What is an RBC test?
The RBC test stands for “Red blood cells,” which means “red blood bodies.” It helps determine the number and saturation of red blood cells, which transport oxygen to the heart.
It is mainly prescribed in the following cases:
- To determine and diagnose blood diseases, during which the level of indicators in the blood decreases (iron deficiency anemia, anemia, oncology, and so on).
- During pregnancy, since blood circulation deteriorates, this is associated with intensive development of the fetus (prescribed for the purpose of prevention and preservation of the child).
- During hospitalization and intensive treatment, during which it is necessary to take tests for the production of red blood cells and their oxygen saturation (especially after chemotherapy).
- During the rehabilitation period after endocrine diseases, in which heart function may deteriorate.
A general blood test for red blood cells helps diagnose serious diseases at the development stage. Therefore, hematologists recommend examinations 1-2 times a year for general prevention.
How are red blood cells formed?
In the red brain, a process called erythropoiesis occurs, which forms red blood cells. The bone marrow and its cells differentiate, and due to this we get red blood cells. Stem cells in the bone marrow transform into these bodies in several stages. It goes like this:
- megaloblast formation;
- from it transformation into erythroblast;
- obtaining normocyte from this substance;
- a normocyte forms a reticulocyte;
- from reticulocyte to erythrocyte.
RBC and their functions
There are many main functions that red cells perform in the body:
They carry oxygen to every cell of the body, and take carbon dioxide from the lungs.
- From the gastrointestinal tract, amino acids are transported by red blood cells to all tissues of the human body.
- They take an active part in various chemical reactions. Enzymes are transported in large quantities to each cell.
- Red blood cells protect the body from antigens and toxins by participating in immune processes.
- The acid-base balance is constantly maintained by rbc.
The rate of red blood cells in humans is reduced
The norm for the male half of humanity is 4 million red blood cells/ml; for women, the norm is an order of magnitude lower. They have indicators of 3.5 million/ml. Depending on the age, the children's norm has different ranges.
A low red blood cell count in a blood test indicates the presence of anemia in your body. This may be a consequence of loss of a large amount of blood, deficiency of vitamins B12 and B9, as well as hemolysis.
Increased rate of red cells in the blood
With erythrocytosis and erythremia, rbc levels increase.
When stem cells have a tumor syndrome, primary erythrocytosis develops in the body. Precursor cells begin to divide rapidly. Such processes lead to an increase not only in red blood cells, but also in leukocytes and platelets. When inflammatory processes are present in the body, thrombocytosis and leukocytosis occur.
There are 3 types of secondary erythrocytosis:
- Physiological blood process. If there has been prolonged hypoxia, the red blood cells will be elevated. When the body has lung disease, congenital pathologies and altitude illness.
- Pathological erythrocytosis. The human body contains kidney cancer, cerebellar hemangioma, adrenal tumors, ovarian problems and other serious diseases. This disease can be triggered by drugs that have been used for a long time with a high content of steroids.
- Relative process. The absolute norm is unchanged in relation to the relative indicators of the corpuscles. This occurs with prolonged vomiting, heavy sweating and diarrhea.
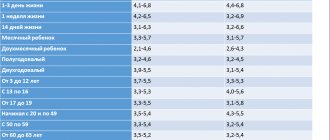
Normal RBC in blood test
RBC blood test is a test that helps determine the level of red blood cells in the blood, which is considered abnormal according to a person's age.
Adults
For women, a value of 4.5-5 liters will be considered the norm; this is influenced by individual sexual development and menstruation. In men, normal levels will be from 5-6 liters, this is due to the active production of testosterone, as a result of which the blood becomes more saturated with oxygen.
In old age, in men and women, levels can decrease to 3.5-4 liters, this is due to the decline of sexual functions as a result of insufficient production of testosterone and progesterone.
Infants
| Age | Normal indicators |
| 1-3 days | 4.5-7 l |
| 3-7 days | 4.5 -6.5 l |
| 2 weeks (14 days) | 3.5-6.1 l |
| 2 weeks -1 month | 3 – 5.5 l |
| 2-11 months | 2.8-4.5 l |
| 11 months-1 year | 3, 1-5 l |
Children
In children from 2 to 12 years old, normal levels are considered to be from 3.5 to 4.5 liters, this is due to physical maturation. From 13 to 18 years, hormones are actively produced and puberty occurs, as a result of which the indicators change from 3.5 to 5.5 liters. Indicators can sharply increase or decrease, this is influenced by the activity of hormone production and the onset of the menstrual cycle in girls.
Mean red blood cell volume MCV
Speaking about red blood cells, one cannot fail to mention such an indicator as the mean erythrocyte volume (MCV). It is measured in cubic micrometers or femtoliters (fl). This indicator can be calculated by dividing the sum of all cell volumes by the number of red blood cells found. It is the average volume of an erythrocyte that makes it possible to evaluate an erythrocyte as a normocyte if the average volume of an erythrocyte is normal (that is, lies within 80-100 fL), but if the average volume of an erythrocyte is reduced - as a microcyte. An erythrocyte is a macrocyte when the average erythrocyte volume is increased. But in general, it should be noted that a reliably average erythrocyte volume can be established only in the absence of erythrocytes with an irregular shape (sickle-shaped erythrocytes).
| Blood from the umbilical cord | 98−118 | 98−118 |
| 1−3 days | 95−121 | 95−121 |
| 1 Week | 88−126 | 88−126 |
| 2 week | 86−124 | 86−124 |
| 1 month | 85−123 | 85−123 |
| 2 months | 77−115 | 77−115 |
| 3−6 months | 77−108 | 77−108 |
| 0.5−2 years | 72−89 | 70−99 |
| 3−6 years | 76−90 | 76−89 |
| 7−12 years | 76−90 | 76−89 |
| 7−12 years | 76−91 | 76−89 |
| 13−19 years old | 80−96 | 79−92 |
| 20−29 years | 82−96 | 81−93 |
| 30−39 years | 81−98 | 80−93 |
| 40−49 years | 80−100 | 81−94 |
| 50−59 years | 82−99 | 82−94 |
| 60−65 years | 80−99 | 81−100 |
| Over 65 years | 80−100 | 78−103 |
Basically, the average red blood cell volume is used to determine the type of anemia.
- Determining the type of anemia
- Microcytic anemia (average erythrocyte volume less than 80 fL): sideroblastic iron deficiency thalassemia, anemia that may be accompanied by macrocytosis: hemoglobinopathies, impaired porphyrin synthesis, lead poisoning;
- Normocytic anemia (average erythrocyte volume in the range of 80−100): aplastic, hemolytic hemoglobinopathies after bleeding, anemia that may be accompanied by normocytosis: regenerative phase of iron deficiency anemia;
- Macrocytic and megaloblastic anemia (average erythrocyte volume more than 100 fl): vitamin B12 deficiency, folic acid deficiency. Anemia that may be accompanied by microcytosis: myelodysplastic syndromes, hemolytic anemia, liver disease.
What test helps determine RBC levels?
The level and quantity of red blood cells can be determined by taking a general blood test.
Donating blood for RBC can also determine:
- The number of red blood cells and their oxygen saturation.
- Hemoglobin level.
- Platelet count.
- Color indicators (oxygen saturation of red blood cells).
- Reticulocyte count.
- Blood erythrocyte sedimentation rate (ESR).
- Leukocyte level.
It is recommended to take a general blood test 1-2 times a year, because low or high levels indicate the development of serious pathologies.
The results are deciphered by a hematologist who, based on the indicators, prescribes treatment.
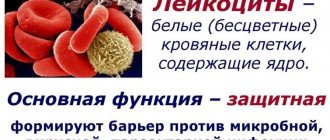
What it is
As we have already said, WBC is an indicator of white blood cells, which are part of the blood
Their importance for the body is as important as the importance of red blood cells, platelets and plasma. However, unlike other cells, they can travel outside the blood vessels to the part of the body where inflammation develops
Leukocytes make up only 1% of the total cell array. But such a small number in no way diminishes the significance of their work. The main activity of these cells is the destruction of foreign agents in the form of viruses and infections, as well as strengthening the protective properties of the body.
Preparing for the study
RBC in a blood test is a test before which preliminary preparation is prescribed.
It goes like this:
- Refusing breakfast and donating blood on an empty stomach , because this way you can accurately determine the level of red blood cells, leukocytes and hemoglobin (it is advisable to carry out the procedure in the morning).
- Avoid coffee , black tea, juice, alcohol and drinks with nitrate additives 8 hours before the test, which reduce hemoglobin and red blood cells.
- Avoid taking medications and antibiotics 12 hours before donating blood, as they disrupt the integrity of red blood cells and leukocytes and reduce hemoglobin.
If the patient is undergoing hospital treatment, then before taking the test, the hematologist performs additional procedures, depending on the disease. It is also recommended to stop smoking, which destroys hemoglobin cells, causing the oxygen concentration in the blood to decrease.
Physiological reasons for changes in hematocrit levels
A natural change in hematocrit level, which is not a consequence of the disease, occurs in the following cases:
- Pregnancy. In women in the second and third trimester of the perinatal period, plasma volume increases significantly, while the number of red blood cells does not change. The blood becomes more dilute, so the hematocrit number drops to 35–40%. In addition, during delivery, heavy blood loss is often observed. In the postpartum period, the ratio of the liquid part of the blood and the formed elements should return to its original values.
- The first 6–7 days of the follicular phase of the menstrual cycle. During the period of natural blood loss by the female body, the composition of the blood changes. The hematocrit percentage decreases. The maximum permissible difference is 5%.
- Conditions associated with oxygen deficiency in body tissues. To compensate for the lack of oxygen, the body strives to produce more red blood cells, and accordingly, the hematocrit increases. An increased need for oxygen occurs during intense sports training (other physical overload), nicotine addiction, and in high mountain climates. And this condition is also observed in newborns, especially with complicated delivery, accompanied by fetal hypoxia.
In the absence of chronic diseases, a slightly reduced HCT is not considered a pathology in people over 65 years of age.
How is blood drawn?
Most often, blood for RBC is taken from a finger; this is a painless and effective way to find out about the indicators of red blood cells and hemoglobin.
Blood sampling from a finger occurs in the following sequence:
- First of all, the laboratory technician lubricates the ring finger on the left hand with alcohol to disinfect and relieve the patient from pain.
RBC in a blood test is often done during a "CBC"
- Then an incision is made on the fingertip with a disposable spear and blood is taken with a pipette, which is placed in a special flask for further examination.
- At the end of the procedure, the laboratory assistant lubricates the finger with cotton wool and alcohol, then the blood from the flask is placed on a special glass, where the indicators are examined.
During pregnancy and serious illnesses, blood donation from a vein is prescribed, which can also be used to determine the functioning of the internal secretion organs. Infectious diseases can cause enlargement of the kidneys, liver and pancreas, so a blood test from a vein will help diagnose abnormalities and select treatment.
Hematocrit - what is it
Hematocrit is one of the conventional blood indicators. It shows the percentage of red blood cell mass to the total volume of biological fluid. The HCT indicator (blood test), the interpretation of which can also be interpreted as the ratio of all formed elements of blood to plasma, most often still determines the volume of red blood cells, because they make up 99% of the total number of blood cells.
The official name of this parameter is the hematocrit number, and in common parlance it is often called “blood density.” Hematocrit is a flask that is used to centrifuge biomaterial, but its name has taken root so well that it is very often used in official medicine.
How long to wait for test results
RBC in a blood test is examined for 1-14 days, because this is an examination that determines the functioning of the immune system and the production of hormones. For patients undergoing inpatient or outpatient treatment, tests are performed within 1-4 hours. This is necessary in order to prescribe appropriate treatment and learn about the progression of serious diseases.
Those who donate blood for preventive purposes need to wait 1-14 days, unless there is a referral from a hematologist. The speed at which results are interpreted is influenced by many factors, especially the quality of equipment in the laboratory.
Increased hematocrit
A high hematocrit is used as an indicator of excessive consumption of exogenous erythropoietin, which stimulates red blood cell production. Athletes can artificially improve their performance by increasing their oxygen carrying capacity with EPO. If the readings are not within the normal range, this does not necessarily mean that there is a disease that requires treatment. To learn more about your results, talk to your doctor.
A high hematocrit reflects an absolute increase in the number of red blood cells or a decrease in plasma volume under conditions such as:
- severe dehydration - such as from burns, diarrhea, or excessive use of diuretics;
- erythrocytosis - increased production of red blood cells;
- polycythemia vera - an abnormal increase in blood cells;
- hemochromatosis is a hereditary disorder of iron metabolism;
- lung or heart disease.
Decoding answers
The results are deciphered by a laboratory assistant, after which the hematologist makes a conclusion and determines the norm of indicators in accordance with age and gender.
The interpretation of the answers will depend on whether the indicators are low or high, which indicates illness or hormonal imbalance.
Definition of the term “erythrocyte”
Red blood cell (RBC), or erythrocyte, is a biconcave disc-shaped red blood cell and belongs to the most numerous group of blood cells. In diameter, a mature erythrocyte has a size from 7.0 to 8.0 µm, sizes less than 5.89 µm and more than 9.13 µm are considered physiological anisocytosis. This structure allows the red blood cells to be maximally saturated with oxygen and carbon dioxide molecules in the bloodstream.
An important component of red blood cells is the pigment hemoglobin, which makes it possible for the lungs to bind oxygen and release this element into tissues and organs.
In addition to transporting oxygen, erythrocytes carry out the function of exchanging lipid molecules in the blood plasma, transporting amino acid residues and biological substances, regulating the acid-base and ionic balance in the blood, and ensuring the body’s water-salt metabolism. They carry out immune reactions by absorbing and destroying toxic substances, and control the coagulation system through the formation of thromboplastin molecules.
Red bone marrow is the site of formation of red blood cells, in which continuous renewal of these cells occurs, therefore their number, like the norm of RBC, remains constant. The lifespan of red blood cells does not exceed 4 months.
Reasons for low values
The concentration and number of red blood cells in the blood may decrease, this happens for the following reasons:
- Severe physical injury or surgery with large loss of blood, resulting in a decrease in the level of red blood cells and hemoglobin in the blood.
- Diseases of the gastrointestinal tract, in which the gastric mucosa is irritated and intestinal function is disrupted (ulcers, gastritis, hemorrhoids, oncology and intestinal anemia).
- Heavy bleeding during menstruation in women, as well as abortions and miscarriages, in which the number of red blood cells and hemoglobin in the blood decreases.
- Iron deficiency anemia and leukemia, in which the concentration of indicators such as red blood cells, hemoglobin and the production of leukocytes decreases.
- Taking antibiotics and medications that increase the production of white blood cells and antibodies in the blood, which reduces the number of red blood cells.
Reference values
The volume of red blood cells in the body is not a constant value, so the hematocrit depends on the following conditions:
- patient's gender;
- age category;
- chronic pathologies.
Temporary conditions of the body (pregnancy, infectious viral diseases, physical overload) are of no small importance. A change in the hematocrit number indicates the density (level of concentration) of the blood. In women, the standard values are lower than in men, since due to physiological characteristics the blood is renewed more often. In addition, the total amount of fluid in the body decreases with age, so children's HCT changes as they get older.
HCT reference values for adults
| Floor | Men | Women | ||
| Age | 18–45 | 45+ | 18–45 | 45+ |
| Norm (%) | 39–49 | 40–50 | 35–45 | 35–47 |
Reference! The average hematocrit for a healthy adult is 40–45% of the total volume of biological fluid.
The maximum permissible upper limit is 50%, the lower limit is 35%. The liquid part of the blood, accordingly, should not occupy less than 50% and more than 65%. When hematocrit values are less than 35%, as a rule, diet correction and systematic monitoring of TCA indicators are prescribed. A decrease in HCT by up to 25% is compensated not only by diet therapy, but also by taking medications. The patient's condition requiring hospital treatment is determined by a hematocrit value of less than 20%.
Normal children's indicators
Children's HCT norm is determined according to age category. Indicators approach adult values at puberty. Standard indicators for children and adolescents:
| Age | Newborn | Infants up to one year old | 1–5 years | 6–11 years | Puberty | |
| Boys | Girls | |||||
| Norm (%) | 33–65 | 33–44 | 32–41 | 33–41 | 35–45 | 34–44 |
Depending on the laboratory conducting the research, standards for children may have a more detailed gradation by age.
The high level of hematocrit in a newborn baby is explained by the transition from the intrauterine state, when the baby is in the amniotic fluid, to a full life (outside the liquid environment).
High level reasons
The intense increase in red blood cells in the blood is influenced by the following factors:
- Pregnancy, in which red blood cells increase due to the growth and development of the fetus (also during Rh conflict between the mother and the unborn child).
- Exicosis and dehydration of the body as a result of diseases, which contributes to a decrease in the number of red blood cells and oxygen, causing the blood to lose saturation.
- Diseases of the gastrointestinal tract and intestines, vomiting, frequent flatulence and diarrhea, which increases the concentration of red blood cells (especially with rotavirus infection).
- Hormonal imbalance and kidney dysfunction, which causes dehydration, which affects the production of red blood cells in the blood and heart function.
To find out exactly why the indicators are abnormal, you need to take a blood test and be examined by a hematologist. Self-medication for deviations from the norm is not recommended, as heart function may worsen due to lack of oxygen.
More about red blood cells and their role in the body
Red blood cells are particularly important formed elements of blood. Their continuous reproduction is carried out by the red bone marrow. Every second, the human body produces about 2.4 million red blood cells, which remain viable for 4 months. At the same time, the level of red blood cell concentration is always maintained in a relatively stable state and corresponds to certain age categories.
Interesting! According to scientists, red bone marrow produces approximately 600 kg of red blood cells during an average life expectancy.
These cells look like a biconcave lens or like small disks squeezed in the middle, which maximizes their surface area. This significantly increases the absorption capacity of red blood cells. Due to the hemoglobin they contain, which contains a red pigment, under a microscope these cells are most noticeable against the background of others, standing out with their bright color. This is why they got their name - red blood cells.
But they acquire this coloring gradually, not from the very beginning of their formation. In the early stages, red blood cells still contain a small amount of hemoglobin and, accordingly, iron, so they differ in their blue tint from other cellular structures. Later they acquire a gray color, and only when their maturation reaches a certain stage, characterized by the appearance of hemoglobin, do the red blood cells become red cells.
Young or immature red blood cells are called progenitor cells or reticulocytes. It should be mentioned that red blood cells that circulate in venous blood are blue in color, since they have already participated in the exchange of oxygen and carbon dioxide, as a result of which they have lost hemoglobin. Despite the fact that red cells have a rather narrow specialization, their role for the normal functioning of the body is difficult to overestimate.
The main functions of red blood cells include:
- transportation of oxygen from the lungs to all cellular structures of internal organs;
- transfer of a metabolic product, carbon dioxide, from the tissues of organs in order to remove it from the body;
- protecting the body from immunological and autoimmune pathological processes;
- participation in a large list of biochemical reactions occurring in the body;
- adsorption (absorption) of toxic substances and pathological antigens;
- ensuring acid-base balance.
The principle of gas exchange carried out with the help of red blood cells
Thus, the body’s respiration and sufficient gas exchange depend on the quality functioning of red blood cells. In addition, they participate in saturating tissues with essential amino acids and enzymes that can attach to the extensive surface of red blood cells.
What to do to normalize the indicator
RBC in a blood test is a test that will help determine the appropriate treatment method if there are deviations from the norm. You can normalize the indicators with the help of medications and folk remedies; you can find out which one will be suitable from your attending hematologist.
Medicinal and traditional methods of increasing RBC levels
To increase the number of red blood cells, the following drugs are recommended:
- Contains divalent ferum sulfate (Tardiferon, Ferretab, Aktiferin, Feroplex, Fero-Folgamma, Sorbifer Durules and Gino-Tardiferon).
- Contains trivalent ferum sulfate for adults (Biofer, Ferrum lek, Ferlatum Fol, Maltofer, Ferlatum and Fenyuls).
- Contains folic acid and vitamin B9, which increases the concentration of hemoglobin and red blood cells in the blood (Biofer, Ferretab, Maltofer Fol and Gyno-Tardiferon).
- With cyanogen cobalamin, vitamin B12 and ascorbic acid, which saturate the blood with red blood cells and hemoglobin (Ferro-Folgamma, Sorbifer Durules and Actiferrin).
- Preparations for injection and internal administration, due to which hemoglobin and oxygen in the blood increase (Venofer, Cosmofer and Argeferr).
There are also traditional methods for raising red blood cells; they are suitable for those who are allergic or intolerant to medications.
The best folk remedies are:
- A decoction of rose hips and wild rosemary. Rosehip and wild rosemary contain a large amount of vitamins and enzymes that help improve blood circulation and increase red blood cells. To prepare, you need to add 100 g of rose hips and wild rosemary, then boil and let sit for 10-15 minutes. It is recommended to drink the decoction 2-3 times a day, on an empty stomach before eating.
- Hawthorn decoction. Hawthorn infusion improves heart function and blood circulation; consuming it has a chance to increase hemoglobin and red blood cells. To prepare, you need to brew 150-200 g of hawthorn, then let it brew for 5-10 minutes. Hawthorn can be drunk by adults and children, if there is no allergic reaction or individual intolerance to the body.
- Radish salad and radishes. Radishes and radishes contain high amounts of iron and vitamin B9, which increase red blood cell counts. To prepare, you need to chop or blend 1-2 radishes and radishes, then add sugar or salt to taste. Eating salad is not recommended for those who have gastritis or stomach ulcers.
- Apple and quince salad. Quince and apples are the main sources of iron that will help improve your RBC levels. To prepare, you need to peel and chop 2-3 apples and 1-2 quinces, then add sugar to taste. You can also add carrots, pears and radishes to taste if you are not allergic.
- Walnuts with honey. Walnuts contain vitamins and enzymes that help increase RBC. You need to consume them with honey 1-2 times a day, unless there is an excess of iodine and thyroid diseases.
Before choosing medications yourself, you need to consult a hematologist and nutritionist. It is also necessary to see an allergist and undergo tests that will determine whether you are allergic to medications and pills.
Drugs and folk remedies to lower RBC
To lower red blood cells and hemoglobin concentration in the blood, hematologists prescribe the following medications:
- Acetylsalicylic acid, which helps thin the blood, making it less saturated with oxygen and hemoglobin (Aspirin, Aspeter, Plocard, Aspecard and Acekor).
- Dipyridamole, which helps to constrict blood vessels and thin the blood with an increased level of red blood cells (Curantil, Aklotin, Agenox and Acekor cardio).
- Clopidogrel, which reduces oxygen in hemoglobin, causing red blood cell counts to decrease (Atherocard, Platogril, Lopigrol and Trental).
When the concentration of red blood cells is high, leeches are also used; this method is called hirudotherapy.
To lower red blood cells and hemoglobin, experts recommend the following folk remedies:
- Tincture of dandelions and horsetail. Dandelion and horsetail leaves help lower red blood cell counts while improving the functioning of the heart and blood vessels. To prepare, you will need 20-50 g of dandelion stem and 50-100 g of horsetail leaves, then boil. After preparation, you need to let the broth brew for 10-15 minutes, then drink 2-3 times a day after meals.
- Chamomile and calendula decoction. To prepare the decoction, you need to pour boiling water over 100 g of chamomile and 100 g of calendula, then let it brew for 10-15 minutes. Chamomile and calendula help thin the blood and constrict blood vessels, which can help get rid of excess RBC and hemoglobin in the blood.
- Lemon juice. Lemon contains a large amount of acetylsalicylic acid, which thins the blood and makes it less saturated. To prepare, just squeeze 1-2 lemons into a glass of water, then add sugar or honey to taste. It is recommended to drink juice 2-3 times a day after meals.
- Dill decoction. Dill improves the functioning of the liver, kidneys and blood, thereby reducing the concentration of red blood cells and hemoglobin in the blood. To prepare the decoction, you need to boil 50 g of dill, then let it brew for 10-15 minutes. Dill decoction can be drunk by adults and children if there are no allergic reactions or other contraindications.
- Banana and apricot salad. To prepare the salad, you need to finely chop or blend 1-2 bananas and 2-3 apricots, then add sugar, dried apricots or raisins to taste. The salad will help improve the functioning of the intestines, heart and blood circulation, thereby reducing the levels of hemoglobin and red blood cells in the blood.
- Black sweet tea. If there is an excess of hemoglobin and red blood cells, it is recommended to drink black tea with sugar 2-3 times a day, which helps reduce levels. It is advisable to drink sweet black tea in its pure form, without flavoring additives that negatively affect the functioning of the intestines and stomach in general.
RBC in a blood test is an examination that will help determine whether the indicators are elevated or decreased. Based on this, treatment can be determined. It is also worth reviewing your diet and adding foods that, based on test results, will increase or decrease RBC levels in the blood.
Deviations
A transcript of the study may show both increased and decreased levels of red cells. Deviations from the norm indicate the development of some disease in the body.
Reduced
If the RBC count is low, the patient needs to undergo additional medical examinations. A pathological RBC level indicates the development of severe pathologies that require immediate treatment.
The process of reducing the number of red blood cells in the blood means the patient develops erythrocytopenia. Most often, the level of these cells decreases due to anemia or massive blood loss. Among the most common causes of erythrocytopenia are:
- increased destruction of red blood cells;
- malignant neoplasms of the hematopoietic system;
- myelomas;
- spread of metastases;
- chronic inflammatory pathologies;
- hereditary pathologies of the blood production process;
- autoimmune pathologies;
- diseases of the kidneys and urinary organs;
- chemotherapy;
- increased water content.
In addition, RBC decreases as a result of insufficient intake of cyanocobalamin - vitamin B12 - into the body. Because of this, erythropoiesis, i.e., the process of formation of blood cells, suffers. Some pathologies of the digestive tract lead to insufficient absorption of iron in the body. Low iron levels in the blood cause a decrease in the amount of hemoglobin and red blood cells.
The reduction of RBC is facilitated by the use of barbiturates and their derivatives.
This is also facilitated by following a diet that avoids meat products. The body does not receive enough essential nutrients, which disrupts the formation of red blood cells.
The interpretation of the blood test shows the presence of anemic and sidereal syndrome in the patient. Anemic syndrome is accompanied by the following symptoms:
- malaise, constant fatigue;
- weakness;
- inability to tolerate prolonged physical and mental stress;
- pain in the head;
- frequent dizziness or fainting;
- sleep disorders;
- dyspnea;
- increased heart rate (both at rest and during exercise);
- blackening of the stool (this symptom appears as a result of bleeding from the digestive tract and requires immediate medical attention).
Important information: What does a reduced leukocyte index of intoxication mean?
Sideropenic syndrome is characterized by the following symptoms:
- disturbance of taste (desire to eat chalk, clay and other inedible substances);
- the emergence of a desire to sniff paint, acetone, household chemicals, gasoline;
- hair fragility, increased tendency to hair loss;
- the appearance of white spots on the nails;
- peeling and drying of the skin;
- paleness of the skin and sclera;
- development of cheilitis (inflammation of the corners of the lips).
In severe stages of anemia, the following symptoms are observed:
- sensation of goosebumps crawling on the skin;
- numbness of hands and feet;
- difficulty swallowing;
- the appearance of uncontrolled bladder emptying.
You can increase the reduced RBC value in this disease with the help of properly selected nutrition and the use of medications.
Beneficial to consume daily:
- beef liver;
- language;
- rabbit and turkey meat;
- fish;
- dried mushrooms;
- fresh peas;
- buckwheat porridge;
- apricots;
- pears and apples;
- cherries;
- plum;
- beets.
Eating animal products helps you better absorb iron.
The most common tablet drugs for enhancing hematopoiesis are Ferroplex, Sorbifer, Totema, Aktiferrin, Maltofer, Ferrostat. These drugs are combined with Ascorbic acid.
Injection use of agents to enhance the production of red blood cells is advisable in a clinical setting, because some of them can cause an intolerance reaction.
Complications with high and low RBC values
If you do not engage in treatment and do not restore the normal level of red blood cells in the blood, you may experience unpleasant symptoms and complications.
At high values, the following symptoms and complications may be of concern:
- An increase in glucose and sugar in the blood, which causes blockage of blood vessels, which causes hormonal imbalance and diabetes.
- Heart failure, risk of stroke and myocardial infarction (acute pain in the heart and cardiac muscles is also a concern).
- Disruption of the pancreas, thyroid and thymus glands, which causes hormonal imbalance and metabolic dysfunction in the body.
- Impaired liver function and hepatomegaly, resulting in an increase in the size of the organ and unpleasant symptoms (rash on the face, discoloration of the skin and bruises under the eyes).
- The total body weight decreases, this is due to dehydration of the body and improper functioning of the gastrointestinal tract (dystrophy and anorexia occur).
With low levels, the following symptoms and complications may occur:
- Disruption of the blood circulation and heart function, which causes frequent shortness of breath and a feeling of lack of oxygen (also associated with brain hypoxia).
- Violation of the gastrointestinal tract and food absorption, which causes flatulence, diarrhea, vomiting and nausea (intestinal anemia may occur).
- Loss of appetite, inability to digest food and irritation of the gastric mucosa, which can lead to serious illnesses (gastritis, ulcers, dystrophy and anorexia).
- Disorders of the menstrual cycle in women, as well as difficult childbirth and frequent miscarriages as a result of insufficient circulation of oxygen in the blood to the fetus.
- The appearance of unpleasant symptoms that impair general health and reduce a person’s physical activity (drowsiness, nausea and weakness).
RBC in a blood test helps determine the concentration of red blood cells and hemoglobin, which makes it possible to diagnose diseases in the early stages. This examination is recommended for adults and children in order to determine indicators in time and begin treatment.
Article design: Vladimir the Great
Reasons for the increase
The growth of RBC in the blood in 80% of cases indicates pathological processes. Which ones and how heavy are another question. Possible factors for violation include:
Megaloblastic anemia
It develops if the body has little vitamin B12. Or when the substance is not absorbed enough. For example, during inflammation of the digestive tract, metabolic disorders.
The disease leads to changes in the hematopoietic pattern. Inferior cells emerge into the channel. But they are registered by hardware analyzers, which is why false results are obtained.
The condition is accompanied by several typical symptoms:
- Weakness.
- Drowsiness.
- Feeling of fog in the head.
- Dyspnea.
- Exercise intolerance.
- Paleness of the skin.
- Pressure surges.
- Cardiac disorders.
Here are just some of the signs of the disorder.
Treatment is carried out by hematology specialists. The goal is to compensate for the vitamin deficiency. If necessary, correct the pathological process that interferes with the absorption of the substance.
Artificial substitutes are used, and inflammation therapy is also carried out. Read more about the megaloblastic form of anemia in this article.
Iron-deficiency anemia
Another type of disorder. In this case, there is not enough iron. Unlike the megaloblastic form, this one is not as aggressive and develops rather slowly.
A full clinic unfolds over several weeks, or even months.
Among the manifestations of the pathological process:
- Feeling weak.
- Heart disorders.
- Drowsiness.
- Brittle hair and nails.
- Dry and dull skin.
- Pallor.
- Tendency to distort taste preferences.
- Dyspnea.
- Impaired memory and cognitive functions in general.
The patient needs to be treated. The task falls on the shoulders of the hematologist. Load doses of iron are prescribed and the drug is administered according to a strictly verified scheme.
If the reason is insufficient absorption of the substance, treatment of the underlying pathological process is required. This is the only way to bring the situation back to normal. Everything takes up to several weeks.
Read more about the causes and treatment of iron deficiency anemia here.
Blood loss
Massive or scanty. Doesn't matter. The point is that the body tries to compensate for the violation on its own. After all, formed cells leave the body mechanically and fall out of active activity.
The intensification of bone marrow function is temporary. Therefore, as soon as the condition returns to normal, the number of red blood cells will also restore itself.
Whether the patient needs to be treated is decided by the doctor in each specific case. The same applies to the treatment regimen.
In case of heavy blood loss, a transfusion of red blood cells, plasma or whole liquid connective tissue is prescribed. In this case, it is necessary to observe that there is no conflict or rejection of the substance. This is the main task for the first few days after the procedure.
If the blood loss is not so great, they look for the cause of the disorder. These may be erosive ulcers, inflammatory diseases of the digestive tract, gynecological problems and other disorders.
The question remains with the specialist. After a thorough diagnosis, the cause is eliminated. From now on, everything should return to normal.
Therapy is the prerogative of the hematologist. Also, if necessary, third party specialists are involved.
Pathologies of the cardiovascular system
Diseases of cardiac structures. Multiple in nature. Here are just the most common options:
- Hypertension. Persistent increase in blood pressure.
- IHD. Cardiac ischemia.
- Coronary insufficiency. When the myocardium does not receive enough oxygen and nutrients.
- Previous heart attack. As an acute, urgent condition.
All diseases of the cardiovascular system, one way or another, are united in the hypoxic factor. There is not enough oxygen. Is the body trying to compensate for the pathological condition through increased production of red blood cells? which causes an increase in RBC in the blood.
For a while this is enough, then everything starts all over again. As soon as decompensation of the condition occurs.
Treatment is specific, depending on the diagnosis. In any case, a cardiologist should work with the patient.
Antihypertensive drugs, cardiac glycosides, and organic nitrates are prescribed.
It is important that the means clearly correspond to the situation. Otherwise it will only get worse.
RBC values will return to normal as soon as the primary pathological process is eliminated. This may take up to several months or a little less.
Hypoxia
Often, RBC in a blood test deviates from the norm upward as a result of the ischemic process. It has already been said about it. A special case of a violation is coronary insufficiency and a heart attack. But there are also situations that are not so pronounced.
For example, among them:
- Encephalopathy. A chronic complex process in which the brain is insufficiently supplied with blood.
- Transient ischemic attacks. Acute nutritional disturbances of cerebral structures without signs of critical condition.
- Stroke. Intense disorder of trophism of nerve tissues of the brain. Urgent help is required, otherwise the patient may die.
- Weakening of trophism against the background of thrombosis and vascular inflammation.
The point is one thing. These disorders cause poor nutrition and breathing. The body tries to compensate for the deficiency. If the disorder is long-standing, there is no point in it. The process will continue to progress.
Treatment is the task of a specialized specialist. If the heart suffers, a cardiologist works. The brain is a neurologist. You may need the help of a vascular surgeon.
Therapy is multifaceted. Depends on the pathological process. Cerebrovascular drugs are prescribed. If the problem is excess cholesterol - fibrates, statins. And further down the list.
Lung pathologies
Disorders of the respiratory system. If you understand how gas exchange occurs, it becomes clear what's what.
The fact is that red blood cells are filled with oxygen upon contact with the lungs. Carbon dioxide is removed in exactly the same way. Therefore, any deviations in the functioning of the respiratory structures lead to the same outcome.
The degree of disturbance depends on how pronounced the primary pathological process is.
Possible diagnoses include:
- Pneumonia.
- Bronchial asthma.
- Respiratory failure.
- Tracheitis, laryngitis. Even if indirectly, they affect the activity of the lungs.
And so on. If the pathology is neglected, it will be difficult to cope. It is necessary to begin correction from the very start of the disease.
Therapy falls on the shoulders of the pulmonologist. Several types of drugs are used:
- Bronchodilators. To expand the lumen of the respiratory tract and restore normal gas exchange.
- Antibiotics. To eliminate the infectious process.
- Stimulators of antibody production. So-called antiviral agents.
The list is far from complete. Glucocorticoids are also used. After correction of the underlying condition, red blood cells return to normal.
Bad habits
Smoking is especially harmful. The problem is not so much nicotine, cadmium compounds, antimony and arsenic. They are contained in cigarettes and any tobacco products and really harm the body.
It's a matter of hot smoke. It burns the walls of the respiratory tract and causes thermal damage. More mucus is produced, a slow but sure degeneration of tissues, the epithelium of the inner lining of the bronchi and lungs, occurs.
The result will not take long to arrive. Chronic inflammation at an early stage leads to an increase in the content of red blood cells, RBC increases.
Then, if you don’t do anything and don’t give up cigarettes, lung cancer is likely to develop. This condition will lead to an even more rapid increase in the number of red cells.
There can be only one treatment here - quit smoking as quickly as possible. It's difficult to cope on your own. If this is the case, you should consult a psychotherapist.
Smoking drugs: marijuana, hashish, nasvay and other chemical rubbish has an equally negative effect and even more so. Complications develop many times faster and are much more dangerous.
Malignant oncology
Simply put, cancer. It doesn’t really matter what localization it is. In any case, when the process is sufficiently developed, bleeding begins.
Unnoticeable at first. But red blood cells leave the body and lose their functional properties. Then more and more pronounced. The body compensates for the lack of cells by producing new ones.
Cancer has specific focal symptoms. But there are some general signs of a violation:
- Increase in body temperature.
- Pathological thinness. Due to the gluttony of cells and the need for abundant nutrition. There is simply nothing left for all other systems.
- Weakness.
The treatment strategy is standard. With some reservations and amendments for a specific clinical case.
- The tumor is removed. As much as possible. Ideally, if you can eliminate it completely.
- Radiation treatment involves exposing tissue to radiation.
- Chemotherapy. To kill remaining cells and prevent relapse.
The prognosis is determined by the oncologist who is caring for the patient. It is better to address the question to him.
Bone marrow disorders
As a rule, acquired forms of the pathological process. These are so-called myeloproliferative diseases. When cells are produced in excess.
RBC in the blood test is increased due to the fact that the brain substance synthesizes them too quickly - the rate of maturation also increases. True and false forms of violation are possible.
- In the first case, the red blood cells are complete. These are ordinary red blood cells.
- In the second, the cells are immature. Defective forms, although registered by analyzers, still cannot perform the functions assigned to them.
Bone marrow disorders are often congenital. Genetically determined types of pathology cannot be treated. All that remains is to fight the symptoms.
In all other cases, etiotropic methods are used.
The basis is cytostatics. They slow down the production of formed cells and suppress bone marrow activity. This is a temporary but absolutely necessary measure.
As a supplement, glucocorticoids are prescribed. True, not always. Hematologists provide treatment.