Pain in the epigastric region, a feeling of heaviness after eating food, belching and the appearance of an unpleasant taste in the mouth are not always associated exclusively with lesions of the stomach. Very often, the cause of unpleasant symptoms is the esophagus - the “conductor” between the oral cavity and the stomach.
Sometimes his condition becomes the reason for numerous patient complaints of severe discomfort and pain, especially after eating or drinking. In this case, you cannot do without a visit to the doctor - only an experienced specialist can make an accurate diagnosis and draw up a plan for the correct treatment of the disease. Since many gastrointestinal diseases are accompanied by similar symptoms, special examinations are indispensable. One of them is radiography of the esophagus.
Description of the method
X-ray of the esophagus belongs to a group of non-invasive methods in which pathological processes are visualized using X-ray irradiation. With radiography, the patient receives a radiation dose of 0.1 to 0.8 mSv, with fluoroscopy up to 3.5 mSv.
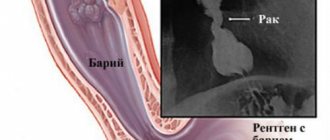
Contrast is done for a clearer image. Without contrast, it is generally difficult to see anything in a survey image. These may be preparations containing iodine compounds or barium sulfate. Sometimes they resort to the double contrast method, when, along with “barium porridge,” an air mixture is pumped under pressure into the esophagus.
A detailed examination of parts of the esophagus is carried out using a thick barium suspension. It slowly moves through the mucous membrane, thanks to which it manages to paint all its folds and highlight pathological neoplasms.
There are usually no problems with swallowing a contrast agent, but sometimes undesirable consequences may occur, such as:
- Asphyxia occurs in cases where the contrast flows into the trachea or bronchi, in the presence of fistulas between the esophagus and trachea or the esophagus and bronchi, and with swallowing disorders.
- Allergic reaction to barium sulfate as a complication of X-ray examination of the esophagus. The physician should be aware of the patient's experience of feeling unwell after taking contrast.
X-rays of the esophagus with contrast can also be done in children. But problems arise with obtaining high-quality images. The child does not cooperate well, which is necessary for the procedure.
Fluoroscopy is distinguished by one feature, the essence of which is the ability to examine the work of the upper part of the digestive tube in dynamics. This makes it possible to find out at what speed the contrast is moving, which gives a complete objective picture of the reserves of the esophagus. The X-ray shows:
- How the circular and sphincter muscles of the esophagus work.
- How intact is the mucous membrane?
- What is the shape and functional state of the esophagus?
X-ray diagnosis of the esophagus
The esophagus normally visible on radiographs. As an example, here is an x-ray of a dog that shows a normal esophagus.
But there are exceptions in which the esophagus can be visualized normally. Such exceptions include the following:
- animal under anesthesia - reflux of stomach contents;
- a spontaneous breath of air at the moment of shooting;
- a small amount of air (mainly in the cranial part of the esophagus) in brachiocephalics.
With a contrast study, it is normal on x-rays taken immediately after the administration of a radiopaque substance in the esophagus that the contrast is either not retained at all and the esophagus is not visualized, or a small amount of contrast can be visualized on the walls of the mucous membrane. In this case, in dogs, the contrast will be visualized in the images in the form of stripes (as presented below), this is due to the fact that the mucous membrane of the dog’s esophagus is collected in longitudinal, easily straightened folds.
And in cats, contrast in the esophagus can normally be visualized in the form of a “herringbone” or “fishbone”, but taking into account that the x-ray was taken immediately after contrast was given. This is due to the fact that the mucous wall of the esophagus has a scaly surface (mainly its distal part).
But we must keep in mind that if a radiopaque substance is visualized in the esophagus on x-rays taken later than 5 minutes after contrast was given, then we can talk about pathology of the esophagus. And in this case, depending on the x-ray picture, one or another x-ray diagnosis will be made.
Let us consider the main pathologies of the esophagus found on radiographs. These include:
- Foreign bodies
- Esophagitis
- Megaesophagus
- Esophageal diverticulum
- Neoplasms
- Perforation of the esophagus
- Esophageal stricture
- Cricopharyngeal achalasia
- Pathology of the vascular ring
Esophagitis
is an inflammation of the esophagus. With this disease, X-ray images clearly visualize the esophagus (mainly the thoracic part of the esophagus against the background of radiolucent caudal lobes of the lungs), which has increased radiological density (the darkening of the esophagus will be visualized on the image) and will be visualized between the aorta and the caudal vena cava.
X-ray photographs of a cat show x-ray pictures of esophagitis (the picture was taken in the right lateral projection) in a cat and a dog.
Cat esophagitis in the right lateral projection Dog esophagitis in the right lateral projection
Foreign bodies of the esophagus.
Due to the different nature of the origin of foreign bodies swallowed by animals, they are divided into radiopaque and non-radiopaque foreign bodies.
Radiopaque foreign bodies can be: meat and fish bones, sewing needles, coins and other metal objects, balls made of dense materials, glass, fishhooks, guitar strings, stones, rings and other jewelry, screws, etc.
Non-radiopaque foreign bodies can be: rags, threads, plastic film, rubber products, pieces of wood, Christmas tree tinsel and rain, socks, cotton wool or cotton toys, etc.
In general, non-radio-opaque foreign bodies are more difficult to distinguish on radiographs than radio-opaque foreign bodies. However, the presence of non-radiopaque foreign bodies in the esophagus can be distinguished by indirect signs: to the location of the foreign body in the esophagus, a significant amount of air will be visualized, and sometimes even a significant expansion of the esophagus itself. In other cases, contrasting of the gastrointestinal tract is necessary.
On X-ray photographs of a cat taken after contrasting with the radiopaque substance Bar-VIPS or Omnipaque, a non-radiopaque foreign body in the esophagus - a thread - immediately becomes easily visible.
Foreign object of the esophagus (thread)
Radiopaque foreign bodies in the esophagus are very easily identified on X-ray films. On X-ray photographs of a cat, a radiopaque foreign body – a needle – is clearly visualized (the pictures were taken in the right lateral and dorsoventral projections).
Also, a radiopaque foreign body of the esophagus can be a fishing hook and fishing line.
Foreign object (hook). Right lateral projection. Foreign object of the esophagus (animal figurine) Foreign object (needle). Right lateral projection. Foreign object (needle) Ventro-dorsal projection.
Here are some more x-rays of a cat with a radiopaque foreign body in the esophagus, which in this case is a chicken breast bone.
Foreign object (chicken bone) Dorso-ventral projection. Foreign object (chicken bone). Lateral projection on the right side. Foreign object (chicken bone) in the esophagus. Ventrodorsal projection
Megaesophagus
is a pathological expansion of the esophagus due to a violation of its motor function. Most often occurs in infancy. With this disease, X-ray images visualize a uniform expansion of the esophagus along its entire length, and depending on the contents, the esophagus is visualized either filled with air, or darkening of the esophagus may be noted. It should also be taken into account that to make an x-ray diagnosis of megaesophagus, it is sufficient to take plain x-rays. You should not resort to contrast because, firstly, if there is complete obstruction, then it is unknown how long the contrast will remain in the esophagus and all this can subsequently lead to perforation or rupture of the esophagus, which means the release of the contrast agent into the lumen of the chest and subsequently lead to the death of the animal. Secondly, if the animal goes to the operating table to resolve this disease, then the contrast will greatly interfere with the surgeon’s ability to carry out such a labor-intensive operation and there is also a risk of the contrast getting into the lumen of the chest cavity.
Now let's look at how megaesophagus is visualized on x-rays.
Megaesophagus of the esophagus. Right lateral projection. Megaesophagus of the esophagus with liquid contents. Right lateral projection.
Neoplasm of the esophagus.
Neoplasms of the esophagus can be different and their locations can also vary. X-rays may show widening of the esophagus or displacement of the esophagus. Most often, on radiographs, a neoplasm of the esophagus is revealed as a rounded shadow with soft tissue density (darkening is observed) in the projection of the distal part of the thoracic esophagus caudal to the heart and in front of the diaphragm. In this case, a small amount of free fluid and bridges between the lobes of the lungs can be visualized in the lumen of the chest cavity. And also, depending on the duration of the process, metastases on the lungs can be visualized.
With the contrast method of examination, the contrast may be delayed in front of the localization of the tumor, and also stain the volumetric formation itself.
On the initial x-ray taken in the right lateral projection, a rounded darkening is visualized in the caudal part of the thoracic esophagus, and air in the esophagus is visualized cephalad from it.
Tumor in the caudal part of the esophagus. Tumor of the esophagus in the lateral projection. The contrast agent used was a tumor of the esophagus. Ventrodorsal projection. X-ray contrast agent was used
The following images were taken 30 minutes after giving the Bar-VIPS contrast agent in the right lateral and ventro-dorsal projections. At the same time, X-ray images clearly visualize that part of the contrast has passed, and part has stopped in front of the localization of the space-occupying formation.
The next photograph was taken the next day in the right lateral view. At the same time, the contrast passed further along the gastrointestinal tract, coloring the neoplasm itself.
Tumor of the esophagus in the caudal region. An image taken one day after the administration of a contrast agent.
Perforation of the esophagus.
With perforation of the esophagus, x-rays taken in direct and lateral projections visualize a significant increase in the distance between the sternum and the heart; depending on the contents, this distance can be either with increased radiological density, or, conversely, with reduced density. Also, in the lumen of the chest cavity, free fluid and bridges between the lobes of the lungs, darkening of the fields of the lungs, the pattern of the pulmonary vessels is significantly blurred, and sometimes atelectasis or pulmonary emphysema can be observed.
The picture was taken 30 minutes after the contrast agent was administered.
Esophageal diverticulum.
Esophageal diverticula are quite rare in animals. They are a sac-like protrusion of the wall of the esophagus and can be congenital or acquired.
Usually, changes are not detected on plain radiographs, but sometimes, depending on the contents of the diverticulum, a sac-like protrusion of the esophagus filled with gas or food is visualized.
When conducting a contrast study, the esophageal diverticulum is clearly identified, since the contrast agent accumulates in the sac-like protrusion of the esophagus.
Esophageal stricture.
Plain radiographs do not reveal any pathology. Sometimes a prestenotic dilatation of the esophagus filled with gas or food is visualized.
To confirm the diagnosis, a contrast study is required. It allows you to identify the number, location and size of strictures, as well as the degree of narrowing of the esophagus. The presence of narrowing in the same place on several radiographs allows us to differentiate a stricture from a spasmodic contraction of the esophagus. In the area of stricture, the normal folds of the esophageal mucosa come together and become uneven.
X-ray shows prestenotic dilatation due to stricture of the caudal esophagus in a cat.
Esophageal stricture
Pathology of the vascular ring.
Pathology of the vascular ring is a congenital pathology of the development of large arteries of the heart. It occurs in animals under 1 year of age, but usually the problem clinically manifests itself after weaning of the puppy and kitten.
Congenital anomalies of blood vessels in the chest cavity can lead to the fact that the vessels or their atrophied areas form constrictions that compress the esophagus at the level of the base of the heart. Such constrictions are called vascular rings. The presence of abnormal vessels near the esophagus prevents its normal expansion during the passage of food. Over time, the esophagus expands cranially from the site of constriction due to the constant accumulation of food in this area.
As a rule, on X-ray photographs, the pathology of the vascular ring manifests itself as follows: in the cervical region, the contrast is distributed evenly, in front of the persistent ring, a prestenotic dilatation of the thoracic part of the esophagus is visualized, then a narrowing and bridge over the base of the heart is visualized, and then a uniformly colored and undilated caudal part of the thoracic esophagus .
Rice. Persistent right aortic arch in a dog: A - dilated cervical part of the esophagus, B - prestenotic dilatation of the esophagus, C - narrowing and filling defect in the area of the base of the heart shadow (corresponds to the level of compression of the esophagus by the right aortic arch), D - cardiac shadow, E - normal caudal part of the esophagus.
You can do x-ray diagnostics in Tver at our veterinary clinic “Doctor Ay and Oy” at the address: Tver, T. Ilyina St. 1 B. If you have any questions, please call; (4822)737-077
Source of the VK article “Doctor Ai and Oi” - 2015
Radiologist M.S. Aleksandrova
Indications and contraindications for fluoroscopy
Your doctor may order an x-ray if you have the following symptoms:
- problems swallowing solid and liquid foods;
- sensation of a foreign body in the throat;
- soreness in the sternum;
- reflux, in which the contents of the stomach are thrown back into the esophagus;
- belching;
- causeless vomiting.
X-rays may also be prescribed:
- if there is a need for bougienage;
- to identify the degree of stenosis;
- for various burns;
- to determine the extent of organ damage after injury.
X-ray anatomy of the esophagus is not applicable if the patient:
- individual hypersensitivity to barium salts;
- severe general condition;
- tumor process affecting the intestines;
- the presence of exudate, purulent process and severe bleeding in the abdominal cavity.
In case of emergency, the method is allowed during pregnancy, if urgent diagnosis justifies the possible risk to the fetus. When examining a patient with mechanical intestinal obstruction, barium porridge is replaced with gastrografin.
Trendelenburg study
This method can be used to diagnose a hernia. In this case, the patient takes a certain position. Lies down with the pelvis elevated at 45 degrees. Before this, accordingly, drinks a barium suspension. Thanks to a certain position, the mixture penetrates into the intestine through the holes of the diaphragm. This results in a clear outline.
This position allows for better visualization of the diaphragm and hiatal hernia. But this method is strictly prohibited:
- in case of fluid accumulation in the abdominal cavity;
- with intestinal tumor;
- disturbances in the functioning of the heart and pulmonary system.
In other cases, the method can be carried out without restrictions.
Preliminary preparation
Prepare for x-rays of the esophagus in the same way as for x-rays of the stomach. It often happens that after studying the condition of the esophagus, the diagnostic search expands and a decision is made to examine the lower gastrointestinal tract. Sometimes, after identifying a tumor process in the esophagus, it becomes necessary to examine the stomach. It is important for the surgeon to obtain the most reliable and detailed information about his condition in order to perform a possible operation to resect it.
If the stomach and intestines are functioning normally, x-rays are performed without special preparation. The patient only needs to follow these rules:
- Take the last meal 8-9 hours before the due time. For children, the fasting period depends on age: up to a year it is 4 hours, older - 6 hours.
- Foods that cause increased gas formation should be excluded from the diet.
Elderly patients and those with stomach problems are specially prepared for the examination:
- For 5 days they follow a diet excluding dairy, bakery products, sweets, and carbonated water.
- If necessary, perform gastric lavage.
The patient should be warned that the barium sulfate suspension has a consistency similar to a lime-flavored milkshake. First, a dense suspension is drunk, and then diluted with a volume of up to 400 ml. The patient should also be warned about the need to observe safety precautions, since the images will be taken in different positions of the examination table.
How to prepare for an x-ray of the stomach and esophagus
As preparation for fluoroscopy of the stomach, only a specialized diet is used. It is necessary in order to free the gastrointestinal tract from undigested food particles, which can interfere with obtaining clear images or create “interference” in the area of X-ray action. In addition, in preparation for x-rays of the esophagus and stomach, it is necessary to exclude the possibility of gas formation in the digestive tract.
A few days before the procedure, it is important to exclude from the diet foods that take a long time to digest:
- vegetables with a lot of fiber and coarse fibers;
- fatty meats;
- smoked meats and marinades.
In preparation for examining the digestive tract using x-rays, products that promote gas formation are excluded from the menu: legumes, carbonated drinks and sweets, fermented milk drinks, cheese. Also, in preparation for an x-ray of the stomach, it is important to exclude foods that affect peristalsis. First of all, these are spices and alcohol.
On the eve of the study, you need to prepare with an enema or laxatives - the intestines and stomach must be completely empty. Therefore, on the eve of the procedure, stop taking food and water for several hours.
In preparation for the examination, it is important to consult with a radiologist regarding the use of certain medications. In most cases, doctors do not advise taking medications on the eve of the test. If the patient has a stomach ache, the doctor may allow you to take medications prescribed by the gastroenterologist during the preparation for the x-ray examination.
Important! During the period of preparation for x-ray of the gastrointestinal tract, it is not recommended to take antispasmodics, as they can cause short-term changes in peristalsis, as a result of which the diagnosis will not be accurate.
What can you eat before the test?
In order for the X-ray of the stomach to be accurate, it is important when preparing for an X-ray of the stomach and esophagus to give preference to easily digestible food prepared by boiling. You can drink herbal or green tea, coffee drink, cocoa, and compotes without restrictions.
Gastroenterologists recommend eating regularly and in small portions before an x-ray. The food temperature should be between 25 and 60 degrees Celsius.
In order for the preparation for the x-ray examination to go correctly, it is important to stop eating in time before the x-ray. Experts recommend avoiding eating in the evening, that is, 8-12 hours before the examination. The fluid intake should take place 2-3 hours before an x-ray of the esophagus and stomach is taken.
If the described measures are followed, the intestines should be empty by the time of the examination. If gastrointestinal diseases prevent this, patients prepare for x-ray examination through an enema.
When can you eat after the test?
After an x-ray of the esophagus and stomach has been taken, you can start eating immediately after diagnosis. However, it should be taken into account that a suspension of barium salt actively absorbs liquid, which can lead to the formation of fairly dense masses in the gastrointestinal tract. Under certain conditions, they can clog the intestinal lumen. To prevent this from happening, it is important to start eating mostly liquid foods after the x-ray, and to drink as much water as possible in the first hours.
Progress of the examination
Before the procedure, the patient removes metal jewelry, puts on a robe, removes dentures, removes hair clips and all objects that may be in the radiation zone, and drinks barium porridge (barium sulfate). In this case, the radiologist watches on the fluoroscope monitor the progress of the barium suspension through the esophagus.
The first sip should be small in volume. It allows you to identify pronounced narrowings that may impede the progress of the contrast agent. If there is a significant impairment of the patency of the esophagus, large volumes of barium suspension do not increase the information content of the technique, but only worsen the patient’s condition. If patency is satisfactory, the patient drinks the entire prescribed volume of barium sulfate. A barium tablet or barium flake will help better visualize dysphagia and small strictures.
An X-ray of the esophagus according to the traditional method is performed in the morning. Cleansing enemas given the night before and 3 hours before the procedure help cleanse the intestines. In addition to the esophagus, the diaphragm, pharynx and other organs of the digestive system are also examined.
At the doctor's request, the patient changes his body position. In a vertical position, the shape of the organ and the speed of movement of contrast along it are assessed. In the horizontal position, a detailed examination of the esophagus is possible, since in this position barium is evacuated into the stomach much more slowly. There are different patient positions, but especially important is the body position in which an angle of 45° is formed between the pelvis and torso.
An X-ray examination of the esophagus lasts about 40 minutes. At the end of the procedure, you may feel slight nausea that goes away on its own. Barium porridge is excreted from the body along with discolored feces. Due to the astringent effect of barium sulfate, the patient may experience constipation. The contrast is removed from the intestines faster if you take 1.5 liters of water after the procedure.
Preparing and performing radiography
When performing radiography without the use of contrast agents, the walls of the esophagus will not be visualized in the images, which will not allow a full diagnosis of pathological changes. Barium sulfate is used as a contrast agent for x-rays of this organ. A whitish suspension of this component is offered to the patient for oral administration by drinking. Barium sulfate can thus fill the hollow tube of the esophagus and visualize its borders. It is important to know that barium sulfate is a substance completely inert to the human body, which does not affect it in any way and is quickly excreted along with feces.
Among the special instructions for preparing the study, doctors highlight only that x-rays of the esophagus are performed on an empty stomach. You should not eat food for at least 6 hours before the study. The day before the examination, you need to exclude foods that provoke flatulence in the gastrointestinal tract - legumes, cabbage, sweets, fresh baked goods, etc. On the day of the study, you should not eat or drink liquids, including drinking alcohol, and it is also undesirable to smoke. If the gag reflex is pronounced at the time of the procedure and the use of contrast, doctors sometimes give patients antiemetic drugs, but more often there is no need for this.
The X-ray procedure is performed standing. After drinking barium sulfate, the patient must sit upright in a special X-ray machine, then the X-ray technician sets up the machine and asks him to remain motionless and not breathe for several seconds, during which the picture is taken. Sometimes it is necessary to change the position in order to obtain other projections of the examined organ.
After completing the examination, the radiologist deciphers the image for some time and writes a report for the attending physician. When conducting an X-ray examination of the esophagus, no side effects can occur, except for the effect of radiation on the body. The dose is very small, but frequent x-rays are not recommended.
Trendelenburg method
The Trendelenburg radiography technique allows you to see a diaphragmatic hernia. Imaging is performed after the patient has taken barium sulfate in the supine position with the pelvis elevated 45°. In this position, the diaphragm is better visualized, since the intestine extends into the sternum.
The Trendelenburg technique cannot be used if:
- blood, pus or exudate has accumulated in the peritoneum;
- there is oncological damage to the peritoneum and intestines;
- the functionality of the heart and lungs is impaired.
How is the photo taken?
While the patient drinks the barium suspension, the radiologist watches the passage of barium through the esophagus on the fluoroscope screen
The first sip should be small in volume. This is necessary to assess the functional state of the esophagus and detect pronounced narrowings that can become an obstacle to the advancement of contrast. If the patency of the organ is significantly impaired, the administration of a large volume of the drug will only lead to discomfort in the patient and vomiting, but will not increase the information content of the study. If the esophagus is passable, the patient drinks the entire glass of barium.
The study is carried out in the vertical and horizontal position of the patient. The first position helps to assess the shape, location of the organ, as well as the speed at which the contrast agent moves through it. The second is used for a detailed examination of pathological formations, since in this position the evacuation of barium into the stomach slows down.
During an X-ray examination of the esophagus, the following patient positions are used:
- Front straight. The patient lies on his back or stands with his back pressed against the cassette. The upper edge of the latter is located 5 cm above shoulder level.
- Lateral. The patient lies on his side or stands with his side facing the cassette. The arms are bent at the elbows and raised to the head.
- Anterior right oblique. The patient lies or stands so that the right front part of the body is adjacent to the cassette at an angle of 35-40°. The right arm is along the body, the left is bent at the elbow and raised to the head.
- Anterior left oblique. The front left part of the body is pressed against the cassette, the body is turned towards the latter at an angle of 35-40°. The left arm is extended along the body, the right is bent at the elbow and raised to the head.
Anterior AP projection can also be taken in the Trendelenburg position. In this case, the foot end of the table rises at an angle of 45°. The patient's pelvis is higher than the head. This position helps diagnose a hiatal hernia.
Detecting a hernia in the diaphragm
A hiatal hernia is detected using the Trendelenburg method if the following signs are observed:
- Folds characteristic of the gastric wall were found in the esophagus.
- Filling a separate cavity when receiving contrast in an angled position.
- The field of the lung near the cavity formation is darkened.
Indirect symptoms may include:
- reduction in stomach volume;
- lack of gas in the stomach contents;
- the tortuous esophagus above the diaphragm.
As a result of an X-ray examination of the esophagus with barium, the patient is given a radiograph in the form of a digital image or x-ray, as well as a form describing the functional state of the esophagus.
What are the indications for the procedure?
Fluoroscopy is performed to make a diagnosis and to monitor treatment. Therefore, there are some indications for this. Firstly, it is a long-term inflammation of the mucous membrane of the esophageal canal and stomach. A patient with GERD .
Carry out to assess the degree of narrowing of the esophageal tube. In this case, the indication will be the appearance of scar tissue in this organ. The method is used to detect and monitor the treatment of hiatal hernias .
The indication is any disease in the esophageal canal and stomach, with the exception of the special cases described above.
Contraindications
An absolute contraindication is pregnancy. X-rays are not performed for symptoms of esophageal and gastric bleeding. They also do not resort to it when the patient is in serious condition. In these cases, more suitable examination methods are used.
Double contrast method
The essence of the double contrast technique is to inject barium sulfate and simultaneously swallow air. The contrast is distributed evenly after massage of the anterior abdominal wall. The administration of antispasmodics relaxes smooth muscles and suppresses peristaltic contractions of the gastrointestinal tract. The double contrast technique allows you to examine the esophagus and nearby organs in detail. With its help, it is also possible to diagnose a malignant process at an early stage of development, when there are still no symptoms of cancer. Side effects may include diarrhea or, conversely, constipation, as well as other reversible phenomena in the functioning of the digestive system. If these symptoms do not go away, you will need medical advice.
Peristalsis is studied as the contrast passes through the intestine. At the same time, the condition of the mucous membrane is examined. 6 hours after taking the contrast, it appears in the corner between the liver and large intestine. Within 24 hours, the contrast fills the lumen of the colon. Images are taken on days 1, 2, 3.
Description
X-ray of the esophagus refers to non-invasive methods for studying the alimentary tract and other organs of the gastrointestinal tract. The method is based on the use of X-rays to visualize pathologies in the human body. In order to more clearly visualize the esophagus, a contrast agent is used in the form of a water-barium mixture or an iodine-containing preparation. In some cases, it is necessary to do double contrast, in which air under pressure is introduced into the esophagus along with a barium mixture.
X-ray examination of the esophagus has an important feature. The method allows you to assess the state of the organ over time. Along with images of the digestive tract, other organs of the gastrointestinal tract are visualized, and the speed and nature of contrast advancement are assessed. As a result, a complete picture is provided with the anatomical and functional capabilities and reserves of the esophagus. Description is given:
- shape and volume of the organ;
- functional state and integrity of the epithelial mucosa;
- work of sphincter and circular muscles in the walls of the organ.
An X-ray of the esophagus can reveal such deviations from the norm as:
- damage to the mucosa;
- presence of polyps;
- ulcers and their consequences;
- tumors;
- motility disorders.
An x-ray can be taken in a clinic on an outpatient or inpatient basis, as well as in private medical centers.
What can be seen on an x-ray of the esophagus?
The esophagus normally resembles an unevenly dilated tube. After filling with contrast, it acquires smooth outlines. The lumen of the esophagus is freely filled with a barium mixture, while the mucous membrane remains smooth and unchanged. In a vertical position, barium sulfate reaches the stomach in 3-5 seconds, in a horizontal position - 2 times longer.
The safety of the patient and the doctor is a prerequisite for X-ray examination. This is achieved through the use of:
- protective aprons, gloves, screens, glass for the doctor;
- filter made of aluminum 1 mm thick.
Safety is promoted by:
- distance of the X-ray tube from the patient;
- accurate calculations of the transillumination period;
- monitoring previous radiation doses to calculate the total cumulative dose.
Other methods for examining the esophagus
Computed tomography (CT), like x-rays, involves radiation exposure to the patient. However, compared to fluoroscopy, CT has advantages. The image shows not only the esophagus, but also nearby structures. Tomography allows you to evaluate the wall of the esophagus, which is impossible with x-rays. This is important for diagnosing tumors and determining the extent of their spread. However, it is difficult to examine the condition of the mucous membrane using CT and fluoroscopy.
Endoscopy (FGDS) allows you to examine the esophagus from the inside. The stomach is also examined at the same time. The method allows you to observe with your own eyes all pathological changes in the mucous membrane, and, if necessary, take material for a biopsy. During an endoscopic examination, therapeutic measures can also be carried out, for example, removal of a foreign body. However, this procedure is not suitable for assessing the location and shape of the organ and the condition of neighboring formations.
Advantages and disadvantages of fluoroscopy
The advantages of X-ray diagnostics of the esophagus include:
- small doses of x-ray radiation;
- painlessness of the procedure;
- rare allergic reactions to barium sulfate;
- no effect of contrast on the esophagus;
- lack of special preparation for the examination;
- universality of the method, allowing use in different age groups of patients;
- high dynamics of the examination;
- low traumatic method.
The disadvantages of the technique include contraindications for its use during pregnancy and in children under 15 years of age.