibits the activity of viruses and is involved in building specific immunity, tissue regeneration, participation in the process of hematopoiesis, suppression of the activity of cancer cells, and protection of the body from cancer.
The monocyte variety of white cells copes more effectively with viral agents than with bacteria and parasites. An increased content of monocytes in the blood is defined by the term “monocytosis”. A reduced amount is called monocytopenia.
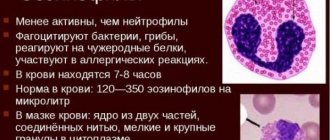
Eosinophils (EOS)
Of all MID representatives, eosinophils remain in the blood for the shortest amount of time. After moving from the bone marrow, they remain in the systemic circulation for several hours and are then transported to the tissues of the digestive system, lungs and epidermis (skin). Eosinophilic leukocytes are intended for the eradication of helminthic infestations through phagocytosis of pathogens, the formation of antiparasitic immunity, and the metabolism of histamine (a bioactive indicator of allergic reactions).
Along with basophils, eosinophil cells take part in the initiation of immediate hypersensitivity (the system's response to the introduction of allergens into the body). Eosinophilia (high concentration of eosinophils), first of all, means the presence of parasites or allergic antigens in the body. Eosinopenia (low cell count) has no particular diagnostic value.
Basophils (BAS)
The smallest, but very important type of granulocyte. The phagocytic properties of the cells are less developed than those of other leukocytes, but their membranes contain receptors for immunoglobulin E (IgE). When allergenic agents enter the body, IgE activates the allergic reaction through the release of histamine.
An increased concentration of basophils in the blood (basophilia) is a clinical sign of the development of allergies. In addition, these colorless cells contain heparin, which maintains stable blood flow in the capillaries and prevents increased blood clotting.
This effect helps maintain optimal blood circulation in small vessels, liver and lungs. Basophils do not have accumulative properties in tissues, like other leukocytes. They move to the inflamed area as needed, eliminate the foreign invasion and die. A decrease in BAS levels is called basopenia.
Lymphocytes and neutrophils
The MID blood test shows the content of monocytes, eosinophils and basophils. However, during a detailed examination, you need to pay attention to other types of leukocyte cells: lymphocytes and neutrophils.
Lymphocytes play a major role in the formation of immunity against infections. Normally their content ranges from 20 to 40%.
Lymphocytosis is observed in serious infectious diseases such as HIV, whooping cough, hepatitis and others. The number of these cells can be increased in case of blood diseases and poisoning with lead, arsenic, and carbon disulfide.
Lymphocytopenia (decreased lymphocytes) can occur with the following diseases:
- immunodeficiency states;
- acute infectious pathologies;
- tuberculosis;
- autoimmune processes;
- anemia.
Neutrophils are divided into band-nuclear (normal 1-6%) and segmented (normal 47-72%). These cells have bactericidal properties; they rush to the site of inflammation and destroy microorganisms.
An increased count of neutrophils is called neutrophilic leukocytosis. This may be due to the following reasons:
- any inflammatory processes;
- malignant diseases of the blood and bone marrow;
- diabetes;
- gestosis and eclampsia;
- the first 24 hours after surgery;
- blood transfusion.
A decrease in the number of neutrophils is observed in the following conditions:
- acute viral infections (measles, rubella, chickenpox, mumps);
- severe bacterial diseases;
- intoxication with chemicals;
- radiation exposure (including radiation therapy);
- anemia;
- high body temperature (from 38.5 degrees);
- taking cytostatics, antidepressants, non-steroidal anti-inflammatory drugs;
- blood diseases.
Reference values
A general blood test determines the amount (absolute indicator) of MID in the composition of all white cells and the percentage value (relative indicator) of the total number of MON, EOS, BAS of the total number of leukocytes. The absolute value is the number of cells per 1 ml of biofluid, otherwise a billion cells per liter. For convenience, a billion is abbreviated as 10 to the 9th power, that is, X * 10^9 / l, where x = the total number of eosinophils, monocytes and basophils.
The value of the relative indicator is measured in percentage (%). Norm X for adults = 0.2–0.8. In percentage equivalent, the reference value is 5–10%. The maximum non-pathological deviation is +5%. There is no gradation of the norm based on gender, that is, the values are identical for men and women. There is a slight discrepancy in the normative indicators of individual components of the MID according to age categories in children.
Preparing for a general blood test
Blood is drawn in the morning on an empty stomach. If the patient is unable to get to the laboratory in the morning, then he must maintain a gap of 4 hours between eating and taking the test.
During the day before the analysis, it is necessary to give up alcohol, fatty foods, and not smoke, as this can increase the actual values in the results. This time must be spent in an emotionally and physically calm state.
Important! If the patient is taking any medications, the doctor must be informed about this.
Depending on the type of analysis in adults, blood is taken from the cubital vein or from a finger. In infants, capillary blood can be collected from the heel.
Norms and deviations of cell analysis
Each group of leukocytes included in the MID has its own laboratory standards. Parameters are measured using absolute (numerical) and relative (percentage) values.
Standard indicators of monocytes
The absolute content of monocytes for adults is 0.09–0.6*10^9/l. A slight excess of the norm is allowed for women in the third trimester of the perinatal period and before childbirth. The children's indicator is 0.05–1.1*10^9/l. The percentage in adults and adolescents (over 15 years old) is from 3 to 11%. In children, the MON range depends on age.
| Age | Up to 1 year | 1-5 years | 5–15 years |
| Norm in % | 4–10 | 3–10 | 3–9 |
Deviation of indicators from the norm in one direction or another indicates the development of infectious viral, oncological or hematological pathologies. Causes of monocytosis characteristic of childhood: acute infection provoked by the Epstein-Barr virus (infectious mononucleosis), specific “childhood” infectious diseases (whooping cough, rubella, measles, mumps).
Infections affecting adults and children: systemic disease of the lung tissue (sarcoidosis), infection with Koch's bacillus (tuberculosis), zoonotic infection transmitted from animals (brucellosis), venereal disease syphilis, typhoid and typhus, helminthic infestations (ascariasis, enterobiasis, opisthorchiasis, teniarinhoz, etc.).
An increase in the number of monocytes in the blood can be a sign of systemic autoimmune diseases (lupus erythematosus, type 1 diabetes mellitus, scleroderma), oncohematological diseases (blood cancer). In rare cases, monocytosis occurs when the body is poisoned with chemicals. Monocytopenia develops in the presence of purulent bacterial infections caused by streptococci and staphylococci. The most dangerous is a generalized lesion of the circulatory system - sepsis.
Eosinophil norms
In adult men and women, the absolute reference values of eosinophils are 0.2–0.4*10^9/l, the relative values are 0.5–5%. Children's indicators (up to 8 years) are graded by age:
The reason for the increased content of eosinophils in children, in comparison with adult norms, is the imperfection of the immune system. Eosinophilia occurs due to:
What do eosinophils show in the blood?
- penetration into the body of helminths (ascaris, pinworms, toxocara, whipworms, bovine tapeworm) and protozoan single-celled parasites (giardia, trichomonas);
- rapidly developing allergic reaction (anaphylactic shock, Quincke's edema, acute allergic rhinitis, etc.);
- lesions of the respiratory system (bronchial asthma, pleurisy);
- relapse of tuberculosis or development of an acute form of the disease;
- diseases of the gastrointestinal tract (eosinophilic gastritis and colitis)
- development of malignant blood pathologies.
Eosinopenia is recorded in purulent-inflammatory processes of a protracted or chronic nature or acute purulent conditions (phlegmonous appendicitis, peritonitis). In addition, a decrease in the level of EOS is associated with the development of a pre-infarction state, pain shock, symptoms of heavy metal intoxication, and distress (constant neuropsychological tension). With progressive blood cancer, the eosinophil count drops to zero.
Reference values for basophils
Normal BAS (BASO) indicators are:
- from 0.01*10^9/l to 0.065*10^9/l – absolute values;
- 1% is a relative value.
The change in standards is provided only for infants up to one year old.
| Newborns | 1 day | 4 days | A week | 2 weeks | 14 days – 1 year |
| 0,75% | 0,25% | 0,4% | 0,5% | 0,5% | up to 0.9% |
Exceeding the norm in women during the ovulation phase of the menstrual cycle does not pose a danger, since it is a physiological feature. In addition, physiological reasons for an increase in BAS concentration include short periods after infectious diseases, X-ray examinations, and taking oral contraceptives.
The pathological causes of basophilia are:
- malignant change in lymphatic tissue (lymphogranulomatosis);
- receiving large doses of ionizing radiation (radiation sickness);
- oncohematology and cancer of other organs;
- the presence of an allergenic antigen in the body (the results of OKA are usually supported by corresponding symptoms: itching, cough, respiratory failure, swelling, rash);
- parasite infestations and infectious diseases of the digestive system;
- disruption of the endocrine system (diabetes, decreased synthesis of thyroid hormones);
- autoimmune pathologies.
In childhood, basophilia most often indicates an allergic reaction of the body. If the results of the OKA reveal basopenia, but there are no pronounced symptoms of changes in well-being, then the reason lies in the patient’s unhealthy eating behavior or unstable psycho-emotional state.
Basophils
If the patient has complaints of allergic reactions, then testing for basophils plays an important role in case of increased MID in the blood test. What it is? Basophils fight allergens that enter the body. This releases histamine, prostaglandins and other substances that cause inflammation.
Normally, the relative amount of basophils in the blood in adults is 0.5-1%, and in children 0.4-0.9%.
An increased content of these cells is called basophilia. This is quite a rare occurrence. It is usually observed in allergic reactions and hematological pathologies such as leukemia and lymphogranulomatosis. Basophils can also be elevated in the following pathologies:
- gastrointestinal diseases;
- diabetes;
- chickenpox;
- early stages of respiratory tumors;
- hypothyroidism;
- iron deficiency;
- taking thyroid hormones, estrogens and corticosteroids.
Sometimes basophils can be slightly elevated in minor chronic inflammations. Slightly increased levels of these cells are observed in women at the beginning of menstruation and during ovulation.
If, with a reduced MID, the decoding of the blood test for basophils shows results less than normal, then this indicates a depletion of the leukocyte supply. The reasons for this analysis result may be different:
- physical and emotional stress;
- increased activity of the thyroid or adrenal glands;
- acute infections;
- exhaustion.
It must be remembered that false test results are possible in women during pregnancy. This is due to an increase in blood volume, which causes the relative number of basophils to decrease.
Results
MID is a combination of indicators of three groups of leukocyte cells: basophils (BAS), eosinophils (EOS) and monocytes (MON), determined during a general clinical analysis of capillary blood. These cells are the smallest in the overall composition of biological fluid, but have important diagnostic value for determining parasitic diseases, allergic reactions, malignant pathologies and infectious processes in the body.
The results of the total amount study (MON+ EOS+BAS) or absolute MID values are 0.2-0.8*10^9/l. Relative values are measured as percentages and amount to 5-10% of the total number of leukocytes. If the MID in the blood test is increased or decreased, it is necessary to thoroughly evaluate and compare all indicators of the leukocyte formula.
The extended leukogram provides separate normative values for all representatives of white blood cells (leukocytes). Unsatisfactory results of the analysis require additional laboratory tests (blood biochemistry, urine analysis, coprogram) and hardware diagnostic procedures (ultrasound, X-ray, MRI, CT, etc.).
How is the test done?
Blood for a general clinical analysis (CCA) is usually taken from a finger, in rare cases it is taken from a vein. An area of skin is treated with a disinfectant solution, a small puncture is made and the material is collected into a test tube. This type of research does not require special preparation. It is advisable to donate blood in the morning on an empty stomach. A general analysis is taken at any clinic. In addition to MID, such an examination reveals other important hematological data: hemoglobin, ESR, red blood cell and platelet counts.
Concept of MID or MXD
MID in meaning and purpose means the same as MXD.
MXD (derived from middle cells) reflects the content of a mixture of the same monocytes, basophils and eosinophils . But because monocytes, basophils and eosinophils are collectively called medium cells, MXD is called MID.
MID is an indicator reflecting the content of a mixture of monocytes, eosinophils, basophils and immature cells.
The MID records the percentage of medium cells, which include monocytes, basophils (partially) and eosinophils, from the total number of leukocytes in the blood (MXD%). The result can also be an absolute number (MID#/MXD#). The MID result is determined using an automatic hematology analyzer. Upon examination, the attending physician establishes the norm or deviation (increased/decreased) amount of one of the types of cells in the indicators.
Sampling process and material examination
For a general blood test, capillary blood is collected in most cases. To do this, the ring finger is pierced with a disposable scarifier and the blood is collected into a sterile tube. This procedure is the same for both children and adults.
The collected material is examined for:
- percentage of leukocytes to total volume;
- content of the leukocyte class, which includes the mid indicator;
- hemoglobin level;
- platelet count;
- hematocrit level;
- erythrocyte component;
- ESR.
After the results are ready and deciphered, the attending physician evaluates the indicators and, if necessary, prescribes treatment.